The Transformative Power of Music in Mental Well-Being
- August 01, 2023
- Healthy living for mental well-being, Patients and Families, Treatment
Music has always held a special place in our lives, forming an integral part of human culture for centuries. Whether we passively listen to our favorite songs or actively engage in music-making by singing or playing instruments, music can have a profound influence on our socio-emotional development and overall well-being.

Recent research suggests that music engagement not only shapes our personal and cultural identities but also plays a role in mood regulation. 1 A 2022 review and meta-analysis of music therapy found an overall beneficial effect on stress-related outcomes. Moreover, music can be used to help in addressing serious mental health and substance use disorders. 2 In addition to its healing potential, music can magnify the message of diversity and inclusion by introducing people to new cultures and amplifying the voice of marginalized communities, thereby enhancing our understanding and appreciation for diverse communities.

Healing Trauma and Building Resilience
Many historically excluded groups, such as racial/ethnic and sexual minorities and people with disabilities, face systemic injustices and traumatic experiences that can deeply impact their mental health. Research supports the idea that discrimination, a type of trauma, increases risk for mental health issues such as anxiety and depression. 3
Music therapy has shown promise in providing a safe and supportive environment for healing trauma and building resilience while decreasing anxiety levels and improving the functioning of depressed individuals. 4 Music therapy is an evidence-based therapeutic intervention using music to accomplish health and education goals, such as improving mental wellness, reducing stress and alleviating pain. Music therapy is offered in settings such as schools and hospitals. 1 Research supports that engaging in music-making activities, such as drumming circles, songwriting, or group singing, can facilitate emotional release, promote self-reflection, and create a sense of community. 5
Empowerment, Advocacy and Social Change
Music has a rich history of being used as a tool for social advocacy and change. Artists from marginalized communities often use music to shed light on social issues (.pdf) , challenge injustices, and inspire collective action. By addressing topics such as racial inequality, gender discrimination, and LGBTQ+ rights, music becomes a powerful medium for advocating for social justice and promoting inclusivity. Through music, individuals can express their unique experiences, struggles, and triumphs, forging connections with others who share similar backgrounds. Research has shown that exposure to diverse musical genres and artists can broaden perspectives, challenge stereotypes, and foster empathy among listeners especially when dancing together. 7
Genres such as hip-hop, reggae, jazz, blues, rhythm & blues and folk have historically served as platforms for marginalized voices, enabling them to reclaim their narratives and challenge societal norms. The impact of socially conscious music has been observed in movements such as civil rights, feminism, and LGBTQ+ rights, where songs have played a pivotal role in mobilizing communities and effecting change. Music artists who engage in activism can reach new supporters and help their fans feel more connected to issues and motivated to participate. 6

Fostering Social Connection and Support
Music can also serve as a catalyst for social connection and support, breaking down barriers and bridging divides. Emerging evidence indicates that music has the potential to enhance prosocial behavior, promote social connectedness, and develop emotional competence. 2 Communities can leverage music’s innate ability to connect people and foster a sense of belonging through music programs, choirs, and music education initiatives. These activities can create inclusive spaces where people from diverse backgrounds can come together, collaborate, and build relationships based on shared musical interests. These experiences promote social cohesion, combat loneliness, and provide a support network that can positively impact overall well-being.
Musicians and Normalizing Mental Health
Considering the healing effects of music, it may seem paradoxical that musicians may be at a higher risk of mental health disorders. 8 A recent survey of 1,500 independent musicians found that 73% have symptoms of mental illness. This could be due in part to the physical and psychological challenges of the profession. Researchers at the Max Planck Institute for Empirical Aesthetics in Germany found that musically active people have, on average, a higher genetic risk for depression and bipolar disorder.
Commendably, many artists such as Adele, Alanis Morrisette, Ariana Grande, Billie Eilish, Kendrick Lamar, Kid Cudi and Demi Lovato have spoken out about their mental health battles, from postpartum depression to suicidal ideation. Having high-profile artists and celebrities share their lived experiences has opened the conversation about the importance of mental wellness. This can help battle the stigma associated with seeking treatment and support.
Dr. Regina James (APA’s Chief of the Division of Diversity and Health Equity and Deputy Medical Director) notes “Share your story…share your song and let's help each other normalize the conversation around mental wellness through the influence of music. My go-to artist for relaxation is jazz saxophonist, “Grover Washington Jr” …what’s yours?” Submit to [email protected] to get featured!
More on Music Therapy
- Music Therapy Fact Sheets from the American Music Therapy Association
- Music Therapy Resources for Parents and Caregivers from Music Therapy Works
By Fátima Reynolds DJ and Music Producer Senior Program Manager, Division of Diversity and Health Equity American Psychiatric Association
- Gustavson, D.E., et al. Mental health and music engagement: review, framework, and guidelines for future studies. Transl Psychiatry 11, 370 (2021). https://doi.org/10.1038/s41398-021-01483-8
- Golden, T. L., et al. (2021). The use of music in the treatment and management of serious mental illness: A global scoping review of the literature. Frontiers in Psychology, 12. https://doi.org/10.3389/fpsyg.2021.649840
- Schouler-Ocak, M., et al. (2021). Racism and mental health and the role of Mental Health Professionals. European Psychiatry, 64(1). https://doi.org/10.1192/j.eurpsy.2021.2216
- Aalbers, S., et al. (2017). Music therapy for Depression. Cochrane Database of Systematic Reviews, 2017(11). https://doi.org/10.1002/14651858.cd004517.pub3
- Dingle, G. A., et al. (2021). How do music activities affect health and well-being? A scoping review of studies examining Psychosocial Mechanisms. Frontiers in Psychology, 12. https://doi.org/10.3389/fpsyg.2021.713818
- Americans for the Arts. (n.d.). A Working Guide to the Landscape of Arts for Change. Animating Democracy. http://animatingdemocracy.org/sites/default/files/Potts%20Trend%20Paper.pdf
- Stupacher, J., Mikkelsen, J., Vuust, P. (2021). Higher empathy is associated with stronger social bonding when moving together with music. Psychology of Music, 50(5), 1511–1526. https://doi.org/10.1177/03057356211050681
- Wesseldijk, L.W., Ullén, F. & Mosing, M.A. The effects of playing music on mental health outcomes. Sci Rep 9, 12606 (2019). https://doi.org/10.1038/s41598-019-49099-9
Medical leadership for mind, brain and body.
Mobile menu.
- Psychiatrists
- Residents & Medical Students
- Patients and Families
- Advocacy & APAPAC
- Diversity & Health Equity
- Research & Registry
- Meetings & Events
- Search Directories & Databases
- International
- Medical Students
- What is Psychiatry?
- Find a Psychiatrist
- Addiction and Substance Use Disorders
- Dementia and Alzheimer's Disease
- Alcohol Use Disorder
- Anxiety Disorders
- Attention-Deficit/Hyperactivity Disorder (ADHD)
- Autism Spectrum Disorder
- Bipolar Disorders
- Climate Change and Mental Health Connections
- Coping After Disaster
- Disruptive, Impulse-Control and Conduct Disorders
- Dissociative Disorders
- Domestic Violence
- Eating Disorders
- E-Cigarettes and Vaping
- Gambling Disorder
- Gender Dysphoria
- Helping a Loved One Cope with Mental Illness
- Hoarding Disorder
- Integrated Behavioral Healthcare
- Intellectual Disability
- Internet Gaming
- Obsessive-Compulsive Disorder
- Opioid Use Disorder
- Perinatal Depression (formerly Postpartum)
- Personality Disorders
- Posttraumatic Stress Disorder (PTSD)
- Prolonged Grief Disorder
- Schizophrenia
- Seasonal Affective Disorder (SAD)
- Sleep Disorders
- Somatic Symptom Disorder
- Specific Learning Disorders
- Stigma, Prejudice and Discrimination Against People with Mental Illness
- Suicide Prevention
- Technology Addictions: Social Media, Online Gaming, and More
- Warning Signs of Mental Illness
- Electroconvulsive Therapy (ECT)
- What is Mental Illness?
- What is Psychotherapy?
- What is Telepsychiatry?
- La Salud Mental
- Childhood Disorders: Medication Guides for Parents
- Lifestyle to Support Mental Health
- Member Benefits
- Honorary Fellowship (FAPA & DFAPA)
- Awards & Leadership Opportunities
- Get Involved
- Directories, Contact Info & FAQs
- District Branches
- APA's Vision, Mission, Values, and Goals
- Meet Our Organization
- Read APA Organization Documents and Policies
- Work At APA
- About APA's Headquarters
- Policy Finder
- News Releases
- Messages from the APA President
- Reporting on Mental Health Conditions
- Goldwater Rule
- Annual Meeting Press Registration + Guidelines
- APA Public Opinion Polls
- Reporter Toolkit: Recommendations on Covering the AAPI Community
- Comunicados de prensa en español
- APA Annual Meeting
- APA Communities
- APA Foundation
- APA JobCentral
- APA Learning Center
- APA Publishing
- Center for Workplace Mental Health
- Melvin Sabshin, M.D. Library & Archives
- Psychiatric News
- Psychiatry Online
- Annual Meeting
- APA On Demand
- At the APA Educational Series
- Books and Journals
- Certification and Licensure
- Diversity and Health Equity Education Resources
- Meeting Submission and Guidelines
- Mental Health Innovation Zone
- The Mental Health Services Conference
- The Virtual Immersive
- Virtual Paid Courses
- Clinical Practice Guidelines
- Covid-19 / Coronavirus
- Digital Mental Health
- Helping Patients Access Care
- Media and Communications
- Mental Health Apps
- Mental Health Parity
- Practice Management
- Professional Interests
- Quality Improvement
- Risk Management
- Social Media
- Sunshine Act
- Telepsychiatry
- The Clozapine Risk Evaluation and Mitigation Strategy (REMS) Program
- Transition to Practice and Early Career Resources
- Well-being and Burnout
- Mental Health and Faith Community Partnership
- Mental Health Equity Looking Beyond Series
- Minority and Underrepresented (M/UR) Caucuses
- Moore Equity in Mental Health Initiative
- News and Updates
- Striving for Excellence Series
- AMNet: Addiction Medicine Practice Based Research Network
- PsychPRO: APA's Mental Health Registry
- Research Colloquium for Junior Psychiatrist Investigators
- Perinatal Mental Health Toolkit
- Psychiatric Bed Crisis Report
- Advocacy Action Center
- Congressional Advocacy Network
- Election Resource Center
- Federal Affairs
- State Affairs
- Implementing 9-8-8
- Advocacy Update Webinars
- 2025 Annual Meeting
- The 2024 Mental Health Services Conference
- Addressing Structural Racism Town Hall Series
- APA Meetings App
- Governance Meetings
- Mental Health Equity Fireside Chat Series
- Moore Equity in Mental Health 5K
- Policy & Practice Insights Series
- September Component Meetings
- Social Determinants of Mental Health Town Hall Series
- Amicus Briefs
- Assembly Directory
- Component Directory
- Conference Publications
- Library and Archive
- Member Directory
- Member Obituaries
- Practice Guidelines
- Resource Documents
- International Trainees
- International Humanitarian Opportunities
- Global Mental Health
- International Medical Graduates Resources
- Residents' Journal
- Featured Publications
- APA/APAF Fellowships
- External Fellowships and Awards
- Helping Residents Cope with a Patient Suicide
- Vacant Resident Positions
- Leadership Positions
- SET for Success
- Apply for Psychiatric Residency
- Choosing a Career in Psychiatry
- Building a Career in Psychiatry
- Medical Student Programs
- Resident-Fellow Census
- Transitioning to Residency During COVID-19
- What Is a Substance Use Disorder?
- Expert Q&A: Addiction and Substance Use Disorders
- What Are Dementia and Alzheimer’s Disease?
- Expert Q&A: Dementia and Alzheimer's Disease
- What are Anxiety Disorders?
- Expert Q&A: Anxiety Disorders
- What is ADHD?
- Expert Q&A: ADHD
- What Is Autism Spectrum Disorder?
- Expert Q&A: Autism Spectrum Disorder
- What Are Bipolar Disorders?
- Expert Q&A: Bipolar Disorder
- How Extreme Weather Events Affect Mental Health
- Who Is Affected by Climate Change?
- What Is Depression?
- Expert Q&A: Depression
- What are Disruptive, Impulse Control and Conduct Disorders?
- Expert Q&A: Disruptive, Impulse Control and Conduct Disorders
- What Are Dissociative Disorders?
- Expert Q&A: Dissociative Disorders
- What are Eating Disorders?
- Expert Q&A: Eating Disorders
- What is Gambling Disorder?
- Expert Q&A: Gambling Disorder
- What is Gender Dysphoria?
- Expert Q&A: Gender Dysphoria
- What is Hoarding Disorder?
- Expert Q&A: Hoarding Disorder
- What is Intellectual Disability?
- Expert Q&A: Intellectual Disability
- What Is Obsessive-Compulsive Disorder?
- Expert Q&A: Obsessive-Compulsive Disorder
- What is Perinatal Depression (formerly Postpartum)?
- Expert Q&A: Perinatal Depression
- What are Personality Disorders?
- Expert Q&A: Personality Disorders
- What is Posttraumatic Stress Disorder (PTSD)?
- Expert Q&A: Posttraumatic Stress Disorder (PTSD)
- What is Schizophrenia?
- Expert Q&A: Schizophrenia
- What are Sleep Disorders?
- Expert Q&A: Sleep Disorders
- What is Somatic Symptom Disorder?
- Expert Q&A: Somatic Symptom Disorder
- What Are Specific Learning Disorders?
- Expert Q&A: Specific Learning Disorders
- What is Technology Addiction?
- Expert Q&A: Technology Addiction
- Cigarrillos electrónicos y vapeo
- Trastorno del espectro autista
- Trastorno por consumo de alcohol
- Trastorno por consumo de opioides
- Trastorno de estrés postraumático (TEPT)
- Adicción a la tecnología: redes sociales, juegos en línea, y más
- ¿Qué es la psiquiatría?
- Conexiones entre el cambio climático y la salud mental
- Más temas de salud mental
- General Members
- Early Career Psychiatrists
- Residents and Fellows
- International Resident-Fellows
- Semi-Retired and Retired
- View Your Profile
- Resident-Fellow Members
- Fellow of the APA
- Distinguished Fellow of the APA
- International Fellow of the APA
- International Distinguished Fellow of the APA
- 2024 Class of Honorary Fellows
- 2025 APA National Elections
- Councils, Committees and Components
- Resident-Fellow Leadership Opportunities
- Advocacy and APAPAC
- APA Insider Sessions
- APA Specialty Interest Caucuses, Listservs & Communities
- Leadership, Equity and Diversity Institute
- Mentorship Program for APA/APAF Fellows
- Research Colloquium
- Contact Your Membership Specialist
- Contact Your District Branch
- Membership FAQs
- Semi-Retired and Retired FAQs
- Lump Sum Dues
- District Branch Resources
- District Branch Dues for General Members
- District Branch Dues for Residents and Fellows
- Mental Health
How Music Affects Mental Health

If you’ve ever released stress by dancing around your room to your favorite tunes or enjoyed a good cry with the help of a touching love song, you know how powerful music can be. It can lift you up when you’re low and calm you down when you’re anxious.
Music is a powerful tool for mood regulation and stress. The best part is, it’s always available to anyone who needs it.
Benefits of Music
Whether you’re on edge or need a boost, even just one song can bring you back to a more even and healthy place. When it comes to your mental health, music can:
Help you rest better. A study involving students found that listening to relaxing classical music at bedtime improved sleep quality. This activity was also associated with decreased signs of depression.
Lift your mood. Research shows that listening to happier music can make you feel happier, especially if you try to lift your mood while listening. There’s also evidence that formal music therapy can help with depression when used alongside other therapies.
Reduce stress. If you’re feeling anxious or stressed, calming music can help to settle your mind. Several studies have shown that when people undergoing surgery hear calming music, they have lower blood pressure and need less pain medication than those who don’t listen to soothing music.
You don’t have to be preparing for surgery to calm yourself with music, though. Simply listening to music can decrease your blood pressure , lower your levels of the stress hormone cortisol , and reduce your heart rate .
Tips to Use Music to Improve Your Well-Being
Music therapists can help you find ways to use music for your mental health. This type of therapist learns how to use music-making and listening to help people understand and process their emotions. Like traditional mental health counseling, music therapy is customized to the needs of the client.
But you don't necessarily need a therapist. You can also use music on your own to improve your mental well-being:
Listen to relaxing music. The best music for stress reduction is the kind that works for you. If you’re not sure where to start, look for music that plays at about 60 beats per minute. Researchers say that this tempo is best for encouraging the alpha brainwaves that signal a relaxed and conscious mind.
Most streaming services have meditation tracks set at this tempo. Many people also find that Celtic, Native American, and Indian string or flute music tends to have a calming effect.
Express yourself with a beat. You don’t need to be a trained musician to make music. Anyone can grab a rhythm instrument like a drum or rain stick and create beats that are mournful, angry, joyful, or excited.
Try this music therapy technique: By yourself or with a few friends, get some rhythm instruments and create the sounds of a storm. Let the storm become more and less intense, raging for a while and then backing down to a calmer state. Create rhythms that express emotions you’ve been feeling. If you’d like you can talk about those feelings after the improvised storm has passed.
Write a song. The concept of songwriting can scare people away if they feel like the song won’t be “good.” Remember that when you use music therapeutically, it doesn’t matter what other people think of it. They never even have to hear it.
If you feel stuck, start with a song that you already know. Let the melody inspire you to write lyrics that express how you feel. Sing it into your phone and play it back. Hearing your own feelings reflected back to you is an important part of healing through music.
Create a mood playlist . If you’re feeling down, anxious, or upset, find a track that expresses how you feel. Feel those emotions and let the lyrics resonate with you. Then, gradually shift your listening choices so that the music takes you into a happier or calmer place. This is a popular technique used by music therapists.
Limits of Music as a Mood Booster
Matching music to your current mood can feel validating, but it can also keep you stuck in a negative emotional state — if you let it.
You can still listen to a sad song when you’re upset or let out your anger to some heavy metal. Just be mindful of where it’s taking you and shift into something different if you feel yourself getting stuck.
It’s also important to consider that while music can be a powerful tool for regulating and shifting your emotions, it's not a substitute for mental health treatment. If you have distressing emotional experiences that interfere with your ability to function, consider talking to a licensed mental health professional .

Top doctors in ,
Find more top doctors on, related links.
- Mental Health Home
- Mental Health News & Features
- Mental Health Reference
- Mental Health Quizzes
- Mental Health Slideshows
- Mental Health Blogs
- Mental Health Videos
- Find a Psychiatrist
- Anxiety & Panic Disorders
- Bipolar Disorder
- Crisis Assistance
- Eating Disorders
- Health & Balance
- Personality Disorders
- Schizophrenia
- Social Media and Mental Health
- Stress Management
- Substance Abuse & Addiction
- More Related Topics
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Review Article
- Open access
- Published: 22 June 2021
Mental health and music engagement: review, framework, and guidelines for future studies
- Daniel E. Gustavson ORCID: orcid.org/0000-0002-1470-4928 1 , 2 ,
- Peyton L. Coleman ORCID: orcid.org/0000-0001-5388-6886 3 ,
- John R. Iversen 4 ,
- Hermine H. Maes 5 , 6 , 7 ,
- Reyna L. Gordon 2 , 3 , 8 , 9 &
- Miriam D. Lense 2 , 8 , 9
Translational Psychiatry volume 11 , Article number: 370 ( 2021 ) Cite this article
44k Accesses
30 Citations
79 Altmetric
Metrics details
- Medical genetics
- Psychiatric disorders
Is engaging with music good for your mental health? This question has long been the topic of empirical clinical and nonclinical investigations, with studies indicating positive associations between music engagement and quality of life, reduced depression or anxiety symptoms, and less frequent substance use. However, many earlier investigations were limited by small populations and methodological limitations, and it has also been suggested that aspects of music engagement may even be associated with worse mental health outcomes. The purpose of this scoping review is first to summarize the existing state of music engagement and mental health studies, identifying their strengths and weaknesses. We focus on broad domains of mental health diagnoses including internalizing psychopathology (e.g., depression and anxiety symptoms and diagnoses), externalizing psychopathology (e.g., substance use), and thought disorders (e.g., schizophrenia). Second, we propose a theoretical model to inform future work that describes the importance of simultaneously considering music-mental health associations at the levels of (1) correlated genetic and/or environmental influences vs. (bi)directional associations, (2) interactions with genetic risk factors, (3) treatment efficacy, and (4) mediation through brain structure and function. Finally, we describe how recent advances in large-scale data collection, including genetic, neuroimaging, and electronic health record studies, allow for a more rigorous examination of these associations that can also elucidate their neurobiological substrates.
Similar content being viewed by others

Biological principles for music and mental health

A comprehensive investigation into the genetic relationship between music engagement and mental health
The effects of playing music on mental health outcomes
Introduction.
Music engagement, including passive listening and active music-making (singing, instrument playing), impacts socio-emotional development across the lifespan (e.g., socialization, personal/cultural identity, mood regulation, etc.), and is tightly linked with many cognitive and personality traits [ 1 , 2 , 3 ]. A growing literature also demonstrates beneficial associations between music engagement and quality of life, well-being, prosocial behavior, social connectedness, and emotional competence [ 4 , 5 , 6 , 7 , 8 ]. Despite these advances linking engagement with music to many wellness characteristics, we have a limited understanding of how music engagement directly and indirectly contributes to mental health, including at the trait-level (e.g., depression and anxiety symptoms, substance use behaviors), clinical diagnoses (e.g., associations with major depressive disorder (MDD) or substance use disorder (SUD) diagnoses), or as a treatment. Our goals in this scoping review are to (1) describe the state of music engagement research regarding its associations with mental health outcomes, (2) introduce a theoretical framework for future studies that highlight the contribution of genetic and environmental influences (and their interplay) that may give rise to these associations, and (3) illustrate some approaches that will help us more clearly elucidate the genetic/environmental and neural underpinnings of these associations.
Scope of the article
People interact with music in a wide variety of ways, with the concept of “musicality” broadly including music engagement, music perception and production abilities, and music training [ 9 ]. Table 1 illustrates the breadth of music phenotypes and example assessment measures. Research into music and mental health typically focuses on measures of music engagement, including passive (e.g., listening to music for pleasure or as a part of an intervention) and active music engagement (e.g., playing an instrument or singing; group music-making), both of which can be assessed using a variety of objective and subjective measures. We focus primarily on music engagement in the current paper but acknowledge it will also be important to examine how mental health traits relate to other aspects of musicality as well (e.g., perception and production abilities).
Our scoping review and theoretical framework incorporate existing theoretical and mechanistic explanations for how music engagement relates to mental health. From a psychological perspective, studies have proposed that music engagement can be used as a tool for encouraging self-expression, developing emotion regulation and coping skills, and building community [ 10 , 11 ]. From a physiological perspective, music engagement modulates arousal levels including impacts on heart rate, electrodermal activity, and cortisol [ 12 , 13 ]. These effects may be driven in part by physical aspects of music (e.g., tempo) or rhythmic movements involved in making or listening to music, which impact central nervous system functioning (e.g., leading to changes in autonomic activity) [ 14 ], as well as by personality and contextual factors (e.g., shared social experiences) [ 15 ]. Musical experiences also impact neurochemical processes involved in reward processing [ 10 , 13 , 14 , 16 , 17 , 18 ], which are also implicated in mental health disorders (e.g., substance use; depression). Thus, an overarching framework for studying music-mental health associations should integrate the psychological, physiological, and neurochemical aspects of these potential associations. We propose expanding this scope further through consideration of genetic and environmental risk factors, which may give rise to (and/or interact with) other factors to impact health and well-being.
Regarding mental health, it is important to recognize the hierarchical structure of psychopathology [ 19 , 20 ]. Common psychological disorders share many features and cluster into internalizing (e.g., MDD, generalized anxiety disorder (GAD), posttraumatic stress disorder (PTSD)), externalizing (e.g., SUDs, conduct disorder), and thought disorders (e.g., bipolar disorder, schizophrenia), with common variance shared even across these domains [ 20 ]. These higher-order constructs tend to explain much of the comorbidity among individual disorders, and have helped researchers characterize associations between psychopathology, cognition, and personality [ 21 , 22 , 23 ]. We use this hierarchical structure to organize our review. We first summarize the emerging literature on associations between music engagement and generalized well-being that provides promising evidence for associations between music engagement and mental health. Next, we summarize associations between music engagement and internalizing traits, externalizing traits/behaviors, and thought disorders, respectively. Within these sections, we critically consider the strengths and shortcomings of existing studies and how the latter may limit the conclusions drawn from this work.
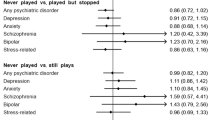
Our review considers both correlational and experimental studies (typically, intervention studies; see Fig. 1 for examples of study designs). We include not only studies that examine symptoms or diagnoses based on diagnostic interviews, but also those that assess quantitative variation (e.g., trait anxiety) in clinical and nonclinical populations. This is partly because individuals with clinical diagnoses may represent the extreme end of a spectrum of similar, sub-clinical, problems in the population, a view supported by evidence that genetic influences on diagnosed psychiatric disorders or DSM symptom counts are similar to those for trait-level symptoms in the general population [ 24 , 25 ]. Music engagement may be related to this full continuum of mental health, including correlations with trait-level symptoms in nonclinical populations and alleviation of symptoms from clinical disorders. For example, work linking music engagement to subjective well-being speaks to potential avenues for mental health interventions in the population at large.
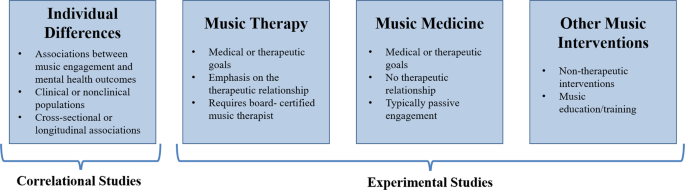
Within experimental studies, music interventions can include passive musical activities (e.g., song listening, music and meditation, lyric discussion, creating playlists) or active musical activities (e.g., creative methods, such as songwriting or improvisation and/or re-creative methods, such as song parody).
The goal of this scoping review was to integrate across related, but often disconnected, literatures in order to propose a comprehensive theoretical framework for advancing our understanding of music-mental health associations. For this reason, we did not conduct a fully systematic search or quality appraisal of documents. Rather, we first searched PubMed and Google Scholar for review articles and meta-analyses using broad search terms (e.g., “review” and “music” and [“anxiety” or “depression” or “substance use”]). Then, when drafting each section, we searched for additional papers that have been published more recently and/or were examples of higher-quality research in each domain. When giving examples, we emphasize the most recent and most well-powered empirical studies. We also conducted some targeted literature searches where reviews were not available (e.g., “music” and [“impulsivity” or “ADHD”]) using the same databases. Our subsequent framework is intended to contextualize diagnostic, symptom, and mechanistic findings more broadly within the scope of the genetic and environmental risk factors on psychopathology that give rise to these associations and (potentially) impact the efficacy of treatment efforts. As such, the framework incorporates evidence from review articles and meta-analyses from various literatures (e.g., music interventions for anxiety [ 26 ], depression [ 27 ]) in combination with experimental evidence of biological underpinnings of music engagement and the perspective provided by newly available methods for population-health approaches (i.e., complex trait genetics, gene–environment interactions).
Music engagement and well-being
A growing body of studies report associations between music engagement and general indices of mental health, including increased well-being or emotional competence, lending support for the possibility that music engagement may also be associated with better specific mental health outcomes. In over 8000 Swedish twins, hours of music practice and self-reported music achievement were associated with better emotional competence [ 5 ]. Similarly, a meta-ethnography of 46 qualitative studies revealed that participation in music activities supported well-being through management of emotions, facilitation of self-development, providing respite from problems, and facilitating social connections [ 28 ]. In a sample of 1000 Australian adults, individuals who engaged with music, such as singing or dancing with others or attending concerts reported greater well-being vs. those who engaged in these experiences alone or did not engage. Other types of music engagement, such as playing an instrument or composing music were not associated with well-being in this sample [ 4 ]. Earlier in life, social music experiences (including song familiarity and synchronous movement to music) are associated with a variety of prosocial behaviors in infants and children [ 6 ], as well as positive affect [ 7 ]. Thus, this work provides some initial evidence that music engagement is associated with better general mental health outcomes in children and adults with some heterogeneity in findings depending on the specific type of music engagement.
Music engagement and internalizing problems
MDD, GAD, and PTSD are the most frequently clustered aspects of internalizing psychopathology [ 19 , 24 , 29 , 30 ]. Experimental studies provide evidence for the feasibility of music intervention efforts and their therapeutic benefits but are not yet rigorous enough to draw strong conclusions. The most severe limitations are small samples, the lack of appropriate control groups, few interventions with multiple sessions, and publications omitting necessary information regarding the intervention (e.g., intervention fidelity, inclusion/exclusion criteria, education status of intervention leader) [ 31 , 32 , 33 ]. Correlational studies, by contrast, suggest musicians are at greater risk for internalizing problems, but that they use music engagement as a tool to help manage these problems [ 34 , 35 ].
Experimental studies
Randomized controlled trials have revealed that music interventions (including both music therapies administered by board-certified music therapists and other music interventions) are associated with reduced depression, anxiety, and PTSD symptoms [ 26 , 27 , 33 , 36 ]. A review of 28 studies reported that 26 revealed significantly reduced depression levels in music intervention groups compared to control groups, including the 9 studies which included active non-music intervention control groups (e.g., reading sessions, “conductive-behavior” psychotherapy, antidepressant drugs) [ 27 ]. A similar meta-analysis of 19 studies demonstrated that music listening is effective at decreasing self-reported anxiety in healthy individuals [ 26 ]. A review of music-based treatment studies related to PTSD revealed similar conclusions [ 36 ], though there were only four relevant studies. More recent studies confirm these findings [ 37 , 38 , 39 ], such as one randomized controlled trial that demonstrated reduced depression symptoms in older adults following musical improvisation exercises compared to an active control group (gentle gymnastic activities) [ 39 ].
This work is promising given that some studies have observed effects even when compared to traditional behavior therapies [ 40 , 41 ]. However, there are relatively few studies directly comparing music interventions to traditional therapies. Some music interventions incorporate components of other therapeutic methods in their programs including dialectic or cognitive behavior therapies [ 42 ], but few directly compare how the inclusion of music augments traditional behavioral therapy. Still other non-music therapies incorporate music into their practice (e.g., background music in mindfulness therapies) [ 43 , 44 ], but the specific contribution of music in these approaches is unclear. Thus, there is a great need for further systematic research relating music to traditional therapies to understand which components of music interventions act on the same mechanisms as traditional therapies (e.g., developing coping mechanisms and building community) and which bolster or synchronize with other approaches (e.g., by adding structure, reinforcement, predictability, and social context to traditional approaches).
Aside from comparison with other therapeutic approaches, an earlier review of 98 papers from psychiatric in-patient studies concluded that promising effects of music therapy were limited by small sample sizes and methodological shortcomings including lack of reporting of adverse events, exclusion criteria, possible confounders, and characteristics of patients lost to follow-up [ 33 ]. Other problems included inadequate reporting of information on the source population (e.g., selection of patients and proportion agreeing to take part in the study), the lack of masking of interviewers during post-test, and concealment of randomization. Nevertheless, there was some evidence that therapies with active music participation, structured sessions, and multiple sessions (i.e., four or more) improved mood, with all studies incorporating these characteristics reporting significant positive effects. However, most studies have focused on passive interventions, such as music listening [ 26 , 27 ]. Active interventions (e.g., singing, improvising) have not been directly compared with passive interventions [ 27 ], so more work is needed to clarify whether therapeutic effects are indeed stronger with more engaging and active interventions.
Correlational studies
Correlational studies have focused on the use of music in emotional self-regulation. Specifically, individuals high in neuroticism appear to use music to help regulate their emotions [ 34 , 35 ], with beneficial effects of music engagement on emotion regulation and well-being driven by cognitive reappraisal [ 45 ]. Music listening may also moderate the association between neuroticism and depression in adolescents [ 46 ], consistent with a protective effect.
A series of recent studies have used validated self-reported instruments that directly assess how individuals use music activities as an emotion regulation strategy [ 47 , 48 , 49 , 50 ]. In adults, the use of music listening for anger regulation and anxiety regulation was positively associated with subjective well-being, psychological well-being, and social well-being [ 50 ]. In studies of adolescents and undergraduates, the use of music listening for entertainment was associated with fewer depression and anxiety symptoms [ 51 ]. “Healthy” music engagement in adolescents (i.e., using music for relaxation and connection with others) was also positively associated with happiness and school satisfaction [ 49 ]. However, the use of music listening for emotional discharge was also associated with greater depression, anxiety, and stress symptoms [ 51 ], and “unhealthy” music engagement (e.g., ‘hiding’ in music to block others out) was associated with lower well-being, happiness, school satisfaction, and greater depression and rumination [ 49 ]. Other work has highlighted the role of valence in these associations, with individuals who listen to happier music when they are in a bad mood reporting stronger ability for music to influence their mood than those who listen to sad music while in a negative mood [ 52 , 53 ].
This work highlights the importance of considering individuals’ motivations for engaging with music in examining associations with well-being and mental health, and are consistent with the idea that individuals already experiencing depression, anxiety, and stress use music as a therapeutic tool to manage their emotions, with some strategies being more effective than others. Of course, these correlational effects may not necessarily reflect causal associations, but could be due to bidirectional influences, as suggested by claims that musicians may be at higher risk for internalizing problems [ 54 , 55 , 56 ]. It is also necessary to consider demographic and socioeconomic factors in these associations [ 57 ], for example, because arts engagement may be more strongly associated with self-esteem in those with higher education [ 58 ].
It is also necessary to clarify if musicians (professional and/or nonprofessional) represent an already high-risk group for internalizing problems. In one large study conducted in Norway ( N = 6372), professional musicians were higher in neuroticism than the general population [ 56 ]. Another study of musician cases ( N = 9803) vs. controls ( N = 49,015) identified in a US-based research database through text-mining of medical records found that musicians are at greater risk of MDD (Odds ratio [OR] = 1.21), anxiety disorders (OR = 1.25), and PTSD (OR = 1.13) [ 55 ]. However, other studies demonstrate null associations between musician status and depression symptoms [ 5 ] or mixed associations [ 59 ]. In N = 10,776 Swedish twins, for example, professional and amateur musicians had more self-reported burnout symptoms [ 54 ]. However, neither playing music in the past, amateur musicianship, nor professional musicianship was significantly associated with depression or anxiety disorder diagnoses.
Even if musicians are at higher risk, such findings can still be consistent with music-making being beneficial and therapeutic (e.g., depression medication use is elevated in individuals with depressive symptoms because it is a treatment). Clinical samples may be useful in disentangling these associations (i.e., examining if those who engage with music more frequently have reduced symptoms), and wider deployment of measures that capture emotion regulation strategies and motivations for engaging with music will help shed light on whether high-risk individuals engage with music in qualitatively different ways than others [ 51 , 57 ]. Later, we describe how also considering the role of genetic and environmental risk factors in these associations (e.g., if individuals at high genetic and/or environmental risk self-select into music environments because they are therapeutic) can help to clarify these questions.
Music engagement and externalizing problems
The externalizing domain comprises SUDs, and also includes impulsivity, conduct disorder, and attention-deficit hyperactivity disorder (ADHD), especially in adolescents [ 20 , 24 , 60 , 61 ]. Similar to the conclusions for internalizing traits, experimental studies show promising evidence that music engagement interventions may reduce substance use, ADHD, and other externalizing symptoms, but conclusions are limited by methodological limitations. Correlational evidence is sparce, but there is less reason to suspect musicians are at higher risk for externalizing problems.
Intervention studies have demonstrated music engagement is helpful in patients with SUDs, including reducing withdrawal symptoms and stress, allowing individuals to experience emotions without craving substance use, and making substance abuse treatment sessions more enjoyable and motivating [ 62 , 63 , 64 ] (for a systematic review, see [ 65 ]). Similar to the experimental studies of internalizing traits, however, these studies would also benefit from larger samples, better controls, and higher-quality reporting standards.
Music intervention studies for ADHD are of similar quality. Such interventions have been shown to reduce inattention [ 66 ], decrease negative mood [ 67 ], and increase reading comprehension for those with ADHD [ 68 ]. However, there is a great amount of variability among children with ADHD, as some may find music distracting while others may focus better in the presence of music [ 69 ].
Little research has been conducted to evaluate music engagement interventions for impulsivity or conduct disorder problems, and findings are mixed. For example, a music therapy study of 251 children showed that beneficial effects on communication skills (after participating in a free improvisation intervention) was significant, though only for the subset of children above age 13 [ 70 ]. Another study suggested the promising effects of music therapy on social skills and problem behaviors in 89 students selected based on social/emotional problem behaviors, but did not have a control group [ 71 ]. Other smaller studies ( N < 20 each) show inconsistent results on disruptive behaviors and aggression [ 72 , 73 ].
Correlational studies on externalizing traits are few and far between. A number of studies examined how listening habits for different genres of music relate to more or less substance use [ 74 , 75 , 76 , 77 ]. However, these studies do not strongly illuminate associations between music engagement and substance use because musical genres are driven by cultural and socioeconomic factors that vary over the lifespan. In the previously cited large study of American electronic medical records [ 55 ] where musicianship was associated with more internalizing diagnoses, associations were nonsignificant for “tobacco use disorder” (OR = 0.93), “alcoholism” (OR = 1.01), “alcohol-related disorders” (OR = 1.00), or “substance addiction and disorders” (OR = 1.00). In fact, in sex-stratified analyses, female musicians were at significantly decreased risk for tobacco use disorder (OR = 0.85) [ 55 ]. Thus, there is less evidence musicians are at greater risk for externalizing problems than in other areas.
Regarding other aspects of externalizing, some studies demonstrate children with ADHD have poor rhythm skills, opening a possibility that working on rhythm skills may impact ADHD [ 78 , 79 ]. For example, music might serve as a helpful scaffold (e.g., for attention) due to its regular, predictable rhythmic beat. It will be important to examine whether these associations with music rhythm are also observed for measures of music engagement, especially in larger population studies. Finally, musicians were reported to have lower impulsiveness than prior population samples, but were not compared directly to non-musicians [ 80 , 81 ].
Music engagement and thought disorders
Thought disorders typically encompass schizophrenia and bipolar disorder [ 20 ]. Trait-level measures include schizotypal symptoms and depression symptoms. Much like internalizing, music interventions appear to provide some benefits to individuals with clinical diagnoses, but musicians may be at higher risk for thought disorders. Limitations of both experimental and correlational studies are similar to those for internalizing and externalizing.
Music intervention studies have been conducted with individuals with schizophrenia and bipolar disorder. A recent meta-analysis of 18 music therapy studies for schizophrenia (and similar disorders) [ 82 ] demonstrated that music therapy plus standard care (compared to standard care alone) demonstrated improved general mental health, fewer negative symptoms of schizophrenia, and improved social functioning. No effects were observed for general functioning or positive symptoms of schizophrenia. Critiques echoed those described above. Most notably, although almost all studies had low risk of biases due to attrition, unclear risk of bias was evident in the vast majority of studies (>75%) for selection bias, performance bias, detection bias, and reporting bias. These concerns highlight the need for these studies to report more information about their study selection, blinding procedure, and outcomes.
More recent papers suggest similar benefits of music therapies in patients with psychosis [ 83 ] and thought disorders [ 84 ], with similar limitations (e.g., one study did not include a control group). Finally, although a 2021 review did not uncover more recent articles related to bipolar disorder, they argued that existing work suggests music therapy has the potential both to treat bipolar disorder symptoms and alleviate subthreshold symptoms in early stages of the disorder [ 85 ].
Much like internalizing, findings from the few existing studies suggest that musicians may be at higher risk for thought disorders. In the large sample of Swedish twins described earlier [ 54 ], playing an instrument was associated with more schizotypal symptoms across multiple comparisons (professional musicians vs. non-players; amateur musicians vs. non-players; still plays an instrument vs. never played). However, no associations were observed for schizophrenia or bipolar disorder diagnoses across any set of comparison groups. Another study demonstrated that individuals with higher genetic risk for schizophrenia or bipolar disorder were more likely to be a member of a creative society (i.e., actor or dancer, musician, visual artist, or writer) or work in a profession in these fields [ 86 ]. Furthermore, musician status was associated with “bipolar disorder” (OR = 1.18) and “schizophrenia and other psychotic disorders” (OR = 1.18) in US electronic health records (EHRs) [ 55 ].
Interim summary
There is promising evidence that music engagement is associated with better mental health outcomes. Music engagement is positively associated with quality of life, well-being, social connectedness, and emotional competence. However, some individuals who engage with music may be at higher risk for mental health problems, especially internalizing and thought disorders. More research is needed to disentangle these contrasting results, including clarifying how “healthy” music engagement (e.g., for relaxation or social connection) leads to greater well-being or successful emotion regulation, and testing whether some individuals are more likely to use music as a tool to regulate emotions (e.g., those with high neuroticism) [ 34 , 35 ]. Similarly, it will be important to clarify whether the fact that musicians may be an at-risk group is an extension of working in an artistic field in general (which may feature lower pay or lack of job security) and/or if similar associations are observed with continuous music engagement phenotypes (e.g., hours of practice). As we elaborate on later, genetically informative datasets can help clarify these complex associations, for example by tested whether musicians are at higher genetic risk for mental health problems but their music engagement mitigates these risks.
Music intervention studies are feasible and potentially effective at treating symptoms in individuals with clinical diagnoses, including depression, anxiety, and SUDs. However, it will be essential to expand these studies to include larger samples, random sampling, and active control groups that compare the benefits of music interventions to traditional therapies and address possible confounds. These limitations make it hard to quantify how specific factors influence the effectiveness of interventions, such as length/depth of music training, age of sample, confounding variables (e.g., socioeconomic status), and type of intervention (e.g., individual vs. group sessions, song playing vs. songwriting, receptive vs. active methods). Similarly, the tremendous breadth of music engagement activities and measures makes it difficult to identify the specific aspects of music engagement that convey the most benefits to health and well-being [ 87 ]. It is therefore necessary to improve reporting quality of studies so researchers can better identify these potential moderators or confounds using systematic approaches (e.g., meta-analyses).
Various mechanisms have been proposed to explain the therapeutic effects of music on mental health, including psychological (e.g., building communities, developing coping strategies) [ 10 , 11 ] and specific neurobiological drivers (e.g., oxytocin, cortisol, autonomic nervous system activity) [ 12 , 13 , 14 ]. However, it will be vital to conduct more systematic research comparing the effects of music interventions to existing therapeutic methods and other types of creative activities (e.g., art [ 88 ]) to quantify which effects and mechanisms are specific to music engagement. Music interventions also do not have to be an alternative to other treatments, but may instead support key elements of traditional interventions, such as being engaging, enjoyable, providing social context, and increasing structure and predictability [ 89 ]. Indeed, some music therapists incorporate principals from existing psychotherapeutic models [ 42 , 90 ] and, conversely, newer therapeutic models (e.g., mindfulness) incorporate music into their practice [ 43 , 44 ]. It is not yet possible to disentangle which aspects of music interventions best synergize with or strengthen standard psychotherapeutic practices (which are also heterogeneous), but this will be possible with better reporting standards and quality experimental design.
To encapsulate and extend these ideas, we next propose a theoretical framework that delineates key aspects of how music engagement may relate to mental health, which is intended to be useful for guiding future investigations in a more systematic way.
Theoretical framework for future studies
Associations between music engagement and mental health may take multiple forms, driven by several different types of genetic predispositions and environmental effects that give rise to, and interact with, proposed psychological and neurobiological mechanisms described earlier. Figure 2 displays our theoretical model in which potential beneficial associations with music are delineated into testable hypotheses. Four key paths characterize specific ways in which music engagement may relate to (and influence) mental health traits, and thus represent key research questions to be addressed in future studies.
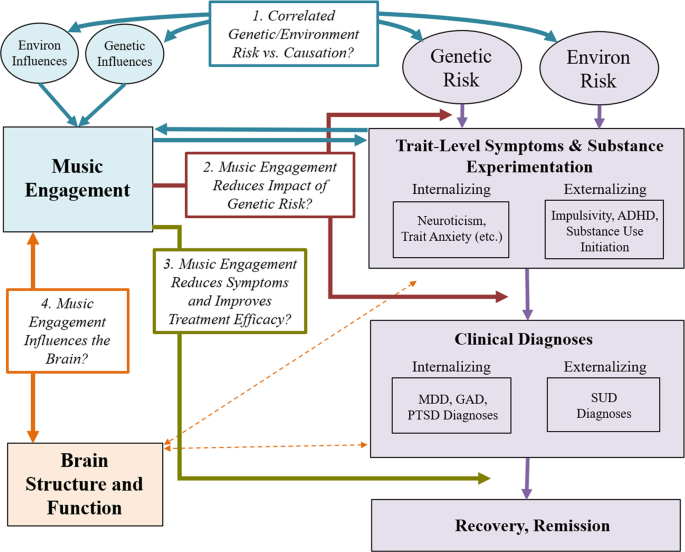
Progression of mental health problems is based on a diathesis-stress model, where genetic predispositions and environmental exposures result in later problems (which can be remedied through treatment). Potential associations with music engagement include (Path 1; blue arrows) correlated genetic/environmental influences and/or causal associations between music engagement and trait-level mental health outcomes; (Path 2; red arrows) interactions between music engagement and risk factors to predict later trait-level or clinical level symptoms; and (Path 3; gold arrow) direct effects of music engagement on reducing symptoms or improving treatment efficacy. Path 4 (orange arrows) illustrates the importance of understanding how these potential protective associations are driven by neuroanatomy and function. MDD major depressive disorder, GAD generalized anxiety disorder, PTSD posttraumatic stress disorder, SUD substance use disorder(s).
Path 1: Music engagement relates to mental health through correlated genetic and environmental risk factors and/or causation
The diathesis-stress model of psychiatric disease posits that individuals carry different genetic liabilities for any given disorder [ 91 , 92 , 93 ], with disorder onset depending on the amount of negative vs. protective environmental life events and exposures the individual experiences. Although at first glance music engagement appears to be an environmental exposure, it is actually far from it. Twin studies have demonstrated that both music experiences and music ability measures are moderately heritable and genetically correlated with cognitive abilities like non-verbal intelligence [ 94 , 95 , 96 , 97 ]. Music engagement may be influenced by its own set of environmental influences, potentially including socioeconomic factors and availability of instruments. Thus, music engagement can be viewed as a combination of genetic and environmental predispositions and availability of opportunities for engagement [ 98 ] that are necessary to consider when evaluating associations with mental health [ 54 ].
When examining music-mental health associations, it is thus important to evaluate if associations are in part explained by correlated genetic or environmental influences (see Fig. 3 for schematic and explanation for interpreting genetic/environmental correlations). On one hand, individuals genetically predisposed to engage with music may be at lower risk of experiencing internalizing or externalizing problems. Indeed, music engagement and ability appear associated with cognitive abilities through genetic correlations [ 3 , 99 ], which may apply to music-mental health associations as well. On the other, individuals at high genetic risk for neuroticism or psychopathology may be more likely to engage with music because it is therapeutic, suggesting a genetic correlation in the opposite direction (i.e., increased genetic risk for musicians). To understand and better contextualize the potential therapeutic effects of music engagement, it is necessary to quantify these potential genetic associations, while simultaneously evaluating whether these associations are explained by correlated environmental influences.
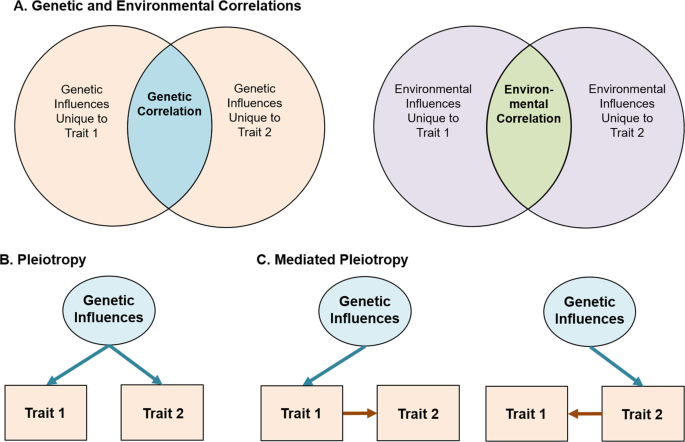
Variance in any given trait is explained by a combination of genetic influences (i.e., heritability) and environmental influences. For complex traits (e.g., MDD or depression symptoms), cognitive abilities (e.g., intelligence), and personality traits (e.g., impulsivity), many hundreds or thousands of independent genetic effects are combined together in the total heritability estimate. Similarly, environmental influences typically represent a multitude of factors, from individual life events to specific exposures (e.g., chemicals, etc.). The presence of a genetic or environmental correlation between traits indicates that some set of these influences have an impact on multiple traits. A Displayed using a Venn diagram. Identifying the strength of genetic vs. environmental correlations can be useful in testing theoretical models and pave the way for more complex genetic investigations. Beyond this, gene identification efforts (e.g., genome-wide association studies) and additional analyses of the resulting data can be used to classify whether these associations represent specific genetic influences that affect both traits equally (i.e., genetic pleiotropy ( B )) or whether a genetic influence impacts only one trait which in turn causes changes in the other (i.e., mediated genetic pleiotropy ( C )). Environmental influences can also act pleiotropically or in a mediated-pleiotropy manner, but only genetic influences are displayed for simplicity.
Beyond correlated genetic and environmental influences, music engagement and mental health problems may be associated with one another through direct influences (including causal impacts). This is in line with earlier suggestions that music activities (e.g., after-school programs, music practice) engage adolescents, removing opportunities for drug-seeking behaviors [ 100 ], increasing their social connections to peers [ 101 ], and decreasing loneliness [ 41 ]. Reverse causation is also possible, for example, if experiencing mental health problems causes some individuals to seek out music engagement as a treatment. Longitudinal and genetically informative studies can help differentiate correlated risk factors (i.e., genetic/environmental correlations) from causal effects of music engagement (Fig. 2 , blue arrows) [ 102 ].
Path 2: Engagement with music reduces the impact of genetic risk
Second, genetic and environmental influences may interact with each other to influence a phenotype. For example, individual differences in music achievement are more pronounced in those who engage in practice or had musically enriched childhood environments [ 97 , 98 ]. Thus, music exposures may not influence mental health traits directly but could impact the strength of the association between genetic risk factors and the emergence of trait-level symptoms and/or clinical diagnoses. Such associations might manifest as decreased heritability of trait-level symptoms in musicians vs. non-musicians (upper red arrow in Fig. 2 ). Alternatively, if individuals high in neuroticism use music to help regulate their emotions [ 34 , 35 ], those who are not exposed to music environments might show stronger associations between neuroticism and later depressive symptoms or diagnoses than those engaged with music (lower red arrow in Fig. 2 ). Elucidating these possibilities will help disentangle the complex associations between music and mental health and could be used to identify which individuals would benefit most from a music intervention (especially preventative interventions). Later, we describe some specific study designs that can test hypotheses regarding this gene-environment interplay.
Path 3: Music engagement improves the efficacy of treatment (or acts as a treatment)
For individuals who experience severe problems (e.g., MDD, SUDs), engaging with music may reduce symptoms or improve treatment outcomes. This is the primary goal of most music intervention studies [ 27 , 33 ] (Fig. 2 , gold arrow). However, and this is one of the central messages of this model, it is important to consider interventions in the context of the paths discussed above. For example, if music engagement is genetically correlated with increased risk for internalizing or externalizing problems (Path 1) and/or if individuals at high genetic risk for mental health problems have already been using music engagement to develop strategies to deal with subthreshold symptoms (Path 2), then may be more likely to choose music interventions over other alternatives and find them more successful. Indeed, the beneficial aspects of music training on cognitive abilities appear to be drastically reduced in samples that were randomly sampled [ 103 ]. Therefore, along with other necessary reporting standards discussed above [ 32 , 33 ], it will be useful for studies to report participants’ prior music experience and consider these exposures in evaluating the efficacy of interventions.
Path 4: Music engagement influences brain structure and function
Exploring associations between music engagement and brain structure and function will be necessary to elucidate the mechanisms driving the three paths outlined above. Indeed, there are strong links between music listening and reward centers of the brain [ 104 , 105 ] including the nucleus accumbens [ 106 , 107 ] and ventral tegmental areas [ 108 ] that are implicated in the reward system for all drugs of abuse [ 109 , 110 , 111 , 112 ] and may relate to internalizing problems [ 113 , 114 , 115 ]. Moreover, activity in the caudate may simultaneously influence rhythmic sensorimotor synchronization, monetary reward processing, and prosocial behavior [ 116 ]. Furthermore, music listening may help individuals control the effect of emotional stimuli on autonomic and physiological responses (e.g., in the hypothalamus) and has been shown to induce the endorphinergic response blocked by naloxone, an opioid antagonist [ 18 , 117 ].
This work focusing on music listening and reward processing has not been extended to music making (i.e., active music engagement), though some differences in brain structure and plasticity between musicians and non-musicians have been observed for white matter (e.g., greater fractional anisotropy in corpus callosum and superior longitudinal fasciculus) [ 118 , 119 , 120 , 121 ]. In addition, longitudinal studies have revealed that instrument players show more rapid cortical thickness maturation in prefrontal and parietal areas implicated in emotion and impulse control compared to non-musician children/adolescents [ 122 ]. Importantly, because the existing evidence is primarily correlational, these cross-sectional and longitudinal structural differences between musicians and non-musicians could be explained by genetic correlations, effects of music training, or both, making them potentially relevant to multiple paths in our model (Fig. 2 ). Examining neural correlates of music engagement in more detail will shed light on these possibilities and advance our understanding of the correlates and consequences of music engagement, and the mechanisms that drive the associations discussed above.
New approaches to studying music and mental health
Using our theoretical model as a guide, we next highlight key avenues of research that will help disentangle these music-mental health associations using state-of-the-art approaches. They include the use of (1) genetic designs, (2) neuroimaging methods, and (3) large biobanks of EHRs.
Genetic designs
Genetic designs provide a window into the biological underpinnings of music engagement [ 123 ]. Understanding the contribution of genetic risk factors is crucial to test causal or mechanistic models regarding potential associations with mental health. At the most basic level, twin and family studies can estimate genetic correlations among music ability or engagement measures and mental health traits or diagnoses. Genetic associations can be examined while simultaneously quantifying environmental correlations, as well as evaluating (bidirectional) causal associations, by testing competing models or averaging across different candidate models [ 102 , 124 ], informing Path 1.
By leveraging samples with genomic, music engagement, and mental health data, investigators can also examine whether individuals at higher genetic risk for psychopathology (e.g., for MDD) show stronger associations between music engagement measures and their mental health outcomes (Path 2). As a theoretical example, individuals with low genetic risk for MDD are unlikely to have many depressive symptoms regardless of their music engagement, so the association between depressive symptoms and music engagement may be weak if focusing on these individuals. However, individuals at high genetic risk for MDD who engage with music may have fewer symptoms than their non-musician peers (i.e., a stronger negative correlation). This is in line with recent work revealing the heritability of depression is doubled in trauma exposed compared to non-trauma exposed individuals [ 125 ].
Gene–environment interaction studies using polygenic scores (i.e., summed indices of genetic risk based on genome-wide association studies; GWAS) are becoming more common [ 126 , 127 ]. There are already multiple large GWAS of internalizing and externalizing traits [ 128 , 129 , 130 ], and the first large-scale GWAS of a music measure indicates that music rhythm is also highly polygenic [ 131 ]. Importantly, is not necessary to have all traits measured in the same sample to examine cross-trait relationships. Studies with only music engagement and genetic data, for example, can still examine how polygenic scores for depression predict music engagement, or interact with music engagement measures to predict other study outcomes. Figure 4 displays an example of a GWAS and how it can be used to compute and apply a polygenic score to test cross-trait predictions.
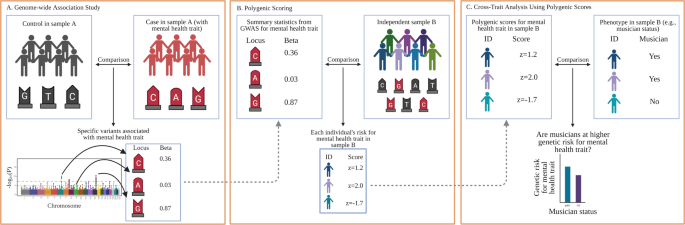
A GWAS are conducted by examining whether individual genetic loci (i.e., single-nucleotide polymorphisms, or SNPs, depicted with G, A, C, and T labels within a sample (or meta-analysis) differentiate cases from controls. The example is based on a dichotomous mental health trait (e.g., major depressive disorder diagnosis), but GWAS can be applied to other dichotomous and continuous phenotypes, such as trait anxiety, musician status, or hours of music practice. Importantly, rather than examining associations on a gene-by-gene basis, GWAS identify relevant genetic loci using SNPs from across the entire genome (typically depicted using a Manhattan plot, such as that displayed at the bottom of A ). B After a GWAS has been conducted on a given trait, researchers can use the output to generate a polygenic score (sometimes called a polygenic risk score) in any new sample with genetic data by summing the GWAS effect sizes for each SNP allele present in a participant’s genome. An individual with a z = 2.0 would have many risk SNPs for that trait, whereas an individual with z = −2 would have much fewer risk SNPs. C Once a polygenic score is generated for all participants, it can be applied like any other variable in the new sample. In this example, researchers could examine whether musicians are at higher (or lower) genetic risk for a specific disorder. Other more complex analyses are also possible, such as examining how polygenic scores interact with existing predictors (e.g., trauma exposure) or polygenic scores for other traits to influence a phenotype or predict an intervention outcome. Created with BioRender.com.
Finally, longitudinal twin and family studies continue to be a promising resource for understanding the etiology and developmental time-course of the correlates of mental health problems. Such designs can be used to examine whether associations between music and mental health are magnified based on other exposures or psychological constructs (gene-by-environment interactions) [ 132 ], and whether parents engaged with music are more likely to pass down environments that are protective or hazardous for later mental health (gene-environment correlations) in addition to passing on their genes. These studies also provide opportunities to examine whether these associations change across key developmental periods. The publicly available Adolescent Brain Cognitive Development study, for example, is tracking over 10,000 participants (including twin and sibling pairs) throughout adolescence, with measures of music engagement and exhaustive measures of mental health, cognition, and personality, as well as neuroimaging and genotyping [ 133 , 134 ]. Although most large samples with genomic data still lack measures of music engagement, key musical phenotypes could be added to existing study protocols (or to similar studies under development) with relatively low participant burden [ 135 ]. Musical questionnaires and/or tasks may be much more engaging and enjoyable than other tasks, improving volunteers’ research participation experience.
Neuroimaging
Another way to orient the design of experiments is through the exploration of neural mechanisms by which music might have an impact on mental health. This is an enormous, growing, and sometimes fraught literature, but there is naturally a great potential to link our understanding of neural underpinnings of music listening and engagement with the literature on neural bases of mental health. These advances can inform the mechanisms driving successful interventions and inform who may benefit the most from such interventions. We focus on two areas among many: (1) the activation of reward circuitry by music and (2) the impact music has on dynamic patterns of neural activity, both of which are likely vectors for the interaction of music and mental health and provide examples of potential interactions.
Music and reward
The strong effect of music on our emotions has been clearly grounded in its robust activation of reward circuitry in the brain, and motivational and hedonic effects of music listening have been shown to be specifically modulated by dopamine [ 16 , 105 , 136 ]. The prevalence of reward and dopaminergic dysfunction in mental illness makes this a rich area for future studies. For example, emotional responses to music might be used as a substitute for reward circuit deficiencies in depression, and it is intriguing to consider if music listening or music engagement could potentiate such function [ 137 , 138 ].
Music and brain network dynamics
The search for neuronally based biomarkers of aspects of mental illness has been a central thrust within the field [ 139 ], holding promise for the understanding of heterogeneity within disorders and identification of common mechanistic pathways [ 140 ]. A thorough review is beyond the scope of this paper, but several points of contact can be highlighted that might suggest neuro-mechanistic mediators of musical effects on mental health. For example, neurofeedback-directed upregulation of activity in emotion circuitry has been proposed as a therapy for MDD [ 141 ]. Given the emotional effects of music, there is potential for using musical stimuli as an adjuvant, or as a more actively patient-controlled output target for neurofeedback. Growing interest in measures of the dynamic complexity of brain activity in health and disease as measured by magnetic resonance imaging or magneto/electroencephalography (M/EEG) [ 142 ] provides a second point of contact, with abnormalities in dynamic complexity suggested as indicative of mental illness [ 143 ], while music engagement has been suggested to reflect and perhaps affect dynamic complexity [ 144 , 145 ].
The caveats identified in this review apply equally to such neuro-mechanistic studies [ 146 ]. High-quality experimental design (involving appropriate controls and randomized design) has been repeatedly shown to be critical to providing reliable evidence for non-music outcomes of music engagement [ 103 ]. For such studies to have maximal impact, analysis of M/EEG activity not at the scalp level, but at the source level, has been shown to improve the power of biomarkers, and their mechanistic interpretability [ 147 , 148 ]. Moreover, as with genetic influences that typically influence a trait through a multitude of small individual effects [ 149 ], the neural underpinnings of music-mental health associations may be highly multivariate. In the longer term, leveraging large-scale studies and large-scale data standardization and aggregation hold the promise of gleaning deeper cross-domain insights, for which current experimentalists can prepare by adopting standards for the documentation, annotation, and storage of data [ 150 ].
Biobanks and electronic health records
Finally, the use of EHR databases can be useful in quantifying associations between music engagement and mental health in large samples. EHR databases can include hundreds of thousands of records and allow for examination with International Statistical Classification of Diseases and Related Health Problems codes, including MDD, SUD, and schizophrenia diagnoses. This would allow for powerful estimates of music-mental health associations, and exploration of music engagement with other health outcomes.
The principal roadblock to this type of research is that extensive music phenotypes are not readily available in EHRs. However, there are multiple ways to bypass this limitation. First, medical records can be scraped using text-mining tools to identify cases of musician-related terms (e.g., “musician”, “guitarist”, “violinist”). For example, the phenome-wide association study described earlier [ 55 ] compared musician cases and controls identified in a large EHR database through text-mining of medical records and validated with extensive manual review charts. This study was highly powered to detect associations with internalizing and thought disorders (but showed null or protective effects for musicians for SUDs). Many EHR databases also include genomic data, allowing for integration with genetic models even in the absence of music data (e.g., exploring whether individuals with strong genetic predispositions for musical ability are at elevated or reduced risk for specific health diagnosis).
EHRs could also be used as recruitment tools, allowing researchers to collect additional data for relevant music engagement variables and compare with existing mental health diagnoses without having to conduct their own diagnostic interviews. These systems are not only relevant to individual differences research but could also be used to identify patients for possible enrollment in intervention studies. Furthermore, if recruitment for individual differences or intervention studies is done in patient waiting rooms of specific clinics, researchers can target specific populations of interest, have participants complete some relevant questionnaires while they wait, and be granted access to medical record data without having to conduct medical interviews themselves.
Concluding remarks
Music engagement, a uniquely human trait which has a powerful impact on our everyday experience, is deeply tied with our social and cultural identities as well as our personality and cognition. The relevance of music engagement to mental health, and its potential use as a therapeutic tool, has been studied for decades, but this research had not yet cohered into a clear picture. Our scoping review and framework integrated across a breadth of smaller literatures (including extant reviews and meta-analyses) relating music engagement to mental health traits and treatment effects, though it was potentially limited due to the lack of systematic literature search or formal quality appraisal of individual studies. Taken together, the current body of literature suggests that music engagement may provide an outlet for individuals who are experiencing internalizing, externalizing, or thought disorder problems, potentially supporting emotion regulation through multiple neurobiological pathways (e.g., reward center activity). Conducting more rigorous experimental intervention studies, improving reporting standards, and harnessing large-scale population-wide data in combination with new genetic analytic methods will help us achieve a better understanding of how music engagement relates to these mental health traits. We have presented a framework that illustrates why it will be vital to consider genetic and environmental risk factors when examining these associations, leading to new avenues for understanding the mechanisms by which music engagement and existing risk factors interact to support mental health and well-being.
Mankel K, Bidelman GM. Inherent auditory skills rather than formal music training shape the neural encoding of speech. Proc Natl Acad Sci. 2018;115:13129–34.
Article CAS PubMed PubMed Central Google Scholar
Swaminathan S, Schellenberg EG. Musical competence is predicted by music training, cognitive abilities, and personality. Sci Rep. 2018;8:9223.
Article PubMed PubMed Central CAS Google Scholar
Mosing MA, Pedersen NL, Madison G, Ullen F. Genetic pleiotropy explains associations between musical auditory discrimination and intelligence. PLos One. 2014;9:e113874.
Weinberg MK, Joseph D. If you’re happy and you know it: Music engagement and subjective wellbeing. Psychol Music. 2017;45:257–67.
Article Google Scholar
Theorell TP, Lennartsson AK, Mosing MA, Ullen F. Musical activity and emotional competence - a twin study. Front Psychol. 2014;5:774.
Article PubMed PubMed Central Google Scholar
Cirelli LK, Trehub SE, Trainor LJ. Rhythm and melody as social signals for infants. Ann N Y Acad Sci. 2018;1423:66–72.
Zentner M, Eerola T. Rhythmic engagement with music in infancy. Proc Natl Acad Sci. 2010;107:5768–73.
Lense MD, Beck S, Liu C, Pfeiffer R, Diaz N, Lynch M, et al. Parents, peers, and musical play: Integrated parent-child music class program supports community participation and well-being for families of children with and without Autism Spectrum Disorder. Front Psychol. 2020;11:11.
Honing H. On the biological basis of musicality. Ann N Y Acad Sci. 2018;1423:51–6.
Maratos AS, Gold C, Wang X, Crawford MJ. Music therapy for depression. Cochrane Database Syst Rev. 2008;1:CD004517.
Ansdell G, Meehan J. “Some Light at the End of the Tunnel”: exploring Users’ evidence for the effectiveness of music therapy in adult mental health settings. Music Med. 2010;2:29–40.
Khalfa S, Bella SD, Roy M, Peretz I, Lupien SJ. Effects of relaxing music on salivary cortisol level after psychological stress. Ann N Y Acad Sci. 2003;999:374–6.
Article PubMed Google Scholar
McKinney CH, Antoni MH, Kumar M, Tims FC, McCabe PM. Effects of guided imagery and music (GIM) therapy on mood and cortisol in healthy adults. Health Psychol. 1997;16:390–400.
Article CAS PubMed Google Scholar
Chanda ML, Levitin DJ. The neurochemistry of music. Trends Cogn Sci. 2013;17:179–93.
Olff M, Koch SB, Nawijn L, Frijling JL, Van Zuiden M, Veltman DJ. Social support, oxytocin, and PTSD. Eur J Psychotraumatol. 2014;5:26513.
Ferreri L, Mas-Herrero E, Zatorre RJ, Ripollés P, Gomez-Andres A, Alicart H, et al. Dopamine modulates the reward experiences elicited by music. Proc Natl Acad Sci. 2019;116:3793–8.
Evers S, Suhr B. Changes of the neurotransmitter serotonin but not of hormones during short time music perception. Eur Arch Psychiatry Clin Neurosci. 2000;250:144–7.
Blum K, Simpatico T, Febo M, Rodriquez C, Dushaj K, Li M, et al. Hypothesizing music intervention enhances brain functional connectivity involving dopaminergic recruitment: Common neuro-correlates to abusable drugs. Mol Neurobiol. 2017;54:3753–58.
Kotov R, et al. The hierarchical Taxonomy of psychopathology (HiTOP): a dimensional alternative to traditional nosologies. J Abnorm Psychol. 2017. https://doi.org/10.1037/abn0000258 .
Caspi A, Houts RM, Belsky DW, Goldman-Mellor SJ, Harrington H, Israel S, et al. The p factor: one general psychopathology factor in the structure of psychiatric disorders? Clin Psychological Sci. 2014;2:119–37.
Whiteside SP, Lynam DR. Understanding the role of impulsivity and externalizing psychopathology in alcohol abuse: Application of the UPPS impulsive behavior scale. Exp Clin Psychopharmacol. 2003;11:210–7.
Tackett JL, Lahey BB, van Hulle C, Waldman I, Krueger RF, Rathouz PJ. Common genetic influences on negative emotionality and a general psychopathology factor in childhood and adolescence. J Abnorm Psychol. 2013;122:1142–53.
Young SE, Friedman NP, Miyake A, Willcutt EG, Corley RP, Haberstick BC, et al. Behavioral disinhibition: liability for externalizing spectrum disorders and its genetic and environmental relation to response inhibition across adolescence. J Abnorm Psychol. 2009;118:117–30.
Gustavson DE, Franz CE, Panizzon MS, Lyons MJ, Kremen WS. Internalizing and externalizing psychopathology in middle age: Genetic and environmental architecture and stability of symptoms over 15 to 20 years. Psychological Med. 2019;50:1–9.
Google Scholar
Martin J, Taylor MJ, Lichtenstein P. Assessing the evidence for shared genetic risks across psychiatric disorders and traits. Psychological Med. 2018;48:1759–74.
Panteleeva Y, Ceschi G, Glowinski D, Courvoisier DS, Grandjean D. Music for anxiety? Meta-analysis of anxiety reduction in non-clinical samples. Psychol Music. 2017;46:473–87.
Leubner D, Hinterberger T. Reviewing the effectiveness of music interventions in treating depression. Front Psychol. 2017;8:1109.
Perkins R, Mason-Bertrand A, Fancourt D, Baxter L, Williamon A. How participatory music engagement supports mental well-being: a meta-ethnography. Qualitative Health Res. 2020. https://doi.org/10.1177/1049732320944142 .
Lilienfeld SO. Comorbidity between and within childhood externalizing and internalizing disorders: reflections and directions. J. Abnorm Child Psychol. 2003;31:285–91.
Kendler KS, Myers J. The boundaries of the internalizing and externalizing genetic spectra in men and women. Psychological Med. 2014;44:647–55.
Article CAS Google Scholar
Robb SL, Burns DS, Carpenter JS. Reporting guidelines for music-based interventions. J Health Psychol. 2011;16:342–52.
Robb SL, Hanson-Abromeit D, May L, Hernandez-Ruiz E, Allison M, Beloat A, et al. Reporting quality of music intervention research in healthcare: a systematic review. Complement Ther Med. 2018;38:24–41.
Carr C, Odell-Miller H, Priebe S. A systematic review of music therapy practice and outcomes with acute adult psychiatric in-patients. PLos One. 2013;8:e70252.
Miranda D, Blais-Rochette C. Neuroticism and emotion regulation through music listening: a meta-analysis. Musica Sci. 2018. https://doi.org/10.1177/1029864918806341 .
Miranda D. The emotional bond between neuroticism and music. Psychomusicology: Music, Mind, Brain. 2019. https://doi.org/10.1037/pmu0000250 .
Landis-Shack N, Heinz AJ, Bonn-Miller MO. Music therapy for posttraumatic stress in adults: a theoretical review. Psychomusicology. 2017;27:334–342.
Schäfer K, Saarikallio S, Eerola T. Music may reduce loneliness and act as social surrogate for a friend: evidence from an experimental listening study. Music Sci. 2020;3. https://doi.org/10.1177/2059204320935709 .
Braun Janzen T, Al Shirawi MI, Rotzinger S, Kennedy SH, Bartel L. A pilot study investigating the effect of music-based intervention on depression and anhedonia. Front Psychol. 2019;10:1038.
Biasutti M, Mangiacotti A. Music training improves depressed mood symptoms in elderly people: a randomized controlled trial. Int J Aging Hum Dev. 2019. https://doi.org/10.1177/0091415019893988 .
Castillo-Pérez S, Gómez-Pérez V, Velasco MC, Pérez-Campos E, Mayoral M-A. Effects of music therapy on depression compared with psychotherapy. Arts Psychother. 2010;37:387–390.
Hendricks CB, Robinson B, Bradley LJ, Davis K. Using music techniques to treat adolescent depression. J Humanist Counseling. 1999;38:39–46.
Chwalek CM, McKinney CH. The use of dialectical behavior therapy (DBT) in music therapy: a sequential explanatory study. J. Music Ther. 2015;52:282–318.
Tang YY, Yang L, Leve LD, Harold GT. Improving executive function and its neurobiological mechanisms through a mindfulness-based intervention: advances within the field of developmental neuroscience. Child Dev. Perspect. 2012;6:361–66.
PubMed PubMed Central Google Scholar
Didonna F. Mindfulness-based interventions in an inpatient setting. In: Clinical handbook of mindfulness. Springer, New York, NY; 2009. p. 447–62.
Chin T, Rickard NS. Beyond positive and negative trait affect: flourishing through music engagement. Psychol Well-Being. 2014;4:25.
Miranda D, Claes M. Personality traits, music preferences and depression in adolescence. Int J Adolescence Youth. 2008;14:277–98.
Fancourt D, Garnett C, Spiro N, West R, Mullensiefen D. How do artistic creative activities regulate our emotions? Validation of the Emotion Regulation Strategies for Artistic Creative Activities Scale (ERS-ACA). PLos One. 2019;14:e0211362.
Saarikallio S. Development and validation of the brief music in mood regulation scale (B-MMR). Music Percept. 2012;30:97–105.
Saarikallio S, Gold C, McFerran K. Development and validation of the healthy-unhealthy music scale. Child Adolesc Ment Health. 2015;20:210–17.
Groarke JM, Hogan MJ. Development and psychometric evaluation of the adaptive functions of music listening scale. Front Psychol. 2018;9:516.
Thomson CJ, Reece JE, Di Benedetto M. The relationship between music-related mood regulation and psychopathology in young people. Musica Sci. 2014;18:150–65.
Shifriss R, Bodner E, Palgi Y. When you’re down and troubled: views on the regulatory power of music. Psychol Music. 2014;43:793–807.
Garrido S, Schubert E. Moody melodies: do they cheer us up? A study of the effect of sad music on mood. Psychol Music. 2013;43:244–261.
Wesseldijk LW, Ullen F, Mosing MA. The effects of playing music on mental health outcomes. Sci Rep. 2019;9:12606.
Niarchou M, Lin G, Lense MD, Gordon RL, Davis LK. The medical signature of musicians: a phenome-wide association study using an electronic health record database. medRxiv. 2020;10:51. https://doi.org/10.1101/2020.08.14.20175109 .
Vaag J, Sund ER, Bjerkeset O. Five-factor personality profiles among Norwegian musicians compared to the general workforce. Musica Sci. 2017;22:434–445.
Fancourt D, Garnett C, Müllensiefen D. The relationship between demographics, behavioral and experiential engagement factors, and the use of artistic creative activities to regulate emotions. Psychol Aesthet Creat Arts. 2020.(advance online publication)
Mak HW, Fancourt D. Longitudinal associations between ability in arts activities, behavioural difficulties and self-esteem: Analyses from the 1970 British Cohort Study. Sci Rep. 2019;9:14236.
West SG, Taylor AB, Wu W. Model fit and model selection in structural equation modeling. In: Hoyle RH, editor. Handbook of structural equation modeling. New York, NY: The Guilford Press; 2012. p. 209–31.
Weiss B, Susser K, Catron T. Common and specific features of childhood psychopathology. J Abnorm Psychol. 1998;107:118–27.
Krueger RF, McGue M, Iacono WG. The higher-order structure of common DSM mental disorders: Internalization, externalization, and their connections to personality. Personal Individ Differences. 2001;30:1245–159.
Morse S, et al. Audio therapy significantly attenuates aberrant mood in residential patient addiction treatment: putative activation of dopaminergic pathways in the meso-limbic reward circuitry of humans. J Addict Res Ther. 2011;3:2.
Baker FA, Gleadhill LM, Dingle GA. Music therapy and emotional exploration: exposing substance abuse clients to the experiences of non-drug-induced emotions. Arts Psychother. 2007;34:321–330.
Dingle GA, Gleadhill L, Baker FA. Can music therapy engage patients in group cognitive behaviour therapy for substance abuse treatment? Drug Alcohol Rev. 2008;27:190–6.
Hohmann L, Bradt J, Stegemann T, Koelsch S. Effects of music therapy and music-based interventions in the treatment of substance use disorders: A systematic review. PLos One. 2017;12:e0187363.
Swope PM. Effects of learning the drums on inattention, vigilance, and sustained attention in adolescents with ADHD. Spalding University; 2018.
Zimmermann MB, Diers K, Strunz L, Scherbaum N, Mette C. Listening to Mozart improves current mood in adult ADHD: a randomized controlled pilot study. Front Psychol. 2019;10:1104.
Madjar N, Gazoli R, Manor I, Shoval G. Contrasting effects of music on reading comprehension in preadolescents with and without ADHD. Psychiatry Res. 2020;291:113207.
Pelham WE, Waschbusch DA, Hoza B, Gnagy EM, Greiner AR, Sams SE, et al. Music and video as distractors for boys with ADHD in the classroom: comparison with controls, individual differences, and medication effects. J Abnorm Child Psychol. 2011;39:1085–98.
Porter S, McConnell T, McLaughlin K, Lynn F, Cardwell C, Braiden HJ, et al. Music therapy for children and adolescents with behavioural and emotional problems: a randomised controlled trial. J Child Psychol Psychiatry. 2017;58:586–94.
Chong HJ, Kim SJ. Education-oriented music therapy as an after-school program for students with emotional and behavioral problems. Arts Psychother. 2010;37:190–96.
Rickson DJ, Watkins WG. Music therapy to promote prosocial behaviors in aggressive adolescent boys—a pilot study. J. Music Ther. 2003;40:283–301.
Montello L, Coons EE. Effects of active versus passive group music therapy on preadolescents with emotional, learning, and behavioral disorders. J Music Ther. 1999;35:49–67.
Mulder J, Ter Bogt TF, Raaijmakers QA, Gabhainn SN, Monshouwer K, Vollebergh WA. The soundtrack of substance use: Music preference and adolescent smoking and drinking. Subst Use Misuse. 2009;44:514–31.
Mulder J, Ter Bogt TF, Raaijmakers QA, Nic Gabhainn S, Monshouwer K, Vollebergh WA. Is it the music? Peer substance use as a mediator of the link between music preferences and adolescent substance use. J Adolescence. 2010;33:387–94.
Chen MJ, Miller BA, Grube JW, Waiters ED. Music, substance use, and aggression. J Stud Alcohol. 2006;67:373–81.
ter Bogt TF, Gabhainn SN, Simons-Morton BG, Ferreira M, Hublet A, Godeau E, et al. Dance is the new metal: adolescent music preferences and substance use across Europe. Subst Use Misuse. 2012;47:130–42.
Slater JL, Tate MC. Timing deficits in ADHD: insights from the neuroscience of musical rhythm. Front Comput Neurosci. 2018;12:51.
Carrer LR. Music and sound in time processing of children with ADHD. Front Psychiatry. 2015;6:127.
Miksza P. Relationships among impulsivity, achievement goal motivation, and the music practice of high school wind players. Bull Council Res Music Educ. 2009;180:9–27.
Miksza P. Relationships among achievement goal motivation, impulsivity, and the music practice of collegiate brass and woodwind players. Psychol Music. 2010;39:50–67.
Geretsegger M, Mössler KA, Bieleninik Ł, Chen XJ, Heldal TO, Gold C. Music therapy for people with schizophrenia and schizophrenia-like disorders. Cochrane Database Syst Rev. 2017;5:CD004025.
PubMed Google Scholar
Volpe U, Gianoglio C, Autiero L, Marino ML, Facchini D, Mucci A, et al. Acute effects of music therapy in subjects with psychosis during inpatient treatment. Psychiatry. 2018;81:218–27.
Pavlov A, Kameg K, Cline TW, Chiapetta L, Stark S, Mitchell AM. Music therapy as a nonpharmacological intervention for anxiety in patients with a thought disorder. Issues Ment Health Nurs. 2017;38:285–8.
Haugwitz, B. (2021). Music therapy in the early detection and indicated prevention in persons at risk of bipolar disorders: state of knowledge and potential. Br J Music Ther. 2021. https://doi.org/10.1177/1359457521997386 .
Power RA, Steinberg S, Bjornsdottir G, Rietveld CA, Abdellaoui A, Nivard MM, et al. Polygenic risk scores for schizophrenia and bipolar disorder predict creativity. Nat Neurosci. 2015;18:953–5.
Fancourt D, Ockelford A, Belai A. The psychoneuroimmunological effects of music: a systematic review and a new model. Brain Behav. Immun. 2014;36:15–26.
Baker FA, Metcalf O, Varker T, O’Donnell M. A systematic review of the efficacy of creative arts therapies in the treatment of adults with PTSD. Psychol Trauma. 2018;10:643–51.
Lense MD, Camarata S. PRESS-Play: musical engagement as a motivating platform for social interaction and social play in young children with ASD. Music Sci. 2020. https://doi.org/10.1177/2059204320933080 .
Walker EF, Diforio D. Schizophrenia: a neural diathesis-stress model. Psychological Rev. 1997;104:667–85.
Zuckerman M, Riskind JH. Vulnerability to psychopathology: a biosocial model. J Cogn Psychother. 2000;14:407–8.
Trucco EM, Madan B, Villar M. The impact of genes on adolescent substance use: a developmental perspective. Curr Addict Rep. 2019;6:522–531.
Butkovic A, Ullen F, Mosing MA. Personality related traits as predictors of music practice: underlying environmental and genetic influences. Personal Individ Differences. 2015;74:133–8.
Coon H, Carey G. Genetic and environmental determinants of musical ability in twins. Behav Genet. 1989;19:183–93.
Ullén F, Mosing MA, Holm L, Eriksson H, Madison G. Psychometric properties and heritability of a new online test for musicality, the Swedish Musical Discrimination Test. Personal Individ Differences. 2014;63:87–93.
Hambrick DZ, Tucker-Drob EM. The genetics of music accomplishment: evidence for gene-environment correlation and interaction. Psychonomic Bull Rev. 2015;22:112–20.
Wesseldijk LW, Mosing MA, Ullen F. Gene-environment interaction in expertise: the importance of childhood environment for musical achievement. Dev Psychol. 2019;55:1473–9.
Ullen F, Mosing MA, Madison G. Associations between motor timing, music practice, and intelligence studied in a large sample of twins. Ann N Y Acad Sci. 2015;1337:125–9.
Botvin GJ. Substance abuse prevention: theory, practice, and effectiveness. Crime Justice. 1990;13:461–519.
Fredricks JA, Simpkins S, Eccles JS. Family socialization, gender, and participation in sports and instrumental music. In: Developmental pathways through middle childhood. Mahwah, NJ: Psychology Press; 2006. p. 53–74.
Maes HH, Neale MC, Kirkpatrick RM, Kendler KS. Using multimodal inference/model averaging to model causes of covariation between variables in twins. Behav Genet. 2020. https://doi.org/10.1007/s10519-020-10026-8 .
Sala G, Gobet F. When the music’s over. Does music skill transfer to children’s and young ado escents’ cognitive and academic skills? A meta-analysis. Educ Res Rev. 2017;20:55–67.
Salimpoor VN, Zald DH, Zatorre RJ, Dagher A, McIntosh AR. Predictions and the brain: how musical sounds become rewarding. Trends Cogn Sci. 2015;19:86–91.
Loui P, Patterson S, Sachs ME, Leung Y, Zeng T, Przysinda E. White matter correlates of musical anhedonia: Implications for evolution of music. Front Psychol. 2017;8:1664.
Salimpoor VN, van den Bosch I, Kovacevic N, McIntosh AR, Dagher A, Zatorre RJ. Interactions between the nucleus accumbens and auditory cortices predict music reward value. Science. 2013;340:216–9.
Zatorre RJ, Salimpoor VN. From perception to pleasure: music and its neural substrates. Proc Natl Acad Sci. 2013;110:10430–7. Suppl 2
Alluri V, Brattico E, Toiviainen P, Burunat I, Bogert B, Numminen J, et al. Musical expertise modulates functional connectivity of limbic regions during continuous music listening. Psychomusicology. 2015;25:443–54.
Vanyukov MM, Tarter RE, Kirisci L, Kirillova GP, Maher BS, Clark DB. Liability to substance use disorders: 1. Common mechanisms and manifestations. Neurosci Biobehav Rev. 2003;27:507–515.
Volkow ND, Morales M. The brain on drugs: from reward to addiction. Cell. 2015;162:712–25.
Wise RA. Dopamine and reward: the anhedonia hypothesis 30 years on. Neurotox Res. 2008;14:169–83.
Koob GF, Volkow ND. Neurocircuitry of addiction. Neuropsychopharmacology. 2010;35:217–38.
Mukherjee S, Coque L, Cao JL, Kumar J, Chakravarty S, Asaithamby A, et al. Knockdown of Clock in the ventral tegmental area through RNA interference results in a mixed state of mania and depression-like behavior. Biol Psychiatry. 2010;68:503–11.
Kaufling J. Alterations and adaptation of ventral tegmental area dopaminergic neurons in animal models of depression. Cell Tissue Res. 2019;377:59–71.
Small KM, Nunes E, Hughley S, Addy NA. Ventral tegmental area muscarinic receptors modulate depression and anxiety-related behaviors in rats. Neurosci Lett. 2016;616:80–5.
Kokal I, Engel A, Kirschner S, Keysers C. Synchronized drumming enhances activity in the caudate and facilitates prosocial commitment-if the rhythm comes easily. PLos One. 2011;6:e27272.
Goldstein A. Thrills in response to music and other stimuli. Physiological Psychol. 1980;8:126–9.
Moore E, Schaefer RS, Bastin ME, Roberts N, Overy K. Can musical training influence brain connectivity? Evidence from diffusion tensor MRI. Brain Sci. 2014;4:405–27.
Imfeld A, Oechslin MS, Meyer M, Loenneker T, Jancke L. White matter plasticity in the corticospinal tract of musicians: a diffusion tensor imaging study. Neuroimage. 2009;46:600–7.
Han Y, Yang H, Lv YT, Zhu CZ, He Y, Tang HH, et al. Gray matter density and white matter integrity in pianists’ brain: a combined structural and diffusion tensor MRI study. Neurosci Lett. 2009;459:3–6.
Schmithorst VJ, Wilke M. Differences in white matter architecture between musicians and non-musicians: a diffusion tensor imaging study. Neurosci Lett. 2002;321:57–60.
Hudziak JJ, Albaugh MD, Ducharme S, Karama S, Spottswood M, Crehan E, et al. Cortical thickness maturation and duration of music training: Health-promoting activities shape brain development. J Am Acad Child Adolesc Psychiatry. 2014;53:1153–61.
Gingras B, Honing H, Peretz I, Trainor LJ, Fisher SE. Defining the biological bases of individual differences in musicality. Philos Trans R Soc B. 2015;370:20140092.
Heath AC, Kessler RC, Neale MC, Hewitt JK, Eaves LJ, Kendler KS. Testing hypotheses about direction of causation using cross-sectional family data. Behav Genet. 1993;23:29–50.
Coleman JRI, Peyrot WJ, Purves KL, Davis KAS, Rayner C, Choi SW, et al. Genome-wide gene-environment analyses of major depressive disorder and reported lifetime traumatic experiences in UK Biobank. Mol Psychiatry. 2020;25:247353–1446.
Domingue BW, Liu HX, Okbay A, Belsky DW. Genetic heterogeneity in depressive symptoms following the death of a spouse: polygenic score analysis of the US Health and Retirement Study. Am J Psychiatry. 2017;174:963–970.
Barcellos SH, Carvalho LS, Turley P. Education can reduce health differences related to genetic risk of obesity. Proc Natl Acad Sci USA. 2018;115:E9765–E9772.
Howard DM, Adams MJ, Shirali M, Clarke TK, Marioni RE, Davies G, et al. Genome-wide association study of depression phenotypes in UK Biobank identifies variants in excitatory synaptic pathways. Nat Commun. 2018;9:1470.
Okbay A, Baselmans BM, De Neve JE, Turley P, Nivard MG, Fontana MA, et al. Genetic variants associated with subjective well-being, depressive symptoms, and neuroticism identified through genome-wide analyses. Nat Genet. 2016;48:624–33.
Walters RK, Polimanti R, Johnson EC, McClintick JN, Adams MJ, Adkins AE, et al. Transancestral GWAS of alcohol dependence reveals common genetic underpinnings with psychiatric disorders. Nat Neurosci. 2018;21:1656–69.
Niarchou M, et al. Unraveling the genetic architecture of music rhythm. https://www.biorxiv.org/content/10.1101/836197v1 . 2019 ; 29:S62.
Purcell S. Variance components models for gene-environment interaction in twin analysis. Twin Res. 2002;5:554–71.
Barch DM, Albaugh MD, Avenevoli S, Chang L, Clark DB, Glantz MD, et al. Demographic, physical and mental health assessments in the adolescent brain and cognitive development study: rationale and description. Dev Cogn Neurosci. 2018;32:55–66.
Uban KA, Horton MK, Jacobus J, Heyser C, Thompson WK, Tapert SF, et al. Biospecimens and the ABCD study: rationale, methods of collection, measurement and early data. Dev Cogn Neurosci. 2018;32:97–106.
Mullensiefen D, Gingras B, Musil J, Stewart L. The musicality of non-musicians: an index for assessing musical sophistication in the general population. PLos One. 2014;9:e89642.
Blood AJ, Zatorre RJ. Intensely pleasurable responses to music correlate with activity in brain regions implicated in reward and emotion. Proc Natl Acad Sci. 2001;98:11818–23.
Jenkins LM, Skerrett KA, DelDonno SR, Patrón VG, Meyers KK, Peltier S, et al. Individuals with more severe depression fail to sustain nucleus accumbens activity to preferred music over time. Psychiatry Res Neuroimaging. 2018;275:21–7.
Belfi AM, Loui P. Musical anhedonia and rewards of music listening: current advances and a proposed model. Ann N Y Acad Sci. 2020;1464:99–114.
Insel T, et al. Research domain criteria (RDoC): toward a new classification framework for research on mental disorders. Am Psychiatric Assoc. 2010;167:748–51.
Loo SK, McGough JJ, McCracken JT, Smalley SL. Parsing heterogeneity in attention-deficit hyperactivity disorder using EEG-based subgroups. J Child Psychol Psychiatry. 2018;59:223–31.
Zotev V, Mayeli A, Misaki M, Bodurka J. Emotion self-regulation training in major depressive disorder using simultaneous real-time fMRI and EEG neurofeedback. Neuroimage Clin. 2020;27:102331.
Yang AC, Jann K, Michel CM, Wang DJJ. Editorial: advances in multi-scale analysis of brain complexity. Front Neurosci. 2020;14:337.
Lin C, Lee SH, Huang CM, Chen GY, Ho PS, Liu HL, et al. Increased brain entropy of resting-state fMRI mediates the relationship between depression severity and mental health-related quality of life in late-life depressed elderly. J Affect Disord. 2019;250:270–7.
Bhattacharya J, Lee EJ. Modulation of EEG theta band signal complexity by music therapy. Int J Bifurc Chaos. 2016;26:1650001.
Carpentier SM, McCulloch AR, Brown TM, Faber S, Ritter P, Wang Z, et al. Complexity matching: brain signals mirror environment information patterns during music listening and reward. J Cogn Neurosci. 2020;32:734–45.
Etkin A. A reckoning and research agenda for neuroimaging in psychiatry. Am J Psychiatry. 2019;176:507–11.
Rissling AJ, Makeig S, Braff DL, Light GA. Neurophysiologic markers of abnormal brain activity in schizophrenia. Curr Psychiatry Rep. 2010;12:572–8.
Loo SK, Makeig S. Clinical utility of EEG in attention-deficit/hyperactivity disorder: a research update. Neurotherapeutics. 2012;9:569–87.
Boyle EA, Li YI, Pritchard JK. An expanded view of complex traits: from polygenic to omnigenic. Cell. 2017;169:1177–86.
Sivagnanam S, Yoshimoto K, Carnevale T, Nadeau D, Kandes M, Petersen T, et al. Neuroscience Gateway enabling large scale modeling and data processing in neuroscience research. In: Practice and Experience in Advanced Research Computing. Association for Computing Machinery, Portland, OR, USA ; 2020. p.510–513.
Download references
Acknowledgements
This work was supported by NIH grants DP2HD098859, R01AA028411, R61MH123029, R21DC016710, U01DA04112, and R03AG065643, National Endowment for the Arts (NEA) research lab grants 1863278-38 and 1855526-38, and National Science Foundation grant 1926794. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or National Endowment for the Arts. The authors would like to thank Navya Thakkar and Gabija Zilinskaite for their assistance.
Author information
Authors and affiliations.
Department of Medicine, Vanderbilt University Medical Center, Nashville, TN, USA
- Daniel E. Gustavson
Vanderbilt Genetics Institute, Vanderbilt University Medical Center, Nashville, TN, USA
Daniel E. Gustavson, Reyna L. Gordon & Miriam D. Lense
Department of Otolaryngology – Head & Neck Surgery, Vanderbilt University Medical Center, Nashville, TN, USA
Peyton L. Coleman & Reyna L. Gordon
Swartz Center for Computational Neuroscience, Institute for Neural Computation, University of California, San Diego, La Jolla, CA, USA
John R. Iversen
Department of Human and Molecular Genetics, Virginia Institute for Psychiatric and Behavioral Genetics, Virginia Commonwealth University, Richmond, VA, USA
- Hermine H. Maes
Department of Psychiatry, Virginia Institute for Psychiatric and Behavioral Genetics, Virginia Commonwealth University, Richmond, VA, USA
Massey Cancer Center, Virginia Commonwealth University, Richmond, VA, USA
Vanderbilt Brain Institute, Vanderbilt University, Nashville, TN, USA
Reyna L. Gordon & Miriam D. Lense
The Curb Center, Vanderbilt University, Nashville, TN, USA
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Daniel E. Gustavson .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Gustavson, D.E., Coleman, P.L., Iversen, J.R. et al. Mental health and music engagement: review, framework, and guidelines for future studies. Transl Psychiatry 11 , 370 (2021). https://doi.org/10.1038/s41398-021-01483-8
Download citation
Received : 23 November 2020
Revised : 03 June 2021
Accepted : 10 June 2021
Published : 22 June 2021
DOI : https://doi.org/10.1038/s41398-021-01483-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
- Laura W. Wesseldijk
- Miriam A. Mosing
Translational Psychiatry (2023)
Effects of music-based interventions on cancer-related pain, fatigue, and distress: an overview of systematic reviews
- Ana Trigueros-Murillo
- Javier Martinez-Calderon
- Alberto Marcos Heredia-Rizo
Supportive Care in Cancer (2023)
A Systematic Review of Music-Based Interventions to Improve Treatment Engagement and Mental Health Outcomes for Adolescents and Young Adults
- Aaron H. Rodwin
- Rei Shimizu
- Michelle R. Munson
Child and Adolescent Social Work Journal (2023)
Heritability of Childhood Music Engagement and Associations with Language and Executive Function: Insights from the Adolescent Brain Cognitive Development (ABCD) Study
- Srishti Nayak
Behavior Genetics (2023)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Brain Behav Immun Health
- v.18; 2021 Dec
Music, mental health, and immunity
Music is a crucial element of everyday life and plays a central role in all human cultures: it is omnipresent and is listened to and played by persons of all ages, races, and ethnic backgrounds. But music is not simply entertainment: scientific research has shown that it can influence physiological processes that enhance physical and mental wellbeing. Consequently, it can have critical adaptive functions. Studies on patients diagnosed with mental disorders have shown a visible improvement in their mental health after interventions using music as primary tool. Other studies have demonstrated the benefits of music, including improved heart rate, motor skills, brain stimulation, and immune system enhancement. Mental and physical illnesses can be costly in terms of medications and psychological care, and music can offer a less expansive addition to an individual's treatment regimen. Interventions using music offers music-based activities in both a therapeutic environment (Music therapy) with the support of a trained professional, and non-therapeutic setting, providing an atmosphere that is positive, supportive, and proactive while learning non-invasive techniques to treat symptoms associated with various disorders – and possibly modulate the immune system.
1. Introduction
Music can play a crucial role to support people at all stages of life: from helping new-born babies develop healthy bonds with their parents to offering vital, sensitive, and compassionate palliative care at the end of life. Singing to new-borns, a widespread activity practised worldwide, has been demonstrated to have valuable benefits such as improving mother-infant interaction and reducing infant distress ( Vlismas et al., 2013 ; Mualem and Klein, 2013a ). In the same way, music has been reported as an aid in the reduction of anxiety and agitation in older adults with senile dementia ( Sung et al., 2012 ).
The clinical and evidence-informed use of music interventions to accomplish individualised goals within a therapeutic relationship is defined as Music therapy ( Press Release on Mus, 2014 ). Established as a profession after World War II, Music therapy has become an important part of internationally therapeutic and healthcare settings ( Greenberg and Rentfrow, 2017 ). Even long before that, Pythagoras (c.570 – c.495 BC), the Ancient Greek philosopher and mathematician, prescribed various musical scales and modes to cure an array of physical and psychological conditions ( Greenberg and Rentfrow, 2017 ). Music therapy is part of the Creative Arts Therapies ( Mind [Internet]. [cited 2, 2021 ), in which arts-based activities are used in a therapeutic environment, with the support of a trained professional. Creative Arts Therapies are particularly effective for people who face barriers in expressing themselves with spoken languages, such as individuals with communication deficits or people with mental health difficulties who find it difficult to talk about their experiences and feelings in words. These therapies provide a safe and supportive environment to enable and encourage the patients to express themselves in whatever way possible, encouraging self-expression and development supported by the therapeutic relationship ( Ahessy, 2013 ). Music therapy interventions involve a therapeutic process developed between the patient (or client) and therapist through the use of personally tailored music experiences ( de Witte et al., 2019 ).
This distinguishes Music therapy from other music interventions, offered mainly by medical or healthcare professionals ( de Witte et al., 2019 ; Agres et al., 2021 ). In fact, music can be utilized not only through a setting lead by a professional Music therapist, but also with individuals and groups in a variety of settings. A wide range of musical styles and instruments can be used, including the voice, enabling people to create their unique musical language to explore and connect with the world and express themselves. Bringing out emotions and thoughts through methods of verbal and nonverbal expression and exploration - such as dance and body movement, music, art ( Havsteen-Franklin ), and expressive writing ( Pennebaker and Chung, 2007 ; Rebecchini, 2019 ) - may deactivate the avoidance mechanism and enable the elaboration of emotions and distress. As Juslin and Vastfjall (2008) , and Levitin ( British Association for M, 2021 ) have underlined, music has evolved from emotional communication, and the musical components of speech provide honest communication about emotions. Because musical participation and response do not depend solely on the ability to speak, music is particularly effective for people who have difficulty communicating verbally ( British Association for M, 2021 ). Hence, working with music can be life-changing for people affected by disability, injury, or mental disorders.
The potential of music to affect mood, cognition, and behavior has been demonstrated in several studies. On a negative side, some studies have shown that men who were exposed to music with misogynistic lyrics displayed higher levels of aggressive behavior than did those who were exposed to neutral music, especially when the aggressive behavior was directed at a female target person. Men also recalled more negative attributes of women after exposure to misogynistic music ( Barongan, Hall ). And when the music contained men-hating lyrics, women recalled more negative than positive attributes about men ( Fischer and Greitemeyer, 2006 ). Furthermore, playing loud music incessantly to prisoners has been reported as a form of “music torture” designed to cause extreme discomfort. In fact, it's been a practice against which the legal charity Reprieve set up its “zero-dB” campaign ( zero, 2021 ) the 60th anniversary of the Universal Declaration of Human Rights in December 2008.
There is a vast body of evidence demonstrating that Music therapy is beneficial both physically and mentally. Recently the attention has also focused on whether general music activities, not led by therapists, can enhance the mental health and wellbeing of service users ( de Witte et al., 2019 ; Fancourt et al., 2016 ). Studies on patients diagnosed with mental disorders such as anxiety, depression, and schizophrenia have shown a visible improvement in their mental health after general music and Music therapy interventions ( Fancourt et al., 2016 ; McCaffrey et al., 2011 ; Mössler et al., 2011 ; Erkkilä et al., 2011 ). Moreover, studies have demonstrated other benefits of music and Music therapy, including improved heart rate, motor skills, stimulation of the brain ( Bradt et al., 2013 ; Magee et al., 2017 ; Norton et al., 2009 ) and enhancement of the immune system ( Taylor, 1997 ; Fancourt et al., 2014 ; Li et al., 2021 ).
Although music might have initially evolved as a pure art expression with entertainment scopes, it is now clear that music can affect physiological processes, improving physical and mental wellbeing. Consequently, it can have critical adaptive functions.
1.1. The role of music since first interactions
The use of the voice through singing is a unique form of interaction and expression. Singing is closely linked to the first forms of interaction between a mother and her infant. The body of research on parent-infant communication has shown that humans' earliest contact has many musical qualities ( Trevarthen and Malloch, 2000 ; Stern, 2010 ). As Dissanayake suggested ( Dissanayake, 2000 ), a mother's use of rhythmical movement appears to be an essential component for the expression communicated while singing with her infant.
Evidence has underlined that a mother's touch and rhythmical movements, co-created with her infant during musical interactions, are central to the infant's feelings of pleasure ( Longhi, 2008 ) and a healthy mother-infant relationship ( Hatch and Maietta, 1991 ). As a mother emotionally engages with her infant, her sensitivity and affection are communicated through her voice ( Fernald, 1989 , 1992 ; Rock et al., 1999 ), touch and facial expressions ( Papoušek and Papoušek, 1987 ; Stack and Muir, 1992 ), and rhythmical movements ( Hatch and Maietta, 1991 ). This co-created communicative interaction has been demonstrating a ‘communicative musicality’ due to its intrinsic music and dance-like qualities of the regularity of pulse and sensitive exchange of gestural narratives ( Malloch and Trevarthen, 2009 ). The positive emotional arousal and synchronisation between a mother and her child could be the root of a positive mother-infant relationship, thus essential for future child development ( Hodges, 1980 ; Mualem and Klein, 2013b ).
A study conducted by Vlismas et al. (2013) on the effect of music and movement on mother-infant interactions showed that maternal engagement in a music and movement programme resulted in changes to both mothers' and infants' behavior. Specifically, it showed that the effect of the programme increased the mothers' self-reported use of music and enjoyment of interactions with their infants; the mothers' self-reported attachment to their infants; the dyadic reciprocity between mother and infant; and the attentional and affective aspects of mothers' speech.
2. Music, music therapy and mental health
Utilising music as a structured intervention in treating mental illnesses such as anxiety, depression and schizophrenia has been reported as beneficial in relieving symptoms ( Mössler et al., 2011 ; Erkkilä et al., 2011 ), while improving mood and social interactions ( Edwards, 2006 ). Some people with mental disorders may be too disturbed to use verbal language alone efficiently as a therapeutic medium. Thus, the musical interaction might support and provide musical resources and competencies very beneficial for patient's everyday life. Music can have unique motivating, relationship-building, and emotionally expressive qualities ( Solli, 2008 ; Rolvsjord, 2001 ).
Numerous studies have focused on the effect of music interventions on individuals in clinical settings. Many of these studies concluded that music interventions positively impact mood and anxious or depressive symptoms in both children ( Kim and Stegemann, 2016 ; Yinger and Gooding, 2015 ; Kemper and Danhauer, 2005 ) and adults ( Carr et al., 2013 ; van der Wal-Huisman et al., 2018 ). Reviews of the evidence have suggested that Music therapy may improve mental health in children and adolescents and communication in children with autistic spectrum disorder ( Gold et al., 2007 ; Whipple, 2004 ). In the same way, clinical reports and pre-experimental studies have suggested that Music therapy may be an effective intervention for adult patients with mental health problems across the world. A recent review which aimed to identify, summarise, and synthesise different experimental studies addressing the effects of Music therapy alone or Music therapy added to standard care on mental health ( Lee and Thyer, 2013 ) has shown the therapy alone or added to standard care to have significantly better effects than psychotherapy ( Castillo-Pérez et al., 2010 ), verbal relaxation ( Lin et al., 2011 ), standard care ( Erkkilä et al., 2011 ; Lin et al., 2011 ; Yang et al., 2009 ) and no treatment ( Mohammadi et al., 2011 ; Siedliecki and Good, 2006 ).
Mental health diseases such as depression and anxiety can have devastating consequences both for patients and their families. Symptoms can be severe and debilitating, leaving individuals alone and isolated. Relationships among family and friends may suffer, and individuals may not receive the support needed to manage their disease. Music can improve symptoms associated with mental illness, but it can also provide an environment for social interaction. As Choi, Lee, and Lim described ( Choi et al., 2008 ), Music therapy helps the individual to express emotions while producing a state of mental relaxation, and consequently it can be beneficial in decreasing symptoms of depression and anxiety, while enhancing interpersonal relationships.
Other music interventions - not lead by a professional music therapist - such as group drumming have been very effective, leading to the enhancement of psychological states, specifically fewer depressive symptoms and greater social resilience ( Fancourt et al., 2016 ): there is a growing body of evidence demonstrating the effects of community group on mental health ( Estevao et al., 2021 ; Clift and Morrison, 2011 ; Coulton et al., 2015 ). For example, a study conducted with mothers suffering from postnatal depression found that mothers with moderate-severe depressive symptoms who participated in 10 weeks of music and singing classes with their babies had a significantly faster improvement in symptoms than mothers who participated in usual care groups ( Fancourt and Perkins, 2018 ).
In the same way, using Music therapy to decrease psychological stress during pregnancy has been reported as an appropriate alternative therapy for pregnant women suffering from mental health problems attempting to avoid the side effects associated with medication. A study conducted in 2007 with the aim of examining the effects of Music therapy on reducing psychological stress during pregnancy reported that listening to music for at least 30 minutes daily substantially reduced psychological stress, anxiety, and depression ( Chang et al., 2008 ). Hence, listening to music daily during pregnancy can generate considerable health benefits.
These experimental results indicate that music promotes psychological health both during pregnancy, and the entire lifetime; it can be easily used in many environments, and it can also be tailored to personal preferences to enhance mental health.
2.1. Music and immune system
The immune system, composed by molecular and cellular components, is a complex system of structures and processes that have evolved to protect us from disease. The function of these components is divided up into nonspecific mechanisms, those which are innate to an organism, and responsive responses, which are adaptive to specific pathogens. The innate immune system represents the first line of defense against infection and includes cells and proteins that are nonspecific to particular antigens. The adaptive immune system provides a secondary, antigen-specific response during which cells with a memory for specific pathogens are created. The adaptive immune system has the capacity to recognize and respond to virtually any protein or carbohydrate imaginable; yet, without the innate immune system to instruct it—in effect, telling it whether, when, how, and where to respond—it is powerless ( Clark and Kupper, 2005 ). As the literature shows, the immune system is strongly associated with mood, psychological condition, and hormonal balance ( Segerstrom and Miller, 2004 ). Thus, as a result of negative mood, psychological stress affects the immune system and may cause dysregulation leads to a change in the humoral and cellular immunity and increases health risks.
Psychological stress can have detrimental effects on both immune system responses, leading to a weakening of defenses against new pathogens and increasing in systemic inflammation ( Chanda and Levitin, 2013a ; Maddock and Pariante, 2001 ). While inflammation is a local, protective response to microbial invasion or injury, it must be fine-tuned and regulated precisely, because deficiencies or excesses of the inflammatory response cause morbidity and shorten lifespan ( Tracey, 2002 ; Bassi et al., 2018 ). Because stress can be a predisposing factor to diseases associated with immunologic responses ( Maddock and Pariante, 2001 ), increased exposure to stressful situations expands the risk of mental and physical disorders ( Hazelgrove et al., 2021 ). Acute stress can affect basal sensitivity, increasing or decreasing pain threshold in acute and chronic pain processes. For the fact that acute and chronic pain are potent stressors, they can alter the body homeostasis: pain can be an activator of the hypothalamic-pituitary-adrenal axis (HPA axis), the major system responsible for stress responses, which may be hypoactive or hyperactive under chronic or persistent stress conditions ( Timmers et al., 2019 ). In turn, the HPA axis modulation directly affects the release levels of glucocorticoids, ‘hormones of stress’, which induce anti-inflammatory and immunosuppressive effects at pharmacological doses, whereas at physiological levels they play an essential regulatory role in the immune system ( Pariante and Miller, 2001 ). Thus, stress can negatively affect the cardiovascular, neuroendocrine, and immune systems, which, consequently, may impair recovery, increase the risk for adverse effects, and delay hospital discharge ( Biondi and Zannino, 1997 ).
Although psychological stress cannot be eliminated, there are ways in which the perception of stress and ability to adapt to stressors can be altered: music has been adapted as a form of stress management and studies have confirmed the effect of music on the reduction of stress responses in the cardiovascular and endocrine system ( Taylor, 1997 ; Mojtabavi et al., 2020 ). Specifically, music has been shown to modify heart rate, respiration rate, perspiration, and other autonomic systems ( Blood et al., 1999 ), supporting reports that many people use music to achieve physical and psychological balance. Lifestyle choices that reduce stress are thought to be highly protective against diseases ( Dimsdale, 2008 ), and music may be among these ( Dileo et al., 2007 ; Nilsson, 2008 ).
The human's biological stress response is highly adaptive in the short term: it is an elegant choreography ( Chanda and Levitin, 2013b ) of neuroendocrine, autonomic, metabolic, and immune system activity that involves multiple feedback loops at the level of the central and peripheral nervous systems ( Landgraf and Neumann, 2004 ). Together these systems trigger short term adaptive behaviours, including arousal, vigilance, focused attention, and temporarily inhibit functions that are nonessential during a crisis, such as eating, digestion, growth, and sex drive. At the same time, cardiovascular changes such as elevated heart rate and rapid breathing are helpful to increase oxygenation and glucose supply to the brain and skeletal muscles.
However, as already mentioned, the prolonged activation of these systems has devastating consequences for health. Continuous and elevated circulating levels of glucocorticoids (e.g., cortisol) act as neurotoxins, weakening the ability of neurons and other cells to resist injury and making them more vulnerable to the effects of toxins and the normal attrition process ( Landgraf and Neumann, 2004 ). Furthermore, although glucocorticoids act as an immunosuppressant under acute stress conditions, they may promote a state of chronic low-grade inflammation in the long term ( Gouin et al., 2008 ). These neurotoxic and pro-inflammatory effects of chronic stress have been linked to a host of adverse health outcomes such as susceptibility to infectious diseases, anxiety and depression ( Pitharouli et al., 2021 ), and cardiovascular diseases ( Chrousos, 2009 ; Lupien et al., 2009 ).
As many studies have demonstrated, neuroinflammation is the cause of several mental diseases such as depression and anxiety ( Zheng et al., 2021 ; Troubat et al., 2021 ). Hence, attention has increasingly focused on the effect of music as a possible anti-inflammatory mechanism in these central inflammatory conditions. A recent work conducted by Dasy Fancourt (2014) - the first systematic review that aimed to assess published studies dealing with psychoneuroimmunological effects of music - showed that music can have effects on various neurotransmitters, cytokines, and hormones ( Fancourt et al., 2014 ). Specifically, fifty-six of the sixty-three studies included in the author's systematic review linked psychoneuroimmunological effects of music to the stress response.
Salivary Immunoglobulin A (s-IgA), a first-line in the defence against bacterial and viral infections ( Woof and Kerr, 2006 ) and a reliable marker of the functional status of the entire mucosal immune system ( Hucklebridge et al., 2000 ), has been revealed to be particularly responsive to music, increasing following exposure to a range of styles of music including both relaxing and stimulating music, as well as for both active involvements and simply listening to recorded music ( Fancourt et al., 2014 ). Strong patterns have also been noticed concerning cortisol, which repeatedly decreased in response to relaxing recorded music ( Fancourt et al., 2014 ). There also appeared to be patterns in the response of epinephrine and norepinephrine, which have been shown to decrease in response to relaxing recorded music ( Leardi et al., 2007 ).
Another study conducted to determine if (i) musical activity could produce a significant change in the immune system measured by s-IgA, and if (ii) active participation in musical activity had a different effect on the immune system than passive participation showed that S-IgA levels of the active group (playing music and singing) had more significant increase than those of the passive group (listening only) ( Kuhn, 2002 ). This result suggested that active participation in musical activity produces a more significant effect on the immune system than passive participation.
Overall, changes have been observed across various immune response biomarkers, including leukocytes, cytokines, immunoglobulins, and hormones and neurotransmitters associated with immune response ( Fancourt et al., 2014 ). Music has begun to be taken seriously in healthcare settings as research findings have started to link the beneficial effects of music on stress to a broader impact on health ( Haake, 2011 ). If music can mediate anti-inflammatory effects, evidenced by decreased levels of inflammatory biomarkers (see Table 1 ), there may be biological plausibility for its use in the care of ill patients. The results of these studies provide further confirmation that the immune system can be enhanced by music and, as Daisy Fancourt has underlined, the trend towards positive findings of the effect of music on psychoneuroimmunological response strongly supports further investigation in this field ( Fancourt et al., 2014 ).
Table 1
Markers of inflammation and immune response influenced by music .
| Type of music activities | Peripheral markers | Brain regions |
|---|---|---|
| Listening to relaxing/pleasant music ( ; ; ; ; ) | Increased levels of: - salivary Immunoglobulin A (s-IgA) Decreased levels of: - cortisol - epinephrine - norepinephrine | Activation of: - ventral striatum: nucleus accumbens (NAc) - opioid-rich midbrain nuclei - anterior superior insula - Rolandi operculum Deactivation of: - amygdala - hippocampus - parahippocampal gyrus - temporal poles |
| Listening to techno music ( ) | Increased levels of: - plasma cortisol - adrenocorticotropic hormone - prolactin - growth hormone - norepinephrine levels | – |
| Active participation in musical activity (playing, singing) ( ; ) | Increased level of: - salivary Immunoglobulin A (s-IgA) | Activation of: - ventral striatum: nucleus accumbens (NAc) |
2.1.1. Other biological effects
In the last decade, there has been growing interest in music's chemical and biological effects ( Table 1 ) ( Khan et al., 2018 ). Some studies have focused on whether music can affect the same neurochemical reward systems as other reinforcing stimuli. Does music have the earmarks of a rewarding stimulus, including the ability to motivate an individual to learn and engage in goal-directed behavior to obtain a pleasurable feeling ( Chanda and Levitin, 2013b )? As Salimpoor et al. have underlined ( Salimpoor et al., 2015 ), dopamine activity can explain why an individual would be motivated to keep listening to a piece of music, or to seek out that music in the future. However, it cannot alone explain the experience of pleasure when listening to music. Berridge and colleagues described ‘hedonic hotspots’ in the nucleus accumbens (NAc) and ventral pallidum that are explicitly linked to the display of pleasure and are triggered by opioid signalling ( Berridge and Kringelbach, 2013 ). Thus, there are crucial interactions between the dopamine and opioid systems. A rapid increase in dopamine release in humans induces euphoria, with the level of euphoria correlating with the level of ventral striatal dopamine release, which also leads to robust increases of endorphin release in the NAc ( Drevets et al., 2001 ). On the other hand, opioid antagonists block the subjective ‘high’ caused by strong dopamine release ( Jayaram-Lindström et al., 2004 ). Consequently, it seems reasonable to hypothesize that a strong induction of dopamine release caused by music can trigger opioid stimulation of so-called hedonic hotspots. In the other direction, the opioid system robustly modulates dopamine release in to the NAc ( Hjelmstad et al., 2013 ). This likely provides a mechanism through which music that is experienced as pleasing can enhance dopamine-mediated positive prediction error signaling and reinforcement learning. Thus, the association of dopamine release and NAc activation during peak musical pleasure may be a direct manifestation of this opioid–dopamine interaction ( Salimpoor et al., 2015 ).
There is an increasing body of evidence demonstrating the functional activation ( Blood and Zatorre, 2001 ; Brown et al., 2004 ; Jeffries et al., 2003 ; Koelsch et al., 2006 ), network connectivity ( Menon and Levitin, 2005 ), and central dopamine release ( Salimpoor et al., 2011 ) during the perception of pleasurable music. A review conducted by Chanda and Levitin (2013b) showed that studies that used positron emission tomography (PET) to investigate regional cerebral blood flow (rCBF) during experienced musical pleasure ( Blood and Zatorre, 2001 ; Brown et al., 2004 ; Jeffries et al., 2003 ) suggested that music reward involve the activation of the NAc, as well as opioid-rich midbrain nuclei known to regulate morphine analgesia and descending inhibition of pain ( Jeffries et al., 2003 ). NAc activation was also reported during listening to unfamiliar pleasant music compared to rest ( Brown et al., 2004 ) and during singing compared to speech ( Jeffries et al., 2003 ). On the other hand, listening to techno-music induced changes in neurotransmitters, peptides and hormonal reactions, related to mental state and emotional involvement: techno music increased plasma cortisol, adrenocorticotropic hormone, prolactin, growth hormone and norepinephrine levels ( Gerra et al., 1998 ). The neuroendocrine pattern induced by this fast music (techno music) turned out to be similar to the biological reaction to psychological stress ( Henry, 1992 ).
Other studies that used higher resolution functional magnetic resonance imaging (fMRI) to investigate the neural correlates of music pleasure ( Koelsch et al., 2006 ; Menon and Levitin, 2005 ; Salimpoor et al., 2011 ; Janata, 2009 ) showed that musical reward is dependent on dopaminergic neurotransmission within a similar neural network as other reinforcing stimuli: pleasant (consonant – positive emotional valence) and unpleasant (dissonant – negative emotional valence) music were contrasted, and the results confirmed activation of the ventral striatum and Rolandi operculum during pleasurable music listening, while strong deactivations were observed in the amygdala, hippocampus, parahippocampal gyrus, and the temporal poles in response to pleasant music ( Koelsch et al., 2006 ). Activation of the anterior superior insula in response to pleasant music has also been observed: a significant finding because of the insula's connectivity to the NAc and its role in the activation of the emotional circuitry and reward system ( Pavuluri et al., 2017 ) which, in turn, increases the innate and adaptive immune system ( Ben-Shaanan et al., 2016 ). All these structures have previously been implicated in the emotional processing of stimuli with (negative) emotional valence ( Heinzel et al., 2005 ; Siegle et al., 2002 ). The results of the studies mentioned above indicate that these structures respond to auditory information with emotional valence, and that listening to music has the capacity to up-as well as down-regulate neuronal activity in these structures.
3. Conclusion and limitations
The increasing evidence of the benefits of music activities and Music therapy provided by the literature is a driving force for developing music-based therapies services in the health care sector. By promoting physical and psychological health, music can be an effective treatment option suitable for every environment and people of every age, race, and ethnic background.
Since music is a complex topic, there are some aspects that this mini review has not fully addressed, such as the role of the autonomic nervous system involved in musical activities; the involvement of music as a possible component of an “enriched environment” ( Kempermann, 2019 ); and, finally, the beneficial effects of rhythmical movements and physical musical activities, and their contribution to the preference for treatment options.
Figure 1. Lavinia Rebecchini is an Italian psychologist currently doing a Ph.D at the Department of Psychological Medicine at the Institute of Psychiatry, Psychology and Neuroscience (IoPPN), King's College London. She graduated from Università Cattolica del Sacro Cuore of Milan and, after completing her Master of Science in Developmental Psychology with full marks, she decided to move to London to broaden her horizons. She started as an intern at the Perinatal Psychiatry section of the Stress, Psychiatry, and Immunology Laboratory (SPI Lab) at the IoPPN and, after being hired as a Research Assistant, she then decided to further cultivate her strong interest in the perinatal mental health field with a PhD. She has always been interested in perinatal psychiatry and the relationship between mothers and their children. Her Ph.D at the SPI Lab is concentrating on mother-infant interaction with mothers suffering from perinatal depression. With her Ph.D project, she focuses on which implications perinatal depression may carry for the developing mother-infant relationship. She looks at whether an intervention of music and singing sessions can help mothers develop compensatory skills to interact with their children appropriately so to better respond to their infants' needs. In addition to her academic experiences, during her free time, she has always volunteered to help children and families in need. She is determined and enthusiastic, and her eight years' experience in alpine skiing competitions has allowed her to build strong determination in achieving her goals.
Declaration of competing interest
The author Lavinia Rebecchini declares that there are no conflicts of interest.
Acknowledgements
Dr Rebecchini is supported by a kind gift from Michael Samuel through King's College London & King's Health Partners, by the UK National Institute for Health Research (NIHR) Biomedical Research Centre at the South London and Maudsley NHS Foundation Trust, and by the Wellcome Trust SHAPER programme (Scaling-up Health-Arts Programme to scale up arts intervention; award reference 219425/Z/19/Z).

Dr. Lavinia Rebecchini.
- Agres K.R., Schaefer R.S., Volk A., van Hooren S., Holzapfel A., Dalla Bella S. Meinard Mü ller 15, Martina de Witte 8. Rafael Ramirez Melendez [Internet] https://us.sagepub.com/en-us/nam/open-access-at-sage [cited 2021 Aug 23];12:1–32. Available from:
- Ahessy B. Creative Arts Therapies: what psychologists need to know. Irish Psychol. 2013; 1 :274–281. [ Google Scholar ]
- Barongan C, Hall GCN. The influence OF misogynous rap music ON sexual aggression against women. Psychol. Women Q.. 19:195–207.
- Bassi G.S., Ulloa L., Santos V.R., del Vecchio F., Delfino-Pereira P., Rodrigues G.J. Cortical stimulation in conscious rats controls joint inflammation. Prog. Neuro Psychopharmacol. Biol. Psychiatr. 2018 Jun 8; 84 :201–213. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Ben-Shaanan T.L., Azulay-Debby H., Dubovik T., Starosvetsky E., Korin B., Schiller M. Activation of the reward system boosts innate and adaptive immunity. Nat. Med. 2016 [ PubMed ] [ Google Scholar ]
- Berridge K.C., Kringelbach M.L. Neuroscience of affect: brain mechanisms of pleasure and displeasure. Curr. Opin. Neurobiol. 2013 Jun 1; 23 (3):294–303. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Biondi M., Zannino L.-G. Psychological stress, neuroimmunomodulation, and susceptibility to infectious diseases in animals and man: a review. Psychother. Psychosom. 1997; 66 (1):3–26. [ PubMed ] [ Google Scholar ]
- Blood A.J., Zatorre R.J. Intensely pleasurable responses to music correlate with activity in brain regions implicated in reward and emotion. Proc. Natl. Acad. Sci. Unit. States Am. 2001; 98 (20):11818–11823. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Blood A.J., Zatorre R.J., Bermudez P., Evans A.C. Emotional responses to pleasant and unpleasant music correlate with activity in paralimbic brain regions. Nat. Neurosci. 1999; 2 (4):382–387. [ PubMed ] [ Google Scholar ]
- Bradt J., Dileo C., Potvin N. Music for stress and anxiety reduction in coronary heart disease patients. Cochrane Database Syst. Rev. 2013; 12 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- https://www.bamt.org/music-therapy/what-is-music-therapy British Association for Music Therapy [Internet]. [cited 2021 May 13]. Available from:
- Brown S., Martinez M.J., Parsons L.M. Passive music listening spontaneously engages limbic and paralimbic systems. Neuroreport. 2004; 15 (13):2033–2037. [ PubMed ] [ Google Scholar ]
- Carr C., Odell-Miller H., Priebe S. A systematic review of music therapy practice and outcomes with acute adult psychiatric in-patients. PLoS One. 2013; 8 (8) [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Castillo-Pérez S., Gómez-Pérez V., Velasco M.C., Pérez-Campos E., Mayoral M.-A. Effects of music therapy on depression compared with psychotherapy. Arts Psychother. 2010; 37 (5):387–390. [ Google Scholar ]
- Chanda M.L., Levitin D.J. Vol. 17. Elsevier Ltd; 2013. The neurochemistry of music; pp. 179–193. (Trends in Cognitive Sciences). [ PubMed ] [ Google Scholar ]
- Chanda M.L., Levitin D.J. The neurochemistry of music. Trends Cognit. Sci. 2013; 17 (4):179–193. [ PubMed ] [ Google Scholar ]
- Chang M., Chen C., Huang K. Effects of music therapy on psychological health of women during pregnancy. J. Clin. Nurs. 2008; 17 (19):2580–2587. [ PubMed ] [ Google Scholar ]
- Choi A.-N., Lee M.S., Lim H.-J. Effects of group music intervention on depression, anxiety, and relationships in psychiatric patients: a pilot study. J. Alternative Compl. Med. 2008; 14 (5):567–570. [ PubMed ] [ Google Scholar ]
- Chrousos G.P. Stress and disorders of the stress system. Nat. Rev. Endocrinol. 2009; 5 (7):374. [ PubMed ] [ Google Scholar ]
- Clark R., Kupper T. 2005. Old Meets New: The Interaction Between Innate and Adaptive Immunity. [ PubMed ] [ Google Scholar ]
- Clift S., Morrison I. Mental Health and Social Inclusion; 2011. Group Singing Fosters Mental Health and Wellbeing: Findings from the East Kent “Singing for Health” Network Project. [ Google Scholar ]
- Coulton S., Clift S., Skingley A., Rodriguez J. Effectiveness and cost-effectiveness of community singing on mental health-related quality of life of older people: randomised controlled trial. Br. J. Psychiatr. 2015; 207 (3):250–255. [ PubMed ] [ Google Scholar ]
- de Witte M., Spruit A., van Hooren S., Moonen X., Stams G.-J. 2019. Effects of Music Interventions on Stress-Related Outcomes: a Systematic Review and Two Meta-Analyses. https://www.tandfonline.com/action/journalInformation?journalCode=rhpr20 [cited 2021 Aug 23]; Available from: [ PubMed ] [ Google Scholar ]
- Dileo C., Bradt J. In: Principles and Practice of Stress Management. Lehrer P.M., editor. Guilford Press; 2007. Music therapy: applications to stress management; pp. 519544–undefined. [ Google Scholar ]
- Dimsdale J.E. Psychological stress and cardiovascular disease. J. Am. Coll. Cardiol. 2008; 51 (13):1237–1246. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Dissanayake E. Antecedents of the temporal arts in early mother-infant interaction. The origins of music. 2000:389–410. [ Google Scholar ]
- Drevets W.C., Gautier C., Price J.C., Kupfer D.J., Kinahan P.E., Grace A.A. Amphetamine-induced dopamine release in human ventral striatum correlates with euphoria. Biol. Psychiatr. 2001 Jan 15; 49 (2):81–96. [ PubMed ] [ Google Scholar ]
- Edwards J. Music therapy in the treatment and management of mental disorders. Ir. J. Psychol. Med. 2006; 23 (1):33–35. [ PubMed ] [ Google Scholar ]
- Erkkilä J., Punkanen M., Fachner J., Ala-Ruona E., Pöntiö I., Tervaniemi M. Individual music therapy for depression: randomised controlled trial. Br. J. Psychiatry. 2011; 199 (2):132–139. [ PubMed ] [ Google Scholar ]
- Estevao C., Fancourt D., Dazzan P., Chaudhuri K.R., Sevdalis N., Woods A. Scaling-up Health-Arts Programmes: the largest study in the world bringing arts-based mental health interventions into a national health service. BJPsych Bull. 2021 Feb; 45 (1):32–39. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Fancourt D., Perkins R. Effect of singing interventions on symptoms of postnatal depression: three-arm randomised controlled trial. Br. J. Psychiatr. 2018; 212 (2):119–121. [ PubMed ] [ Google Scholar ]
- Fancourt D., Ockelford A., Belai A. Vol. 36. 2014. The psychoneuroimmunological effects of music: a systematic review and a new model; pp. 15–26. (Brain, Behavior, and Immunity). [ PubMed ] [ Google Scholar ]
- Fancourt D., Perkins R., Ascenso S., Carvalho L.A., Steptoe A., Williamon A. Effects of group drumming interventions on anxiety, depression, social resilience and inflammatory immune response among mental health service users. PLoS One. 2016 Mar 1; 11 (3) [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Fernald A. Intonation and communicative intent in mothers' speech to infants: is the melody the message? Child Dev. 1989:1497–1510. [ PubMed ] [ Google Scholar ]
- Fernald A. Nonverbal Vocal Communication: Comparative and Developmental Approaches. 1992. Meaningful melodies in mothers' speech to infants; p. 262. [ Google Scholar ]
- Fischer P., Greitemeyer T. 2006. Music and Aggression: The Impact of Sexual-Aggressive Song Lyrics on Aggression-Related Thoughts, Emotions, and Behavior Toward the Same and the Opposite Sex. [ PubMed ] [ Google Scholar ]
- Gerra G., Zaimovic A., Franchini D., Palladino M., Giucastro G., Reali N. Neuroendocrine responses of healthy volunteers to `techno-music’: relationships with personality traits and emotional state. Int. J. Psychophysiol. 1998 Jan 1; 28 (1):99–111. [ PubMed ] [ Google Scholar ]
- Gold C., Wigram T., Voracek M. Effectiveness of music therapy for children and adolescents with psychopathology: a quasi-experimental study. Psychother. Res. 2007; 17 (3):289–296. [ Google Scholar ]
- Gouin J.-P., Hantsoo L., Kiecolt-Glaser J.K. Immune dysregulation and chronic stress among older adults: a review. Neuroimmunomodulation. 2008; 15 (4–6):251–259. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Greenberg D.M., Rentfrow P.J. Music and big data: a new frontier. Current opinion in behavioral sciences. 2017; 18 :50–56. [ Google Scholar ]
- Haake A.B. Individual music listening in workplace settings: an exploratory survey of offices in the UK. Music. Sci. 2011 Mar; 15 (1):107–129. [ Google Scholar ]
- Hatch F.W., Maietta L. 1991. The Role of Kinesthesia in Pre-and Perinatal. [ Google Scholar ]
- Havsteen-Franklin D. Creative arts therapies C a T. http://ebookcentral.proquest.com/lib/kcl/detail.action?docID=5790646 [Internet]. Available from:
- Hazelgrove K., Biaggi A., Waites F., Fuste M., Osborne S., Conroy S. Risk factors for postpartum relapse in women at risk of postpartum psychosis: the role of psychosocial stress and the biological stress system. Psychoneuroendocrinology. 2021; 128 :105218. [ PubMed ] [ Google Scholar ]
- Heinzel A., Bermpohl F., Niese R., Pfennig A., Pascual-Leone A., Schlaug G. How do we modulate our emotions? Parametric fMRI reveals cortical midline structures as regions specifically involved in the processing of emotional valences. Cognit. Brain Res. 2005 Sep 1; 25 (1):348–358. [ PubMed ] [ Google Scholar ]
- Henry J.P. Biological basis of the stress response. Integr. Physiol. Behav. Sci. 1992; 27 :1. https://link.springer.com/article/10.1007/BF02691093 [Internet]. 1992 Jan [cited 2021 Aug 29];27(1):66–83. Available from: [ PubMed ] [ Google Scholar ]
- Hjelmstad G.O., Xia Y., Margolis E.B., Fields H.L. Opioid modulation of ventral pallidal afferents to ventral tegmental area neurons. Journal of Neuroscience [Internet] 2013 Apr 10 https://www.jneurosci.org/content/33/15/6454 [cited 2021 Aug 30];33(15):6454–9. Available from: [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Hodges D.A. National Association for Music Therapy; 1980. Handbook of Music Psychology. [ Google Scholar ]
- Hucklebridge F., Lambert S., Clow A., Warburton D.M., Evans P.D., Sherwood N. Modulation of secretory immunoglobulin A in saliva; response to manipulation of mood. Biol. Psychol. 2000; 53 (1):25–35. [ PubMed ] [ Google Scholar ]
- Janata P. The neural architecture of music-evoked autobiographical memories. Cerebr. Cortex. 2009; 19 (11):2579–2594. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Jayaram-Lindström N., Wennberg P., Hurd Y.L., Franck J. Effects of naltrexone on the subjective response to amphetamine in healthy volunteers. Journal of Clinical Psychopharmacology [Internet] 2004 https://journals.lww.com/psychopharmacology/Fulltext/2004/12000/Effects_of_Naltrexone_on_the_Subjective_Response.16.aspx [cited 2021 Aug 30];24(6):665–9. Dec. [ PubMed ] [ Google Scholar ]
- Jeffries K.J., Fritz J.B., Braun A.R. Words in melody: an H215O PET study of brain activation during singing and speaking. Neuroreport. 2003; 14 (5):749–754. [ PubMed ] [ Google Scholar ]
- Juslin P.N., Vastfjall D. Emotional responses to music: the need to consider underlying mechanisms. Behav. Brain Sci. 2008; 31 (5):559. [ PubMed ] [ Google Scholar ]
- Kemper K.J., Danhauer S.C. Music as therapy. South. Med. J. 2005; 98 (3):282–288. [ PubMed ] [ Google Scholar ]
- Kempermann G. Vol. 20. Nature Publishing Group; 2019. Environmental enrichment, new neurons and the neurobiology of individuality; pp. 235–245. (Nature Reviews Neuroscience). [ PubMed ] [ Google Scholar ]
- Khan S.H., Kitsis M., Golovyan D., Wang S., Chlan L.L., Boustani M. Effects of music intervention on inflammatory markers in critically ill and post-operative patients: a systematic review of the literature. Heart Lung. 2018; 47 (5):489–496. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Kim J., Stegemann T. Music listening for children and adolescents in health care contexts: a systematic review. Arts Psychother. 2016; 51 :72–85. [ Google Scholar ]
- Koelsch S., Fritz T., Cramon DY v., Müller K., Friederici A.D. Investigating emotion with music: an fMRI study. Hum. Brain Mapp. 2006; 27 (3):239–250. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Kuhn D. The effects of active and passive participation in musical activity on the immune system as measured by salivary immunoglobulin A (SlgA) J. Music Ther. 2002; 39 (1):30–39. [ PubMed ] [ Google Scholar ]
- Landgraf R., Neumann I.D. Vasopressin and oxytocin release within the brain: a dynamic concept of multiple and variable modes of neuropeptide communication. Front. Neuroendocrinol. 2004; 25 (3–4):150–176. [ PubMed ] [ Google Scholar ]
- Leardi S., Pietroletti R., Angeloni G., Necozione S., Ranalletta G., del Gusto B. Randomized clinical trial examining the effect of music therapy in stress response to day surgery. Br. J. Surg. 2007; 94 (8):943–947. [ PubMed ] [ Google Scholar ]
- Lee J., Thyer B.A. Does music therapy improve mental health in adults? A review. J. Hum. Behav. Soc. Environ. 2013; 23 (5):591–603. [ Google Scholar ]
- Levitin D.J. Penguin; 2008. The World in Six Songs: How the Musical Brain Created Human Nature. [ Google Scholar ]
- Li J., Li X., Liu H., Li J., Han Q., Wang C. Effects of music stimulus on behavior response, cortisol level, and horizontal immunity of growing pigs. Journal of Animal Science [Internet] 2021 May 1; 99 (5) doi: 10.1093/jas/skab043. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lin M., Hsieh Y., Hsu Y., Fetzer S., Hsu M. A randomised controlled trial of the effect of music therapy and verbal relaxation on chemotherapy-induced anxiety. J. Clin. Nurs. 2011; 20 (7-8):988–999. [ PubMed ] [ Google Scholar ]
- Longhi E. Emotional responses in mother-infant musical interactions: a developmental perspective. Behav. Brain Sci. 2008; 31 (5):586. [ Google Scholar ]
- Lupien S.J., McEwen B.S., Gunnar M.R., Heim C. Effects of stress throughout the lifespan on the brain, behaviour and cognition. Nat. Rev. Neurosci. 2009; 10 (6):434–445. [ PubMed ] [ Google Scholar ]
- Maddock C., Pariante C.M. How does stress affect you? An overview of stress, immunity, depression and disease. Epidemiol. Psichiatr. Soc. 2001; 10 :153–162. [ PubMed ] [ Google Scholar ]
- Magee W.L., Clark I., Tamplin J., Bradt J. Music interventions for acquired brain injury. Cochrane Database Syst. Rev. 2017; 1 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Malloch S., Trevarthen C. 2009. Communicative Musicality. Exploring the Basis of Human. [ Google Scholar ]
- McCaffrey T., Edwards J., Fannon D. Is there a role for music therapy in the recovery approach in mental health? Arts Psychother. 2011; 38 (3):185–189. [ Google Scholar ]
- Menon V., Levitin D.J. The rewards of music listening: response and physiological connectivity of the mesolimbic system. Neuroimage. 2005; 28 (1):175–184. [ PubMed ] [ Google Scholar ]
- https://www.mind.org.uk/information-support/drugs-and-treatments/arts-and-creative-therapies/about-arts-and-creative-therapies/ Mind [Internet]. [cited 2021 May 13]. Available from:
- Mohammadi A.Z., Shahabi T., Panah F.M. An evaluation of the effect of group music therapy on stress, anxiety and depression levels in nursing home residents. Can. J. Music Ther. 2011; 17 (1) [ Google Scholar ]
- Mojtabavi H., Saghazadeh A., Valenti V.E., Rezaei N. Can music influence cardiac autonomic system? A systematic review and narrative synthesis to evaluate its impact on heart rate variability. Compl. Ther. Clin. Pract. 2020 May 1; 39 :101162. [ PubMed ] [ Google Scholar ]
- Mössler K., Chen X., Heldal T.O., Gold C. Music therapy for people with schizophrenia and schizophrenia-like disorders. Cochrane Database Syst. Rev. 2011; 12 [ PubMed ] [ Google Scholar ]
- Mualem O., Klein P.S. The communicative characteristics of musical interactions compared with play interactions between mothers and their one-year-old infants. Early Child Development and Care [Internet] 2013 https://www.tandfonline.com/action/journalInformation?journalCode=gecd20 [cited 2021 May 14];183(7):899–915. Available from: [ Google Scholar ]
- Mualem O., Klein P.S. The communicative characteristics of musical interactions compared with play interactions between mothers and their one-year-old infants. Early Child. Dev. Care. 2013; 183 (7):899–915. [ Google Scholar ]
- Nilsson U. The anxiety-and pain-reducing effects of music interventions: a systematic review. AORN J. 2008; 87 (4):780–807. [ PubMed ] [ Google Scholar ]
- Norton A., Zipse L., Marchina S., Schlaug G. Melodic intonation therapy: shared insights on how it is done and why it might help. Ann. N. Y. Acad. Sci. 2009; 1169 :431. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Papoušek H., Papoušek M. 1987. Intuitive Parenting: a Dialectic Counterpart to the Infant's Integrative Competence. [ Google Scholar ]
- Pariante C.M., Miller A.H. REVIEW glucocorticoid receptors in major depression: relevance to pathophysiology and treatment. Biol. Psychiatr. 2001; 49 [ PubMed ] [ Google Scholar ]
- Pavuluri M., Volpe K., Yuen A. Vol. 4. AIMS Press; 2017. Nucleus accumbens and its role in reward and emotional circuitry: a potential hot mess in substance use and emotional disorders; pp. 52–70. (AIMS Neuroscience). [ Google Scholar ]
- Pennebaker J.W., Chung C.K. 2007. Expressive Writing, Emotional Upheavals, and Health. [ Google Scholar ]
- Pitharouli M.C., Hagenaars S.P., Glanville K.P., Coleman J.R.I., Hotopf M., Lewis C.M. Elevated C-reactive protein in patients with depression, independent of genetic, health, and psychosocial factors: results from the UK biobank. Am. J. Psychiatr. 2021 May 14 [ PubMed ] [ Google Scholar ]
- AMTA Press Release on Music Therapy - Jan 2014. https://www.musictherapy.org/amta_press_release_on_music_therapy_-_jan_2014/ General News - News | American Music Therapy Association (AMTA) [Internet]. [cited 2021 Aug 23]. Available from:
- Rebecchini L. https://www.inspirethemind.org/blog/2019/06/26/using-expressive-writing-to-cope-with-the-childbirth?rq=lavinia Using Expressive Writing to cope with childbirth [Internet]. 2019. Available from:
- Rock A.M.L., Trainor L.J., Addison T.L. Distinctive messages in infant-directed lullabies and play songs. Dev. Psychol. 1999; 35 (2):527. [ PubMed ] [ Google Scholar ]
- Rolvsjord R. Sophie Learns to Play her Songs of Tears: –A case study exploring the dialectics between didactic and psychotherapeutic music therapy practices. Nord. J. Music Ther. 2001; 10 (1):77–85. [ Google Scholar ]
- Salimpoor V.N., Benovoy M., Larcher K., Dagher A., Zatorre R.J. Anatomically distinct dopamine release during anticipation and experience of peak emotion to music. Nat. Neurosci. 2011; 14 (2):257. [ PubMed ] [ Google Scholar ]
- Salimpoor V.N., Zald D.H., Zatorre R.J., Dagher A., Mcintosh A.R. Predictions and the brain: how musical sounds become rewarding. Trends in Cognitive Sciences [Internet] 2015; 19 (2) doi: 10.1016/j.tics.2014.12.001. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Segerstrom S.C., Miller G.E. Psychological stress and the human immune system: a meta-analytic study of 30 Years of inquiry. Psychological bulletin [Internet] 2004; 130 (4):601. pmc/articles/PMC1361287/ cited 2021 Aug 29. Jul. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Siedliecki S.L., Good M. Effect of music on power, pain, depression and disability. J. Adv. Nurs. 2006; 54 (5):553–562. [ PubMed ] [ Google Scholar ]
- Siegle G.J., Steinhauer S.R., Thase M.E., Stenger V.A., Carter C.S. Can't shake that feeling: event-related fMRI assessment of sustained amygdala activity in response to emotional information in depressed individuals. Biol. Psychiatr. 2002 May 1; 51 (9):693–707. [ PubMed ] [ Google Scholar ]
- Solli H.P. “Shut up and play!” Improvisational use of popular music for a man with schizophrenia. Nord. J. Music Ther. 2008; 17 (1):67–77. [ Google Scholar ]
- Stack D.M., Muir D.W. Adult tactile stimulation during face-to-face interactions modulates five-month-olds’ affect and attention. Child Dev. 1992; 63 (6):1509–1525. [ PubMed ] [ Google Scholar ]
- Stern D.N. Oxford University Press; 2010. Forms of Vitality: Exploring Dynamic Experience in Psychology, the Arts, Psychotherapy, and Development. [ Google Scholar ]
- Sung H., Lee W., Li T., Watson R. A group music intervention using percussion instruments with familiar music to reduce anxiety and agitation of institutionalized older adults with dementia. Int. J. Geriatr. Psychiatr. 2012; 27 (6):621–627. [ PubMed ] [ Google Scholar ]
- Taylor D.B. MMB Music. Inc; Saint Louis: 1997. Biomedical Foundations of Music as Therapy. [ Google Scholar ]
- Timmers I., Quaedflieg C.W.E.M., Hsu C., Heathcote L.C., Rovnaghi C.R., Simons L.E. Vol. 107. Elsevier Ltd; 2019. The interaction between stress and chronic pain through the lens of threat learning; pp. 641–655. (Neuroscience and Biobehavioral Reviews). [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Tracey K.J. The inflammatory reflex. Nature. 2002; 420 :6917. https://www.nature.com/articles/nature01321 [Internet]. 2002 Dec 26 [cited 2021 Aug 23];420(6917):853–9. Available from: [ PubMed ] [ Google Scholar ]
- Trevarthen C., Malloch S.N. The dance of wellbeing: defining the musical therapeutic effect. Nordisk tidsskrift for musikkterapi. 2000; 9 (2):3–17. [ Google Scholar ]
- Troubat R., Barone P., Leman S., Desmidt T., Cressant A., Atanasova B. Neuroinflammation and depression: a review. Eur. J. Neurosci. 2021 Jan 1; 53 (1):151–171. [ PubMed ] [ Google Scholar ]
- van der Wal-Huisman H., Dons K.S.K., Smilde R., Heineman E., van Leeuwen B.L. The effect of music on postoperative recovery in older patients: a systematic review. Journal of geriatric oncology. 2018; 9 (6):550–559. [ PubMed ] [ Google Scholar ]
- Vlismas W., Malloch S., Burnham D. The effects of music and movement on mother–infant interactions. Early Child. Dev. Care. 2013; 183 (11):1669–1688. [ Google Scholar ]
- Whipple J. Music in intervention for children and adolescents with autism: a meta-analysis. J. Music Ther. 2004; 41 (2):90–106. [ PubMed ] [ Google Scholar ]
- Woof J.M., Kerr M.A. The function of immunoglobulin A in immunity. J. Pathol.: A Journal of the Pathological Society of Great Britain and Ireland. 2006; 208 (2):270–282. [ PubMed ] [ Google Scholar ]
- Yang M., Li L., Zhu H., Alexander I.M., Liu S., Zhou W. Music therapy to relieve anxiety in pregnant women on bedrest: a randomized, controlled trial. MCN Am. J. Matern./Child Nurs. 2009; 34 (5):316–323. [ PubMed ] [ Google Scholar ]
- Yinger O.S., Gooding L.F. A systematic review of music-based interventions for procedural support. J. Music Ther. 2015; 52 (1):1–77. [ PubMed ] [ Google Scholar ]
- zero dB. Pav [Internet] https://pavt.co.uk/zero-dB [cited 2021 Aug 30]. Available from:
- Zheng Z.H., Tu J.L., Li X.H., Hua Q., Liu W.Z., Liu Y. Neuroinflammation induces anxiety- and depressive-like behavior by modulating neuronal plasticity in the basolateral amygdala. Brain Behav. Immun. 2021 Jan 1; 91 :505–518. [ PubMed ] [ Google Scholar ]
Home — Essay Samples — Nursing & Health — Music Therapy — Connection between Music and Mental Health

Connection Between Music and Mental Health
- Categories: Music Therapy
About this sample

Words: 581 |
Published: Sep 1, 2023
Words: 581 | Page: 1 | 3 min read

Cite this Essay
Let us write you an essay from scratch
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Get high-quality help

Dr. Karlyna PhD
Verified writer
- Expert in: Nursing & Health

+ 120 experts online
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
Related Essays
3 pages / 1578 words
7 pages / 2977 words
5 pages / 2723 words
2 pages / 729 words
Remember! This is just a sample.
You can get your custom paper by one of our expert writers.
121 writers online
Still can’t find what you need?
Browse our vast selection of original essay samples, each expertly formatted and styled
Related Essays on Music Therapy
Music therapy is a powerful and effective form of treatment that harnesses the healing power of music. It has a rich history, with roots in ancient civilizations, and has evolved into a recognized profession in the 20th century. [...]
Music has long been recognized as a universal language that transcends boundaries and connects people across cultures. Beyond its entertainment value, music holds the remarkable ability to influence our emotions and well-being. [...]
The influence of music on mental health is a subject that has garnered increasing attention in recent years. Music, a universal language that transcends cultural boundaries, has the power to evoke emotions, alter moods, and [...]
Music has been an integral part of human culture for millennia, serving various functions from entertainment to ritualistic purposes. However, beyond its recreational and cultural significance, music holds a therapeutic [...]
Nowadays, current society is familiar with music more than in any other time in history because of the youth. A big percentage of the young listen to music everyday while performing their daily activities for many of the [...]
The healing influence of music was talked about and proved from long ago. Nowadays, the research done in the field of music therapy show the benefits obtained with the help of the new measuring instruments or new discoveries in [...]
Related Topics
By clicking “Send”, you agree to our Terms of service and Privacy statement . We will occasionally send you account related emails.
Where do you want us to send this sample?
By clicking “Continue”, you agree to our terms of service and privacy policy.
Be careful. This essay is not unique
This essay was donated by a student and is likely to have been used and submitted before
Download this Sample
Free samples may contain mistakes and not unique parts
Sorry, we could not paraphrase this essay. Our professional writers can rewrite it and get you a unique paper.
Please check your inbox.
We can write you a custom essay that will follow your exact instructions and meet the deadlines. Let's fix your grades together!
Get Your Personalized Essay in 3 Hours or Less!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free
Popular Searches
- Back to school
- Why do I feel weird
- School programs
- Managing stress
- When you’re worried about a friend who doesn’t want help
How Music Can Improve Your Mental Health
Music can be distracting and lower your stress, music can help you feel your feelings, music can make it easier to talk about what’s bothering you, music can help you figure out who you are, music builds community, music can be a quick mood booster, music can benefit people who are deaf or have hearing loss, how to use music to feel better, find more ways to support your mental health.
Share this resource

By Alexandra Frost
Since her grandfather died five years ago, Casey Clark doesn’t go a day without listening to music. It helps her cope with the grief , depression , and symptoms of post-traumatic stress disorder (PTSD) from seeing him in the hospital before he passed. When her symptoms flare, she listens to a Michael Bublé album because it was the last present she gave her grandfather, and they shared many happy memories listening to it together.
“It sounds cliché, but music actually serves as an escape in those moments when the flashbacks are so intense, and I can’t get out of them with other grounding techniques,” says Clark, 22, a writer who lives in New York City.
The teen and young adult years have long been known as the most pivotal in developing a personal taste in music, and for many, it’s the time that music matters the most. The average teen spends 2.5 hours per day listening to music, and over half of young adults , ages 18 to 29, report streaming music every day (compared to 24% of all adults).
This is good news, because music can be a great way to take care of your mental health .
Research suggests that listening to music may lessen the impact of depression and anxiety . A 2019 study found that college students who listened to classical music every day for two months had significantly lower levels of anxiety.
Another 2016 study looked at the connection between music and anxiety by studying people who have a fear of heights. Participants were put in a virtual reality simulation of riding up nine floors in an elevator. One group listened to music during the experiment, and the other didn’t. The researchers found that those who listened to music recovered faster from the stress of the experience than those who didn’t. And many studies suggest that listening to music can lower stress hormones as well as blood pressure and heart rate (both spike when you’re stressed).
When you want music to give you a break from what you’re going through, pick songs that have a storyline different from the challenges you’re facing, recommends Bethany Cook , PsyD, a psychologist and music therapist in Chicago. This can temporarily transport you elsewhere and give you a short break from your concerns, just like when you read a good book.
When her clients are in a bad mood, feeling weird or off , or managing difficult emotions, Cook recommends putting on a piece of classical music. “Listening to music that does not have lyrics attached to it lets the listener project their personal feelings and their personal struggle into the music,” she says. And some research has found that even listening to “sad” music can make you feel some pleasant emotions, which might lessen the pain you are feeling or allow you to more safely feel sad feelings we sometimes try to avoid in life.
If you don’t have the words to explain what you’re going through, or if you don’t feel comfortable talking about it, song lyrics provide another way to express yourself. Lyrics give you permission to better understand your own situation through someone else’s perspective, Cook says. She uses something called “lyric analysis” when she works with kids and teens in group therapy settings. You can try it alone or with a friend or loved one. Here’s how:
- Bring up the lyrics on your phone(s)
- Listen to the song
- Mark or highlight words and sentences that stand out to you
- Listen to the song again, pausing at the marked places, and discuss or think about why those lyrics spoke to you and how you relate to them
- Listen a final time reflecting on your new appreciation of what the song means to you or your friends
Discovering music that resonates is one key way teens and young adults define who they are and who they want to be , says Michael Viega , PhD, a professor of music therapy at Montclair State University in Montclair, New Jersey. Both Viega and Cook strongly encourage parents, teachers, and caregivers to approach teens’ and young adults’ music with curiosity.
Showing interest in musical taste is a way to show an interest in who a young person is or is becoming. Even listening to music with questionable lyrics is an “opportunity,” says Viega. It gives caregivers a chance to open a dialogue, asking teens what they think is happening in the song. Doing so can lead to meaningful conversations about important topics that can be difficult to talk about, says Viega.
“Music first turned me on to drag culture and the queer community when I was a teenager,” says Viega. “It turned me on to feminist ideals, to ecology and ecological thinking.”
Making music — through singing or playing an instrument in school, in a band, or with friends — can connect you with a community of people who share a common interest. And even if you don’t play or sing, you can also find people who share your love for a particular band or type of music. Feeling a sense of belonging to something larger than yourself is a proven way to improve mental health.
Research has found that listening to upbeat music with the intention of getting in a better mood actually works. You might not even need the research to believe this, as you might already experience this yourself.
Research into music therapy for people who are deaf and also have mental health disorders is more limited, but case studies suggest, just as in hearing people, music can help people with hearing loss express emotions and improve cognitive abilities. Cook uses table drums to connect with her deaf cousin. “Table drums are massive, and you can lie underneath them and all of that sound vibration goes straight into your body,” Cook says. Playing them with her cousin has increased their connection and nonverbal communication.
If you would like to explore using music to help you feel better, Cook and Viega recommend:
- Sampling different types of music to expand your horizons and find what you like
- Using music as a stress reliever when you are feeling anxious
- Discussing meaningful song lyrics with a friend
- Trying an instrument
- Talking about why you love a particular song with the adults in your life (or, if you’re a caregiver, with your teen)
- Listening to classical music when you have confusing or difficult emotions
- Creating playlists to match or inspire different moods
How to Take Care of Yourself By Connecting With Others
How to Use Activism as Self-Care
4 Steps to Adding Joy to Your Life
How to Cope When You’re Feeling Hopeless About the World
8 Ways to Take Care of Yourself When You’re Waiting for Mental Health Care
How to Relieve Stress: Breathing Exercises You Can Do Anywhere
How to Tell Your Parents or Caregivers You’re Struggling
Related resources
Creating a plan to take care of your mental health, how to take care of yourself when you’re taking care of friends, tips for dealing with hopelessness, search resource center.
If you or someone you know needs to talk to someone right now, text, call, or chat 988 for a free confidential conversation with a trained counselor 24/7.
You can also contact the Crisis Text Line by texting HOME to 741-741.
If this is a medical emergency or if there is immediate danger of harm, call 911 and explain that you need support for a mental health crisis.
- Bipolar Disorder
- Therapy Center
- When To See a Therapist
- Types of Therapy
- Best Online Therapy
- Best Couples Therapy
- Managing Stress
- Sleep and Dreaming
- Understanding Emotions
- Self-Improvement
- Healthy Relationships
- Student Resources
- Personality Types
- Sweepstakes
- Guided Meditations
- Verywell Mind Insights
- 2024 Verywell Mind 25
- Mental Health in the Classroom
- Editorial Process
- Meet Our Review Board
- Crisis Support
Music May Be Just as Powerful as Exercise in Improving Mental Health
Maskot / Getty Images
Key Takeaways
- Music interventions were associated with significant improvements in mental health, and included listening to music, music therapy, singing, gospel music, etc.
- The positive effects associated with music interventions may be just as powerful as those associated with a commitment to exercise or weight loss.
- For individuals who may have limited capacity for physical activity to boost mental health functioning, music may provide a welcome alternative.
Many report mental health benefits from music . A new study published in JAMA Network Open found that the positive effects of enjoying music are comparable to the impacts of exercise in terms of mental health.
Based on a systematic review and meta-analysis of 26 studies, with 779 individuals total, researchers found that music interventions were associated with significant mental health improvement.
Given how challenging it can feel to get active when navigating mental illness, music interventions may serve as another viable option.
Understanding the Research
Researchers analyzed a total of 26 studies of music interventions, and found clear and quantitative moderate evidence that these were associated with clinically significant improvements in mental health.
Of the 26 reviewed, researchers found that 8 studies demonstrated that adding music interventions to usual treatment was associated with clinically significant mental health changes in various conditions.
Music interventions such as listening to music, singing, music therapy, etc. were comparable to the benefits of non-pharmaceutical interventions and linked to smaller changes in quality of life regarding physical health.
Researchers found that a broad range of music interventions were linked to meaningful improvements in wellbeing, and may not bring the same challenges with uptake and adherence as exercise, weight loss, etc.
Music Interventions May Benefit Many
Anna Boyd, LPC , a licensed professional counselor with Mindpath Health , says, "The impact of music on our human experience is undeniable."
Boyd explains, "The research on alternative and complementary approaches to traditional psychotherapy and western, pharmaceutical interventions is an ever-growing field of research that seeks to support treating the individual from many different spectrums."
When it comes to how and why these methods are effective, Boyd notes that the research is still evolving, but this study compares the positive outcomes of music interventions to that of increasing physical activity and exercise.
Boyd underscores, "This study does a thorough job of collecting evidence from a myriad of spectrums of music therapy interventions rather than one succinct approach to the assertion that music therapy holds power to increase the positive outcomes of mental health treatment."
Anna Boyd, LPC
Like exercise, music elicits responses from the brain activity to respond to the vibrations that are associated with the act of listening and receiving.
The researchers concluded that there are many overlapping benefits between the music and exercise interventions, according to Boyd. "It is widely accepted that exercise boosts the impacts of self esteem and the increase of positive hormonal activity within the brain and body," she says.
By integrating music from the lens of drama therapy, Boyd highlights, "Like exercise, music elicits responses from the brain activity to respond to the vibrations that are associated with the act of listening and receiving."
Boyd explains, "In drama therapy, we utilize the notion of 'aesthetic distance,' which essentially speaks to the ability to explore our own stories through the safety of someone else's. This creates a space for the client to relate and express their experiences, while also promoting the safety of not having to share their own story so openly and directly."
Music is a powerful mechanism, according to Boyd. "This study supports the notion of promoting more music therapy referrals as a complementary tool to promote and foster personal growth and wellbeing," she says.
Music Can Enhance Other Activities
Abby Klemm, MT-BC , a board certified music therapist, says, "These general findings show that finding ways to include music in your daily life can benefit your physical and mental quality of life."
Klemm explains, "Consider how you can incorporate your preferred music into your daily routines – can you listen to a playlist of favorite songs on your commute to get in a positive mindset before work?"
Alternatively, Klemm asks if music can help to decompress on your way home. "Would your favorite 'pump-up jams' give you more motivation in your workout? If you enjoy live music, can you block time out regularly to see a local band perform?" she inquires.
Music is not a prescriptive intervention, as Klemm notes there is not one most effective approach. "Music not only affects our brain and body as a whole but is so personal to us that its effects can vary from person to person and from setting to setting," she says.
Klemm explains, "In music therapy research, the largest consistency seems to be that an individual’s preferred music produces the strongest effects. Music affects many parts of the brain at once. One area of the brain it affects is our reward center."
Abby Klemm, MT-BC
I’ve supported clients in actively creating music, as a way to express feelings that they don’t have words for.
Similar to other pleasurable activities, Klemm highlights how engaging in music can release neurotransmitters in the brain that increase motivation, improve mood, and decrease stress levels.
Klemm notes, "This research supports anecdotal evidence that music is good for us – it clearly affects our physical, emotional, and mental well-being. Keeping this general finding balanced with the understanding of the nuanced effects of music that vary by individual will help people find the most effective ways to use music."
The ways in which music has benefited Klemm's clients vary. "I have worked with patients who used their love of singing to improve their language and communication," she says.
Klemm explains, "I’ve supported clients in actively creating music, as a way to express feelings that they don’t have words for. Other clients have listened to specific music to affect their mood – lower stress, improve self-esteem, distract from destructive urges, instill feelings of hope, etc."
Music Therapy Can Offer Self-Expression
Christina Myers, MMT, MT-BC , a board certified music therapist with Four Diamonds at Penn State Health Children's Hospital, says, "For readers who are just learning about this, it’s helpful to know that your body and mind can respond in a similar way to music as it does exercise."
Myers explains, "Whether on a run or at a workout class, you can energize the body by increasing your heart rate. With music, you can increase your beats per minute and other characteristics in the music, so that your body releases pleasure system hormones like dopamine and serotonin."
While the music that inspires a reaction is dependent upon the listener, Myers notes that there are a variety of music qualities that may allow for similar responses in the body as exercise. "Some of these might include upbeat tempos, increased beats per minute and music that holds a variety of movement or emotional meaning to the listener," she says.
Myers highlights, "For those who are interested in intentionally using music to improve your health-related quality of life it is important to find what you jive with, and be purposeful about using it."
If you are struggling to figure out what this might look like for you, Myers recommends starting with your overall awareness of the music that creates the most motivation for you and recognize how your body responds.
Christina Myers, MMT, MT-BC
For those new to music therapy, interventions can represent a variety of methods that a music therapist might use to reach their therapeutic goals, which might include physical, emotional or spiritual goals to support a client’s needs.
Myers encourages questions like, "What music is resonating with you?" and "How does that music impact your body, as well as your emotional state?" Once the style of music that provides a connection is identified, Myers notes there can be more awareness of how the body and mind are reacting.
If music is of interest, Myers recommends connecting with a local board certified music therapist for support to explore ways to actively engage in the music process for self-expression and find an outlet.
As a music therapist who regularly combines songwriting, live music improvisation and active listening into her work with patients, Myers was surprised that songwriting was not included in this research.
Myers explains, "Throughout this research, positive impacts were measured by the number of interventions that were explored. For those new to music therapy, interventions can represent a variety of methods that a music therapist might use to reach their therapeutic goals, which might include physical, emotional or spiritual goals to support a client’s needs."
Powerful Untapped Resource in Music
Grace Meadows, FRSA , a qualified music therapist who has worked for the British Association for Music Therapy, and campaign director for Music for Dementia, says, "There is a clinically significant change in health-related quality of life when people are engaged with a music intervention."
Meadows explains, "Music can significantly improve our quality of life and there is more each of us can be doing now with music, be that helping to raise awareness and understanding of the benefits of music amongst family and friends, using music as part of every day routines, to support health and wellbeing for yourself and others."
Music may be a powerful untapped resource, which Meadows notes should be used more. "That might be using music as a motivator to move and exercise to, to lift mood and spirit, to connect with others through musical experiences to reduce social isolation and loneliness, or work with a music therapist to address psychological issues," she says.
Meadows explains, "A simple way of thinking about how you can use music is to think about your day – when are the moments you might be feeling more stressed than others, is getting up in the mornings a challenge, do you find switching off at night difficult, do you find it hard to want to exercise or get moving, do you dislike doing the daily tasks?"
Grace Meadows, FRSA
A series of responses are triggered when we engage with music, whether we’re listening to it or playing a musical instrument.
In this way, Meadows recommends thinking about what music can offer. "Do you need it to soothe and relax you or motivate and inspire you? Do you need something that’s going to provide a distraction while you get on with everyday tasks or do you need something that will allow you to wind down after a long day and help reduce your cortisol levels?" she asks.
Once an understanding of what music offers is confirmed, Meadows notes choices can be made. "It could be something more rhythmic, upbeat and lively if you need motivation to get moving or something slower in tempo, possibly instrumental to help you relax both mind and body," she says.
Meadows explains, "The style or genre of music you listen to will be down to personal preference. You could listen to upbeat, rhythmical classical music to get you motivated but it might not resonate with you in the same way your favorite disco track does. Choose the music you want."
When we listen to music, Meadows notes that the whole brain can be activated. "A series of responses are triggered when we engage with music, whether we’re listening to it or playing a musical instrument," she says.
What This Means For You
As the research demonstrates, the mental health benefits of music may compare to exercise activities. Given how physical and mental health challenges may make uptake and adherence of exercise challenging, music may offer a worthwhile alternative or complementary option.
McCrary JM, Altenmüller E, Kretschmer C, Scholz DS. Association of music interventions with health-related quality of life . JAMA Netw Open . 2022;5(3):e223236. doi:10.1001/jamanetworkopen.2022.3236
By Krystal Jagoo Krystal Kavita Jagoo is a social worker, committed to anti-oppressive practice.
Embrace your Joyful Aging Journey with Wish of a Lifetime from AARP.
AARP daily Crossword Puzzle
Hotels with AARP discounts
Life Insurance
AARP Dental Insurance Plans
LIMITED TIME OFFER: Labor Day Sale!
Join AARP for just $9 per year with a 5-year membership and get a FREE Gift!
Get instant access to members-only products, hundreds of discounts, a free second membership, and a subscription to AARP the Magazine.
- right_container
Work & Jobs
Social Security
- AARP en Español
- Membership & Benefits
- Members Edition
AARP Rewards
- AARP Rewards %{points}%
Conditions & Treatments
Drugs & Supplements
Health Care & Coverage
Health Benefits

AARP Hearing Center
Advice on Tinnitus and Hearing Loss

Get Happier
Creating Social Connections

Brain Health Resources
Tools and Explainers on Brain Health

Your Health
8 Major Health Risks for People 50+
Scams & Fraud
Personal Finance
Money Benefits

View and Report Scams in Your Area

AARP Foundation Tax-Aide
Free Tax Preparation Assistance

AARP Money Map
Get Your Finances Back on Track

How to Protect What You Collect
Small Business
Age Discrimination

Flexible Work
Freelance Jobs You Can Do From Home

AARP Skills Builder
Online Courses to Boost Your Career

31 Great Ways to Boost Your Career

ON-DEMAND WEBINARS
Tips to Enhance Your Job Search

Get More out of Your Benefits

When to Start Taking Social Security

10 Top Social Security FAQs

Social Security Benefits Calculator

Medicare Made Easy
Original vs. Medicare Advantage

Enrollment Guide
Step-by-Step Tool for First-Timers

Prescription Drugs
9 Biggest Changes Under New Rx Law

Medicare FAQs
Quick Answers to Your Top Questions
Care at Home
Financial & Legal
Life Balance

LONG-TERM CARE
Understanding Basics of LTC Insurance

State Guides
Assistance and Services in Your Area

Prepare to Care Guides
How to Develop a Caregiving Plan

End of Life
How to Cope With Grief, Loss
Recently Played
Word & Trivia
Atari® & Retro
Members Only
Staying Sharp
Mobile Apps
More About Games

Right Again! Trivia

Right Again! Trivia – Sports

Atari® Video Games

Throwback Thursday Crossword
Travel Tips
Vacation Ideas
Destinations
Travel Benefits

Beach Vacation Ideas
Fun Beach Vacations

Road Trips For Every Personality

Passport Access
Passports Can Be Renewed Online

AARP National Park Guide
Black Canyon of the Gunnison
Entertainment & Style
Family & Relationships
Personal Tech
Home & Living
Celebrities
Beauty & Style

Movies for Grownups
Summer Movie Preview

Jon Bon Jovi’s Long Journey Back
Looking Back
50 World Changers Turning 50

Sex & Dating
7 Dating Dos and 7 Don'ts

Friends & Family
Veterinarians May Use AI to Treat Pets

Home Technology
Caregiver’s Guide to Smart Home Tech

Virtual Community Center
Join Free Tech Help Events

Creative Ways to Store Your Pets Gear

Meals to Make in the Microwave

Wearing Shoes Inside: Pros vs. Cons
Driver Safety
Maintenance & Safety
Trends & Technology

AARP Smart Guide
How to Clean Your Car

We Need To Talk
Assess Your Loved One's Driving Skills

AARP Smart Driver Course

Building Resilience in Difficult Times

Tips for Finding Your Calm

Weight Loss After 50 Challenge

Cautionary Tales of Today's Biggest Scams

7 Top Podcasts for Armchair Travelers

Jean Chatzky: ‘Closing the Savings Gap’

Quick Digest of Today's Top News

AARP Top Tips for Navigating Life

Get Moving With Our Workout Series
You are now leaving AARP.org and going to a website that is not operated by AARP. A different privacy policy and terms of service will apply.
Music Can Be a Great Mood Booster
7 tips for using the power of music to help you feel happier.
Sarah Elizabeth Adler,

Your favorite album doesn’t just sound good — it may also be good for your mental health.
That’s according to a report from the Global Council on Brain Health (GCBH), an AARP-founded working group of scientists, health care professionals and other experts. Their report, “Music on Our Minds,” highlights research showing music’s positive effect on emotional well-being, including improving mood, decreasing anxiety and managing stress.

Join AARP for just $9 per year with a 5-year membership and get a FREE Gift!
“There are so many mechanisms which explain the powerful impact that listening to a piece of music can have,” says report contributor Suzanne Hanser, president of the International Association for Music & Medicine (IAMM) and a professor of music therapy at Berklee College of Music.
As the report details, that impact starts in the brain where music activates many regions, including those associated with emotion and memory . “The music that was played at your wedding or in a religious service, or even at a concert you attended or a dance you were at — that music remains preserved for those neuropathways, which connect that music with really positive feelings,” Hanser says.
Research shows that music can have a beneficial effect on brain chemicals such as dopamine, which is linked to feelings of pleasure, and oxytocin, the so-called “love hormone.” And there is evidence that music can help lower levels of the stress hormone cortisol.
How music can keep your brain healthy
The report also includes findings from the 2020 AARP Music and Brain Health Survey, a nationally representative survey of 3,185 adults, which found that listening to music — whether in the background, by focused listening to recordings or at musical performances — had a small positive impact on mental well-being, depression and anxiety.
“In times when people feel sad, stressed, anxious or lonely, listening to or making music can often help people boost their mental well-being,” says GCBH Executive Director Sarah Lenz Lock, AARP’s senior vice president for policy.
To boost music’s mental-health benefits in your life, Hanser says anyone can adapt some of the techniques used by trained music therapists. One of them is what she calls “deep” or active listening — instead of putting on music as background noise, set aside time to concentrate on what you hear, taking note of the feelings, memories and bodily sensations (whether that’s a slowing of your heart rate or the urge to get up and dance) that arise as you listen.
“We can do that even when we’re feeling at our most isolated and sad,” she says. “We can take control, we can be empowered by the music to feel differently.”

AARP NEWSLETTERS

%{ newsLetterPromoText }%
%{ description }%
Privacy Policy
ARTICLE CONTINUES AFTER ADVERTISEMENT
How to use music to provide a mental boost
1. Explore technology that can enable you to listen to music across multiple devices, such as your phone or television. Try music apps, such as Spotify or Pandora, which will suggest new music you might enjoy based on algorithms identifying music similar to your current selections.
AARP® Dental Insurance Plan administered by Delta Dental Insurance Company
Dental insurance plans for members and their families
2. Enjoy listening to familiar music that comforts you and evokes positive memories and associations.
3. If you are unhappy, try listening to or making music to improve your mood or relieve feelings of depression.
4. Dance , sing or move to music. These activities not only provide physical exercise but can also relieve stress and build social connections — and they’re fun ways to stimulate your brain.
5. While listening to music that you know and like tends to cause the strongest brain response and dopamine release, try listening to new music. Unfamiliar melodies may stimulate your brain, while providing a new source of pleasure as you get used to hearing them.
6. Make music yourself! Music making includes singing and playing an instrument . Learning to play a musical instrument can offer a sense of mastery and self-esteem, while enhancing brain activity. Singing may be the simplest way to get started.
7. Listen to fun music when you exercise. Music can help motivate you to move. “And it can hasten clearance of lactic acid buildup during recovery from vigorous exercise, according to the GCBH report.
Editor’s note: This story, originally published June 30, 2020, was updated to reflect new information.
Sarah Elizabeth Adler joined aarp.org as a writer in 2018. Her pieces on science, art and culture have appeared in The Atlantic , where she was previously an editorial fellow, California magazine and elsewhere.
Unlock Access to AARP Members Edition
Already a Member? Login

More From AARP

The Extraordinary World of Music and the Mind
It can remind you of the best days of your life. It can comfort you. It can even make those who remember little sing again.

Music and Dance Help People with Parkinson's
People with Parkinson's harness the power of music to connect, move with others

Music Therapy Boosts Stroke Recovery Rates
Health experts explore how a song could become the prescription of the future
Recommended for You
AARP Value & Member Benefits

Learn, earn and redeem points for rewards with our free loyalty program

The National Hearing Test
Members can take a free hearing test by phone

AARP® Staying Sharp®
Activities, recipes, challenges and more with full access to AARP Staying Sharp®
SAVE MONEY WITH THESE LIMITED-TIME OFFERS

Music Seems to Help the Pain… to Cultivate the Brain
The many health benefits of music therapy..
Posted August 13, 2024 | Reviewed by Abigail Fagan
- What Is Therapy?
- Take our Do I Need Therapy?
- Find counselling near me
This post is a review of I Heard There Was A Secret Chord: Music As Medicine. By Daniel J. Levitin. W.W. Norton & Co. 405 pp. $32.50.
In 1993, Nature magazine reported on a study suggesting that listening to Mozart was associated with an improvement in spatial reasoning tasks. A media frenzy ensued, followed by sales of Baby Einstein CDs and a proposal by the governor of Georgia to use public funds to supply parents of newborns with Mozart tapes. Listening to Mozart, it turned out, does not make people smarter.

Nonetheless, Daniel Levitin (an emeritus professor of neuroscience , psychology and music at McGill University and author, among other books, of This Is Your Brain On Music ) agrees with Pink Floyd: “Music seems to help the pain… to cultivate the brain.”
I Heard There Was A Secret Chord examines the many and varied neurological benefits of listening to and performing music. Along the way, Levitin, who also plays the saxophone, guitar, and bass, is a vocalist, composer, producer and recording consultant, tells memorable stories about Ella Fitzgerald, Tony Bennett, Glen Campbell, Bruce Springsteen, Bobby McFerrin, Joni Mitchell, Keith Jarrett, Linda Ronstadt and other popular music icons. In an analysis of compositions by Beethoven and the Beatles, he also speculates about how and why music resonates with virtually all of us.
That said, Levitin focuses primarily on music’s impact on the treatment of depression , pain, cognitive impairments and injuries. Because they combine motor, auditory, and semantic functions (structures that hold everything together), Levitin indicates, musical memories can connect “different modes of awareness with our internal narrative, our sense of self, where we’ve been, and, most important, where we want to go.” Uniquely robust, with any of their many attributes – pitch, melody, harmony, note duration, meter, rhythm, tempo, loudness and timbre able to trigger pattern-making circuits of the brain – musical memories can boost immune function and survive even in individuals with Alzheimer’s disease.
Stutterers, Levitin reports, achieve more fluency while singing songs with a steady beat than they do during normal conversations. Rhythmic auditory stimulation (RAS) helps Multiple Sclerosis and Parkinson’s patients increase their walking stability and balance and reduce falls and episodes in which they freeze. Music stimulates neuroplasticity, enhances brain recovery, and normalizes stress responses for many people with traumatic injuries. Based in Anchorage, Alaska, the Creative Forces Music Therapy program provides and encourages individuals with concussions and PTSD to express emotions and forge social connections. Listening to music reduces post-operative pain and the amount of anesthesia required during recovery, even for spinal surgery. And the pain doesn’t always return when the music stops. Older adults who take piano lessons improve their fine motor control more than a group of music listeners; both groups improve their mental processing speed.
More generally, as world-class musician Carlos Reyes declared, “You can talk about endorphins, serotonin, immune system signaling, and all that stuff, but that’s the bottom line – good music can make you feel better.”
Music therapy is relatively new, however, and Levitin acknowledges that positive results are often based on anecdotes, case studies, and animal models. A review of 18 studies of the impact of music on mood, motivation and the duration and intensity of hallucinations on schizophrenics, for example, concluded the evidence was of “moderate to low quality” and recommended further research using more rigorous experimental methodologies. All but 2 of 1,200 studies of music therapy and eating disorders are case studies, lack a control group or other essential design features. And two-thirds of the 114 peer-reviewed articles published between January 2000 and June 2018 on connections between music training and non-musical ability, brain structure or brain function, “incorrectly inferred causation from correlational designs.”
That is not to say, Levitin hastens to add, that music therapy is not effective. Indeed, I Heard There Was A Secret Chord provides ample evidence to justify Levitan’s claim that “music offers a dynamic interplay of sound, structure, and meaning,” continually prompts our brains to adjust and reinterpret and stimulates “neuroplasticity, growth of whole new brain pathways and healing or rerouting of damaged ones.”
And so, Levitin provides a 21st-century perspective on the hyperbolic claim made more than 200 years ago by the poet Georg Philipp Friedrich Freiherr von Hardenberg (Novalis): “Every illness is a musical problem – its cure a musical solution.”

Glenn C. Altschuler, Ph.D. , is the Thomas and Dorothy Litwin Professor of American Studies at Cornell University.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Online Therapy
- International
- New Zealand
- South Africa
- Switzerland
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Self Tests NEW
- Therapy Center
- Diagnosis Dictionary
- Types of Therapy

Sticking up for yourself is no easy task. But there are concrete skills you can use to hone your assertiveness and advocate for yourself.
- Emotional Intelligence
- Gaslighting
- Affective Forecasting
- Neuroscience

Kids’ mental health is in crisis. Here’s what psychologists are doing to help
Research is focused on child and teen mental health, exploring why they are struggling and what can be done to help them
Vol. 54 No. 1 Print version: page 63
- Mental Health
[ This article is part of the 2023 Trends Report ]
The Covid -19 pandemic era ushered in a new set of challenges for youth in the United States, leading to a mental health crisis as declared by the United States surgeon general just over a year ago. But U.S. children and teens have been suffering for far longer.
In the 10 years leading up to the pandemic, feelings of persistent sadness and hopelessness—as well as suicidal thoughts and behaviors—increased by about 40% among young people, according to the Centers for Disease Control and Prevention’s (CDC) Youth Risk Behavior Surveillance System .
“We’re seeing really high rates of suicide and depression, and this has been going on for a while,” said psychologist Kimberly Hoagwood, PhD, a professor of child and adolescent psychiatry at New York University’s Grossman School of Medicine. “It certainly got worse during the pandemic.”
In addition to the social isolation and academic disruption nearly all children and teens faced, many also lost caregivers to Covid -19, had a parent lose their job, or were victims of physical or emotional abuse at home.
All these difficulties, on top of growing concerns about social media, mass violence, natural disasters, climate change, and political polarization—not to mention the normal ups and downs of childhood and adolescence—can feel insurmountable for those who work with kids.
“The idea of a ‘mental health crisis’ is really broad. For providers and parents, the term can be anxiety-provoking,” said Melissa Brymer, PhD, who directs terrorism and disaster programs at the UCLA–Duke University National Center for Child Traumatic Stress. “Part of our role is to highlight specific areas that are critical in this discussion.”
Across the field, psychologists are doing just that. In addition to studying the biological, social, and structural contributors to the current situation, they are developing and disseminating solutions to families, in schools, and at the state level. They’re exploring ways to improve clinical training and capacity and working to restructure policies to support the most vulnerable children and teens.
Psychologists were also behind new mental health recommendations from the U.S. Preventive Services Task Force, a group of volunteer health professionals who evaluate evidence on various preventive health services. The task force now recommends regular anxiety screenings for youth ages 8 to 18 and regular depression screenings for adolescents ages 12 to 18.
“I see these trends in children’s mental health problems as being critical, but there are solutions,” Hoagwood said. “If we refocus our efforts toward those solutions, we could see some of these tides turn.”
Sources of stress
Across the United States, more than 200,000 children lost a parent or primary caregiver to Covid -19 (“ Covid -19 Orphanhood,” Imperial College London, 2022). In the face of those losses, families had to curtail mourning rituals and goodbye traditions because of social distancing requirements and other public health measures, Brymer said. Many children are still grieving, sometimes while facing added challenges such as moving to a different home or transferring to a new school with unfamiliar peers.
The CDC also reports that during the pandemic, 29% of U.S. high school students had a parent or caregiver who lost their job, 55% were emotionally abused by a parent or caregiver, and 11% were physically abused ( Adolescent Behaviors and Experiences Survey—United States, January–June 2021 , CDC ).
“Schools are crucial for keeping kids safe and connecting them with services, but the pandemic completely disrupted those kinds of supports,” Brymer said.
Those extreme disruptions didn’t affect all young people equally. Echoing pre- Covid -19 trends, the CDC also found that girls, LGBTQ+ youth, and those who have experienced racism were more likely to have poor mental health during the pandemic, said social psychologist Kathleen Ethier, PhD, director of the CDC’s Division of Adolescent and School Health.
Contributing factors likely include stigma, discrimination, and online bullying, Ethier said. Female students also report much higher levels of sexual violence than their male peers, which can further harm mental health.
As much hardship as Covid -19 wrought, it’s far from the only factor contributing to the current crisis. Biology also appears to play a role. The age of puberty has been dropping for decades, especially in girls, likely leading to difficulty processing complex feelings and knowing what to do about them ( Eckert-Lind, C., et al., JAMA Pediatrics , Vol. 174, No. 4, 2020 ). In early puberty, regions of the brain linked to emotions and social behavior are developing more quickly than regions responsible for the cognitive control of behavior, such as the prefrontal cortex, Ethier said.
Those developmental changes drive young people to seek attention and approval from their peers . For some, using social media fulfills that need in a healthy way, providing opportunities for connection and validation to youth who may be isolated from peers, geographically or otherwise.
For others, negative messages—including online bullying and unrealistic standards around physical appearance—appear to have a detrimental effect, but more research is needed to understand who is most at risk.
“There is clearly some aspect of young people’s online life that’s contributing [to the mental health crisis], we just don’t know exactly what that is,” said Ethier.
Finally, structural factors that affect millions of U.S. children, including poverty, food insecurity, homelessness, and lack of access to health care and educational opportunities, can lead to stress-response patterns that are known to underlie mental health challenges.
“Even in very young children, prolonged stress can trigger a cycle of emotion-regulation problems, which can in turn lead to anxiety, depression, and behavioral difficulties,” Hoagwood said. “These things are well established, but we’re not doing enough as a field to address them.”
Building capacity in schools
The biggest challenge facing mental health care providers right now, experts say, is a shortage of providers trained to meet the mounting needs of children and adolescents.
“There’s a growing recognition that mental health is just as important as physical health in young people’s development, but that’s happening just as mental health services are under extreme strain,” said clinical psychologist Robin Gurwitch, PhD, a professor in the Department of Psychiatry and Behavioral Sciences at Duke University Medical Center.
Schools, for example, are a key way to reach and help children—but a 2022 Pew Research Center survey found that only about half of U.S. public schools offer mental health assessments and even fewer offer treatment services. Psychologists are now ramping up efforts to better equip schools to support student well-being onsite.
Much of that work involves changing policies at the school or district level to provide more support for all students. For example, school connectedness—the degree to which young people feel that adults and peers at school care about them and are invested in their success—is a key contributor to mental health. Youth who felt connected during middle and high school have fewer problems with substance use, mental health, suicidality, and risky sexual behavior as adults ( Steiner, R. J., et al., Pediatrics , Vol. 144, No. 1, 2019 ).
Through its What Works in Schools program , the CDC funds school districts to make changes that research shows foster school connectedness. Those include improving classroom management, implementing service-learning programs for students in their communities, bringing mentors from the community into schools, and making schools safer and more supportive for LGBTQ+ students.
Psychologists are also building training programs to help teachers and other school staff create supportive classrooms and aid students who are in distress. Classroom Wise (Well-Being Information and Strategies for Educators), developed by the Mental Health Technology Transfer Center Network and the University of Maryland’s National Center for School Mental Health (NCSMH), is a free, flexible online course and resource library that draws on psychological research on social-emotional learning, behavioral regulation, mental health literacy, trauma, and more ( Evidence-Based Components of Classroom Wise (PDF, 205KB), NCSMH, 2021 ).
“We’re using evidence-based practices from child and adolescent mental health but making these strategies readily available for teachers to apply in the classroom,” said clinical psychologist Nancy Lever, PhD, codirector of NCSMH, who helped develop Classroom Wise .
The course incorporates the voices of students and educators and teaches actionable strategies such as how to create rules and routines that make classrooms feel safe and how to model emotional self-regulation. The strategies can be used by anyone who interacts with students, from teachers and administrators to school nurses, coaches, and bus drivers.
“What we need is to build capacity through all of the systems that are part of children’s lives—in families, in schools, in the education of everybody who interacts with children,” said psychologist Ann Masten, PhD, a professor of child development at the University of Minnesota.
Other training efforts focus on the students themselves. Given that preteens and teenagers tend to seek support from their peers before turning to adults, the National Child Traumatic Stress Network (NCTSN) created conversation cards to equip kids with basic skills for talking about suicide. The advice, available in English and Spanish, includes how to ask about suicidal thoughts, how to listen without judgment, and when to seek guidance from an adult ( Talking About Suicide With Friends and Peers, NCTSN, 2021 ).
While training people across the school population to spot and address mental health concerns can help reduce the strain on mental health professionals, there will always be a subset of students who need more specialized support.
Telehealth, nearly ubiquitous these days, is one of the best ways to do that. In South Carolina, psychologist Regan Stewart, PhD, and her colleagues colaunched the Telehealth Outreach Program at the Medical University of South Carolina in 2015. Today, nearly every school in the state has telehealth equipment (Wi-Fi and tablets or laptops that kids can use at school or take home) and access to providers (psychology and social work graduate students and clinicians trained in trauma-focused cognitive behavioral therapy). Students who need services, which are free thanks to grant funding or covered by Medicaid, meet one-on-one with their clinician during the school day or after hours ( American Psychologist , Vol. 75, No. 8, 2020 ).
“We learned a lot about the use of technology during the pandemic,” Ethier said. “At this point, it’s very much a matter of having sufficient resources so more school districts can access those sources of care.”
Expanding the workforce
Limited resources are leaving families low on options, with some young people making multiple trips to the emergency room for mental health-related concerns or spending more than six months on a waiting list for mental health support. That points to a need for more trained emergency responders and psychiatric beds, psychologists say, but also for better upstream screening and prevention to reduce the need for intensive care.
“Just as we need more capacity for psychiatric emergencies in kids, we also need an infusion of knowledge and ordinary strategies to support mental health on the positive side,” Masten said.
In New York, Hoagwood helped launch the state-funded Evidence Based Treatment Dissemination Center in 2006, which offers free training on evidence-based practices for trauma, behavioral and attention problems, anxiety, depression, and more to all mental health professionals who work with children in state-licensed programs, which include foster care, juvenile justice, and school settings, among others. The center provides training on a core set of tools known as PracticeWise ( Chorpita, B. F., & Daleiden E. L., Journal of Consulting and Clinical Psychology , Vol. 77, No. 3, 2009 ). It also offers tailored training based on requests from community agency leaders and clinicians who provide services to children and their families.
Hoagwood, in collaboration with a consortium of family advocates, state officials, and researchers, also helped build and test a state-approved training model and credentialing program for family and youth peer advocates. The peer advocate programs help expand the mental health workforce while giving families access to peers who have similar lived experience ( Psychiatric Services , Vol. 71, No. 5, 2020).
Youth peer advocates are young adults who have personal experience with systems such as foster care, juvenile justice, or state psychiatric care. They work within care teams to provide basic education and emotional support to other youth, such as giving advice on what questions to ask a new mental health practitioner and explaining the differences between psychologists, psychiatrists, and social workers. Youth peer advocates in New York can now receive college credit for their training in peer specialist work.
“Making community health work into a viable career can also increase diversity among mental health workers and help us address structural racism,” Hoagwood said.
Pediatricians are another group that can provide a first line of defense, drawing on their relationships with parents to destigmatize mental health care.
“Pediatricians are in many ways uniquely positioned to help address the mental health crisis in youth,” said Janine A. Rethy, MD, MPH, division chief of community pediatrics at MedStar Georgetown University Hospital and an associate professor of pediatrics at Georgetown University School of Medicine. “We have the privilege of building long-term relationships with children and their families over many years,” with at least 12 well-child checkups in just the first three years of a child’s life, followed by annual visits.
During these visits, they can watch for warning signs of social and behavioral problems and screen for maternal depression and other issues in parents, which is now recommended by the American Academy of Pediatrics (PDF, 660KB) . Several new resources provide guidance for integrating mental health care into pediatric practices, including the Behavioral Health Integration Compendium (PDF, 4.1MB) and the Healthy Steps program . But most pediatricians need more education on mental health issues in order to effectively respond, Rethy said—yet another area where psychologists may be able to help. Psychologists can provide direct consultations and training to pediatricians through the Pediatric Mental Health Care Access program.
“The more we can weave mental health knowledge, capacity, and checkpoints into places where parents feel comfortable—like the doctor’s office and at school—the better,” Masten said. “All professionals who work with young people really need the knowledge that’s being generated by psychologists.”
11 emerging trends for 2023

Scientists reach a wider audience

Psychologists take aim at misinformation

Psychological research becomes more inclusive

EDI roles expand

Worker well-being is in demand

Efforts to improve childrens’ mental health increase

Partnerships accelerate progress

Suicide prevention gets a new lifeline

Some faculty exit academia

Venture capitalists shift focus

Psychologists rebrand the field
Further reading
Science shows how to protect kids’ mental health, but it’s being ignored Prinstein, M., & Ethier, K. A., Scientific American , 2022
How pediatricians can help mitigate the mental health crisis Rethy, J. A., & Chawla, E. M., Contemporary Pediatrics , 2022
Review: Structural racism, children’s mental health service systems, and recommendations for policy and practice change Alvarez, K., et al., Journal of the American Academy of Child and Adolescent Psychiatry , 2022
Six Things Psychologists are Talking About
The APA Monitor on Psychology ® sister e-newsletter offers fresh articles on psychology trends, new research, and more.
Welcome! Thank you for subscribing.
Speaking of Psychology
Subscribe to APA’s audio podcast series highlighting some of the most important and relevant psychological research being conducted today.
Subscribe to Speaking of Psychology and download via:

Contact APA
Related topics.
- Mental health
You may also like
15 Things You Can Do With ChatGPT

Your changes have been saved
Email is sent
Email has already been sent
Please verify your email address.
You’ve reached your account maximum for followed topics.
Quick Links
What is chatgpt.
- Quickly Write a Customized Resume and Cover Letter
- Create Original Jokes and Memes
- Explain Complex Topics
- Solve Tricky Math Problems Step-by-Step
- Write Music In Almost Any Genre
- Write, Debug, and Explain Code
- Create, Edit, and Modify Media Files
- Decide What to Watch Next
- Get Cooking Help
- Improve Your Health
- Translate and Learn In Multiple Languages
- Prepare for a Job Interview
- Write Essays on Almost Any Topic
- A Chat Companion
Key Takeaways
- ChatGPT is a versatile tool that can help with tasks like writing customized resumes & cover letters.
- The AI can generate original jokes and memes, as well as explain complex topics in an easy-to-understand manner.
- ChatGPT can assist with mathematics, music composition, coding, media file manipulation, and health improvement.
Artificial intelligence tools have seen a meteoric rise within the last few years. We've been wowed by AI writing tools, AI image generators, and even AI self-portraits. Since its launch in November 2022, ChatGPT has gotten a lot of attention for its numerous uses. To help you leverage this tool, here are 15 ways you can also use ChatGPT.
If you've somehow missed the whole ChatGPT buzz, or you're not exactly sure what it's all about, let's help you get up to speed. ChatGPT is a conversational artificial intelligence chatbot that can answer just about any question you throw at it.
You can think of it as a supercharged Google Search. Rather than just providing links or snippets, ChatGPT generates thoughtful, conversational responses to queries. It synthesizes information from diverse sources into cohesive answers on nearly any topic, similar to how a knowledgeable human would respond.
While not infallible, ChatGPT demonstrates an impressive ability to understand natural language questions and offers nuanced explanations in a lot of fields.
ChatGPT is more than just hype—it has practical uses. Here are some cool day-to-day uses for ChatGPT you can try right now.
1. Quickly Write a Customized Resume and Cover Letter
If you're currently job-hunting, one of the most tiring parts of the job application process is writing a personalized resume and cover letter for every job you apply for. You need custom-made copies for each job to increase your chances of getting hired. ChatGPT can help you create a customized resume or craft professional cover letters in minutes.
We asked ChatGPT to write a resume for a content marketing role at a fictional SaaS company, and it was near perfect.
We also prompted it to prepare a cover letter for the same role, and the first result wasn't bad.
Notice how detail-rich and well-formatted the resume and cover letter are? How did I do it? I pasted my LinkedIn profile details, and then asked ChatGPT to write a resume for the target role "using LaTex." I copied the result, pasted it in a free latex editor like Overleaf , and compiled it.
2. Create Original Jokes and Memes
What's life without a bit of fun? Whether you're looking for a good laugh or to create some hilarious jokes to impress your friends, ChatGPT can come in handy. Sure, AI chatbots aren't exactly known to be great comedians, but ChatGPT shows some potential. We asked ChatGPT to tell us a joke about Apple and foldable smartphones; we'll let you judge the results:
ChatGPT can also create images, so you can also play around with meme ideas. Here's one to try: Ask ChatGPT to create a meme about the grind of 9-to-5 jobs.
3. Explain Complex Topics
Sometimes, simply Googling a topic doesn't give you a clear understanding. Think of topics like wormholes, dark matter, and all those head-spinning theories. Or maybe it's a weird sport you don't understand.
ChatGPT could be useful in explaining them in layperson terms. We prompted ChatGPT to "Explain wormholes like I'm 5," and here's the result:
We also prompted it to explain the internet similarly. It wasn't too bad, either.
4. Solve Tricky Math Problems Step-by-Step
Whether you're looking to tackle complex algebra problems or simple math problems that are too tricky to piece together, ChatGPT is particularly strong at handling math. You'll need to present your problems clearly and concisely for the best results. We prompted ChatGPT to answer a tricky math problem, and here's the result:
5. Write Music In Almost Any Genre
One of the most exciting things you can do with ChatGPT is writing a song. It might sound like a bad idea at first, but it's really a fun thing to try. The results can be amazing when you get the prompts right. The key to getting the best result is to provide as many details as possible about how you want the song to be. Need a mix of English and some Spanish with a touch of Afrobeat style? Just say it.
If you really want to find out how good your lyrics would sound in an actual song, you'll need to head over to a tool like Suno.ai to turn the lyrics into music. Just paste the lyrics into the tool, make some tweaks and listen to what ChatGPT could make.
6. Write, Debug, and Explain Code
Whether you're an experienced programmer or a newbie, you're bound to run into a few bugs in your code from time to time. ChatGPT can help you narrow down the problem within your code, saving you hours looking for a misplaced comma. You can also write entire blocks of functional code snippets from scratch or analyze existing code bases to figure out the best ways to use them. There are endless ways you can use ChatGPT in programming .
We prompted ChatGPT to write a simple to-do list app using HTML, CSS, and JavaScript, and here's the result:
We also got the AI chatbot to write us a simple Tetris game, snake game, pong game, and even code a complete chat web app from scratch . ChatGPT is a very useful programming tool.
7. Create, Edit, and Modify Media Files
With ChatGPT, you can create, edit, modify, and read from a wide range of media files. The feature which is available on the ChatGPT Plus plan provides an interface to programmatically create images, modify videos, adjust audio tracks, and retrieve crucial metadata from media files with ease and precision.
To learn more about manipulating media files with ChatGPT, read our guide on how to use the ChatGPT Code Interpreter feature .
8. Decide What to Watch Next
ChatGPT is one of the most powerful movie recommendation tools on the internet if you know how to use it. While there are dozens of powerful movie recommendation tools you can get your hands on, ChatGPT stands out because of the accuracy and precision you get from simply describing the kind of movies you want using simple natural language prompts.
We asked ChatGPT to give us some movies that are similar to "The Walking Dead" and here's the result:
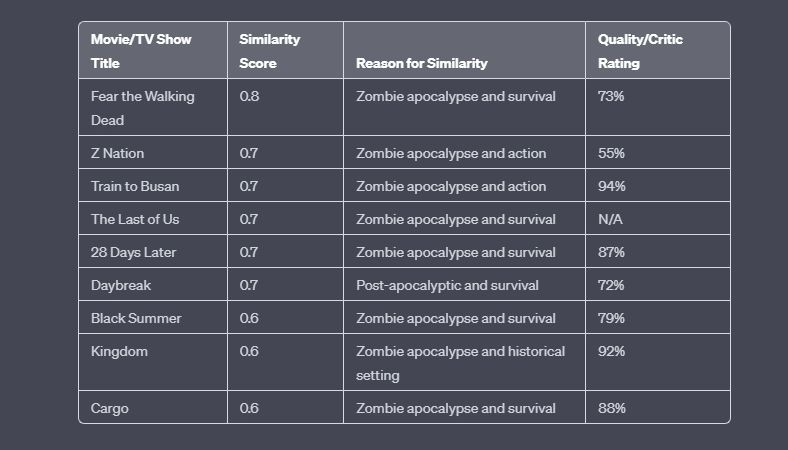
Not sure how to use ChatGPT as a movie recommendation tool? We've previously put together a detailed guide on how to use ChatGPT to decide what to watch next .
9. Play Games
Looking for a fun activity? ChatGPT has some creative game ideas to try with friends or by yourself. You could play classic games like tic-tac-toe or trivia with new twists that ChatGPT can suggest to make it more engaging. Whether you want a competitive game against ChatGPT or a cooperative game you can all play together, ChatGPT can provide unique game suggestions tailored to what you're looking for.
So if you're bored and want to try something new, ask ChatGPT to invent a fun, customized game—it's a great way to liven up your day! Not sure which games you can play with ChatGPT? Here are some interesting games you can play with ChatGPT right now .
10. Get Cooking Help
A robot help in the kitchen? ChatGPT and cooking seem like a weird combination, but it works excellently if you know the right prompts to use. You can use ChatGPT to explore new recipes, prepare shopping lists, brainstorm new flavor combinations, learn new cooking tips, or explore healthier ways to cook popular meals .
Fancy testing ChatGPT's culinary skills? Here are some interesting ways you can use ChatGPT as a cooking assistant .
11. Improve Your Health
With its vast wealth of health information, you can leverage ChatGPT to improve your health in several ways. It can help you create personalized workout and meal plans tailored to your unique needs.
You can also use it to develop healthy habits like sleep routines and mindfulness practices or even use it as a medical symptom checker. Although ChatGPT has its limitations in the field of health, it is still an immensely useful tool you can utilize to improve your health. We've put together a guide on how to use ChatGPT to improve your health .
12. Translate and Learn In Multiple Languages
ChatGPT is a great tool to have around if you need to work in multiple languages. It is fluent in dozens of languages. If you're a content creator who would love to reach a wider audience, ChatGPT could be incredibly useful for creating content in multiple languages.
Sure, there's Google Translate, but writing in one language and translating to the other means context and language-specific tones could be lost. When we compared ChatGPT to Google Translate in translation tasks, ChatGPT was noticeably better in several metrics.
With ChatGPT's latest voice mode, the tool has become even significantly more powerful for those trying to learn a new language or communicate with someone that speaks a different one.
13. Prepare for a Job Interview
With its wealth of knowledge across several fields, ChatGPT is one of the best AI tools to help you prepare for a job interview. With a few intelligent prompts, ChatGPT can help you get your dream job . You can use it to generate hypothetical scenarios in a job interview, possible questions, intelligent replies to possible questions, and many other useful interview prep tips.
We created a hypothetical situation during an interview and asked ChatGPT for help. Here's the result:
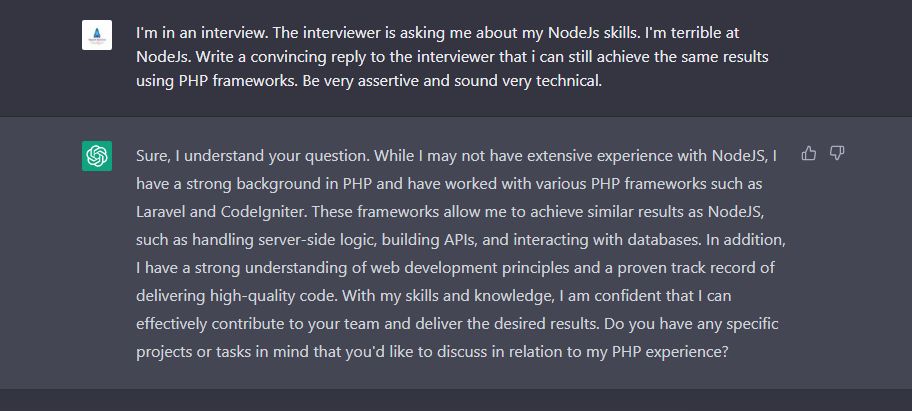
14. Write Essays on Almost Any Topic
While we strongly advise you to write your essays yourself, ChatGPT can compose amazing essays on a wide range of topics, even the most complex. If the tone of the resulting write-up doesn't suit your test, you can teach ChatGPT how to write like you so you can get the chatbot to replicate your writing style.
15. A Chat Companion
When all is said and done, ChatGPT is an AI chatbot. Despite its almost endless use cases, ChatGPT is a very accommodating companion when you need someone (or a robot) to talk to.
Despite ChatGPT's impressive capabilities, the AI chatbot is not infallible. Consequently, exercising caution with ChatGPT's information is highly advised. Always strive to verify any critical data from ChatGPT before applying it, especially for important health or financial choices. While ChatGPT is a game-changing tool, it is still a work in progress, and human oversight remains essential.
- Technology Explained
- Share full article
For more audio journalism and storytelling, download New York Times Audio , a new iOS app available for news subscribers.
How Air-Conditioning Conquered America
Indoor cooling has transformed american life, reshaping homes, skylines and where people choose to live. as the planet warms, is that sustainable.
This transcript was created using speech recognition software. While it has been reviewed by human transcribers, it may contain errors. Please review the episode audio before quoting from this transcript and email [email protected] with any questions.
From “The New York Times,” I’m Michael Barbaro. This is “The Daily.”
[MUSIC PLAYING]
Today, the story of how air conditioning has become both our answer to a warming planet and a major obstacle to actually confronting it. My colleague, Emily Badger, on the increasingly dangerous paradox of trying to control the temperature.
It’s Friday, August 16.
Emily, I want to start with a very personal question for you. What is your relationship to air conditioning?
So, at this exact moment, I am sitting in no air conditioning and it is kind of uncomfortable. And I’ve turned it off because it’s loud and it’s not very conducive to recording a podcast.
[CHUCKLES]: I didn’t mean right now, I meant in the larger arc of your life. But thank you for turning it off for the purposes of this episode.
Yeah. So I grew up in Chicago in this brick three flat apartment building, this very classic Chicago architecture, you know, built in the early 1900s. And it didn’t have air conditioning, so I didn’t have air conditioning growing up. Hardly anybody I knew had air conditioning growing up because we all lived in buildings like this.
Not even window units, just didn’t happen.
Nope, we didn’t even have a window unit in my family. And it wasn’t that big of a deal, in retrospect. We had, in this apartment, these big open windows that you could open and you’d generate a cross breeze through them. And there’s this kind of lovely breeze that comes off of Lake Michigan in the summer. And when it gets really, really hot, you know, you take a cold shower at night before you get in bed. You eat a lot of ice cream.
I can’t even remember if we had air conditioning in the schools that I went to. But it just wasn’t something that I thought very much about or really even experienced very much.
Right. You didn’t miss it. You didn’t even know it could be.
Yeah, exactly.
And then, the first job that I got out of college, I moved to Orlando, and totally different environment. I mean, living in Florida is the story of moving from one air conditioned box into another. You’re in your air conditioned apartment. You get in your air conditioned car. You don’t walk anywhere. You drive everywhere you go. You drive to your air conditioned office. You go to air conditioned bars. And it’s a really, really integral to life there in a way that was very foreign to me as someone growing up in the North.
So you went from a dearth of air conditioning to suddenly being saturated by it. And was that a happy development?
You know, I don’t think that I really gave it that much thought. I mean, living in Orlando surrounded by air conditioning, it’s just sort of that’s the air that you breathe. That’s the way everyone lives. And I think this is probably true for lots of people. We don’t really give it a lot of thought. It’s just sort of a background part of our environment.
But as I have written for years now about urban policy in cities, and how we live, and how we develop cities, it’s sort of become increasingly clear to me that air conditioning is this incredibly important thing that is shaping everything around us. You know, it’s shaping where Americans live, where they choose to move to. It shapes how our houses look. It shapes what our skylines look like. It’s responsible for saving lives and heat waves. In many ways, it’s really improved our quality of life.
But it’s increasingly clear to us that there are some downsides to this. And one of those downsides is that while we’re all sitting in our air conditioned homes, and offices, and cars, and we’ve set the thermostat to exactly 72 degrees, we’re becoming increasingly detached from what’s happening in the environment outside. It is a lot easier to ignore that it’s 100 degrees outside when you’re sitting inside air conditioning.
And, in some ways, I think we have forgotten how to live with heat. We have forgotten how to live with the climate as it existed before air conditioning. And having forgotten that, it’s probably going to cause some problems for us going forward.
Well, Emily, what did the American landscape look like when people did have to contend with the heat in the days before air conditioning?
So I think about two big things in particular. One is that the buildings that we spend time in looked different. We designed houses and other kinds of buildings in ways that were really sort of thoughtfully trying to contend with the temperature outside.
And so you’ve got these buildings in the Southwest in the United States that have these thick Adobe walls that do a really good job of keeping the sun and its heat out. You’ve got these cottages and bungalows in the Southeast that are raised up off the ground so that they’re not receiving the heat that’s absorbed by the Earth.
They’ve got big windows. They’re thinking a lot about cross ventilation. They’ve got high ceilings so that, as heat rises inside your home, you’re not marinating in it while you’re sitting in your living room. They’ve got front porches where people sit at the end of the day in order to try to cool off.
And then you’ve got the building like the one I grew up in, in Chicago, which I mentioned — these sort of thick brick masonry buildings, which are also designed in a way that is making it possible for me to grow up in the 1980s and ‘90s and be OK with the fact that I don’t have air conditioning.
Because brick kind of retains cool air.
Right. Right. And so part of what results from all of this is that the buildings in Georgia look different from the buildings in Arizona, look different from the buildings in Chicago. Because in each of those places, we’re designing buildings that react to the particular climate in those environments. And so this is the first big change.
Think of a time when you have to design a building to interact with what’s going on outside, with how humid it is, with how hot it gets. But the other thing that was very different in the pre-air conditioning environment is that there were just a lot fewer people living in the parts of the United States that were really hot and swampy. So it’s kind of incredible to think about it, but 1940, there are fewer people living in the state of Florida than living in the state of Arkansas.
There are about 8,000 people total living in the city of Las Vegas. Dallas and Houston are nowhere to be found on the list of the largest cities in America. So fundamentally, before air conditioning, there just aren’t a lot of people living in places where it is uncomfortable if you’re not controlling the temperature in some way.
Right. If it’s too hot, then you just don’t live there.
Right. So climate shapes your decisions about where to live. It shapes your decisions about how to build housing. It shapes your decisions about where to spend your time and your house. Maybe you go onto your front porch in the evening when it’s cooling down. You know, in many ways, our behavior is shaped by the climate. And then air conditioning comes along and it totally changes everything that I’ve been talking about. Because now the outdoor climate doesn’t really affect what your life is like indoors.
Just tell us about that moment, because I don’t think any of us really know the story.
Yeah. So there have been contraptions invented in the 1900s that were trying to do things like blow forced air over big blocks of ice in order to cool it. But the thing that we really think of as air conditioning is just totally a 20th century story.
It starts at the very beginning of the 20th century in 1902, when Willis Carrier invents this machine that’s kind of controlling the temperature, and the humidity, and the purity of air, particularly in an industrial context. The very first use of this in 1902 is in a printing plant, and fundamentally the problem that it’s solving is that the moisture content in the air is really becoming a problem for printing documents.
You’re saying basically, publishing, journalism is responsible for air conditioning.
Yes, everybody can thank us and then later they can blame us.
And so, in the beginning, what air conditioning is doing is it’s solving an industrial problem. The machines are hot, or maybe it’s a textile mill and too much humidity is sort of destroying your textiles. And also, you want your workers to be productive in these manufacturing spaces.
Lots of people in a small space with hot machines. Right.
Yeah. And so in the very beginning of the 20th century, it’s not about providing comfort for people. It’s about conditioning the environments that manufacturing and industry is having. And then it is this very sort of long story that plays out over several decades, where this invention moves from these industrial spaces into these other kinds of spaces.
Yes, you lucky people. Just sit back for a moment, relax, and notice the delightfully clean, cool, and refreshing atmosphere of this scientifically air conditioned theater. Great, isn’t it?
So then it comes into theaters and becomes almost this marketing tool to attract people inside.
You can enjoy great motion picture entertainment all summer long in cool comfort.
Go see a movie and enjoy air conditioning while you’re in there.
Yes, low-cost all-season air conditioning is the right kind for you. And you’re so right to choose a ‘55 Rambler Cross Country, now at all dealers.
And then, at the same time, cars in America that have air conditioning in them — the share of those cars is rising and rising. It moves into office buildings.
Instead of traveling away from business and home to seek relief, you can obtain this same comfort right in your own home or office through air conditioning.
And then, eventually, after decades of refining this technology, and it gets smaller, and it gets more affordable, and it becomes more advanced —
This lucky baby will sleep quietly through the night.
— it reaches the American home and we get the window unit.
This baby’s RCA air conditioner will keep his room filled with cool, dry, fresh air.
And the window unit is this much more affordable, portable, easy to pick up at the store, bring to your house. You don’t need to get a special installer. You stick it in your window, and now all of a sudden you’re getting all of these benefits of humidity controlled, temperature controlled air inside of your home.
Humidity, controlled, dust and pollen filtered. My indoor climate is always perfect.
At that point it’s off to the races. It takes over the American home. And we can see in census data, for instance, that by about the start of the 1970s, about half of all new single family homes that are built in America have air conditioning in them.
And the other thing that we see in census data at this time is that Americans themselves are starting to move to places that are really hot, like Florida, like Texas, like Arizona, like Nevada, places that are kind of uninhabitable before air conditioning. Now they’re booming in population.
And there was this wonderful editorial that was actually published in “The Times” in 1970 about the census that year, and how 1970 was like, the air conditioning census. And it refers to how air conditioning had become this really powerful influence for circulating people as well as air in this country.
And this is a story that continues right up until this day, where air conditioning is sort of extending its reach into every corner of the country, every sort of housing type. And today, about 2/3 of American households in this country have central air, and about 90 percent, so 9 in 10 of them, have some kind of error conditioning if we include things like window units. And if we look just at New housing that’s built in America today, looking back in 2023, about 98 percent of new single family homes in America had air conditioning.
What you’re talking about is basically 200 or so million air conditioning units, condensers, boxes. That’s a lot.
Yeah. And as air conditioning has extended its reach into every corner of the country, into so many of the buildings where we spend time, I think it becomes clear that we’ve really kind of engineered our modern lives entirely around it.
And our reliance on this technology going forward is both unsustainable, and in fact, it’s put a lot of people in a very vulnerable position.
We’ll be right back.
Emily, walk us through how our reliance on air conditioning is both, as you just said, unsustainable and perhaps even kind of dangerous to us.
So the first obvious thing that it does is it just requires an enormous amount of energy for so many people to be air conditioning so many spaces all the time. And so to think about this in a larger sense, our buildings in the United States are responsible for about 30 percent of the greenhouse gas emissions. And that refers to the fossil fuels that we burn directly to heat and cool buildings, and to cook in them, but also to generate the electricity that then allows us to do things plug in our window units.
So there’s a ton of energy use happening here. But part of what’s also happening is that all of these buildings have been fundamentally designed to consume lots of energy. A lot of these buildings were built during a time, you know, in the ‘50s and the ‘60s and in more recent years, where energy was cheap. The idea that you’re designing a building that demands lots of energy — who cares? We’re not paying a ton of money for the energy.
And in the ‘60s and in the ‘50s, we weren’t particularly thinking about whether or not using energy is going to cause climate change. So because of this, we get this glut of inefficient houses. And this happens not just with houses, but with everything in the built environment.
Think about strip malls, shopping centers, workplaces, even offices — the sort of ubiquitous, tall, boxy, glass-covered office building that we think about in cities all over the country, all over the world — this is a building that is born out of the air conditioning age. That glassy box is designed around air conditioning such that without air conditioning, those kinds of offices don’t make sense.
Right. I’m thinking about the office that you and I call home, the “New York Times” high-rise building in Midtown. That does not feel, for all its virtues, like a building, you’d want to be in without air conditioning.
It’s glass, and tall, and I think it’d be very hot.
Yeah. When you think about tall glass office buildings, they’re basically greenhouses if you’re not controlling the air inside. They’re designed such that not only do you not have to open a window in order to cool off, you couldn’t open a window even if you wanted to. These buildings don’t have windows that open, because they’re designed to be these hermetically sealed environments where we’re going to keep the outside climate out and we’re going to control the climate on the inside. And this idea that the outside doesn’t matter is true in the design of so many of our buildings, our offices, even our homes. And that actually puts people into an incredibly vulnerable situation.
And vulnerable how, exactly?
So let’s assume a storm comes through and the power goes out, or your air conditioning stops working because you’ve been running it all the time, all summer long, or when we have these extreme heat conditions and the electric utility tells you, please try to preserve the amount of air conditioning that you’re using. What happens when, all of a sudden, millions of people who have been living in an environment designed entirely around air conditioning can’t have that air conditioning? We start to see real problems.
And this is an abstract. We have actually seen this happen in the United States even this year, in other recent years, where terrible storms have ripped through the state of Texas and millions of people have been left without power. And when this happens in the middle of a heat wave, people die.
Right. And that seems an example of the multiple ways that air conditioning conspires to make us avoid contending with the realities of heat to return to this idea you introduced earlier on. AC allows more people to go to a place like Texas than they’d ever go if there weren’t AC making them comfortable, and to design and live in homes and offices that become a cauldron without air conditioning when it fails.
Exactly. Air conditioning makes it possible for people to believe that you could be comfortable in Texas in the summer, in Arizona in the summer. And so people move to these places in large numbers. And then, when the air conditioning fails, they’re sort of suddenly thrust into a world where they’re living in the middle of the Arizona desert or they’re living in the middle of Texas on a 110 degree day. And that could be life threatening.
Especially with climate change making it even hotter in these places, it doesn’t really seem sustainable for a lot of people to live in those places without air conditioning, without some kind of artificial tempering of the environment.
Yeah. And it’s not just because of the heat. I mean, is it sustainable for a Metropolitan area of 5 million people to exist in Phoenix in the middle of the desert when there’s also not enough water there for everyone? So air conditioning sort of lulls people into moving to these places, which might be problematic for lots of other reasons, as well. But we’ve sort of convinced ourselves that the climate doesn’t matter. We’re going to control it. We’re going to engineer our way into living with it.
You’re reminding me, Emily, of an episode we did on the show about this very idea. It focused on the water shortage in Arizona and the plans to pipe in — and, as I recall, desalinate ocean water — to deal with the problem of not enough water in Arizona. And it doesn’t really seem fathomable that proposition would ever occur to people if they weren’t living there in the comfort of air conditioning in the first place.
Yeah. So there have been people living in the region of Phoenix for centuries, so it’s not that nobody can ever live there. But what air conditioning does is it enables millions of people to live there who don’t actually want to contend with 100 degree temperatures all summer long. So a place like Phoenix then becomes this perfect example where we now have 5 million people living in the middle of the Arizona desert, and they all have this expectation of comfort there, that any environment that I move into — in my home, in my office, in my car — I should be encased in this cooling, calm, 72 degree humidity controlled environment. And that sense of comfort becomes so deeply entrenched kind of culturally. And this isn’t just about Phoenix. This is about all of us. I think we have set up an expectation or even an entitlement around comfort such that it makes it really difficult to start to ask people, do you really need to turn up your air conditioning today?
So that makes me wonder how people are ever going to get off the air conditioning hamster wheel that we’re describing here. I mean, why would anyone?
Well, we have to figure out how to do something if we want to address climate change. So there are a number of different things that are going to happen here. Air conditioning is going to become more efficient. We’re going to have more renewable energy sources to power it in the future. And I think we’re increasingly going to see architects and builders trying to rediscover these lost ideas that we used to have about how to design buildings with the climate in mind, how to shade them, how to ventilate them in a more natural way.
But I also have talked to some people who say that all of that is not going to be enough. One of them is Daniel Barber, who’s an architectural historian who has thought a lot about life after air conditioning or, as he puts it, after comfort — life in a world where we’re not depending on air conditioning so much. And the point that he makes is that there are difficult things and changes that we would have to do going forward if we know that our buildings are responsible for a lot of greenhouse gas emissions.
Our dependence on air conditioning is responsible for a large share of that, and we have to reduce it in some way. What we all need to do is change our own behavior. We need to think anew about our relationship to comfort. And are we willing to be uncomfortable some of the time? Am I willing to wait until July to turn my air conditioning on? Am I willing to turn it off at night when it’s not really necessary to use it? Am I willing to sleep at 80 degrees instead of 72 degrees?
Or 68 or 65. And he’s talking about asking people to do something really difficult. He is asking people to be uncomfortable.
You are, of course, by conveying this message, putting this problem on individuals, not governments, not states. And lots of people might hear this and think the real solutions have to come from regulators, have to come from institutions, have to come from the people who have a lot more control over how this all works.
I think that there are some ways in which that will happen, too. When we think about new buildings that are being designed or renovated today that are trying to adopt some of these techniques to be less reliant on indoor air conditioning. They’re often institutional buildings you will see cities commit to when we rebuild our schools, when we build a new library, when we build a new civic center, we are going to embody these things that we are asking other people to do, too.
And, obviously, there are government incentives in the United states, for instance, to better insulate your home, to do things that would make your home greener. So there’s certainly a role for government. But what Daniel Barber at least would argue is that we all bear some responsibility. And air conditioning has lulled us into thinking that we’re not impacted by how hot it is outside. But it’s also maybe lulled us into thinking like, I’m not the one who needs to particularly change my behavior in any way.
But, fundamentally, what we’re talking about is people embracing a kind of different cultural idea about what it means to be comfortable. The idea that existing in a room that is artificially cooled to 68 to 72 degrees fahrenheit, that that’s the ideal temperature — that’s not some true fact about the human body. It’s a cultural idea that’s been created over decades by the air conditioning industry, by architects, and builders, and culture, and shopping malls, and movie theaters. And the idea that comfort means this one particular thing is an idea that we have constructed ourselves. And so what if we culturally came up with a different idea about comfort?
What if more people came to accept the idea that going and sitting out on my front porch in the evening is where I get comfort from? And it’s also, by the way, how I interact with my neighbors. And I had stopped doing that when we were all retreating inside to air conditioning. What if we revived the idea that it’s actually quite lovely in the summertime to sleep with an open window and to have fresh air? It’s not impossible to change ideas about this because we created these ideas in the first place.
Well, Emily, thank you very much. We really appreciate it.
Yeah. Thanks, Michael.
Here’s what else you need to know today. On Thursday, the White House said that its newfound authority to use the Medicare program to negotiate prices of prescription drugs with pharmaceutical companies is likely to save taxpayers about $6 billion a year. That power came from President Biden’s Inflation Reduction Act, which became law two years ago. Under it, regulators have now lowered the price of widely used treatments, including blood thinners and medications for arthritis and diabetes, some by up to 79 percent.
And both vice presidential nominees, Minnesota Governor Tim Walz and Ohio Senator JD Vance, have agreed to debate each other on October 1 during a televised face-off hosted by CBS News. That means there will be three debates before election day — one vice presidential debate and two presidential debates between Donald Trump and Kamala Harris.
Finally, remember to catch a new episode of “The Interview” right here tomorrow. This week, David Marchese speaks with the singer Jelly Roll about addiction recovery and putting his whole self into his music.
I think of everything as a going out of business sale, and I give everything I got everything I do every time I do it right now.
Today’s episode was produced by Shannon Lin and Diana Nguyen with help from Michael Simon Johnson. It was edited by Devon Taylor, contains research help from Susan Lee, original music by Marion Lozano, Dan Powell, Rowen Niemisto, and Will Reid, and was engineered by Alyssa Moxley. Our theme music is by Jim Brunberg and Ben Landsverk of Wonderly.
That’s it for “The Daily.” I’m Michael Barbaro. See you on Monday.

- Apple Podcasts
- Google Podcasts

Hosted by Michael Barbaro
Featuring Emily Badger
Produced by Shannon M. Lin and Diana Nguyen
With Michael Simon Johnson
Edited by Devon Taylor
Original music by Marion Lozano Dan Powell Rowan Niemisto and Will Reid
Engineered by Alyssa Moxley
Listen and follow ‘The Daily’ Apple Podcasts | Spotify | Amazon Music | YouTube | iHeartRadio
Air-conditioning has become both our answer to a warming planet and a major obstacle to actually confronting it.
Emily Badger, who covers cities and urban policy for The Times, explains the increasingly dangerous paradox of trying to control the temperature.
On today’s episode

Emily Badger , who covers cities and urban policy for The New York Times.

Background reading
From 2017: How air-conditioning conquered America .
Air-conditioning use will surge in a warming world , the U.N. has warned.
There are a lot of ways to listen to The Daily. Here’s how.
We aim to make transcripts available the next workday after an episode’s publication. You can find them at the top of the page.
Research help by Susan Lee .
The Daily is made by Rachel Quester, Lynsea Garrison, Clare Toeniskoetter, Paige Cowett, Michael Simon Johnson, Brad Fisher, Chris Wood, Jessica Cheung, Stella Tan, Alexandra Leigh Young, Lisa Chow, Eric Krupke, Marc Georges, Luke Vander Ploeg, M.J. Davis Lin, Dan Powell, Sydney Harper, Michael Benoist, Liz O. Baylen, Asthaa Chaturvedi, Rachelle Bonja, Diana Nguyen, Marion Lozano, Corey Schreppel, Rob Szypko, Elisheba Ittoop, Mooj Zadie, Patricia Willens, Rowan Niemisto, Jody Becker, Rikki Novetsky, Nina Feldman, Will Reid, Carlos Prieto, Ben Calhoun, Susan Lee, Lexie Diao, Mary Wilson, Alex Stern, Sophia Lanman, Shannon Lin, Diane Wong, Devon Taylor, Alyssa Moxley, Olivia Natt, Daniel Ramirez and Brendan Klinkenberg.
Our theme music is by Jim Brunberg and Ben Landsverk of Wonderly. Special thanks to Sam Dolnick, Paula Szuchman, Lisa Tobin, Larissa Anderson, Julia Simon, Sofia Milan, Mahima Chablani, Elizabeth Davis-Moorer, Jeffrey Miranda, Maddy Masiello, Isabella Anderson, Nina Lassam and Nick Pitman.
Emily Badger writes about cities and urban policy for The Times from Washington. She’s particularly interested in housing, transportation and inequality — and how they’re all connected. More about Emily Badger
Advertisement

IMAGES
COMMENTS
The answer is, because music can activate almost all brain regions and networks, it can help to keep a myriad of brain pathways and networks strong, including those networks that are involved in well-being, learning, cognitive function, quality of life, and happiness. In fact, there is only one other situation in which you can activate so many ...
Moreover, music can be used to help in addressing serious mental health and substance use disorders. 2 In addition to its healing potential, music can magnify the message of diversity and inclusion by introducing people to new cultures and amplifying the voice of marginalized communities, thereby enhancing our understanding and appreciation for ...
Another significant way music influences mental health is through its ability to foster social connectivity and a sense of community. Group musical activities, such as choirs, bands, and dance ensembles, offer opportunities for social interaction and collective expression. Engaging in these activities can enhance social bonds, reduce feelings ...
Music therapy also had significant benefit in preventing burnout in operating room staff. A 6-week study. Trusted Source. showed that after having access to 30-minute music listening sessions each ...
Listening to music can be entertaining, and some research suggests that it might even make you healthier. Music can be a source of pleasure and contentment, but there are many other psychological benefits as well. Music can relax the mind, energize the body, and help people manage pain better. The notion that music can influence your thoughts ...
When it comes to your mental health, music can: . Help you rest better. A study involving students found that listening to relaxing classical music at bedtime improved sleep quality. This ...
The analysis also points to just how music influences health. The researchers found that listening to and playing music increase the body's production of the antibody immunoglobulin A and natural killer cells — the cells that attack invading viruses and boost the immune system's effectiveness. Music also reduces levels of the stress hormone ...
251 Altmetric. Metrics. The association between active musical engagement (as leisure activity or professionally) and mental health is still unclear, with earlier studies reporting contrasting ...
Research into music and mental health typically focuses on measures of music engagement, including passive (e.g., listening to music for pleasure or as a part of an intervention) and active music ...
In music therapy, clients play and listen to music as treatment for stress, depression and anxiety. Here's how it works. Isobell, 17, plays guitar and sings during a music therapy session at ...
Music even shows promise in preventing injury: A study by Annapolis, Maryland-based neurologic music therapist Kerry Devlin and colleagues showed that music therapy can help older adults with Parkinson's disease and other movement disorders improve their gait and reduce falls ( Current Neurology and Neuroscience Reports, Vol. 19, No. 11, 2019).
Music therapy, or just listening to music, can be good for the heart. November 2009 Reviewed and updated March 25, 2015 Music can make you laugh or cry, rile you up or calm you down. Some say it's good for the soul. It just might be good for the heart, too. Make no mistake—daily doses of Mozart won't clean
Music and health. Music is a fundamental attribute of the human species. Virtually all cultures, from the most primitive to the most advanced, make music. It's been true through history, and it's true throughout an individual's lifespan. In tune or not, we humans sing and hum; in time or not, we clap and sway; in step or not, we dance and bounce.
2. Music, music therapy and mental health. Utilising music as a structured intervention in treating mental illnesses such as anxiety, depression and schizophrenia has been reported as beneficial in relieving symptoms (Mössler et al., 2011; Erkkilä et al., 2011), while improving mood and social interactions (Edwards, 2006).Some people with mental disorders may be too disturbed to use verbal ...
This recent systematic review and meta-analysis (a study of studies) showed that the use of music interventions (listening to music, singing, and music therapy) can create significant improvements in mental health, and smaller improvements in physical health-related quality of life. While the researchers found a positive impact on the ...
One of the ways in which music affects mental health is through its impact on mood modulation. Certain types of music, such as upbeat and rhythmic tunes, have been shown to increase feelings of happiness and excitement. Slow and calming music, on the other hand, can help reduce stress and anxiety. The brain's response to music involves the ...
Research into music therapy for people who are deaf and also have mental health disorders is more limited, but case studies suggest, just as in hearing people, music can help people with hearing loss express emotions and improve cognitive abilities. Cook uses table drums to connect with her deaf cousin. "Table drums are massive, and you can ...
Music has also been used successfully to support recovery after surgery. A study published in The Lancet in 2015 reported that music reduced postoperative pain and anxiety and lessened the need ...
Taryn from Mind blogs about new research confirming the power of music to reduce stress. Last month, researchers found that music releases dopamine, the feel-good chemical in your brain. It also found that dopamine was up to 9% higher when volunteers listened to music that they enjoyed. It may be obvious to us, but it is strong evidence for the ...
The positive effects associated with music interventions may be just as powerful as those associated with a commitment to exercise or weight loss. For individuals who may have limited capacity for physical activity to boost mental health functioning, music may provide a welcome alternative. Many report mental health benefits from music.
Music making includes singing and playing an instrument. Learning to play a musical instrument can offer a sense of mastery and self-esteem, while enhancing brain activity. Singing may be the simplest way to get started. 7. Listen to fun music when you exercise. Music can help motivate you to move.
Music and mental health. Music therapy is a practice where music engagement — activities like songwriting, listening to music, singing and playing an instrument — is used to address the ...
This post is a review of I Heard There Was A Secret Chord: Music As Medicine. By Daniel J. Levitin. W.W. Norton & Co. 405 pp. $32.50. In 1993, Nature magazine reported on a study suggesting that ...
The Covid-19 pandemic era ushered in a new set of challenges for youth in the United States, leading to a mental health crisis as declared by the United States surgeon general just over a year ago.But U.S. children and teens have been suffering for far longer. In the 10 years leading up to the pandemic, feelings of persistent sadness and hopelessness—as well as suicidal thoughts and ...
ChatGPT is a versatile tool that can help with tasks like writing customized resumes & cover letters. The AI can generate original jokes and memes, as well as explain complex topics in an easy-to-understand manner. ChatGPT can assist with mathematics, music composition, coding, media file manipulation, and health improvement.
Research help by Susan Lee.. The Daily is made by Rachel Quester, Lynsea Garrison, Clare Toeniskoetter, Paige Cowett, Michael Simon Johnson, Brad Fisher, Chris Wood ...