Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- 27 January 2021

How epidemiology has shaped the COVID pandemic
You have full access to this article via your institution.

Measures such as mask-wearing have been used around the world to try to stop the spread of coronavirus. Credit: Chine Nouvelle/SIPA/Shutterstock
Epidemiology is essential to the fight against any disease. The study of how diseases spread, and why, has loomed large in the struggle to understand, contain and respond to COVID-19. Analyses of data on infections and deaths, and projections from studies that model the virus’s spread, have driven policy decisions all over the world. Many of these, such as locking down countries, imposing quarantines, and mandating social distancing and mask-wearing, are now commonplace.
This editorial — the third instalment in Nature ’s series of pandemic progress reports — explores some of the key research developments that have helped to illuminate the nature of the infection and the scale of the pandemic.
We also highlight how epidemiology will be important as the pandemic progresses — for example, in understanding the potential impact of the new variants that are currently wreaking havoc around the world. Epidemiology is changing the course of the pandemic, but the coronavirus has stress-tested epidemiology, too, and this report briefly explores how the field is changing as a result.
Epidemiology’s early role
It is now more than a year since reports began to emerge of a previously unknown coronavirus causing pneumonia-like symptoms. By 5 January 2020, the virus was reported to have infected 59 people in the city of Wuhan in China’s Hubei province; 7 were in a critical condition . By 20 January, the Chinese authorities had reported more than 200 infections and 3 deaths.
Initially, little was known about the virus’s transmissibility, but that quickly changed. By about the middle of January, epidemiologists began reporting the results of modelling studies, which indicated that case numbers were likely to be much higher 1 than had initially been documented.
These studies found, for example, that the ‘ R 0 ’ rate — which describes the number of people an infected person will pass the virus on to, on average, if the virus is allowed to spread uncontrolled — to be between 2 and 4 2 , 3 Studies also estimated crucial parameters for understanding the virus’s epidemic potential. This included its mean incubation period 4 — the time between a person getting infected and the onset of symptoms — and the proportion of people for whom the infection will be fatal 5 . Even early on, it was evident that the risk to people aged over 60 was substantially higher than that for younger age groups. Some estimates suggested that more than 1 in 10 of those over the age of 80 who became infected would not survive 5 .
In these first weeks, researchers were working with limited patient data. However, as more data became available, epidemiologists were able to confirm that the virus could be transmitted by people showing no symptoms 6 and that it had high pandemic potential 1 .
Taken together, these studies helped to alert many governments to the fact that the situation might be much more severe than they had anticipated. The findings suggested that hospitals worldwide needed to prepare for a high number of admissions to intensive care.
At the end of January, the World Health Organization declared a Public Health Emergency of International Concern, which included advice for countries on implementing public-health measures, including testing and isolating infected people, and tracing and quarantining their contacts. These moves were based, in part, on research done by epidemiologists after previous infectious-disease outbreaks 7 . But few countries followed this advice .
At the same time, the epidemiological community also began turning its attention to evaluating measures that might help to contain the virus.
Lockdowns and masks
As case numbers started to soar, countries’ options for reducing infections and deaths were very limited. It was hard to know what drug regimes might help to combat the disease, and there were no vaccines. In the absence of such tools, researchers began modelling the effectiveness of what are called non-pharmaceutical interventions.
Their models suggested that infections and deaths could be reduced if people wore face masks and maintained a degree of distance from one another, and if more people stayed at home 8 , 9 .
Wuhan went into lockdown on 23 January, and by the middle of February movement was being restricted in about 80 other cities in China. Some months later, researchers would confirm that a range of public-health measures, including closing schools, restricting travel and reducing mixing to within households, brought transmission rates in Wuhan down 3 .
Studies from outside China also later affirmed that transmission dropped considerably after educational institutions were closed, gatherings limited and essential businesses closed 10 , 11 . Moreover, researchers predicted that cities that delayed enacting restrictions would have to keep restrictions in place for longer periods before the virus could be controlled 12 .
Although mask-wearing is known to help combat the spread of many infectious respiratory diseases, the lack of controlled trials and direct data meant more time would be required before researchers were able to establish the effectiveness of the measure against the coronavirus. But by the summer of 2020, a number of studies had found that masks contribute to slowing the spread of coronavirus 13 , 14 .
New unknowns
As the virus continues to surge across much of the world, new variants have emerged, and are prompting new questions for epidemiologists. Researchers say that these newer variants, such as B.1.1.7 (also known as VOC 202012/01), first identified in the United Kingdom, are more transmissible and potentially more severe than earlier lineages of the virus ( go.nature.com/3a9i9p4 ). Such findings have implications for policy interventions that were based on earlier data on transmission. Epidemiologists will need to re-evaluate, on the basis of more recent data, whether guidelines on interventions such as social distancing need to be revised and made more stringent to account for the different ways the new variants behave.
Another new challenge for epidemiologists is measuring how the vaccines currently being rolled out around the world affect the virus’s spread. Countries where rollouts have already begun might soon be looking to relax restrictions, especially if cases and deaths fall to levels seen before the start of the second wave. But they should not do so before epidemiologists have established the extent to which vaccines are contributing to increased immunity and the extent to which a fall in cases is the result of the effects of restrictions.
Epidemiology is changing
The pandemic has changed epidemiology. As with many fields that are directly involved in the study of COVID-19, epidemiologists are collaborating across borders and time zones. They are sharing their data using online platforms — preprint servers are giving scientists early access to results — and journals are publishing at a faster rate.
Epidemiology itself is expanding, with the involvement of researchers from other fields, such as physics, mathematics, computer science and network science, who have been contributing their ideas and expertise. The US government has announced that it will establish a National Center for Epidemic Forecasting and Outbreak Analytics. We hope that this will be the epidemiological equivalent of a central meteorological office, an independent body that provides forecasts using advanced computational power, and the best available data. Other countries should consider doing the same.
With many more researchers joining the field from different disciplines — and more people using epidemiological data, including the public, policymakers and the media — researchers must find ways to make sure that their data and findings are communicated transparently, and to ensure the highest standards of research and data ethics.
Communication challenge
The pandemic has thrust epidemiologists and epidemiological models into the policy and media spotlight like never before, and they have faced many challenges. Epidemiology — in particular, epidemic modelling and forecasting — relies on statistical methods to make probabilistic predictions from real-time data. These initial predictions are often not accurate, in part because the underlying data can be incomplete and inconsistently categorized. Over time, as the data improve and more research groups become involved, results start to look more certain. But often, decisions such as whether to impose restrictions on movement need to be made before there is certainty. Epidemiologists need to communicate both the certainty and the uncertainty of their findings so that the best decisions can be reached.
This has meant that researchers have had to learn how to communicate the inherent uncertainty in their models and predictions in such a way that people can understand that an inaccurate prediction does not invalidate the model and that a general conclusion can still stand. It has also meant that people and policymakers have been exposed to new terminology — words and phrases that help to explain and visualize uncertainty — and models providing a range of probabilistic forecasts from best- to worst-case scenarios.
These challenges also represent an opportunity. They provide a chance to showcase science as it is happening, in real time — something that only researchers normally see. The pandemic has helped people to understand that science, by its very nature, needs to be continually corrected and refined, its conclusions changing as the balance of evidence changes. This contrasts with the way many may have previously viewed science — as a body of knowledge that is fixed and unchanging. The change in how science is perceived might give the impression that scientists are changing their minds, but to do so when the facts change can only be a good thing.
If the past year has taught us anything, it is that knowledge of public-health tools and access to data are not enough to control a pandemic. People have a natural desire for certainty in the face of something as alarming as a pandemic, yet the science informing the pandemic response, by its nature, operates through probabilities. This does not diminish the impact of epidemiology, but, rather, highlights the importance of maintaining a continuous and transparent conversation between researchers, policymakers and the public.
Nature 589 , 491-492 (2021)
doi: https://doi.org/10.1038/d41586-021-00183-z
Wu, J. T., Leung, K. & Leung, G. M. Lancet 395 , 689–697 (2020).
Article PubMed Google Scholar
Li, Q. et al. N. Engl. J. Med. 382 , 1199–1207 (2020).
Hao, X. et al. Nature 584 , 420–424 (2020).
Wu, J. T. et al. Nature Med. 26 , 506–510 (2020).
Verity, R. et al. Lancet Infect. Dis. 20 , 669–677 (2020).
He, X. et al. Nature Med. 26 , 672–675 (2020).
Fraser, C., Riley, S., Anderson, R. M. & Ferguson, N. M. Proc. Natl Acad. Sci. USA 101 , 6146–6151 (2004).
Davies, N. G. et al. Lancet Public Health 5 , e375–e385 (2020).
Ferguson, N. M. et al. COVID-19 Report 9 https://doi.org/10.25561/77482 (Imperial Coll. Lond., 2020).
Flaxman, S. et al. Nature 584 , 257–261 (2020).
Hsiang, S. et al. Nature 584 , 262–267 (2020).
Du, Z. et al. Emerg. Infect. Dis. 26 , 2267–2269 (2020).
Article Google Scholar
Lyu, W. & Wehby, G. L. Health Aff. https://doi.org/10.1377/hlthaff.2020.00818 (2020).
IHME COVID-19 Forecasting Team. Nature Med. 27 , 94–105 (2021).
Download references
Reprints and permissions
Related Articles

- Public health

Animal-to-human viral leap sparked deadly Marburg outbreak
News 24 OCT 24
Just widening access to the right drugs won’t solve antimicrobial resistance
Correspondence 15 OCT 24
Rwanda’s seven steps in seven days for managing Marburg virus
Correspondence 10 OCT 24

How to demonstrate the real-world impact of your research
Career Column 30 OCT 24

How to recover when a climate disaster destroys your city
News Feature 30 OCT 24

A thaw in scientific relations could help clear the air in India and Pakistan
Editorial 30 OCT 24

Diabetes risk soars for adults who had a sweet tooth as kids
News 31 OCT 24
PhD studentship in Analytical Chemistry
Urban Lab invites applications for PhD studentship in Analytical Chemistry. The graduate research will encompass development of novel analytical to...
Hsinchu (TW)
Urban Lab at National Tsing Hua University
Global Faculty Recruitment of School of Life Sciences, Tsinghua University
The School of Life Sciences at Tsinghua University invites applications for tenure-track or tenured faculty positions at all ranks (Assistant/Ass...
Beijing, China
Tsinghua University (The School of Life Sciences)
Full-Time Faculty Member in Molecular Agrobiology at Peking University
Faculty positions in molecular agrobiology, including plant (crop) molecular biology, crop genomics and agrobiotechnology and etc.
School of Advanced Agricultural Sciences, Peking University
Tenure-track Faculty Positions in Particle Physics and Cosmology
Faculty Positions in Particle Physics and Cosmology
Hong Kong (HK)
Department of Physics, The Hong Kong University of Science & Technology (HKUST)

Assistant/Associate Professor
Center for Virology and Vaccine Research at Beth Israel Deaconess Medical Center is seeking Assistant or Associate Professor.
Boston, Massachusetts (US)
Beth Israel Deaconess Medical Center (BIDMC)
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List

The COVID-19 Pandemic: Public Health and Epidemiology
Colin binns , mbbs, phd, wah yun low , phd, lee mi kyung , phd.
- Author information
- Article notes
- Copyright and License information
Colin Binns, School of Public Health, Curtin University, Perth, Western Australia 6102, Australia. Email: [email protected]
Issue date 2020 May.
This article is distributed under the terms of the Creative Commons Attribution 4.0 License ( https://creativecommons.org/licenses/by/4.0/ ) which permits any use, reproduction and distribution of the work without further permission provided the original work is attributed as specified on the SAGE and Open Access page ( https://us.sagepub.com/en-us/nam/open-access-at-sage ).
In this issue of the journal, we publish a review of COVID-19 infection by 2 eminent virologists, MacKenzie and Smith (see in this issue). It is too early in the history of the COVID-19 outbreak to write the full history, but their article provides a good outline of the emerging pandemic. The disease is causing widespread social disruption in many countries, and it has just been announced that the 2020 Asia Pacific Academic Consortium for Public Health (APACPH) Conference has been postponed indefinitely. The media are full of daily totals of new cases, hospital and intensive care admissions, and deaths. The actual numbers are dependent on the testing regimes in use at different locations. In the first 2 months of 2020, there were hundreds of papers and commentaries published on Corona viruses, including a major clinical review in the Lancet that has already had almost 500 citations. 1 Corona viruses are a large family of viruses that can cause human diseases, but usually mild in nature, such as a common cold. There have been two previous severe outbreaks of novel corona viruses: severe acute respiratory syndrome (SARS) in 2003 and Middle East respiratory syndrome coronavirus (MERS-CoV) in 2012, which together caused more than 10 000 cases. The case fatality rates (CFRs) were 10% for SARS-CoV and 37% for MERS-CoV. 1 In this commentary, we will discuss additional public health issues that will assist in teaching at our public health institutions.
Since the first cases of COVID-19, the reported numbers have increased rapidly with more than 1.2 million cases and 3200 deaths to the end of February 2020, and cases are now being reported from all of the more populous countries. 2 The symptoms of COVID-19 infection are nonspecific and include elevated temperature and cough. This, then, progresses to shortness of breath. 3 A clinical report of the first patients from Wuhan (n = 41) with COVID-19 infection gave the following details of clinical symptoms: fever 98%, cough 76%, myalgia or fatigue 44%, sputum 28%, and dyspnea 55%. The average time from the first onset of symptoms to the development of dyspnea was 8 days. In the first report from outside of Wuhan (from Zhejiang Province, n = 62), the symptoms were fever 77%, cough 81%, sputum 56%, headache 34%, and myalgia or fatigue 52%. The disease is more likely to occur in people who have a chronic illness, are immunocompromised, or are older. Those who contracted the virus and were older than 60 years of age, and particularly older than 80 years, were more likely to require admission to intensive care unit, and have an increased CFR 4 (see Table 1 in Mackenzie and Smith, this issue). In Wuhan, there were 1023 deaths from the 44 672 confirmed cases, an overall CFR of 2.3%.
The initial clinical symptoms of COVID-19 are the symptoms of a common cold and influenza. Every adult gets 2 to 3 colds per year, and more frequently in children. 5 With a world population of around 7.8 billion, this suggests that there are 20 billion cases every year. Screening all of these cases for possible COVID-19 would obviously be impossible, and so testing for the virus is confined to those with other risk factors, including contact with confirmed cases and travel from outbreak epicenters.
COVID-19 is the latest in a continuing series of infectious disease epidemics in the history of the human race. As population numbers and population density increases, the likelihood of epidemics increases. Probably, the greatest epidemic of all time was the influenza epidemic of 1918, which caused an estimated 50 million deaths worldwide and had a CFR of more than 2.5% and which could have been as high as 10%. 6 This was in the pre-antibiotic days, and before an influenza vaccine and antiviral therapy had been developed. Infectious diseases remain a major challenge for public health.
To assist in defining, containing, preventing, and ultimately in successfully treating those who become ill in an epidemic, it is important to understand the basic epidemiology of the outbreak. Experts from many institutions have collaborated together in an effort to categorize the COVID-19 outbreak. Most infectious diseases have a spectrum of severity from clinically undetected disease through to death. 7 Figure 1 is modified from the paper prepared by Imperial College. It is likely that only the cases with severe symptoms or other risk factors (e.g. contact with a known case) are being identified at present, but it varies between countries.
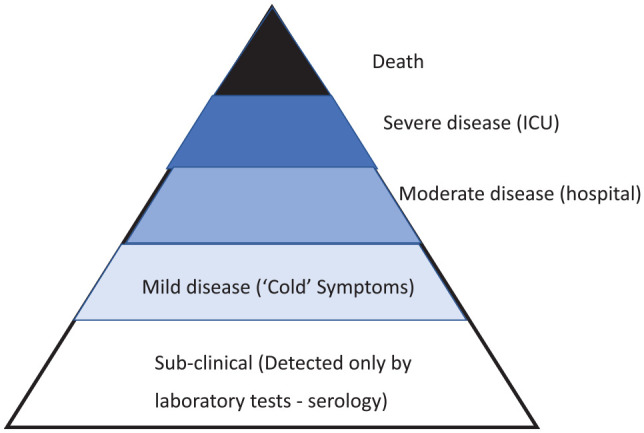
The clinical spectrum of COVID-19 infection.
For some diseases, the base of the triangle in Figure 1 would be much wider, and this may be the situation with COVID-19. The base of subclinical cases with minimal symptoms may be much greater than those with disease severe enough for hospital admission. The history of public health contains a number of examples of infectious diseases that were initially thought to have had a very high CFR only for it to be revised downward later. Lassa fever was initially described as a very severe disease, with a CFR close to 100%. However, as more widespread epidemiological studies were undertaken in West Africa, it was found that 50% or more of the population of Sierra Leone and Guinea were seropositive to the disease without showing any symptoms. 8 Under these circumstances, the CFR for Lassa virus is now thought to be low (<1%), but the CFR for severe disease remains very high.
Definitions (Some Terms in the Epidemiology)
When assessing the likely impact of an infectious disease, there are two parameters that are considered: the likelihood of transmission of the disease (its capacity to spread), and the severity of the disease and its capacity to kill (or disable) those infected. These are assessed using the reproduction rate and the CFR.
Reproduction rate ( R 0 ): The base reproduction number ( R 0 ) for transmission indicates the number of secondary infections due to an initial case ( R 0 = virgin state, a population with no previous exposure to this infection 9 ). In populations that have previously been exposed to the infection, and have some immunity, the reproduction rate may be lower.
Case fatality rate is defined as the proportion of reported cases of a specified disease that are fatal within a specified time. 10 The CFR depends on the definition of disease, the accuracy of diagnosis (case detection), and the availability of treatment.
Transmissibility and severity are the two most critical factors that determine the public health impact of an epidemic. 11 A disease that has a high transmission rate and is very severe is the greatest public health risk. COVID-19 has a high transmission rate, and the CFR appears to be greater than for influenza epidemics, and it is, therefore, potentially a major public health threat.
Infectivity is the tendency to spread the infection from host to host. The period of infectivity for some diseases commences before symptoms appear, making it far more difficult to control spread.
The spectrum of clinical disease (see Figure 1 ) makes it difficult to define a case and even more difficult to calculate a CFR, as the denominator is not readily defined. In February, the CFR for COVID-19 infection was estimated by the World Health Organization (WHO) to be 2%, much lower than for MERS and SARS, but estimates of the CFR have changed over time as the criteria for counting the number of cases in the denominator has changed to include very mild or even asymptomatic infections. 12 Changes in the denominator decrease the CFR and increase the reproducibility rate. In some situations, the reproducibility rate changes and the quarantine of passengers on a cruise ship in Yokohama had a R 0 4 times greater (as high as 14) compared with the initial R 0 in Wuhan. 9
The use of diagnostic tests has traditionally been reported using measures of sensitivity (proportion of true positives that are correctly identified by the test) and specificity (proportion of true negatives that are correctly identified by the test). 13 At the present time, COVID-19 disease is diagnosed by detecting the virus in throat and nasal swabs in patients who have symptoms of an upper respiratory tract infection who have been in a region with disease transmission. No other screening tests are yet available, and in the absence of “gold standard” for diagnosis, these parameters are not yet being calculated.
Incubation period is the time between exposure to an infectious agent and the appearance of clinical symptoms (or physiological evidence of disease). It is not known if transmission of the virus occurs during this period and before the presence of clinical symptoms. The WHO estimates of the incubation period for COVID-19 range from 1 to 14 days, most commonly around 5 days. Modeling of the role of contact tracing and case isolation suggest that these are effective in the control of epidemics such as COVID-19. 14 In Australia, the home isolation (quarantine) of contacts or suspected cases is recommended for 14 days. 15 If transmission is occurring before symptoms appear, it makes it more difficult to control an infectious disease.
The virus is contained in droplets from coughing and nasal secretions. It can survive up to 24 hours on surfaces under favorable conditions. Most transmission will occur through spread by hands and not from the direct inhalation of droplets. The WHO recommends the following to prevent transmission of the virus:
Regularly and thoroughly clean your hands with an alcohol-based hand rub or wash them with soap and water.
Maintain at least 1 m distance between yourself and others, and in particular from anyone who is coughing or sneezing.
Avoid touching eyes, nose, and mouth.
Make sure you, and the people around you, follow good respiratory hygiene. This means covering your mouth and nose with your bent elbow or tissue when you cough or sneeze. Then dispose of the used tissue immediately.
Stay at home if you feel unwell. If you have a fever, cough, and difficulty breathing, seek medical attention and call in advance. Follow the directions of your local health authority. 16
Vaccine Development
Despite much research and success in some animal models, including primates, there is still no vaccine for SARS. The first clinical cases of SARS were noted in November 2002, but it was not until 5 months later that a causative agent was isolated. 17 Transmission and dispersion around the world occurred by respiratory aerosols and contact via hands, and in several cases, this was from touching door handles. There were 8098 reported cases of SARS and 774 deaths from many different countries. 18 While there is no doubt that the virus has the potential to reemerge at present, it is not a clinical issue at present. SARS has a lower transmissibility than COVID-19.
The development, testing, and mass production of vaccines is always time-consuming before they can be deployed on a population-wide scale. The development, testing, and distribution of a vaccine will take years. Despite the interest in SARS, there is still no vaccine, and in other cases, important diseases have defied vaccine development, notably malaria and dengue.
Seasonality
Will COVID-19 decline in the northern summer following the pattern of influenza? This may be because people are more likely to have closer contact with others because it is colder. It could also relate to relative humidity levels that are lower in winter. In Western countries, when it is cooler in winter, respiratory infections increase (e.g. influenza). However, this seasonality does not apply to influenza in India. 19 A study of a new strain of influenza in Vietnam shows that in the early years of this variant, there was significant transmission throughout the first year and the usual seasonal transmission pattern evolved a few years later. 20 In Australia, it is summer and hot, and the COVID-19 is spreading here. This suggests that COVID-19 transmission may not be related to climatic conditions and may not be seasonal in its early year(s) as the population is being exposed for the first time.
Smallpox as an Example of the Role of Epidemiology in Disease Control
The history of smallpox elimination provides an example of the role of epidemiology in defeating an infectious disease. The practice of variolation to prevent smallpox had been in existence for several centuries, particularly in the Middle East, before Edward Jenner popularized the process and published his paper on the topic. 21 Vaccination against smallpox developed for almost 2 centuries before the disease was certified as being eliminated in 1980. 22 What was needed was a thorough understanding of the epidemiology of the disease. By studying seasonal variation and transmission within an infection cluster, it was shown that with vaccination of perhaps 5% of the population, the immediate case contacts was just as effective as vaccinating 100% of the population. 23 Understanding the epidemiology of outbreaks proved to be the effective way of eliminating the disease. 24 Recording all of the details of the COVID-19 outbreak is basic to understanding its epidemiology and the natural history of the disease and could provide the key to defeating the disease outbreak.
Health Ethics
There are several ethical issues that have already been raised in this outbreak. The importance of preserving the physical and mental health and availability of health workers in an epidemic situation is very important. The quality of health care depends almost entirely on them having a professional service ethic that motivates them to provide the highest quality care to all with the resources available to them. 25 This often leads them to put their own health and safety at risk, especially in infectious disease outbreaks. After the SARS outbreak of 2003 that caused illness and deaths among health workers, the ethics of exposing staff to the disease was still being debated in 2019. 26 The history of public health is full of the writings of the heroism of health workers providing care to those in need, despite endangering themselves. 27 However, experience has shown that risks associated with outbreaks of life-threatening infections only receive attention after health workers have suffered serious adverse consequences. Institutions need to prepare for outbreaks and provide the best available protective equipment to their workers and volunteers.
A further ethical issue is the development of vaccines. If this proves possible, it will take several years to develop, test, and submit for approval. Then issues of distribution and cost will need to be finalized. Professor Jeffrey Sachs, health economist, public health advocate, and former advisor to the Secretary General of the United Nations for the development of the Sustainable Development Goals, has written an editorial on the development of a vaccine for COVID-19. 28 Sachs states that in earlier public health emergencies, governments, nonprofit foundations, and international organizations took the lead in the development of preventive measures and made the vaccine or knowledge available freely. Sachs discusses the example of Jonas Salk who did not patent the polio vaccine, making it affordable to programs all over the world. However, in the case of COVID-19, the present US administration is stating that commercial companies will develop the vaccine and its availability will depend on the market. Will the profits of multinational companies come before the survival of the poor in lower income countries 28 ?
Public Health Actions
Reducing the peak of new cases by slowing down the spread of new cases is very useful as it
Reduces the load on diagnostic and treatment services
Reduces the number of health workers who contact the disease and who can continue working
If the epidemic curve can be smoothed, it will result in a lower overall disease burden
There are examples from the historical control of epidemics using public health measures that may be applied to COVID-19. An analysis of records from 17 cities in the United States during the 1918 influenza pandemic shows that cities that implemented public health measures (isolation, banning meetings, etc) were successful in reducing epidemic peaks and overall mortality. 29 This was in a naive population not previously exposed to this virus. Hatchett et al documented the substantial differences between St. Louis (which banned mass gatherings) and the higher death rates in Philadelphia, which allowed the massed celebratory marches following World War I to proceed. 29
Useful public health interventions to reduce the peak of new cases include the following:
Personal hygiene : no handshaking, no direct physical contact with others, keeping 1 m distance from others, no coughing in public, do not touch your face, wash hands frequently with soap and water, and eat cooked food that is still hot. These measures require clean water supplies (also important for nutrition and food safety)
Reducing person to person contact by banning public gatherings, closing schools, home quarantining, controlling public transport, and so on, has been effective, but disruptive, in some communities
Isolation of cases and quarantine (usually self-quarantine) of contacts.
There is more information on the WHO and Centers for Disease Control and Prevention websites. 2 , 3
In their modeling, Hellewell et al suggest that isolation of cases and tracing of contacts may be successful in controlling an outbreak within 3 months. 14 In the current global situation, it appears that some countries have been able to slow the epidemic while others have been overwhelmed by peaks of cases.
Universities are presented with major challenges to manage the COVID-19 epidemic. They are gathering places for thousands of young adults and academics who are usually older and are more vulnerable to complications. Obviously, large gatherings should be avoided and wider use be made of online teaching and tutorials. On campus, the usual precautions of avoiding contact, keeping distance, and frequent handwashing should apply. Within the memory of one of us (CB), these personal precautions were applied with success to polio, influenza, and hepatitis. We hope that these precautions will lead to a containment of the epidemic allowing time to continue development and clinical trials of a vaccine.
The emergence of COVID-19 is a serious global public health problem. The future direction of the epidemic is unknown. The size of the outbreak will depend on reducing transmission, which at the present time means using traditional public health measures. These include contact tracing and quarantine of cases, or sometimes the quarantine of localities. Modeling suggests that these measures may be effective. Health promotion programs should emphasize avoiding crowds, handwashing and hygiene, and extensive testing of at-risk persons. Vaccine development is a slow process, and it will be a year(s) before it can become a component of public health interventions.
Schools of Public Health and Research Institute members of APACPH are actively involved in basic research, epidemiology of outbreaks, and health promotion. This journal welcomes submissions that document the outbreak and contribute to the control of the disease.
Dear readers,
For the next few issues, we will publish a selection of letters and short papers that we are receiving on the COVID-19 epidemic. In this day and age, there are more rapid means of communication, but the printed word remains unsurpassed as long-term record of what has happened. For our journal, the teaching of public health undergraduate and postgraduate students is important, and this will be a useful resource.
The Editors
- 1. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497-506. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 2. World Health Organization. WHO Director-General’s opening remarks at the media briefing on COVID. Published March 5, 2020. Accessed May 6, 2020 https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19—5-march-2020
- 3. Centers for Disease Control and Prevention. Coronavirus disease 2019 (COVID-19). Symptoms of coronavirus. Accessed March 6, 2020 https://www.cdc.gov/coronavirus/2019-ncov/about/symptoms.html
- 4. The Novel Coronavirus Pneumonia Emergency Response Epidemiology Team. Vital Surveillances: the epidemiological characteristics of an outbreak of 2019 Novel coronavirus diseases (COVID-19)—China, 2020. China CDC Weekly. 2020;2:113-122. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 5. Center for Disease Control and Prevention. Disease of the week. Common cold. Accessed March 9, 2020 https://www.cdc.gov/dotw/common-cold/
- 6. Binns C, Low WY. Remembering Gustav Klimt and 50 million others: the 100 year anniversary of the greatest human epidemic. Asia Pac J Public Health. 2018;30:412-414. [ DOI ] [ PubMed ] [ Google Scholar ]
- 7. Dorigatti I, Okell L, Cori A, et al. ; MRC Centre for Global Infectious Disease Analysis. Report 4: Severity of 2019-novel coronavirus (nCoV). Accessed March 6, 2020 https://www.imperial.ac.uk/mrc-global-infectious-disease-analysis/covid-19/report-4-severity-of-covid-19/
- 8. Richmond JK, Baglole DJ. Lassa fever: epidemiology, clinical features, and social consequences. BMJ. 2003;327:1271-1275. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 9. Rocklöv J, Sjödin H, Wilder-Smith A. COVID-19 outbreak on the Diamond Princess cruise ship: estimating the epidemic potential and effectiveness of public health countermeasures. Preprint. Posted online February 28, 2020. J Travel Med. doi: 10.1093/jtm/taaa030 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 10. World Health Organization. Cholera case fatality rate. Accessed March 8, 2020 https://www.who.int/gho/epidemic_diseases/cholera/case_fatality_rate_text/en/
- 11. Swerdlow DL, Finelli L. Preparation for possible sustained transmission of 2019 novel coronavirus: lessons from previous epidemics. JAMA. 2020;323:1129-1130. [ DOI ] [ PubMed ] [ Google Scholar ]
- 12. Mahase E. Coronavirus: covid-19 has killed more people than SARS and MERS combined, despite lower case fatality rate. BMJ. 2020;368:m641. [ DOI ] [ PubMed ] [ Google Scholar ]
- 13. Altman DG, Bland JM. Diagnostic tests. 1: Sensitivity and specificity. BMJ. 1994;308:1552. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 14. Hellewell J, Abbott S, Gimma A, et al. Feasibility of controlling COVID-19 outbreaks by isolation of cases and contacts. Lancet Glob Health. 2020;8:e488-e496. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 15. Australian Government Department of Health. Coronavirus (COVID-19) health alert. Accessed March 9, 2020 https://www.health.gov.au/news/health-alerts/novel-coronavirus-2019-ncov-health-alert
- 16. World Health Organization. Coronavirus disease (COVID-19) advice for the public. Accessed March 14, 2020 https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public
- 17. Peiris JSM, Yuen KY, Osterhaus A, Stöhr K. The severe acute respiratory syndrome. N Engl J Med. 2003;349:2431-2441. [ DOI ] [ PubMed ] [ Google Scholar ]
- 18. Hui DSC, Zumla A. Severe acute respiratory syndrome: historical, epidemiologic, and clinical features. Infect Dis Clin North Am. 2019;33:869-889. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 19. Koul PA, Broor S, Saha S, et al. Differences in influenza seasonality by latitude, northern India. Emerg Infect Dis. 2014;20:1723-1726. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 20. Manabe T, Yamaoka K, Tango T, et al. Chronological, geographical, and seasonal trends of human cases of avian influenza A (H5N1) in Vietnam, 2003-2014: a spatial analysis. BMC Infect Dis. 2016;16:64. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 21. Riedel S. Edward Jenner and the history of smallpox and vaccination. Proc (Bayl Univ Med Cent). 2005;18:21-25. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 22. Binns C, Low WY. Infections and public health: who will win? Asia Pac J Public Health. 2014;26:4-6. [ DOI ] [ PubMed ] [ Google Scholar ]
- 23. Mack TM, Thomas DB, Khan MM. Epidemiology of smallpox in west-Pakistan. II. Determinants of intravillage spread other than acquired immunity. Am J Epidemiol. 1972;95:169-177. [ DOI ] [ PubMed ] [ Google Scholar ]
- 24. Hopkins DR. Smallpox: ten years gone. Am J Public Health. 1988;78:1589-1595. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 25. Segall M. From cooperation to competition in national health systems—and back? Impact on professional ethics and quality of care. Int J Health Plann Manage. 2000;15:61-79. [ DOI ] [ PubMed ] [ Google Scholar ]
- 26. Millar M, Hsu DTS. Can healthcare workers reasonably question the duty to care whilst healthcare institutions take a reactive (rather than proactive) approach to infectious disease risks? Public Health Ethics. 2019;12:94-98. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 27. Pawlikowski J, Banasiuk J, Sak J, Jojczuk M, Grzybowski A. Damien de Veuster (1840-1889): a life devoted to lepers. Clin Dermatol. 2018;36:680-685. [ DOI ] [ PubMed ] [ Google Scholar ]
- 28. Sachs J. The Trump administration’s ludicrous approach to coronavirus vaccine. Updated March 5, 2020. Accessed March 8, 2020 https://edition.cnn.com/2020/03/05/opinions/ludicrous-plan-coronavirus-vaccine-opinion-sachs/index.html
- 29. Hatchett RJ, Mecher CE, Lipsitch M. Public health interventions and epidemic intensity during the 1918 influenza pandemic. Proc Natl Acad Sci U S A. 2007;104:7582-7587. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- View on publisher site
- PDF (407.6 KB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections

IMAGES
VIDEO