What Works In Schools : Sexual Health Education
CDC’s What Works In Schools Program improves the health and well-being of middle and high school students by:
- Improving health education,
- Connecting young people to the health services they need, and
- Making school environments safer and more supportive.

What is sexual health education?
Quality provides students with the knowledge and skills to help them be healthy and avoid human immunodeficiency virus (HIV), sexually transmitted infections (STI) and unintended pregnancy.
A quality sexual health education curriculum includes medically accurate, developmentally appropriate, and culturally relevant content and skills that target key behavioral outcomes and promote healthy sexual development. 1
The curriculum is age-appropriate and planned across grade levels to provide information about health risk behaviors and experiences.

Sexual health education should be consistent with scientific research and best practices; reflect the diversity of student experiences and identities; and align with school, family, and community priorities.
Quality sexual health education programs share many characteristics. 2-4 These programs:
- Are taught by well-qualified and highly-trained teachers and school staff
- Use strategies that are relevant and engaging for all students
- Address the health needs of all students, including the students identifying as lesbian, gay, bisexual, transgender, queer and questioning (LGBTQ)
- Connect students to sexual health and other health services at school or in the community
- Engage parents, families, and community partners in school programs
- Foster positive relationships between adolescents and important adults.
How can schools deliver sexual health education?
A school health education program that includes a quality sexual health education curriculum targets the development of functional knowledge and skills needed to promote healthy behaviors and avoid risks. It is important that sexual health education explicitly incorporate and reinforce skill development.
Giving students time to practice, assess, and reflect on skills taught in the curriculum helps move them toward independence, critical thinking, and problem solving to avoid STIs, HIV, and unintended pregnancy. 5
Quality sexual health education programs teach students how to: 1
- Analyze family, peer, and media influences that impact health
- Access valid and reliable health information, products, and services (e.g., STI/HIV testing)
- Communicate with family, peers, and teachers about issues that affect health
- Make informed and thoughtful decisions about their health
- Take responsibility for themselves and others to improve their health.
What are the benefits of delivering sexual health education to students?
Promoting and implementing well-designed sexual health education positively impacts student health in a variety of ways. Students who participate in these programs are more likely to: 6-11
- Delay initiation of sexual intercourse
- Have fewer sex partners
- Have fewer experiences of unprotected sex
- Increase their use of protection, specifically condoms
- Improve their academic performance.
In addition to providing knowledge and skills to address sexual behavior , quality sexual health education can be tailored to include information on high-risk substance use * , suicide prevention, and how to keep students from committing or being victims of violence—behaviors and experiences that place youth at risk for poor physical and mental health and poor academic outcomes.
*High-risk substance use is any use by adolescents of substances with a high risk of adverse outcomes (i.e., injury, criminal justice involvement, school dropout, loss of life). This includes misuse of prescription drugs, use of illicit drugs (i.e., cocaine, heroin, methamphetamines, inhalants, hallucinogens, or ecstasy), and use of injection drugs (i.e., drugs that have a high risk of infection of blood-borne diseases such as HIV and hepatitis).
What does delivering sexual health education look like in action?
To successfully put quality sexual health education into practice, schools need supportive policies, appropriate content, trained staff, and engaged parents and communities.
Schools can put these four elements in place to support sex ed.
- Implement policies that foster supportive environments for sexual health education.
- Use health content that is medically accurate, developmentally appropriate, culturally inclusive, and grounded in science.
- Equip staff with the knowledge and skills needed to deliver sexual health education.
- Engage parents and community partners.
Include enough time during professional development and training for teachers to practice and reflect on what they learned (essential knowledge and skills) to support their sexual health education instruction.
By law, if your school district or school is receiving federal HIV prevention funding, you will need an HIV Materials Review Panel (HIV MRP) to review all HIV-related educational and informational materials.
This review panel can include members from your School Health Advisory Councils, as shared expertise can strengthen material review and decision making.
For More Information
Learn more about delivering quality sexual health education in the Program Guidance .
Check out CDC’s tools and resources below to develop, select, or revise SHE curricula.
- Health Education Curriculum Analysis Tool (HECAT), Module 6: Sexual Health [PDF – 70 pages] . This module within CDC’s HECAT includes the knowledge, skills, and health behavior outcomes specifically aligned to sexual health education. School and community leaders can use this module to develop, select, or revise SHE curricula and instruction.
- Developing a Scope and Sequence for Sexual Health Education [PDF – 17 pages] .This resource provides an 11-step process to help schools outline the key sexual health topics and concepts (scope), and the logical progression of essential health knowledge, skills, and behaviors to be addressed at each grade level (sequence) from pre-kindergarten through the 12th grade. A developmental scope and sequence is essential to developing, selecting, or revising SHE curricula.
- Centers for Disease Control and Prevention. Health Education Curriculum Analysis Tool, 2021 , Atlanta: CDC; 2021.
- Goldfarb, E. S., & Lieberman, L. D. (2021). Three decades of research: The case for comprehensive sex education. Journal of Adolescent Health, 68(1), 13-27.
- Centers for Disease Control and Prevention (2016). Characteristics of an Effective Health Education Curriculum .
- Pampati, S., Johns, M. M., Szucs, L. E., Bishop, M. D., Mallory, A. B., Barrios, L. C., & Russell, S. T. (2021). Sexual and gender minority youth and sexual health education: A systematic mapping review of the literature. Journal of Adolescent Health , 68 (6), 1040-1052.
- Szucs, L. E., Demissie, Z., Steiner, R. J., Brener, N. D., Lindberg, L., Young, E., & Rasberry, C. N. (2023). Trends in the teaching of sexual and reproductive health topics and skills in required courses in secondary schools, in 38 US states between 2008 and 2018. Health Education Research , 38 (1), 84-94.
- Coyle, K., Anderson, P., Laris, B. A., Barrett, M., Unti, T., & Baumler, E. (2021). A group randomized trial evaluating high school FLASH, a comprehensive sexual health curriculum. Journal of Adolescent Health , 68 (4), 686-695.
- Marseille, E., Mirzazadeh, A., Biggs, M. A., Miller, A. P., Horvath, H., Lightfoot, M.,& Kahn, J. G. (2018). Effectiveness of school-based teen pregnancy prevention programs in the USA: A systematic review and meta-analysis. Prevention Science, 19(4), 468-489.
- Denford, S., Abraham, C., Campbell, R., & Busse, H. (2017). A comprehensive review of reviews of school-based interventions to improve sexual-health. Health psychology review, 11(1), 33-52.
- Chin HB, Sipe TA, Elder R. The effectiveness of group-based comprehensive risk-reduction and abstinence education interventions to prevent or reduce the risk of adolescent pregnancy, human immunodeficiency virus, and sexually transmitted infections: Two systematic reviews for the guide to community preventive services. Am J Prev Med 2012;42(3):272–94.
- Mavedzenge SN, Luecke E, Ross DA. Effective approaches for programming to reduce adolescent vulnerability to HIV infection, HIV risk, and HIV-related morbidity and mortality: A systematic review of systematic reviews. J Acquir Immune Defic Syndr 2014;66:S154–69.
To receive email updates about this page, enter your email address:
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
Internet Explorer Alert
It appears you are using Internet Explorer as your web browser. Please note, Internet Explorer is no longer up-to-date and can cause problems in how this website functions This site functions best using the latest versions of any of the following browsers: Edge, Firefox, Chrome, Opera, or Safari . You can find the latest versions of these browsers at https://browsehappy.com
- Publications
- HealthyChildren.org
Shopping cart
Order Subtotal
Your cart is empty.
Looks like you haven't added anything to your cart.
- Career Resources
- Philanthropy
- About the AAP
- Confidentiality in the Care of Adolescents: Policy Statement
- Confidentiality in the Care of Adolescents: Technical Report
- AAP Policy Offers Recommendations to Safeguard Teens’ Health Information
- One-on-One Time with the Pediatrician
- American Academy of Pediatrics Releases Guidance on Maintaining Confidentiality in Care of Adolescents
- News Releases
- Policy Collections
- The State of Children in 2020
- Healthy Children
- Secure Families
- Strong Communities
- A Leading Nation for Youth
- Transition Plan: Advancing Child Health in the Biden-Harris Administration
- Health Care Access & Coverage
- Immigrant Child Health
- Gun Violence Prevention
- Tobacco & E-Cigarettes
- Child Nutrition
- Assault Weapons Bans
- Childhood Immunizations
- E-Cigarette and Tobacco Products
- Children’s Health Care Coverage Fact Sheets
- Opioid Fact Sheets
- Advocacy Training Modules
- Subspecialty Advocacy Report
- AAP Washington Office Internship
- Online Courses
- Live and Virtual Activities
- National Conference and Exhibition
- Prep®- Pediatric Review and Education Programs
- Journals and Publications
- NRP LMS Login
- Patient Care
- Practice Management
- AAP Committees
- AAP Councils
- AAP Sections
- Volunteer Network
- Join a Chapter
- Chapter Websites
- Chapter Executive Directors
- District Map
- Create Account
- Early Relational Health
- Early Childhood Health & Development
- Safe Storage of Firearms
- Promoting Firearm Injury Prevention
- Mental Health Education & Training
- Practice Tools & Resources
- Policies on Mental Health
- Mental Health Resources for Families
The Importance of Access to Comprehensive Sex Education
Comprehensive sex education is a critical component of sexual and reproductive health care.
Developing a healthy sexuality is a core developmental milestone for child and adolescent health.
Youth need developmentally appropriate information about their sexuality and how it relates to their bodies, community, culture, society, mental health, and relationships with family, peers, and romantic partners.
AAP supports broad access to comprehensive sex education, wherein all children and adolescents have access to developmentally appropriate, evidence-based education that provides the knowledge they need to:
- Develop a safe and positive view of sexuality.
- Build healthy relationships.
- Make informed, safe, positive choices about their sexuality and sexual health.
Comprehensive sex education involves teaching about all aspects of human sexuality, including:
- Cyber solicitation/bullying.
- Healthy sexual development.
- Body image.
- Sexual orientation.
- Gender identity.
- Pleasure from sex.
- Sexual abuse.
- Sexual behavior.
- Sexual reproduction.
- Sexually transmitted infections (STIs).
- Abstinence.
- Contraception.
- Interpersonal relationships.
- Reproductive coercion.
- Reproductive rights.
- Reproductive responsibilities.
Comprehensive sex education programs have several common elements:
- Utilize evidence-based, medically accurate curriculum that can be adapted for youth with disabilities.
- Employ developmentally appropriate information, learning strategies, teaching methods, and materials.
- Human development , including anatomy, puberty, body image, sexual orientation, and gender identity.
- Relationships , including families, peers, dating, marriage, and raising children.
- Personal skills , including values, decision making, communication, assertiveness, negotiation, and help-seeking.
- Sexual behavior , including abstinence, masturbation, shared sexual behavior, pleasure from esx, and sexual dysfunction across the lifespan.
- Sexual health , including contraception, pregnancy, prenatal care, abortion, STIs, HIV and AIDS, sexual abuse, assault, and violence.
- Society and culture , including gender roles, diversity, and the intersection of sexuality and the law, religion, media, and the arts.
- Create an opportunity for youth to question, explore, and assess both personal and societal attitudes around gender and sexuality.
- Focus on personal practices, skills, and behaviors for healthy relationships, including an explicit focus on communication, consent, refusal skills/accepting rejection, violence prevention, personal safety, decision making, and bystander intervention.
- Help youth exercise responsibility in sexual relationships.
- Include information on how to come forward if a student is being sexually abused.
- Address education from a trauma-informed, culturally responsive approach that bridges mental, emotional, and relational health.
Comprehensive sex education should occur across the developmental spectrum, beginning at early ages and continuing throughout childhood and adolescence :
- Sex education is most effective when it begins before the initiation of sexual activity.
- Young children can understand concepts related to bodies, gender, and relationships.
- Sex education programs should build an early foundation and scaffold learning with developmentally appropriate content across grade levels.
- AAP Policy outlines considerations for providing developmentally appropriate sex education throughout early childhood, middle childhood, adolescence, and young adulthood.
Most adolescents report receiving some type of formal sex education before age 18. While sex education is typically associated with schools, comprehensive sex education can be delivered in several complementary settings:
- Schools can implement comprehensive sex education curriculum across all grade levels
- The Sexuality Information and Education Council of the United States (SIECUS) provides guidelines for providing developmentally appropriate comprehensive sex education across grades K-12.
- Pediatric health clinicians and other health care providers are uniquely positioned to provide longitudinal sex education to children, adolescents, and young adults.
- Bright Futures: Guidelines for Health Supervision of Infants, Children, and Adolescents outlines clinical considerations for providing comprehensive sex education at all developmental stages, as a part of preventive health care.
- Research suggests that community-based organizations should be included as a source for comprehensive sexual health promotion.
- Faith-based communities have developed sex education curricula for their congregations or local chapters that emphasize the moral and ethical aspects of sexuality and decision-making.
- Parents and caregivers can serve as the primary sex educators for their children, by teaching fundamental lessons about bodies, development, gender, and relationships.
- Many factors impact the sex education that youth receive at home, including parent/caregiver knowledge, skills, comfort, culture, beliefs, and social norms.
- Virtual sex education can take away feelings of embarrassment or stigma and can allow for more youth to access high quality sex education.
Comprehensive sex education provides children and adolescents with the information that they need to:
- Understand their body, gender identity, and sexuality.
- Build and maintain healthy and safe relationships.
- Engage in healthy communication and decision-making around sex.
- Practice healthy sexual behavior.
- Understand and access care to support their sexual and reproductive health.
Comprehensive sex education programs have demonstrated success in reducing rates of sexual activity, sexual risk behaviors, STIs, and adolescent pregnancy and delaying sexual activity. Many systematic reviews of the literature have indicated that comprehensive sex education promotes healthy sexual behaviors:
- Reduced sexual activity.
- Reduced number of sexual partners.
- Reduced frequency of unprotected sex.
- Increased condom use.
- Increased contraceptive use.
However, comprehensive sex education curriculum goes beyond risk-reduction, by covering a broader range of content that has been shown to support social-emotional learning, positive communication skills, and development of healthy relationships.
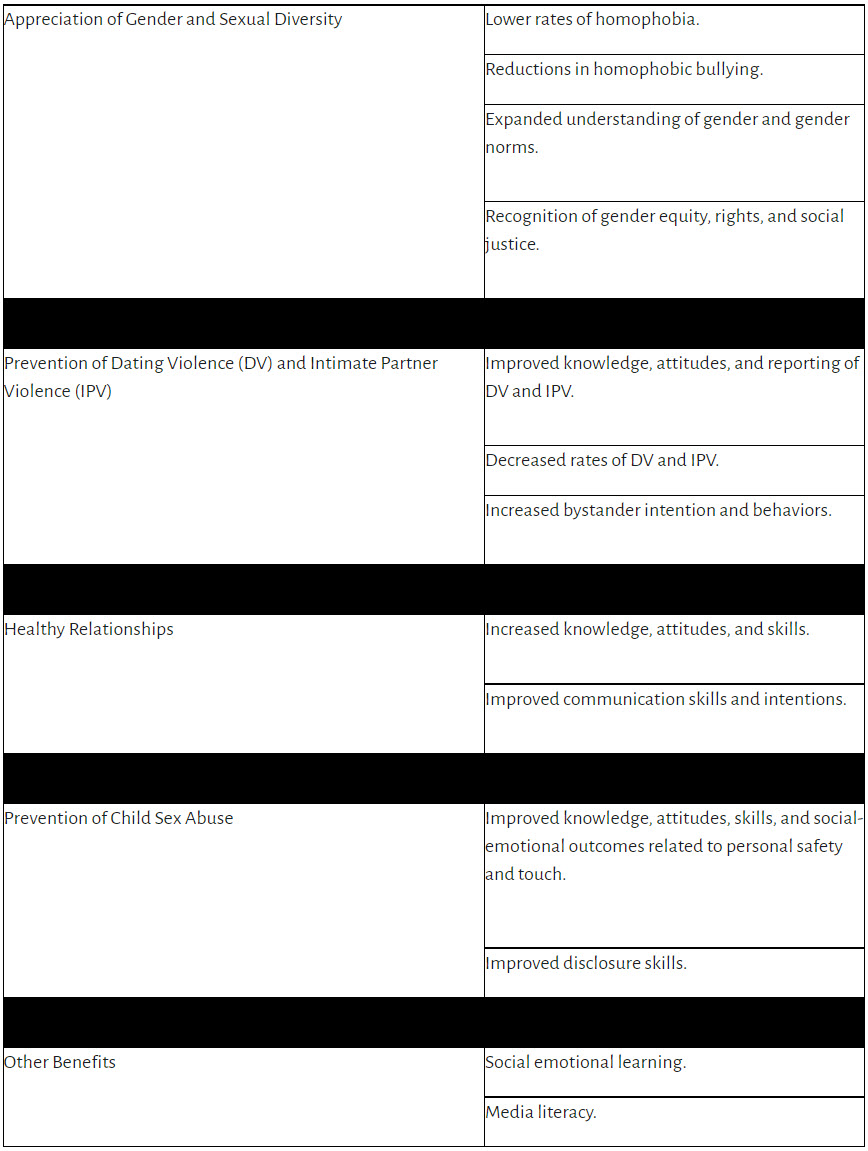
A 2021 review of the literature found that comprehensive sex education programs that use a positive, affirming, and inclusive approach to human sexuality are associated with concrete benefits across 5 key domains:
Benefits of comprehensive sex education programs
When children and adolescents lack access to comprehensive sex education, they do not get the information they need to make informed, healthy decisions about their lives, relationships, and behaviors.
Several trends in sexual health in the US highlight the need for comprehensive sex education for all youth.
Education about condom and contraceptive use is needed:
- 55% of US high school students report having sexual intercourse by age 18 .
- Self-reported condom use has decreased significantly among high school students.
- Only 9% of sexually active high school students report using both a condom for STI-prevention and a more effective form of birth control to prevent pregnancy .
STI prevention is needed:
- Adolescents and young adults are disproportionately impacted by STIs.
- Cases of chlamydia, gonorrhea, and syphilis are rising rapidly among young people.
- When left untreated , these infections can lead to infertility, adverse pregnancy and birth outcomes, and increased risk of acquiring new STIs.
- Youth need comprehensive, unbiased information about STI prevention, including human papillomavirus (HPV) .
Continued prevention of unintended pregnancy is needed:
- Overall US birth rates among adolescent mothers have declined over the last 3 decades.
- There are significant geographic disparities in adolescent pregnancy rates, with higher rates of pregnancy in rural counties and in southern and southwestern states.
- Social drivers of health and systemic inequities have caused racial and ethnic disparities in adolescent pregnancy rates.
- Eliminating disparities in adolescent pregnancy and birth rates can increase health equity, improve health and life outcomes, and reduce the economic impact of adolescent parenting.
Misinformation about sexual health is easily available online:
- Internet use is nearly universal among US children and adolescents.
- Adolescents report seeking sexual health information online .
- Sexual health websites that adolescents visit can contain inaccurate information .
Prevention of sex abuse, dating violence, and unhealthy relationships is needed:
- Child sexual abuse is common: 25% of girls and 8% of boys experience sexual abuse during childhood .
- Youth who experience sexual abuse have long-term impacts on their physical, mental, and behavioral health.
- 1 in 11 female and 1 in 14 male students report physical DV in the last year .
- 1 in 8 female and 1 in 26 male students report sexual DV in the last year .
- Youth who experience DV have higher rates of anxiety, depression, substance use, antisocial behaviors, and suicide risk.
The quality and content of sex education in US schools varies widely.
There is significant variation in the quality of sex education taught in US schools, leading to disparities in attitudes, health information, and outcomes. The majority of sex education programs in the US tend to focus on public health goals of decreasing unintended pregnancies and preventing STIs, via individual behavior change.
There are three primary categories of sex educational programs taught in the US :
- Abstinence-only education , which teaches that abstinence is expected until marriage and typically excludes information around the utility of contraception or condoms to prevent pregnancy and STIs.
- Abstinence-plus education , which promotes abstinence but includes information on contraception and condoms.
- Comprehensive sex education , which provides medically accurate, age-appropriate information around development, sexual behavior (including abstinence), healthy relationships, life and communication skills, sexual orientation, and gender identity.
State laws impact the curriculum covered in sex education programs. According to a report from the Guttmacher Institute :
- 26 US states and Washington DC mandate sex education and HIV education.
- 18 states require that sex education content be medically accurate.
- 39 states require that sex education programs provide information on abstinence.
- 20 states require that sex education programs provide information on contraception.
US states have varying requirements on sex education content related to sexual orientation :
- 10 states require sex education curriculum to include affirming content on LGBTQ2S+ identities or discussion of sexual health for youth who are LGBTQ2S+.
- 7 states have sex education curricular requirements that discriminate against individuals who are LGBTQ2S+.Youth who live in these states may face additional barriers to accessing sexual health information.
Abstinence-only sex education programs do not meet the needs of children and adolescents.
While abstinence is 100% effective in preventing pregnancy and STIs, research has conclusively shown that abstinence-only sex education programs do not support healthy sexual development in youth.
Abstinence-only programs are ineffective in reaching their stated goals, as evidenced by the data below:
- Abstinence-only programs are unsuccessful in delaying sex until marriage .
- Abstinence-only sex education programs do not impact the rates of pregnancy, STIs, or HIV in adolescents .
- Youth who take a “virginity pledge” as part of abstinence-only education programs have the same rates of premarital sex as their peers who do not take pledges, but are less likely to use contraceptives .
- US states that emphasize abstinence-only education have higher rates of adolescent pregnancy and birth .
Abstinence-only programs can harm the healthy sexual and mental development of youth by:
- Withholding information or providing inaccurate information about sexuality and sexual behavior .
- Contributing to fear, shame, and stigma around sexual behaviors .
- Not sharing information on contraception and barrier protection or overstating the risks of contraception .
- Utilizing heteronormative framing and stigma or discrimination against students who are LGBTQ2S+ .
- Reinforcing harmful gender stereotypes .
- Ignoring the needs of youth who are already sexually active by withholding education around contraception and STI prevention.
Abstinence-plus sex education programs focus solely on decreasing unintended pregnancy and STIs.
Abstinence-plus sex education programs promote abstinence until marriage. However, these programs also provide information on contraception and condom use to prevent unintended pregnancy and STIs.
Research has demonstrated that abstinence-plus programs have an impact on sexual behavior and safety, including:
- HIV prevention.
- Increase in condom use .
- Reduction in number of sexual partners .
- Delay in initiation of sexual behavior .
While these programs add another layer of education, they do not address the broader spectrum of sexuality, gender identity, and relationship skills, thus withholding critical information and skill-building that can impact healthy sexual development.
AAP and other national medical and public health associations support comprehensive sex education for youth.
Given the evidence outlined above, AAP and other national medical organizations oppose abstinence-only education and endorse comprehensive sex education that includes both abstinence promotion and provision of accurate information about contraception, STIs, and sexuality.
National medical and public health organizations supporting comprehensive sex education include:
- American Academy of Pediatrics .
- American Academy of Family Physicians.
- American College of Obstetricians and Gynecologists .
- American Medical Association .
- American Public Health Association .
- Society for Adolescent Health and Medicine .
Pediatric clinics provide a unique opportunity for comprehensive sex education.
Pediatric health clinicians typically have longitudinal care relationships with their patients and families, and thus have unique opportunities to address comprehensive sex education across all stages of development.
The clinical visit can serve as a useful adjunct to support comprehensive sex education provided in schools, or to fill gaps in knowledge for youth who are exposed to abstinence-only or abstinence-plus curricula.
AAP policy and Bright Futures: Guidelines for Health Supervision of Infants, Children, and Adolescents provide recommendations for comprehensive sex education in clinical settings, including:
- Encouraging parent-child discussions on sexuality, contraception, and internet/media use.
- Understanding diverse experiences and beliefs related to sexuality and sex education and meeting the unique needs of individual patients and families.
- Including discussions around healthy relationships, dating violence, and intimate partner violence in clinical care.
- Discussing methods of contraception and STI/HPV prevention prior to onset of sexual intercourse.
- Providing proactive and developmentally appropriate sex education to all youth, including children and adolescents with special health care needs.
Perspective

Karen Torres, Youth activist
There were two cardboard bears, and a person explained that one bear wears a bikini to the beach and the other bear wears shorts – that is the closest thing I ever got to sex ed throughout my entire K-12 education. I often think about that bear lesson because it was the day our institutions failed to teach me anything about my body, relationships, consent, and self-advocacy, which became even more evident after I was sexually assaulted at 16 years old. My story is not unique, I know that many young people have been through similar traumas, but many of us were also subjected to days, months, and years of silence and embarrassment because we were never given the knowledge to know how to spot abuse or the language to ask for help. Comprehensive sex ed is so much more than people make it out to be, it teaches about sex but also about different types of experiences, how to respect one another, how to communicate in uncomfortable situations, how to ask for help and an insurmountable amount of other valuable lessons.
From these lessons, people become well-rounded, people become more empathetic to other experiences, and people become better. I believe comprehensive sex ed is vital to all people and would eventually work as a part to build more compassionate communities.
Many US children and adolescents do not receive comprehensive sex education; and rates of formal sex education have declined significantly in recent decades.
Barriers to accessing comprehensive sex education include:
Misinformation, stigma, and fear of negative reactions:
- Misinformation and stigma about the content of sex education curriculum has been the primary barrier to equitable access to comprehensive sex education in schools for decades .
- Despite widespread parental support for sex education in schools, fears of negative public/parent reactions have led school administrators to limit youth access to the information they need to make healthy decisions about their sexuality for nearly a half-century.
- In recent years, misinformation campaigns have spread false information about the framing and content of comprehensive sex education programs, causing debates and polarization at school board meetings .
- Nearly half of sex education teachers report that concerns about parent, student, or administrator responses are a barrier to provision of comprehensive sex education.
- Opponents of comprehensive sex education often express concern that this education will lead youth to have sex; however, research has demonstrated that this is not the case . Instead, comprehensive sex ed is associated with delays in initiation of sexual behavior, reduced frequency of sexual intercourse, a reduction in number of partners, and an increase in condom use.
- Some populations of youth lack access to comprehensive sex education due to a societal belief that they are asexual, in need of protection, or don’t need to learn about sex. This barrier particularly impacts youth with disabilities or special health care needs .
- Sex ed curricula in some schools perpetuate gender/sex stereotypes, which could contribute to negative gender stereotypes and negative attitudes towards sex .
Inconsistencies in school-based sex education:
- There is significant variation in the content of sex education taught in schools in the US, and many programs that carry the same label (eg, “abstinence-plus”) vary widely in curriculum.
- While decisions about sex education curriculum are made at the state level, the federal government has provided funding to support abstinence-only education for decades , which incentivizes schools to use these programs.
- Since 1996, more than $2 billion in federal funds have been spent to support abstinence-only sex education in schools.
- 34 US states require schools to use abstinence-only curriculum or emphasize abstinence as the main way to avoid pregnancy and STIs.
- Only 16 US states require instruction on condoms or contraception.
- It is not standard to include information on how to come forward if a student is being sexually abused, and many schools do not have a process for disclosures made.
- Because of this, abstinence-only programs are commonly used in US schools, despite overwhelming evidence that they are ineffective in delaying sexual behavior until marriage, and withhold critical information that youth need for healthy sexual and relationship development.
Need for resources and training:
- Integration of comprehensive sex education into school curriculum requires financial resources to strengthen and expand evidence-based programs.
- Successful implementation of comprehensive sex education requires a trained workforce of teachers who can address the curriculum in age-appropriate ways for students in all grade-levels.
- Education, training, and technical assistance are needed to support pediatric health clinicians in addressing comprehensive sex education in clinical settings, as a complement to school-based education.
Lack of diversity and cultural awareness in curricula:
- A history of systemic racism, discrimination, and long-standing health, social and systemic inequities have created racial and ethnic disparities in access to sexual health services and representation in sex education materials. The legacy of intergenerational trauma in the medical system should be acknowledged in sex education curricula.
- Sex education curriculum is often centered on a white audience, and does not address or reflect the role of systemic racism in sexuality and development .
- Traditional abstinence-focused sex education programs have a heteronormative focus and do not address the unique needs of youth who are LGBTQ2S+ .
- Sex education programs often do not address reproductive body diversity, the needs of those with differences in sex development, and those who identify as intersex .
- Sex education programs often do not reflect the unique needs of youth with disabilities or special health care needs .
- Sex education programs are often not tailored to meet the religious considerations of faith communities.
- There is a need for sex education programs designed to help youth navigate sexual health and development in the context of their own culture and community .
Disparities in access to comprehensive sex education.
The barriers listed above limit access to comprehensive sex education in schools and communities. While these barriers impact youth across the US, there are some populations who are less likely to have access to comprehensive to sex education.
Youth who are LGBTQ2S+:
- Only 8% of students who are LGBTQ2S+ report having received sexual education that was inclusive .
- Students who are LGBTQ2S+ are 50% more likely than their peers who are heterosexual to report that sex education in their schools was not useful to them .
- Only 13% of youth who are bisexual+ and 10% of youth who are transgender and gender expansive report receiving sex education in schools that felt personally relevant.
- Only 20% of youth who are Black and LGBTQ2S+ and 13% of youth who are Latinx and LGBTQ2S+ report receiving sex education in schools that felt personally relevant.
- Only 10 US states require affirming content on LGBTQ2S+ relationships in sex education curriculum.
Youth with disabilities or special health care needs:
- Youth with disabilities or special health care needs have a particular need for comprehensive sex education, as these youth are less likely to learn about sex or sexuality form their parents , healthcare providers , or peer groups .
- In a national survey, only half of youth with disabilities report that they have participated in sex education .
- Typical sex education may not be sufficient for youth with Autism Spectrum Disorder, and special methods and curricula are necessary to match their needs .
- Lack the desire or maturity for romantic or sexual relationships.
- Are not subject to sexual abuse.
- Do not need sex education.
- Only 3 states explicitly include youth with disabilities within their sex education requirements.
Youth from historically underserved communities:
- Students who are Black in the US are more likely than students who are white to receive abstinence-only sex education , despite significant support from parents and students who are Black for comprehensive sex education.
- Youth who are Black and female are less likely than peers who are white to receive education about where to obtain birth control prior to initiating sexual activity.
- Youth who are Black and male and Hispanic are less likely than their peers who are white to receive formal education on STI prevention or contraception prior to initiating sexual activity.
- Youth who are Hispanic and female are less likely to receive instruction about waiting to have sex than youth of other ethnicities.
- Tribal health educators report challenges in identifying culturally relevant sex education curriculum for youth who are American Indian/Alaska Native.
- In a 2019 study, youth who were LGBTQ2S+ and Black, Latinx, or Asian reported receiving inadequate sex education due to feeling unrepresented, unsupported, stigmatized, or bullied.
- In survey research, many young adults who are Asian American report that they received inadequate sex education in school.
Youth from rural communities:
- Adolescents who live in rural communities have faced disproportionate declines in formal sex education over the past two decades, compared with peers in urban/suburban areas.
- Students who live in rural communities report that the sex education curriculum in their schools does not serve their needs .
Youth from communities and schools that are low-income:
- Data has shown an association between schools that are low-resource and lower adolescent sexual health knowledge, due to a combination of fewer school resources and higher poverty rates/associated unmet health needs in the student body.
- Youth with family incomes above 200% of the federal poverty line are more likely to receive education about STI prevention, contraception, and “saying no to sex,” than their peers below 200% of the poverty line.
Youth who receive sex education in some religious settings:
- Most adolescents who identify as female and who attended church-based sex education programs report instructions on waiting until marriage for sex, while few report receiving education about birth control.
- Young people who received sex education in religious schools report that education focused on the risks of sexual behavior (STIs, pregnancy) and religious guilt; leading to them feeling under-equipped to make informed decisions about sex and sexuality later in life.
- Youth and teachers from religious schools have identified a need for comprehensive sex education curriculum that is tailored to the needs of faith communities .
Youth who live in states that limit the topics that can be covered in sex education:
- Students who live in the 34 states that require sex education programs to stress abstinence are less likely to have access to critical information on STI prevention and contraception.
- Prohibitions on addressing abortion in sex education or mandates that sex education curricula include medically inaccurate information on abortion designed to dissuade youth from terminating a pregnancy.
- Limitations on the types of contraception that can be covered in sex education curricula.
- Requirements that sex education teachers promote heterosexual, monogamous marriage in sex education.
- Lack of requirements to address healthy relationships and communication skills.
- Lack of requirements for teacher training or certification.
Comprehensive sex education has significant benefits for children and adolescents.
Youth who are exposed to comprehensive sex education programs in school demonstrate healthier sexual behaviors:
- Increased rates of contraception and condom use.
- Fewer unplanned pregnancies.
- Lower rates of STIs and HIV.
- Delayed initiation of sexual behavior.
More broadly, comprehensive sexual education impacts overall social-emotional health , including:
- Enhanced understanding of gender and sexuality.
- Lower rates of homophobia and related bullying.
- Lower rates of dating violence, intimate partner violence, sexual assault, and child sexual abuse.
- Healthier relationships and communication skills.
- Understanding of reproductive rights and responsibilities.
- Improved social-emotional learning, media literacy, and academic achievement.
Comprehensive sex education curriculum goes beyond risk reduction, to ensure that youth are supported in understanding their identity and sexuality and making informed decisions about their relationships, behaviors, and future. These benefits are critical to healthy sexual development.
Impacts of a lack of access to comprehensive sex education.
When youth are denied access to comprehensive sex education, they do not get the information and skill-building required for healthy sexual development. As such, they face unnecessary barriers to understanding their gender and sexuality, building positive interpersonal relationships, and making informed decisions about their sexual behavior and sexual health.
Impacts of a lack of comprehensive sex education for all youth can include :
- Less use of condoms, leading to higher risk of STIs, including HIV.
- Less use of contraception, leading to higher risk of unplanned pregnancy.
- Less understanding and increased stigma and shame around the spectrum of gender and sexual identity.
- Perpetuated stigma and embarrassment related to sex and sexual identity.
- Perpetuated gender stereotypes and traditional gender roles.
- Higher rates of youth turning to unreliable sources for information about sex, including the internet, the media, and informal learning from peer networks.
- Challenges in interpersonal communication.
- Challenges in building, maintaining, and recognizing safe, healthy peer and romantic relationships.
- Lower understanding of the importance of obtaining and giving enthusiastic consent prior to sexual activity.
- Less awareness of appropriate/inappropriate touch and lower reporting of child sexual abuse.
- Higher rates of dating violence and intimate partner violence, and less intervention from bystanders.
- Higher rates of homophobia and homophobic bullying.
- Unsafe school environments.
- Lower rates of media literacy.
- Lower rates of social-emotional learning.
- Lower recognition of gender equity, rights, and social justice.
In addition, the lack of access to comprehensive sex education can exacerbate existing health disparities, with disproportionate impacts on specific populations of youth.
Youth who identify as women, youth from communities of color, youth with disabilities, and youth who are LGBTQ2S+ are particularly impacted by inequitable access to comprehensive sex education, as this lack of education can impact their health, safety, and self-identity. Examples of these impacts are outlined below.
A lack of comprehensive sex education can harm young women.
- Female bodies are more prone to STI infection and more likely to experience complications of STI infection than male bodies.
- Female bodies are disproportionately impacted by long-term health consequences of STIs , including pelvic inflammatory disease, infertility, and ectopic pregnancy.
- Female bodies are less likely to have or recognize symptoms of certain STI infections .
- Human papillomavirus (HPV) is the most common STI in young women , and can cause long-term health consequences such as genital warts and cervical cancer.
- Women bear the health and economic effects of unplanned pregnancy.
- Comprehensive sex education addresses these issues by providing medically-accurate, evidence based information on effective strategies to prevent STI infections and unplanned pregnancy.
- Students who identify as female are more likely to experience sexual or physical dating violence than their peers who identify as male. Some of this may be attributed to underreporting by males due to stigma.
- Students who identify as female are bullied on school property more often than students who identify as male.
- Young women ages 16-19 are at higher risk of rape, attempted rape, or sexual assault than the general population.
- Comprehensive sex education addresses these issues by guiding the development of healthy self-identities, challenging harmful gender norms, and building the skills required for respectful, equitable relationships.
A lack of comprehensive sex education can harm youth from communities of color.
- Youth of color benefit from seeing themselves represented in sex education curriculum.
- Sex education programs that use a framing of diversity, equity, rights, and social justice , informed by an understanding of systemic racism and discrimination, have been found to increase positive attitudes around reproductive rights in all students.
- There is a critical need for sex education programs that reflect youth’s cultural values and community .
- Comprehensive sex education can address these needs by developing curriculum that is inclusive of diverse communities, relationships, and cultures, so that youth see themselves represented in their education.
- Racial and ethnic disparities in STI and HIV infection.
- Racial and ethnic disparities in unplanned pregnancy and births among adolescents.
- Nearly half of youth who are Black ages 13-21 report having been pressured into sexual activity .
- Adolescent experience with dating violence is most prevalent among youth who are American Indian/Alaska Native, Native Hawaiian/Pacific Islander, and multiracial.
- Adolescents who are Latinx are more likely than their peers who are non-Latinx to report physical dating violence .
- Youth who are Black and Latinx and who experience bullying are more likely to suffer negative impacts on academic performance than their white peers.
- Students who are Asian American and Pacific Islander report bullying and harassment due to race, ethnicity, and language.
- Comprehensive sex education addresses these issues by guiding the development of healthy self-identities, challenging harmful stereotypes, and building the skills required for respectful, equitable relationships.
- Young people of color—specifically those from Black , Asian-American , and Latinx communities– are often hyper-sexualized in popular media, leading to societal perceptions that youth are “older” or more sexually experienced than their white peers.
- Young men of color—specifically those from Black and Latinx communities—are often portrayed as aggressive or criminal in popular media, leading to societal perceptions that youth are dangerous or more sexually aggressive or experienced than white peers.
- These media portrayals can lead to disparities in public perceptions of youth behavior , which can impact school discipline, lost mentorship and leadership opportunities, less access to educational opportunities afforded to white peers, and greater involvement in the juvenile justice system.
- Comprehensive sex education addresses these issues by including positive representations of diverse youth in curriculum, challenging harmful stereotypes, and building the skills required for respectful relationships.
A lack of comprehensive sex education can harm youth with disabilities or special health care needs.
- Youth with disabilities need inclusive, developmentally-appropriate, representative sex education to support their health, identity, and development .
- Youth with special health care needs often initiate romantic relationships and sexual behavior during adolescence, similar to their peers.
- Youth with disabilities and special health care needs benefit from seeing themselves represented in sex education to access the information and skills to build healthy identities and relationships.
- Comprehensive sex education addresses this need by including positive representation of youth with disabilities and special health care needs in curriculum and providing developmentally-appropriate sex education to all youth.
- When youth with disabilities and special health care needs do not get access to the comprehensive sex education that they need, they are at increased risk of sexual abuse or being viewed as a sexual offender.
- Youth with disabilities and special health care needs are more likely than peers without disabilities to report coercive sex, exploitation, and sexual abuse.
- Youth with disabilities and special health care needs report more sexualized behavior and victimization online than their peers without disabilities.
- Youth with disabilities are at greater risk of bullying and have fewer friend relationships than their peers.
- Comprehensive sex education addresses these issues by providing education on healthy relationships, consent, communication, and bodily autonomy.
A lack of comprehensive sex education can harm youth who are LGBTQ2S+.
- Most sex education curriculum is not inclusive or representative of LGBTQ2S+ identities and experiences.
- Because school-based sex education often does not meet their needs, youth who are LGBTQ2S+ are more likely to seek sexual health information online , and thus are more likely to come across misinformation.
- The majority of parents support discussion of sexual orientation in sex education classes.
- Comprehensive sex education addresses these issues by including positive representation of LGBTQ2S+ individuals, romantic relationships, and families.
- Sex education curriculum that overlooks or stigmatizes youth who are LGBTQ2S+ contributes to hostile school environments and harms the healthy sexual and mental development .
- Youth who are LGBTQ2S+ face high levels of discrimination at school and are more likely to miss school because of bullying or victimization .
- Ongoing experiences with stigma, exclusion, and harassment negatively impact the mental health of youth who are LGBTQ2S+.
- Comprehensive sex education provides inclusive curriculum and has been shown to improve understanding of gender diversity, lower rates of homophobia, and reduce homophobic bullying in schools.
- Youth who are LGBTQ2S+ are more likely than their heterosexual peers to report not learning about HIV/STIs in school .
- Lack of education on STI prevention leaves LGBTQ2S+ youth without the information they need to make informed decisions, leading to discrepancies in condom use between LGBTQ2S+ and heterosexual youth.
- Some LGBTQ2S+ populations carry a disproportionate burden of HIV and other STIs: these disparities begin in adolescence , when youth who are LGBTQ2S+ do not receive sex education that is relevant to them.
- Comprehensive sex education provides the knowledge and skills needed to make safe decisions about sexual behavior , including condom use and other forms of STI and HIV prevention.
- Youth who are LBGTQ2S+ or are questioning their sexual identity report higher rates of dating violence than their heterosexual peers.
- Youth who are LGBTQ2S+ or are questioning their sexual identity face higher prevalence of bullying than their heterosexual peers.
- Comprehensive sex education teaches youth healthy relationship and communication skills and is associated with decreases in dating violence and increases in bystander interventions .
A lack of comprehensive sex education can harm youth who are in foster care.
- More than 70% of children in foster care have a documented history of child abuse and or neglect.
- More than 80% of children in foster care have been exposed to significant levels of violence, including domestic violence.
- Youth in foster care are racially diverse, with 23% of youth identifying as Black and 21% of identifying as Latinx, who will have similar experiences as those highlighted in earlier sections of this report.
- Removal is emotionally traumatizing for almost all children. Lack of consistent/stable placement with a responsive, nurturing caregiver can result in poor emotional regulation, impulsivity, and attachment problems.
- Comprehensive sex education addresses these issues by providing evidence-based, culturally appropriate information on healthy relationships, consent, communication, and bodily autonomy.
Sex education is often the first experience that youth have with understanding and discussing their gender and sexual health.
Youth deserve to a strong foundation of developmentally appropriate information about gender and sexuality, and how these things relate to their bodies, community, culture, society, mental health, and relationships with family, peers, and romantic partners.
Decades of data have demonstrated that comprehensive sex education programs are effective in reducing risk of STIs and unplanned pregnancy. These benefits are critical to public health. However, comprehensive sex education goes even further, by instilling youth with a broad range of knowledge and skills that are proven to support social-emotional learning, positive communication skills, and development of healthy relationships.
Last Updated
American Academy of Pediatrics
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
School Based Sex Education and HIV Prevention in Low- and Middle-Income Countries: A Systematic Review and Meta-Analysis
* E-mail: [email protected]
Affiliation Johns Hopkins Bloomberg School of Public Health, International Health Department, Baltimore, Maryland, United States of America
Affiliation Medical University of South Carolina, Department of Psychiatry and Behavioral Sciences, Charleston, South Carolina, United States of America
- Virginia A. Fonner,
- Kevin S. Armstrong,
- Caitlin E. Kennedy,
- Kevin R. O'Reilly,
- Michael D. Sweat

- Published: March 4, 2014
- https://doi.org/10.1371/journal.pone.0089692
- Reader Comments
School-based sex education is a cornerstone of HIV prevention for adolescents who continue to bear a disproportionally high HIV burden globally. We systematically reviewed and meta-analyzed the existing evidence for school-based sex education interventions in low- and middle-income countries to determine the efficacy of these interventions in changing HIV-related knowledge and risk behaviors.
We searched five electronic databases, PubMed, Embase, PsycInfo, CINAHL, and Sociological Abstracts, for eligible articles. We also conducted hand-searching of key journals and secondary reference searching of included articles to identify potential studies. Intervention effects were synthesized through random effects meta-analysis for five outcomes: HIV knowledge, self-efficacy, sexual debut, condom use, and number of sexual partners.
Of 6191 unique citations initially identified, 64 studies in 63 articles were included in the review. Nine interventions either focused exclusively on abstinence (abstinence-only) or emphasized abstinence (abstinence-plus), whereas the remaining 55 interventions provided comprehensive sex education. Thirty-three studies were able to be meta-analyzed across five HIV-related outcomes. Results from meta-analysis demonstrate that school-based sex education is an effective strategy for reducing HIV-related risk. Students who received school-based sex education interventions had significantly greater HIV knowledge (Hedges g = 0.63, 95% Confidence Interval (CI): 0.49–0.78, p<0.001), self-efficacy related to refusing sex or condom use (Hedges g = 0.25, 95% CI: 0.14–0.36, p<0.001), condom use (OR = 1.34, 95% CI: 1.18–1.52, p<0.001), fewer sexual partners (OR = 0.75, 95% CI:0.67–0.84, p<0.001) and less initiation of first sex during follow-up (OR = 0.66, 95% CI: 0.54–0.83, p<0.001).
Conclusions
The paucity of abstinence-only or abstinence-plus interventions identified during the review made comparisons between the predominant comprehensive and less common abstinence-focused programs difficult. Comprehensive school-based sex education interventions adapted from effective programs and those involving a range of school-based and community-based components had the largest impact on changing HIV-related behaviors.
Citation: Fonner VA, Armstrong KS, Kennedy CE, O'Reilly KR, Sweat MD (2014) School Based Sex Education and HIV Prevention in Low- and Middle-Income Countries: A Systematic Review and Meta-Analysis. PLoS ONE 9(3): e89692. https://doi.org/10.1371/journal.pone.0089692
Editor: Sten H. Vermund, Vanderbilt University, United States of America
Received: May 20, 2013; Accepted: January 27, 2014; Published: March 4, 2014
Copyright: © 2014 Fonner et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Funding: This research was supported by the US National Institute of Mental Health, Grants R01 MH090173 and RC1 MH088950. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Competing interests: The authors have declared that no competing interests exist.
Introduction
Worldwide, young people aged 15–24 accounted for almost half of all new HIV infections among individuals aged 15 and older in 2010 [1] . School-based sex education is an intervention that has been promoted to increase HIV-related knowledge and shape safer sexual behaviors to help prevent new infections among this vulnerable group. As sexual debut is common in adolescence, so are the associated risks of engaging in transactional sex, having multiple concurrent partnerships, and experiencing sexual violence and coercion, all of which increase HIV-related risk [2] . School-based interventions are logistically well-suited to educate youth about sexual activity given their ability to reach large numbers of young people in an environment already equipped to facilitate educational lessons and group learning [3] .
Contentious debates have raged in the past decade regarding whether abstinence-only or comprehensive sexual education interventions are effective and appropriate. Abstinence-only interventions promote delaying sex until marriage with little to no information provided about contraceptives or condom use, whereas comprehensive sexual education provides information on abstinence as well as information on how to engage in safer sex and prevent pregnancies and sexually transmitted infections (STIs). In the 1990s various groups in the United States invested in abstinence-only education, and with the creation of the President's Emergency Plan for AIDS Relief (PEPFAR) in 2004, money was earmarked for “ABC” programs (abstain, be faithful, use condoms), with a heavy emphasis on the “A” component, to be implemented in low- and middle-income countries most impacted by HIV [4] . Critics of abstinence-only education claim that it violates human rights by withholding potentially life-saving information from people about other means to protect themselves from HIV, such as condom use [5] . Others argue that abstinence is only a viable option for those who are able to choose when, how, and with whom to have sex, which is not always the case for many young women [6] . Additionally, promoting abstinence until marriage excludes gay children and adolescents who have no option for marriage in most countries. As an alternative, comprehensive school-based sex education programs present participants with all prevention options, including condom use and partner reduction. Abstinence-plus interventions present prevention options as hierarchical with abstinence being presented as the only strategy that completely eliminates HIV/STI risk.
Previous research has been conducted on the effectiveness of youth-oriented HIV prevention and sex education interventions in school settings. A review of 35 school-based sex education programs by Kirby and Coyle [7] found that abstinence based programs had no significant effect on delaying sexual debut, while some comprehensive programs were effective in reducing certain sexual risk behaviors. Gallant and Maticka-Tyndale [3] reviewed 11 school-based HIV education programs in Africa and concluded that most studies had an effect on either increasing HIV-related knowledge or changing attitudes or behaviors relating to sexual risk. Paul-Ebhohimhen et al. [8] systematically reviewed 10 school-based sex education studies implemented in sub-Saharan Africa and noted that interventions were more likely to report changes in knowledge as opposed to changes in sexual behavior. Speizer et al. [9] reviewed 41 adolescent reproductive health interventions in developing countries, including 22 based in schools, and found that the majority of school-based interventions (17/21) demonstrated improved HIV-related knowledge. Chin et al. [10] conducted parallel systematic reviews and meta-analyses of comprehensive and abstinence-only educational interventions and found that comprehensive sex education programs significantly reduced HIV, STI, and unintended pregnancies, but results for the abstinence-only review were inconclusive.
However, few reviews have attempted to quantitatively synthesize the effects of school-based interventions on HIV-related risk behaviors across studies, and no review to date has attempted to compare the effectiveness of abstinence-only or abstinence plus interventions with comprehensive sex education in low- and middle-income countries. Therefore, the current review seeks to address this gap by conducting a systematic review and meta-analysis on the efficacy of school-based sex education interventions, including abstinence-only/abstinence-plus and comprehensive sex education programs, in changing HIV-related knowledge and risk behaviors in low- and middle-income countries. This review sought to answer the following research question: Does participating in school-based sex education vs. not participating in school-based sex education reduce HIV-related risk behaviors among youth in low- and middle-income countries?
This review is part of a large systematic review and meta-analysis project, called The Evidence Project, which is a joint collaboration between investigators at the Medical University of South Carolina and the Johns Hopkins Bloomberg School of Public Health. The Evidence Project reviews the efficacy of behavioral HIV prevention interventions in low- and middle-income countries. Other reviews published with this project include topics such as voluntary counseling and testing [11] , [12] , provider-initiated testing and counseling [13] , condom social marketing [14] , behavioral interventions for people living with HIV [15] , peer education [16] , psychosocial support [17] , mass media [18] , and treatment as prevention [19] . This review used standardized data abstraction forms and procedures that have been employed in all reviews published as part of The Evidence Project, although no standalone protocol has been published specifically for this review. Additionally, we followed standard systematic review and meta-analysis procedures set forth in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [20] .
Definition and Inclusion Criteria
School-based sex education was defined as programs designed to encourage sexual risk reduction strategies for HIV prevention delivered in school settings. This definition allowed for the inclusion of abstinence-only, abstinence-plus, and comprehensive sex education programs. Studies included in the review had to meet the following criteria: conducted in a low- or middle-income country as defined by the World Bank [21] ; published in a peer-reviewed journal from January 1, 1990 to June 16, 2010; presented results of pre-post or multi-arm experimental design and analysis of outcome(s) of interest; and involved an HIV prevention intervention administered in a school setting that encouraged one or more sexual risk reduction strategies, including abstinence, condom use, or partner reduction.
There were no restrictions on language; eligible non-English articles were translated by consultants fluent in English and the language in which the article was written. Participant age was also not restricted. Therefore, studies across a variety of educational settings, from primary schools through college and vocational schools, were included. Additionally, in order to include as many studies as possible, a wide range of study designs were eligible for inclusion: randomized controlled trials (both individual and cluster-randomized, i.e., school or classroom), non-randomized controlled trials, prospective or retrospective cohorts, time-series, before-after, case-control, cross-sectional, and serial cross-sectional studies.
Search strategy
Our search strategy involved three methods. First, five electronic databases, including PubMed, PsycInfo, EMBASE, CINAHL, and Sociological Abstracts, were searched using a combination of terms for sex education, schools/youth, and HIV or AIDS (full list available from the authors upon request). The search was limited to a date range of January 1, 1990 to June 16, 2010. We also searched the table of contents of AIDS , AIDS Care , AIDS and Behavior , and AIDS Education and Prevention for relevant citations. Finally, we searched the reference lists of all included studies for additional eligible studies. This process was iterative and continued until no additional studies were identified.
Trained research assistants conducted an initial screening of all citations and excluded studies clearly not relevant to school-based sex education. Two senior study staff members then independently screened all remaining citations and categorized studies as eligible for inclusion, not eligible for inclusion, or questionable. Discrepancies in categorization were resolved through consensus. Full article texts were obtained and discussed by senior researchers to ascertain eligibility if questionable. Articles were retained and included as background studies if they failed to meet the inclusion criteria but still contained information relevant to school-based sex education in low- and middle-income countries, including prior reviews, cost-effectiveness analyses, and qualitative studies.
Data Abstraction
The following data were abstracted from each eligible study using standardized forms: location, year(s) of study implementation, study setting, study population, sample size, study design, sampling frame and sampling methods, description of the intervention, composition of intervention and control groups (if applicable), length of follow-up, description of outcomes, effect sizes, confidence intervals, statistical tests employed, and study limitations. Two trained research assistants independently abstracted data from each study; any discrepancies were resolved through consensus. Data were double entered into EpiData version 3.1 (EpiData Association, Odense, Denmark) and later exported to an SPSS database (IBM SPSS Statistics for Windows, Version 20.0. Armonk, NY).
We also evaluated the methodological rigor of studies to assess risk of bias based on the following criteria: whether the study 1) included a cohort of participants, 2) had a control and experimental/intervention group, 3) compared baseline demographic equivalence of control and intervention groups, 4) compared outcome measures between control and intervention groups at baseline (if applicable), 5) contained both pre- and post-intervention data, 6) randomly selected participants for assessment (i.e. sampling strategy), 7) randomly assigned participants to the intervention, and 8) maintained a follow-up rate of greater than 80%.
Selection of outcomes
Outcomes were chosen for meta-analysis based on relevance to HIV prevention and frequency in available studies. The five most commonly reported outcomes across studies were: HIV knowledge, condom use, self-efficacy related to HIV prevention (e.g., confidence in refusing sex or confidence in using condoms during sex), initiation of first sex, and number of sexual partners. All outcomes were based on self-report. Studies containing at least one of these outcomes were included in meta-analysis if they met the following criteria:
- Provided an estimate of effect size and its variance, or provided statistics needed to calculate an effect size and variance. If enough information was not provided to calculate an effect size, study authors were contacted for clarification or additional statistics. If study authors did not provide this information after one month, the study was removed from the analysis.
- Presented pre-post or multi-arm results comparing either participants who received the intervention to those who did not, or comparing outcomes before and after the intervention. If results of a repeated measures analysis were reported, authors needed to provide the correlation between pre-post measurements or provide enough information to calculate the correlation between measurements. If these statistics were not available, either in publication or after request, and the study was a controlled design, an effect size was generated using post-intervention statistics provided groups were similar at baseline with respect to the outcome of interest and other relevant covariates.
- Presented an outcome of interest that was measured in such a way as to be comparable to outcomes assessed by other studies. In other words, outcomes needed to be similar enough to synthesize across studies.
- Presented data based on an individual unit of analysis (studies presenting classroom- or school-level data only were excluded from meta-analysis).
Meta-analysis
Using standard meta-analytic methods [22] , we standardized effect sizes as either Hedges' g (for continuous outcomes) or odds ratios (for dichotomous outcomes). For several outcomes, including HIV knowledge, self-efficacy, and number of sexual partners, both continuous and dichotomous effect sizes were combined in meta-analysis. In these instances, Comprehensive Meta-Analysis (CMA) was used to either convert the standard mean difference into an odds ratio when transforming the effect size from continuous to dichotomous or vice versa using methods developed by Hasselblad and Hedges [23] . This transformation assumes that the outcome under study involves an underlying continuous trait with a logistic distribution [24] and that outcomes are measured in relatively similar terms, regardless of whether they are presented dichotomously or continuously. For example, several studies reported number of sexual partners as a dichotomous outcome, such as having two or more partners in the past 6 months, whereas others reported a mean number of partners. The same logic holds for outcomes such as knowledge, where some studies presented knowledge outcomes on a continuous scale whereas others created a cut-off for “high” and “low” knowledge scores and presented results as a proportion. Combining both dichotomous and continuous effect sizes allowed us to utilize all available data.
CMA V.2.2 was used for all analyses [25] . Random effects models were used as included studies contained considerable heterogeneity of effects, and the purpose of the analysis was to generate inferences beyond the set of included studies [26] .
When possible, data were analyzed in several ways per outcome. Stratifications by age, gender, instructor (e.g., teacher, peer, or health care professional), intervention type (abstinence vs. comprehensive sex education), and length of follow-up were made when three or more studies could be retained per category. Additionally, when possible, we investigated the role of certain characteristics of the data itself, including comparing differences between continuous and dichotomous effect sizes and whether the effect size was based on data collected pre-post intervention or post-only. Mixed effects meta-regression techniques were used to compare effect sizes across strata when possible. The I 2 statistic and its confidence interval were calculated for each meta-analysis to describe inconsistencies in effect sizes across studies [24] , [27] . When possible adjusted effect sizes were used in the pooled analyses; however, outcomes were most frequently reported in unadjusted terms, thus the analyses contain both adjusted and unadjusted effect sizes. Potential bias across studies, such as publication bias and selective reporting, was assessed for the HIV-related knowledge outcome by constructing a funnel plot. Funnel plots were not constructed for the remaining meta-analyses because there were too few studies to interpret the dispersion of effect sizes across the range of standard errors.
Description of studies
Of 6191 studies initially identified, 64 studies in 63 articles met the inclusion criteria for this review ( Figure 1 ). In five cases, more than one article presented data from the same study [28] – [39] . If articles from the same study presented different outcomes or follow-up times, both articles were retained and included in the review as one study [30] , [31] , [37] , [38] . If both articles presented similar data, such as by providing an update with longer follow-up, the most recent article or the article with the largest sample size was chosen for inclusion [28] , [33] , [36] , [39] .
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0089692.g001
Table 1 provides descriptions of included studies. The majority of studies took place in sub-Saharan Africa (n = 29, 45.3%). Studies also took place in East Asia/Pacific (n = 15, 23.4%), Europe/Central Asia (n = 2, 3.1%), Latin American/Caribbean (n = 16, 25.0%), and South Asia (n = 4, 6.3%). The most commonly used study design was a group randomized trial (n = 21), with schools or classrooms as the unit of randomization. Other study designs included individual randomized controlled trials (n = 4), before-after studies (n = 14), non-randomized individual trials (n = 2), non-randomized group trials (n = 12), serial cross-sectional studies (n = 4), cross-sectional studies (n = 5), and two studies utilized a study design classified as “other” which involved a hybrid of eligible study designs.
https://doi.org/10.1371/journal.pone.0089692.t001
Table 2 presents the methodological rigor assessment for included studies. Regarding methodological rigor, forty-seven studies used a control group, but only 18 studies reported whether intervention and control groups were equivalent on socio-economic variables at baseline, and only 14 reported whether intervention and control groups were equivalent on outcome measures at baseline.
https://doi.org/10.1371/journal.pone.0089692.t002
Most studies included both male and female participants; three studies evaluated school based sex education for girls only [40] , [42] . Most studies (n = 56) took place among primary or secondary school students, five studies were implemented among university students [43] – [47] , two involved secondary and university students [36] , [48] , one study involved student nurses [49] , and another involved teacher trainees [50] . Ages of study participants ranged from 9, for an intervention among 4 th graders in Mexico [51] , to 38, for an intervention among university students in Malaysia [44] . Of the 27 studies reporting a mean age of study participants, the average age was 16.5 (SD = 2.7). Many studies included study populations with a wide range of ages. The age range in six studies spanned 10 years or more [52] – [55] . Generally, in studies measuring sexual risk behaviors, only a small portion of students in the study population were sexually active, thus substantially reducing the sample size for these outcomes.
Content of interventions.
Nine studies either taught abstinence-only or emphasized abstinence or delay of sexual debut over other risk reduction strategies among in-school youth [29] , [33] , [40] , [41] , [55] – [60] . The remaining studies provided comprehensive sex education.
Many studies reported using a variety of instructional formats to convey information and generate discussion. For example, 35 studies used lectures, 34 employed interactive discussions, 30 incorporated role-plays, and 21 utilized skill-based sessions, such as learning the steps involved in correct condom use. Use of media such as videos and audio tapes was also common. Two studies relied on drama, including creating plays and skits, for the bulk of the intervention [61] , [62] and one study used a comic book to impart information [63] . Two studies were internet-based [36] , [64] and involved students completing online modules during school hours at their own pace. Thirty three interventions reported basing their intervention on theory. Theories commonly referenced were Social Cognitive Theory, Health Belief Model, and Theory of Reasoned Action.
Intervention content varied widely. Several interventions were adapted from curricula that had been developed and implemented elsewhere, such as the US-based “Focus on Kids” [31] , [38] , [43] , “Making Proud Choices” [41] , and WHO's “Responsible Behavior: Delaying Sex” [40] . Other interventions worked with local community members and health educators to develop appropriate curricula. Forty-one studies included some form of commnity involvement in the intervention, such as consulting with parents and communities about what content could and could not be included in the intervention [33] , [55] , [56] , [58] , [60] , [65] – [68] . Many studies reported a reluctance by teachers, parents, and/or communities to discuss or allow discussion of condoms during the intervention [33] , [55] , [56] , [65] , [66] , [68] . Interventions commonly addressed health-related issues in addition to HIV/AIDS prevention (n = 43), including reproductive biology (n = 22), pregnancy prevention (n = 16), STI prevention (n = 22), relationships (n = 10), violence (n = 5), and values clarification (n = 5).
Intervention duration, location, and instructor type.
Interventions ranged from 2 or 3 hours in total [69] , [70] to spanning multiple years and involving community-based components such as the creation of a youth resource center, youth-led condom distribution [30] , [37] , and training healthcare workers how to provide youth-friendly health information [68] . Most studies took place during the regular school day, although several studies included alternate times for the school-based sex education, such as having sessions on Saturdays [40] or after school hours [31] , [38] , [60] . Interventions were facilitated by health professionals, teachers, or peer educators, although several studies involved a mix of facilitator types throughout the intervention. The majority of studies took place in urban (n = 34) or peri-urban settings (n = 2). Only 3 studies specified that interventions took place in rural areas, 14 studies were conducted in a mix of urban and rural settings, and 11 studies did not provide enough information to determine the type of setting in which the intervention took place.
Meta-analysis results
Hiv/aids knowledge..
HIV-related knowledge was the most commonly reported study outcome. Of all included studies, 49 (76.6%) evaluated the effect of the intervention on HIV-related knowledge. The measures used to assess HIV-related knowledge varied by study but centered on aspects such as HIV biology, HIV transmission, and HIV prevention. Some studies measuring HIV-related knowledge were excluded from meta-analysis for not controlling for baseline differences in socio-demographics or outcome variables (n = 3) [29] , [71] , [72] , not providing enough data to convert results into standardized effect sizes (n = 18) [36] , [47] – [50] , [56] , [57] , [62] , [63] , [65] , [69] , [73] – [78] , presenting knowledge outcomes not specifically related to HIV (n = 2), such as asking students whether they knew about HIV/AIDS [58] , and measuring how many STIs students correctly identified [66] .
Twenty-six studies were included in the meta-analysis for knowledge; results are presented in Table 3 and Figure 2 . Nineteen studies reported knowledge as a continuous outcome; seven reported it dichotomously. In meta-analysis, dichotomous outcomes were converted to standardized mean differences for comparison across all studies. Random effects meta-analysis suggests that students who were exposed to a sexual education intervention were more knowledgeable of HIV and related topics than youth who did not experience an intervention. The standardized mean difference (Hedges' g ) was 0.63 with a 95% confidence interval of 0.49 to 0.78, p<0.001. Meta-regression indicated no significant standardized mean difference when comparing males and females (p = 0.194); however, only 3 studies reported data disaggregated by gender with two additional studies reporting on entirely female samples. Similarly there was no significant difference in standardized mean knowledge score differences comparing abstinence-focused to comprehensive sex education interventions (p = 0.501). When stratified by instructor type, interventions led by health professionals (e.g. doctors, nurses, or health educators), appeared to produce more knowledgeable students than those led by either teachers, peers, or a mix of different types of instructors (β = 0.65, p = 0.004). However, when the two interventions implemented among college students were removed [42] , [43] , this effect was no longer significant.
A: Effect of school-based sex education on HIV-related knowledge (random effects, Hedges' G). B: Effect of school-based sex education on condom use (random effects, odds ratio). C: Effect of school-based sex education on self-efficacy (random effects, Hedges' G). D: Effect of school-based sex education on number of sexual partners (random effects, odds ratio). E: Effect of school-based sex education on initiation of first sex (random effects, odds ratio). Note . Results from Diaz et al., 2005, Fiscian et al., 2009, Givauden et al., 2008, Klepp et al., 1997, Visser et al., 1996, Visser et al., 2005, Cartagena et al., 2006, Okonofua et al., 2003, and Li et al., 2008 were adjusted for baseline differences and certain covariates. Values from remaining studies are unadjusted. *p<0.05, **p<0.010, and ***p<0.001.
https://doi.org/10.1371/journal.pone.0089692.g002
https://doi.org/10.1371/journal.pone.0089692.t003
When considering length of follow-up time, standardized mean differences in knowledge scores were largest when data were collected 3 to 11 months post-intervention compared to all other categories of follow-up time (Hedges' g = 0.87, 95% CI 0.60–1.13, p<0.001). The smallest differences were seen when knowledge was measured 3 months or less post-intervention (Hedges' g = 0.70, 95% CI: 0.43–0.97, p<0.001). Studies with the shortest follow-up time generally corresponded to studies of the shortest duration (≤3 weeks). However, duration was difficult to measure due to wide variations in length and intensity of intervention implementation. Two studies evaluated the long-term effects (≥3 years post-intervention) of year-long interventions based in schools in Tanzania [30] and Kenya [68] . The study from Tanzania found that effects on knowledge remained significant after 3 years, but limited sustained effects on behaviors were seen [30] . The study from Kenya found significant improvements in HIV-related knowledge 3 years post-intervention, although knowledge initially appeared to decline in the period from pre-intervention to 18-months [68] . Regarding type of measure used, studies measuring knowledge as a dichotomous outcome generated smaller effect sizes than studies measuring knowledge continuously; this difference was statistically significant (β = −0.42, p = 0.02).
A funnel plot of the distribution of effect sizes by their standard error (figure not shown) suggests that some bias exists across studies as the plot was asymmetrical, indicating a possible underdispersion of less precise effect sizes. Following the assumption of normally distributed effect sizes across studies, finding more studies demonstrating at least a null effect would be expected, but finding studies showing a negative effect is less likely given the nature of the outcome, knowledge. Given the wide range of scales used to assess knowledge and the different facets of sexual education being taught across interventions, the asymmetrical plot could also be interpreted as presenting more evidence of a truly heterogeneous effect of school-based sexual education on HIV-related knowledge. The I 2 value also supports this hypothesis.
Self-efficacy.
Twenty-two studies measured self-efficacy. Fourteen of these studies were excluded from meta-analysis for measuring general self-efficacy or self-efficacy not related to condom use or sex refusal (n = 8) [41] , [46] , [51] , [64] , [71] , [79] , [80] or for not providing enough data to convert to standardized effect size measures (n = 6) [50] , [62] , [73] , [74] , [77] , [78] . The remaining eight studies measured self-efficacy related to either sex refusal or condom use and were included in meta-analysis [31] , [43] , [68] , [81] – [85] . All but one study included in meta-analysis measured self-efficacy on a continuous scale; the remaining study measured self-efficacy as a proportion. The one dichotomous outcome was transformed into a standardized mean difference to allow comparison across studies. The standardized mean difference (Hedges' g) comparing those who received the intervention to those who did not was 0.25 (95% CI: 0.14–0.36, p<0.001), meaning those receiving the intervention exhibited significantly more self-efficacy in regards to being able to refuse sex or use a condom during sex. The intervention with the largest mean difference in self-efficacy was implemented among university students in Nanjing, China using an adapted version of the “Focus on Kids” program originally identified as an effective intervention by the U.S. Centers for Disease Control and Prevention (CDC), which involved group activities and games facilitated by trained graduate students and faculty [43] . The intervention with the second highest mean difference in self-efficacy involved an intervention delivered to secondary students in Ukraine by trained young physicians consisting of 6 weekly 1 hour sessions focusing on HIV transmission and biology, condom use negotiation skills, preventive measures, and dangers of drug use through small group activities, role playing, games, and discussions [83] . This intervention was adapted using the WHO Training and Resource Manual on School Health and HIV Prevention. One included study involving a 3 hour HIV-prevention workshop found no increase in condom use self-efficacy [85] .
Condom use.
Twenty one studies measured condom use as a primary outcome. Of these, 13 were eligible for meta-analysis [31] , [37] , [52] , [59] , [66] , [68] , [73] , [85] – [88] . Eight studies were excluded for not presenting enough data to convert to a standardized effect size [39] , [43] , [45] , [62] , [77] , [78] , [82] , [89] . Condom measures included in the analysis were condom use at last sex, 100% condom use, and consistent condom use (all dichotomous measures). When synthesized across interventions, condom use was significantly higher among intervention participants (OR = 1.34, 95% CI: 1.18–1.52, p<0.001). Individually, only three of the twelve studies found a significant difference in condom use between intervention and control groups [37] , [66] , [68] . All three of these studies included some form of training for healthcare workers outside of the school-setting on how to provide youth-friendly sexual and reproductive health information, including condom use [37] , [66] , [68] . In one study based in Kenya, providing lessons on condom use was met with strong resistance from teachers who feared that teaching students about condoms would encourage sexual activity [68] . As a result, condom use was not included in the regular lesson plans although teachers were trained on how to respond to students' questions about condoms in a factual manner [68] . Of all interventions included in this meta-analysis, there was one abstinence-plus program that reported emphasizing delay of sexual debut until marriage while still provided information on other prevention measures, such as condom use [59] . This study did not find a significant difference in consistent condom use comparing those who received the intervention to those who did not 3-months post-intervention (OR = 1.13, 95% CI: 0.30–4.20, p = 0.86).
Number of sex partners.
Of 10 studies measuring participants' number of sexual partners, four were eligible for meta-analysis [31] , [37] , [58] , [87] . Six were excluded for not containing enough data to convert results into standardized effect sizes [36] , [45] , [59] , [62] , [78] , [90] . Of the four studies included in meta-analysis, three presented results dichotomously; the remaining study presented results continuously (mean number of sex partners). The continuous outcome was converted to a standardized mean difference to allow for comparison across all studies. Outcomes synthesized for this analysis included: having greater than 1 partner in the last 12 months [37] , mean reported number of partners [58] , having greater than 2 sexual partners in the last 6 months [31] , and reporting multiple partners during the past 3 months [87] . Across studies students receiving interventions demonstrated a 25% reduction in odds of reporting more partners compared to control or comparison groups (OR = 0.75, 95% CI: 0.67–0.84, p<0.001). However, individually, only one study with a large sample size (n = 6877) showed students receiving the intervention reported fewer sex partners [37] whereas the other studies showed a non-significant difference. Data from this study were collected 36 months following the intervention, which was the longest reported follow-up of all included studies [37] .
Initiation of first sex.
Nine studies measured initiation of first sex. Three were excluded for not containing enough data to convert results into standardized effect sizes for meta-analysis [62] , [78] , [90] . The remaining six studies were included in meta-analysis [31] , [33] , [37] , [60] , [68] , [85] . All studies measured this outcome dichotomously. Participants who received the intervention had a 34% reduction in odds of initiating sexual intercourse during follow-up compared to control or comparison groups (OR = 0.66, 95% CI = 0.54–0.83, p<0.001). Individually all but one study [60] showed significant reductions in sexual debut for those who received the intervention. The study showing the highest reduction in sexual debut involved activities that took place beyond the classroom setting, including the provision of youth friendly reproductive health services, condom distribution, and community mobilization [37] . The one abstinence-only program that measured sexual initiation [33] also showed a significant reduction in odds of sexual debut between the 6 th and 7 th grade school years for youth who received the intervention (OR = 0.36, 95% CI 0.21–0.62, p<0.001).
This review found that school-based sex education is an effective intervention for generating HIV-related knowledge and decreasing sexual risk behaviors among participants, including delaying sexual debut, increasing condom use, and decreasing numbers of sexual partners. Importantly, no individual study included in meta-analysis, including abstinence-only, abstinence-plus, and comprehensive school-based sex education interventions, found detrimental effects of school-based sex education on increased risky sexual behavior. This finding is notable given that some argue programs including information on abstinence and safe sex strategies give mixed messages to students and may promote sexual activity [91] .
Comprehensive school-based sex education comprised the majority of interventions included in this review despite extensive attempts to identify abstinence-only and abstinence-plus interventions. Given PEPFAR's past emphasis on abstinence-only and abstinence-plus interventions [4] , it is surprising to find so few peer reviewed evaluations of this strategy that met our inclusion criteria. The uneven distribution in comprehensive versus abstinence-only or abstinence-plus interventions made it difficult to compare the effectiveness of these intervention types. Additionally, many abstinence-only or abstinence-plus interventions measured outcomes related to HIV-knowledge but did not include outcomes related to sexual risk behavior, such as condom use or number of sexual partners, thus rendering comparisons to comprehensive sex education unfeasible. These findings are similar to those of parallel systematic reviews and meta-analyses comparing the effectiveness of comprehensive sex education and abstinence-only interventions, which found that although comprehensive sex education interventions were effective at reducing high-risk sexual behavior, no conclusion could be drawn from interventions emphasizing abstinence due to the small number of eligible studies and inconsistent findings [10] .
Interventions producing the most significant changes in behavior seemed to have several characteristics in common. First, several effective interventions included community-based components that extended beyond school-based sex education by involving resources and activities outside of the school environment, such as training healthcare staff to offer youth-friendly services, distributing condoms, and involving parents, teachers, and community members in intervention development. Additionally, studies that adapted curricula from interventions already deemed efficacious also tended to produce significant changes on HIV-related behaviors. These findings are similar to another review which concluded that replicating effective sex education programs continued to produce significant behavior changes even when programs were implemented in different settings [92] .
It is encouraging that many of the reviewed studies used controlled designs and randomized intervention assignments, especially as earlier reviews have emphasized the need to improve study designs when evaluating school-based sex education interventions [92] , [93] . Despite this improvement, many studies exhibited methodological flaws that have been discussed at length elsewhere [94] , which inhibited our ability to include these studies in meta-analysis. Out of 64 included studies, 50 measured at least one of the five outcomes included in this meta-analysis, and of these 33 provided enough data to include in the quantitative synthesis. This finding highlights the need to further improve the methodological rigor of studies.
Limitations
This review must be seen in light of several limitations. Firstly, all outcomes reported in this review were based on self-report, which creates potential for social desirability bias and memory error. Secondly, we combined outcomes in meta-analysis that are not identical, such as combining effect sizes generated from different scales measuring HIV-related knowledge, which could lead to inaccuracies in synthesized effects. We also combined both continuous and dichotomous outcomes in several meta-analyses, which could introduce error [95] , although comparability has been shown between continuous and dichotomous outcomes used in meta-analysis when certain assumptions are met [96] . Additionally, it is possible our search strategy excluded potentially eligible articles. We used multiple search strategies in an effort to minimize this risk. This review could also be affected by publication bias, which was assessed by constructing funnel plots when feasible, although several studies showing null effects for various outcomes were included.
School-based sex education is a critical tool for HIV prevention among youth, and research suggests school-based HIV prevention programs are cost-effective when implemented in the context of combination prevention [97] . Intervention evaluations need to go beyond addressing the question of whether school-based sex education increases knowledge and focus instead on understanding implementation factors that led to the most success in shaping and changing subsequent HIV-related risk behaviors. As recently stated by the United Nations Special Rapporteur on the Right to Education, access to education about sex and reproductive health is a human right [98] ; therefore greater efforts should be made to identify and scale-up effective interventions. However, school-based education alone cannot be relied on to prevent HIV infections among young people since not all young people attend school and since school funds and resources are often already strained. Instead, school-based sex education should be part of more holistic HIV prevention intervention aiming to engage young people in learning about and shaping their sexual and reproductive future.
Supporting Information
Checklist s1..
PRISMA Checklist for systematic reviews.
https://doi.org/10.1371/journal.pone.0089692.s001
Acknowledgments
The authors thank Samantha Herrera, Jewel Gausman, Alexandria Smith, Hieu Pham, Jeremy Lapedis, Erica Layer, Tina Dickenson, Eugenia Pyntikova, Lorraine Beraho, Meera Seshadri, and Aisha Yansaneh, for their coding work on this review. The authors also thank Sarah Robbins and Jenny Tighe for their help with formatting and manuscript review.
Author Contributions
Conceived and designed the experiments: MS KO CK VF. Analyzed the data: KA VF. Wrote the paper: VF KA CK KO MS.
- 1. UNAIDS (2012) UNAIDS Report on the Global AIDS Epidemic. Geneva, Switzerland.
- View Article
- Google Scholar
- 21. WorldBank In: Regions Ca, editor.
- 22. (1994) The Handbook of research synthesis. In: Cooper HM, Hedges LV, editors. New York :: Russell Sage Foundation.
- 24. Borenstein M, Hedges LV, Higgins JPT, Rothstein HR (2009) Introduction to Meta-Analysis. John Wiley & Sons, Ltd.
- 25. Borenstein M, Hedges L, Higgins J, Rothstein;(2005) Comprehensive Meta Analysis (CMA). Version 2.2, Biostat, Englewood NJ
- 98. UN Human Rights Council (2010) Report of the Special Rapporteur on the right to education, Addendum : Communications sent to and replies received from Governments,. 17 May 2010, A/HRC/14/25/Add.1, available at: http://www.unhcr.org/refworld/docid/4c29b2342.html .

State Profiles
Access the SIECUS State Education Profiles: A living document of real-time updates on U.S. state policies for sex education. Our color-coded, state-by-state analysis evaluates existing laws and legislative activities, providing a detailed view of regional educational policies. These profiles serve as a crucial tool for advancing informed, comprehensive sex education, reflecting our ongoing commitment to shape policy that supports equitable and effective teaching standards.
State Profile Highlights
- 30 states and the District of Columbia require sex education, either explicitly by law or by proxy via enforced state standards.
- 39 states and the District of Columbia specifically require instruction on HIV/AIDS in schools.
- 35 states require schools to emphasize the importance of abstinence when sex education or HIV/STI instruction is provided.
- 17 states provide abstinence-only sex education
- 21 states require instruction on condoms or contraception when sex education or HIV/STI instruction is provided.
- 12 states do not require sex education or HIV/STI instruction to be any of the following, by law: age-appropriate, medically accurate, culturally responsive, or evidence-based/evidence-informed.
- 12 states require sex education or HIV/STI instruction to include information on consent.
- 10 states have policies that include affirming sexual orientation instruction on LGBTQ identities or discussion of sexual health for LGBTQ youth.
- 4 states explicitly require instruction that discriminates against LGBTQ people
- 3 states (CA, OR, WA) require comprehensive sex education to be taught in all schools
- 2 states (CO and IL) require sex education curriculum to be comprehensive, IF it is taught in schools.
The provided highlights are not a comprehensive view of how sex education is implemented in each state; rather, it only represents the policies and laws in place that influence the kind of sex education that might exist in your local jurisdiction. . As a result, these highlights do not reflect the realities of how sex education looks like in classrooms across the United States due to the intricacies of local control at the school district and individual school level. For more detailed inquiries regarding these statistics, please contact Alison Macklin, Director of Policy and Advocacy, [email protected]
For a detailed look at sex ed policies that impact you based on where you live, click on your state in the map above.
About the SIECUS State Profiles
The SIECUS State Profiles provides an in-depth and up-to-date look at the state of sex education in all 50 states, the District of Columbia, Puerto Rico, and the outer United States territories and associated states, pursuant to data available.
The profiles include an overview of each state’s current sex education laws, policies, and guidelines, newly introduced legislation, and relevant action that advocates have taken to advance or defend sex education in their communities. This report also incorporates the Centers for Disease Control and Prevention’s School Health Profiles data to help paint a comprehensive picture of what sexual health education topics are, or are not, being taught to young people in the classroom.
The SIECUS State Profiles serves as an evolving guide and will be regularly updated as new legislation and related activity becomes available.
This resource is intended to be used by advocates, educators, policymakers, health care providers, parents, and youth to aid in efforts to advance sex education in every community across the country. To request older editions of the SIECUS State Profiles (2003 – 2015), please email [email protected] .
Other State Profile Editions (Archive)

Review the 2022 Sex Ed State Profiles
Review the 2021 Sex Ed State Profiles
Review the 2020 Sex Ed State Profiles
Older Archives (2016-2018)
Summary State Policies on Sex Education in Schools
Why is sexual education taught in schools.
A 2017 Centers for Disease Control and Prevention (CDC) survey indicates that nearly 40 percent of all high school students report they have had sex, and 9.7 percent of high school students have had sex with four or more partners during their lifetime. Among students who had sex in the three months prior to the survey, 54 percent reported condom use and 30 percent reported using birth control pills, an intrauterine device (IUD), implant, shot or ring during their last sexual encounter.
The birth rate for women aged 15-19 years was 18.8 per 1,000 women in 2017, a drop of 7 percent from 2016. According to CDC, reasons for the decline are not entirely clear, but evidence points to a higher number of teens abstaining from sexual activity and an increased use of birth control in teens who are sexually active. Though the teen birth rate has declined to its lowest levels since data collection began, the United States still has the highest teen birth rate in the industrialized world.
Certain social and economic costs can result from teen pregnancy. Teenage mothers are less likely to finish high school and are more likely than their peers to live in poverty, depend on public assistance, and be in poor health. Their children are more likely to suffer health and cognitive disadvantages, come in contact with the child welfare and correctional systems, live in poverty, drop out of high school and become teen parents themselves. These costs add up, according to The National Campaign to Prevent Teen and Unplanned Pregnancy, which estimates that teen childbearing costs taxpayers at least $9.4 billion annually. Between 1991 and 2015, the teen birth rate dropped 64%, resulting in approximately $4.4 billion in public savings in one year alone.
Sexually transmitted infections (STIs) disproportionately affect adolescents due to a variety of behavioral, biological and cultural reasons. Young people ages 15 to 24 represent 25 percent of the sexually active population, but acquire half of all new STIs, or about 10 million new cases a year. Though many cases of STIs continue to go undiagnosed and unreported , one in four sexually-active adolescent females is reported to have an STI.
Human papillomavirus is the most common STI and some estimates find that up to 35 percent of teens ages 14 to 19 have HPV. The rate of reported cases of chlamydia, gonorrhea, and primary and secondary syphilis increased among those aged 15-24 years old between 2017-2018. Rates of reported chlamydia cases are consistently highest among women aged 15-24 years, and rates of reported gonorrhea cases are consistently highest among men aged 15-24 years. A CDC analysis reveals the annual number of new STIs is roughly equal among young women and young men. However, women are more likely to experience long-term health complications from untreated STIs and adolescent females may have increased susceptibility to infection due to biological reasons.
The estimated direct medical costs for treating people with STIs are nearly $16 billion annually, with costs associated with HIV infection accounting for more than 81% of the total cost. In 2017, approximately 21 percent of new HIV diagnoses were among young people ages 13 to 24 years.
Sex Education and States
All states are somehow involved in sex education for public schoolchildren.
As of October 1, 2020:
- Thirty states and the District of Columbia require public schools teach sex education, 28 of which mandate both sex education and HIV education.
- Thirty-nine states and the District of Columbia require students receive instruction about HIV.
- Twenty-two states require that if provided, sex and/or HIV education must be medically, factually or technically accurate. State definitions of “medically accurate" vary, from requiring that the department of health review curriculum for accuracy, to mandating that curriculum be based on information from “published authorities upon which medical professionals rely.” (See table on medically accuracy laws.)
Many states define parents’ rights concerning sexual education:
- Twenty-five states and the District of Columbia require school districts to notify parents that sexual or HIV education will be provided.
- Five states require parental consent before a child can receive instruction.
- Thirty-six states and the District of Columbia allow parents to opt-out on behalf of their children.
*Medical accuracy is not specifically outlined in state statue, rather it is required by the New Jersey Department of Education, Comprehensive Health and Physical Education Student Learning Standards.
** Medical accuracy requirement is pursuant to rule R277-474 of the Utah Administrative Code.
***Medical accuracy is not outlined in state statute, rather it is included in the Virginia Department of Education Standards of Learning Document for Family Life Resources.
Source: NCSL, 2019; Guttmacher Institute, 2019; Powered by StateNet
Related Resources
Health costs, coverage and delivery state legislation, state public health legislation database, ems legislative database, contact ncsl.
For more information on this topic, use this form to reach NCSL staff.
- What is your role? Legislator Legislative Staff Other
- Is this a press or media inquiry? No Yes
- Admin Email
- Subject List
- Take a Tour
- For Authors
- Subscriber Services
- Publications
- African American Studies
- African Studies
- American Literature
- Anthropology
- Architecture Planning and Preservation
- Art History
- Atlantic History
- Biblical Studies
- British and Irish Literature
- Childhood Studies
- Chinese Studies
- Cinema and Media Studies
- Communication
- Criminology
- Environmental Science
- Evolutionary Biology
- International Law
- International Relations
- Islamic Studies
- Jewish Studies
- Latin American Studies
- Latino Studies
- Linguistics
- Literary and Critical Theory
- Medieval Studies
- Military History
- Political Science
Public Health
- Renaissance and Reformation
- Social Work
- Urban Studies
- Victorian Literature
- Browse All Subjects
How to Subscribe
- Free Trials
In This Article Expand or collapse the "in this article" section Sex Education in HIV/AIDS Prevention
Introduction, general history of hiv/aids.
- Sex Education Resources
- Sex Education Programs in Schools, Communities, and Clinics
- Abstinence-Based
- Comprehensive Approach
- Evidence-Based HIV/AIDS Prevention Programs
Related Articles Expand or collapse the "related articles" section about
About related articles close popup.
Lorem Ipsum Sit Dolor Amet
Vestibulum ante ipsum primis in faucibus orci luctus et ultrices posuere cubilia Curae; Aliquam ligula odio, euismod ut aliquam et, vestibulum nec risus. Nulla viverra, arcu et iaculis consequat, justo diam ornare tellus, semper ultrices tellus nunc eu tellus.
- Child Maltreatment
- Health Communication
- Health Education
- Health Promotion
- Population Health Objectives and Targets
Other Subject Areas
Forthcoming articles expand or collapse the "forthcoming articles" section.
- Cultural Considerations in Disability
- Health Fraud, Quackery, and Misinformation
- Motivational Interviewing
- Find more forthcoming articles...
- Export Citations
- Share This Facebook LinkedIn Twitter
Sex Education in HIV/AIDS Prevention by Jessica M. Sales , Ralph J. DiClemente LAST REVIEWED: 23 February 2011 LAST MODIFIED: 23 February 2011 DOI: 10.1093/obo/9780199756797-0115
HIV/AIDS is the largest epidemic in modern history, resulting in approximately 25 million deaths since 1981, with an estimated 33.4 million people living with HIV/AIDS. Since the discovery of HIV/AIDS in 1981, researchers have been working to combat the spread of this devastating illness. In spite of recent attempts, there is neither a vaccine to prevent the acquisition of HIV, the virus that causes AIDS, nor a cure for the illness once it is contracted. Thus, education-based prevention programs or “sex education” programs are among the strongest means of curtailing the spread of HIV/AIDS. It is widely accepted that young people have a right to sex education because it is a means by which they can protect themselves against unintended pregnancies and sexually transmitted diseases (STDs), including HIV infection. Sex education programs, implemented in diverse venues including schools or medical clinics, typically provide information to young people to help them form healthy attitudes and beliefs about sex, sexual identity, relationships, and intimacy. Sex education programs often also provide skills-based training to accompany knowledge so that young people can make informed decisions about their behavior, as well as feel capable of acting on and communicating those decisions to others. Sex education programs designed to reduce sexual and drug-associated HIV risk behaviors are, for all intents and purposes, today’s “HIV vaccine,” but there has been a great deal of debate on what constitutes appropriate content for sex education programs for young people. Recent reviews have identified effective components of sex education programs/interventions, and also many effective, evidence-based HIV/AIDS prevention programs for diverse adolescent populations.
In 1981 the United States became the first country to officially recognize a strange and fatal illness among a small number of gay men. The first official documentation of the condition now known as HIV/AIDS was published in Centers for Disease Control and Prevention 1981 . The CDC report details the cases of five young gay men hospitalized with rare cancers or serious pneumonias. Timeline: A Brief History of HIV/AIDS provides an excellent timeline of the HIV epidemic. Today, the CDC’s HIV/AIDS Surveillance Reports continue to offer updated statistics on HIV/AIDS in the United States, and UNAIDS: Joint United Nations Programme on HIV/AIDS provides updated global surveillance reports.
AEGiS. Timeline: A Brief History of HIV/AIDS .
This online resource provides a brief yet detailed timeline of the history of HIV/AIDS from the first known case to the present.
Centers for Disease Control and Prevention. 1981. Pheumocystis pneumonia—Los Angeles. Morbidity and Mortality Weekly Report 30.21: 1–3.
This report contains a detailed description of the first US cases of AIDS and provides an interesting account of the “birth” of a disease that is quite familiar in the early 21st century.
Centers for Disease Control and Prevention. HIV Surveillance Reports .
The annual HIV Surveillance Report contains tabular and graphic information about US AIDS and HIV cases, including data by state, metropolitan statistical area, mode of exposure to HIV, sex, race/ethnicity, age group, vital status, and category of case definition.
UNAIDS: The Joint United Nations Programme on HIV/AIDS .
This online resource provides updated global HIV/AIDS Surveillance Reports for countries around the world and serves as a good general reference for gaining a better understanding of the global epidemic. Additionally, this resource is available in a variety of languages, including English, French, and Spanish.
back to top
Users without a subscription are not able to see the full content on this page. Please subscribe or login .
Oxford Bibliographies Online is available by subscription and perpetual access to institutions. For more information or to contact an Oxford Sales Representative click here .
- About Public Health »
- Meet the Editorial Board »
- Access to Health Care
- Action Research
- Active Aging
- Active Living
- Adolescent Health, Socioeconomic Inequalities in
- Adolescent Risk-Taking Behavior in the United States
- Advocacy, Public Health
- Agricultural Safety and Public Health
- Air Quality: Health Effects
- Air Quality: Indoor Health Effects
- Alcohol Availability and Violence
- Alternative Research Designs
- Ambient Air Quality Standards and Guidelines
- American Perspectives on Chronic Disease and Control
- Antimicrobial Resistance (AMR)
- Arts in Health
- Asthma in Children
- Asthma, Work-Related
- Attachment as a Health Determinant
- Behavior Change Theory in Health Education and Promotion
- Behavioral Risk Factor Surveillance
- Bicycling and Cycling Safety
- Birth and Death Registration
- Birth Cohort Studies
- Board of Health
- Breastfeeding
- Built Environment and Health, The
- Business and Corporate Practices
- Cancer Communication Strategies in North America
- Cancer Prevention
- Cancer Screening
- Capacity Building
- Capacity Building for NCDs in LMICs
- Capacity-Building for Applied Public Health in LMIC: A US ...
- Cardiovascular Health and Disease
- Child Labor
- Children, Air Pollution and
- Children, Injury Risk-Taking Behaviors in
- Children, Obesity in
- Citizen Advisory Boards
- Climate Change and Human Health
- Climate Change: Institutional Response
- Clinical Preventive Medicine
- Community Air Pollution
- Community Development
- Community Gardens
- Community Health Assessment
- Community Health Interventions
- Community Partnerships and Coalitions
- Community-Based Participatory Research
- Complexity and Systems Theory
- Critical Health Literacy
- Cultural Capital and Health
- Cultural Safety
- Culture and Public Health
- Definition of Health
- Dental Public Health
- Design and Health
- Dietary Guidelines
- Directions in Global Public Health Graduate Education
- Driving and Public Health
- Ecological Approaches
- Enabling Factors
- Environmental Health, Pediatric
- Environmental Laws
- Environmental Protection Agency
- Ethics of Public Health
- Evidence-Based Pediatric Dentistry
- Evidence-Based Public Health Practice
- Family Planning Services and Birth Control
- Food Safety
- Food Security and Food Banks
- Food Systems
- Frail Elderly
- Functional Literacy
- Genomics, Public Health
- Geographic Information Systems
- Geography and Health
- Global Health
- Global Health Diplomacy
- Global Health Promotion
- Global Health Security
- Guide to Community Preventive Services, The
- Health Administration
- Health Disparities
- Health Impact Assessment
- Health in All Policies
- Health in All Policies in European Countries
- Health Literacy
- Health Literacy and Noncommunicable Diseases
- Health Measurement Scales
- Health Planning
- Health Promoting Hospitals
- Health Promotion Foundations
- Health Promotion Workforce Capacity
- Health Systems of Low and Middle-Income Countries, The
- Healthy People Initiative
- Healthy Public Policy
- Hepatitis C
- High Risk Prevention Strategies
- Homelessness
- Human Rights, Health and
- Human Sexuality and Sexual Health: A Western Perspective
- IANPHI and National Public Health Institutes
- Immigrant Populations
- Immunization and Pneumococcal Infection
- Immunization in Pregnancy
- Indigenous Peoples, Public Health and
- Indigenous Populations of North America, Australasia, and ...
- Indoor Air Quality Guidelines
- Infant Mortality
- Internet Applications in Promoting Health Behavior
- Intersectoral Action
- Intersectoral Strategies in Low - Middle Income Countries ...
- Justice, Social
- Knowledge Translation and Exchange
- Knowledge Utilization and Exchange
- Law of Public Health in the United States
- Media Advocacy
- Mental Health
- Mental Health Promotion
- Migrant Health
- Migrant Worker Health
- Motor Vehicle Injury Prevention
- Multi-Drug-Resistant Tuberculosis
- Nanotechnology
- National Association of Local Boards of Health
- National Public Health Institutions
- Needs Assessment
- Needs Assessments in International Disasters and Emergenci...
- Obesity Prevention
- Occupational Cancers
- Occupational Exposure to Benzene
- Occupational Exposure to Erionite
- Occupational Safety and Health
- Occupational Safety and Health Administration (OSHA)
- Oral Health Equity for Minority Populations in the United ...
- Ottawa Charter
- Parenting and Work
- Parenting Skills and Capacity
- Participatory Action Research
- Patient Decision Making
- Pesticide Exposure and Pesticide Health Effects
- Physical Activity and Exercise
- Physical Activity Promotion
- Pneumoconiosis
- Polio Eradication in Pakistan
- Population Aging
- Population Determinants of Unhealthy Foods and Beverages
- Precautionary Principle
- Prenatal Health
- Preparedness
- Program Evaluation in American Health Education
- Program Planning and Evaluation
- Public Health, History of
- Public Health Surveillance
- Public-Private Partnerships in Public Health Research and ...
- Public-Private Partnerships to Prevent and Manage Obesity ...
- Quantitative Microbial Risk Assessment
- Racism as a Structural Determinant of Health
- Radiation Emergencies and Public Health: Impacts, Prepared...
- Randomized Controlled Trials
- Real World Evaluation Strategies
- Reducing Obesity-Related Health Disparities in Hispanic an...
- Research Integrity in Public Health
- Resilient Health Systems
- Rural Health in the United States
- Safety, Patient
- School Health Programs in the Pacific Region
- Sex Education in HIV/AIDS Prevention
- Skin Cancer Prevention
- Smoking Cessation
- Social Determinants of Health
- Social Epidemiology
- Social Marketing
- Statistics in Public Health
- STI Networks, Patterns, and Control Strategies
- Stillbirths
- Sustainable Development Goals
- Systems in the United States, Public Health
- Systems Modeling and Big Data for Non-Communicable Disease...
- Systems Theory in Public Health
- Traditional, Complementary, Alternative, and Integrative M...
- Translation of Science to Practice and Policy
- Traumatic Stress and Post-Traumatic Stress Disorder
- Tuberculosis among Adults and the Determinants of Health
- UK Public Health Systems
- Unintentional Injury Prevention
- Urban Health
- Vaccination, Mandatory
- Vaccine Hesitancy
- Vermiculite
- Violence Prevention
- Vulnerability, Intersectionality and Health in Migration
- Water Quality
- Water Quality and Water-Related Disease
- Weight Management in US Occupational Settings
- Welfare States, Public Health and Health Inequalities
- Worksite Health Promotion
- World Health Organization (WHO)
- Privacy Policy
- Cookie Policy
- Legal Notice
- Accessibility
Powered by:
- [66.249.64.20|91.193.111.216]
- 91.193.111.216
- What Are HIV and AIDS?
- How Is HIV Transmitted?
- Who Is at Risk for HIV?
- Symptoms of HIV
- U.S. Statistics
- Impact on Racial and Ethnic Minorities
- Global Statistics
- HIV and AIDS Timeline
- In Memoriam
- Supporting Someone Living with HIV
- Standing Up to Stigma
- Getting Involved
- HIV Treatment as Prevention
- Pre-exposure Prophylaxis (PrEP)
- Post-exposure Prophylaxis (PEP)
- Preventing Sexual Transmission of HIV
- Alcohol and HIV Risk
- Substance Use and HIV Risk
- Preventing Perinatal Transmission of HIV
- HIV Vaccines
- Long-acting HIV Prevention Tools
- Microbicides
- Who Should Get Tested?
- HIV Testing Locations
- HIV Testing Overview
- Understanding Your HIV Test Results
- Living with HIV
- Talking About Your HIV Status
- Locate an HIV Care Provider
- Types of Providers
- Take Charge of Your Care
- What to Expect at Your First HIV Care Visit
- Making Care Work for You
- Seeing Your Health Care Provider
- HIV Lab Tests and Results
- Returning to Care
- HIV Treatment Overview
- Viral Suppression and Undetectable Viral Load
- Taking Your HIV Medicine as Prescribed
- Tips on Taking Your HIV Medication Every Day
- Paying for HIV Care and Treatment
- Other Health Issues of Special Concern for People Living with HIV
- Alcohol and Drug Use
- Coronavirus (COVID-19) and People with HIV
- Hepatitis B & C
- Vaccines and People with HIV
- Flu and People with HIV
- Mental Health
- Mpox and People with HIV
- Opportunistic Infections
- Sexually Transmitted Infections
- Syphilis and People with HIV
- HIV and Women's Health Issues
- Aging with HIV
- Emergencies and Disasters and HIV
- Employment and Health
- Exercise and Physical Activity
- Food Safety and Nutrition
- Housing and Health
- Traveling Outside the U.S.
- Civil Rights
- Workplace Rights
- Limits on Confidentiality
- National HIV/AIDS Strategy (2022-2025)
- Implementing the National HIV/AIDS Strategy
- Prior National HIV/AIDS Strategies (2010-2021)
- Key Strategies
- Priority Jurisdictions
- HHS Agencies Involved
- Learn More About EHE
- Ready, Set, PrEP
- Ready, Set, PrEP Pharmacies
- Ready, Set, PrEP Resources
- AHEAD: America’s HIV Epidemic Analysis Dashboard
- HIV Prevention Activities
- HIV Testing Activities
- HIV Care and Treatment Activities
- HIV Research Activities
- Activities Combating HIV Stigma and Discrimination
- The Affordable Care Act and HIV/AIDS
- HIV Care Continuum
- Syringe Services Programs
- Finding Federal Funding for HIV Programs
- Fund Activities
- The Fund in Action
- About PACHA
- Members & Staff
- Subcommittees
- Prior PACHA Meetings and Recommendations
- I Am a Work of Art Campaign
- Awareness Campaigns
- Global HIV/AIDS Overview
- U.S. Government Global HIV/AIDS Activities
- U.S. Government Global-Domestic Bidirectional HIV Work
- Global HIV/AIDS Organizations
- National Black HIV/AIDS Awareness Day February 7
- HIV Is Not A Crime Awareness Day February 28
- National Women and Girls HIV/AIDS Awareness Day March 10
- National Native HIV/AIDS Awareness Day March 20
- National Youth HIV & AIDS Awareness Day April 10
- HIV Vaccine Awareness Day May 18
- National Asian & Pacific Islander HIV/AIDS Awareness Day May 19
- HIV Long-Term Survivors Awareness Day June 5
- National HIV Testing Day June 27
- Zero HIV Stigma July 21
- Southern HIV/AIDS Awareness Day August 20
- National Faith HIV/AIDS Awareness Day August 27
- National African Immigrants and Refugee HIV/AIDS and Hepatitis Awareness Day September 9
- National HIV/AIDS and Aging Awareness Day September 18
- National Gay Men's HIV/AIDS Awareness Day September 27
- National Latinx AIDS Awareness Day October 15
- World AIDS Day December 1
- Event Planning Guide
- U.S. Conference on HIV/AIDS (USCHA)
- National Ryan White Conference on HIV Care & Treatment
- AIDS 2020 (23rd International AIDS Conference Virtual)
Want to stay abreast of changes in prevention, care, treatment or research or other public health arenas that affect our collective response to the HIV epidemic? Or are you new to this field?
HIV.gov curates learning opportunities for you, and the people you serve and collaborate with.
Stay up to date with the webinars, Twitter chats, conferences and more in this section.
Schools Are Vital in the Fight Against Youth HIV Infection
- Share on Facebook
- Share on Twitter
- Share on LinkedIn
- Share on Email
Each April 10th, we recognize National Youth HIV & AIDS Awareness Day (NYHAAD) . Since 2013, this day has provided an opportunity for education and served as a reminder that our young people continue to be at risk for HIV. It is also a time to highlight the work still needed.
Schools play a critical role in promoting the health and safety of youth and hold a pivotal place in the fight to prevent HIV. Every day, more than 56 million students spend their day in school, which provides a unique opportunity to provide them with the knowledge, skills, and resources they need to prevent HIV during adolescence and into adulthood. True primary prevention includes quality health education, a connection to needed health services, and school environments that support youth and help them feel safe and connected, which can ensure their academic success.
Over the last 10 years: condom use among adolescents continued to decrease; 14% of youth report that they have used illicit drugs; more than 10% of high school females have been the victims of sexual assault; and more than 30% of students have experienced emotional distress in the last year. At the same time STDs among young people have continued to increase and 1 in 5 new HIV diagnoses were reported in young people aged 13-24 years.
CDC’s adolescent and school health program implements activities focused on primary prevention within the U.S. education system. Currently, CDC reaches approximately 2 million students by funding education agencies and a network of leaders in school-based HIV, STD, and pregnancy prevention . These funded partners:
- Deliver HIV, STD, and pregnancy prevention programs grounded in the latest research
- Select and implement effective health education curricula
- Build local capacity to connect students to school- and community-based health services , and
- Establish safe environments where students feel connected to school and supportive adults.
Over the last 5 years, these programs have increased the number of middle and high schools implementing quality sexual health education, made over 65,000 referrals for youth-friendly sexual health services, and expanded by 60% the establishment of student-led clubs dedicated to creating safe and supportive environments for all students.
Through analysis of CDC’s data on youth risk behaviors and experiences [PDF, 16.7MB] and school health policies and practices , we know that progress is being made. For example, from 2007 to 2017, CDC data showed declines in sexual risk behaviors among youth, including fewer currently sexually active high school students. There was also a decrease in the proportion of high school students who ever had sex during that same time period (from 48% in 2007 to 40% in 2017).
All youth deserve a healthy future. That is why schools, families, and communities must work together to provide safe and nurturing environments for youth. On NYHAAD, CDC joins with partners across the country to recommit to our efforts and resources to ensure that youth know how to protect themselves against HIV infection. We know what works and have the tools to provide support for all students. By providing sexual health education, health services, and safe and supportive school environments for all students, we can make a difference and help end the HIV epidemic.
Related HIV.gov Blogs
- Awareness Days
- CDC Centers for Disease Control & Prevention
- Youth Awareness Day National Youth HIV/AIDS Awareness Day
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Environ Res Public Health

Sex Education in the Spotlight: What Is Working? Systematic Review
Associated data.
The data presented in this study are available from the corresponding author on reasonable request.
Adolescence, a period of physical, social, cognitive and emotional development, represents a target population for sexual health promotion and education when it comes to achieving the 2030 Agenda goals for sustainable and equitable societies. The aim of this study is to provide an overview of what is known about the dissemination and effectiveness of sex education programs and thereby to inform better public policy making in this area. Methodology : We carried out a systematic review based on international scientific literature, in which only peer-reviewed papers were included. To identify reviews, we carried out an electronic search of the Cochrane Database Reviews, ERIC, Web of Science, PubMed, Medline, Scopus and PsycINFO. This paper provides a narrative review of reviews of the literature from 2015 to 2020. Results : 20 reviews met the inclusion criteria (10 in school settings, 9 using digital platforms and 1 blended learning program): they focused mainly on reducing risk behaviors (e.g., VIH/STIs and unwanted pregnancies), whilst obviating themes such as desire and pleasure, which were not included in outcome evaluations. The reviews with the lowest risk of bias are those carried out in school settings and are the ones that most question the effectiveness of sex education programs. Whilst the reviews of digital platforms and blended learning show greater effectiveness in terms of promoting sexual and reproductive health in adolescents (ASRH), they nevertheless also include greater risks of bias. Conclusion : A more rigorous assessment of the effectiveness of sexual education programs is necessary, especially regarding the opportunities offered by new technologies, which may lead to more cost-effective interventions than with in-person programs. Moreover, blended learning programs offer a promising way forward, as they combine the best of face-to-face and digital interventions, and may provide an excellent tool in the new context of the COVID-19 pandemic.
1. Introduction
Adolescence is a period of transition, growth, exploration and opportunities that the World Health Organization defines as referring to individuals between 10 years and 19 years of age [ 1 ]. During this life phase, adolescents undergo physical, psychological and sexual maturation and tend to develop an increased interest in sex and relationships, with positive relationships becoming strongly linked to sexual and reproductive health as well as overall wellbeing [ 2 ]. Sexual health is understood as a state of wellness comprising physical, emotional, mental, and social dimensions [ 3 ]: it represents one of the necessary requirements to achieve the general objective of sustainable and equitable societies in terms of the 2030 Agenda [ 4 ], which advocates the need for a sexual education that is anchored in a gender- and human rights-oriented perspective.
In high-income countries, sexual debut usually occurs during adolescence [ 5 ], though research suggests that sexual initiation is increasingly occurring at earlier ages [ 6 ]. Adolescents have to deal with the results of unhealthy sexual behaviors, including unplanned pregnancies and sexually transmitted infections [ 7 ], as well as experiences of sexual violence [ 8 , 9 ]. Adolescents are aware that they need more knowledge in order to enjoy healthy relationships [ 10 ], yet do not receive enough of the kind of information from parents or other formal sources that would allow them to develop a more positive, respectful experience of sexuality and sexual relationships [ 11 ].
Sexual education can be defined as any combination of learning experiences aimed at facilitating voluntary behavior conducive to sexual health. Sex education during adolescence has centered on the delivery of content (abstinence-only vs. comprehensive instruction) by teachers, parents, health professionals or community educators, and on the context (within school and beyond) of such delivery [ 12 ]. As regards content, the proponents of abstinence-only programs aim to help young adults avoid unintended pregnancies and sexually transmitted diseases (STDs), working on the assumption that while contraceptive use merely reduces the risk, abstinence will eliminate it entirely [ 13 ]. Nevertheless, an overwhelming majority of studies in this field have shown that programs advocating abstinence-only-until-marriage (AOUM) are neither effective in delaying sexual debut nor in changing other sexual risk behaviors [ 14 , 15 ], and participants in abstinence-only sex education programs consider that these had only a low impact in their lives [ 16 ]. On the other hand, holistic and comprehensive approaches to sex education go beyond risk behaviors and acknowledge other important aspects, as for example love, relationships, pleasure, sexuality, desire, gender diversity and rights, in accordance with internationally established guidelines [ 17 ], and with the 2030 Agenda [ 4 ]. Comprehensive Sexuality Education (CSE) “plays a central role in the preparation of young people for a safe, productive, fulfilling life” (p. 12) [ 17 ] and adolescents who receive comprehensive sex education are more likely to delay their sexual debut, as well as to use contraception during sexual initiation [ 18 ]. Comprehensive sexual education initiatives thereby promote sexual health in a way that involves not only the biological aspects of sexuality but also its psychological and emotional aspects, allowing young people to have enjoyable and safe sexual experiences.
With regard to context, sexual education may occur in different settings. School settings are key sites for implementing sexual education and for promoting adolescent sexual health [ 19 ], but today internet is becoming an increasingly important source of information and advice on these topics [ 20 ]. Access to the internet by adolescents is almost universal in high-income countries. The ubiquity and accessibility of digital platforms result in adolescents spending a great deal of time on the internet, and the search for information is the primary purpose of health-related internet use [ 21 ]. At the same time, this widespread use of technology by young people offers interesting possibilities for sexual health education programs, given the ease of access, availability, low cost, and the possibility of participating remotely [ 22 ]. The topics that young people search for online include information on everyday health-related issues, physical well-being and sexual health [ 23 ]. The majority of internet users of all ages in the US (80%) search online for health information including sexual health information [ 24 ], and among adolescents social media platforms are the most frequent means of obtaining information about health, especially regarding sexuality [ 25 ].
Thanks to the ubiquity and popularity of technologies, digital media interventions for sexual education offer a promising way forward, both via the internet (eHealth) and via mobile phones (mHealth, a specific way of promoting eHealth), given the privacy and anonymity they afford, especially for young people. Digital interventions in school—both inside and outside the classroom—offer interesting possibilities, because of their greater flexibility with regard to a variety of learning needs and benefits in comparison with traditional, face-to-face interventions, and because they offer ample opportunities for customization, interactivity as well as a safe, controlled, and familiar environment for transmitting sexual health knowledge and skills [ 26 ]. As Garzón-Orjuela et al. [ 27 ] argues, contemporary adolescents’ needs are mediated by their digital and technological environment, making it important to adapt interventions in the light of these realities. Online searches for sexual health information are likely to become increasingly important for young people with diminishing access to information from schools or health care providers in the midst of the lockdowns and widespread school closures during the COVID-19 pandemic [ 28 ], with more than two million deaths and 94 million people infected around the world [ 29 ]. Specifically, blended learning programs, consisting of internet-based educational interventions complemented by face-to-face interventions, may prove a significant addition to regular secondary school sex education programs [ 30 , 31 ]. Blended learning programs can be especially helpful in promoting sexual and reproductive health in the context of the COVID-19 pandemic, which is challenging the way we have so far approached formal education, with its focus on face to face interventions, given the need, now more than ever, to “develop and disseminate online sex education curricula, and ensure the availability of both in-person and online instruction in response to school closures caused by the pandemic” [ 28 ].
The present study sets out to research the dissemination and effectiveness in different settings (school, digital and blended learning) of sex education programs that promote healthy and positive relationships and the reduction of risk behaviors, so as to make current sexual health interventions more effective [ 32 ]. Numerous researchers have carried out trials and systematic reviews so as to evaluate the effectiveness of school-based sexual health and relationship education [ 19 , 27 , 33 , 34 , 35 ], as well as that of digital platform programs [ 36 , 37 , 38 , 39 ]. However, there has not been a review that is representative of the literature as a whole. Furthermore, in the reviews that have been carried out, differing aims and inclusion criteria have led to differences in the sampling of available primary studies [ 19 ]. As Garzón-Orjuela et al. [ 27 ] asserts, the field of adolescent sex education is continuously evolving and in need of evaluation and improvement. Better assessments are necessary in order to clarify whether they offer a viable and effective strategy for influencing adolescents, especially with respect to improved ASRH behaviors. Hence, given the need for an up-to-date revision so as to consider more recent emerging evidence in this field, in this study we carry out a review of reviews that includes reviews of interventions both in school settings and via digital platforms, as well as, for the first time, those that combine both formats (blended learning).
The decision to conduct a review of reviews (RoR), assessing the quality and summarizing the findings of existing systematic reviews, rather than working directly with primary intervention studies, addresses the need to include as wide a range of topics covered within the field of sex education as possible [ 40 ]. As Schackleton et al. [ 35 ] (p. 383) point out, in order to provide overviews of research evidence that are relevant to policy making, it is important “to bring together evidence on different forms of intervention and on different outcomes because it is useful for policy makers to know what is the range of approaches previously evaluated and whether these have consistent effects across different outcomes.” Carrying out and publicly sharing reviews of reviews such as the present study constitutes one way of better providing practitioners with evidence they can then carry over into their interventions [ 32 ].
2. Methodology
(1) To systematically review existing reviews of Sex Education (SE) of school-based (face-to-face), digital platforms and blended learning programs for adolescent populations in high-income countries.
(2) To summarize evidence relating to effectiveness.
2.2. Methods
The review is structured in accordance with the PRISMA checklist (Preferred Reporting Items for Systematic Reviews and Meta-Analysis) (see Figure A1 ), and the systematic review protocol has previously been published on the PROSPERO International Prospective Registry of Technical Reviews (CRD42021224537).
2.3. Search Strategy
This systematic review is based on international scientific literature and only peer- reviewed papers have been included. Only meta-analyses (publications that combine results from different studies) and systematic reviews (literature reviews that synthesize high-quality research evidence) were used for this review. Findings from reviews of reviews were not analyzed. To identify reviews, we electronically searched the Cochrane Database Reviews, ERIC, Web of Science, PubMed, Medline, Scopus and PsycINFO. After the list was completed the duplicated papers were automatically removed. Two reviewers working independently applied inclusion criteria in screening citations by titles, abstracts, and keywords to identify records for full-text review. A third reviewer reconciled any disagreement. The same procedure was carried out in screening the full text of studies selected after the title and abstract screening phase. Two reviewers then examined the full text of each article to determine which satisfied inclusion criteria. Data extraction was carried out independently by the first and second reviewer. The extracted data included specific details about the interventions, populations, study methods and outcomes significant to the review question and objective. Any discrepancies were discussed until consensus was reached. Search terms are included in Table A1 .
This RoR included the reviews published since 2015, when the United Nations decided on new Global Sustainable Development Goals, until December 2020. The 2030 Agenda for Sustainable Development [ 4 ] takes into account the relevance of Sexual Health to achieve peace and prosperity.
2.4. Inclusion Criteria
We extracted data using a “Population, Intervention, Comparison, Outcome” structure, PICO [ 41 ].
Population: Reviews of interventions targeting adolescents (aged 10–19 years), school-setting, digital platforms or blended learning education were eligible for inclusion. Reviews in which studies of interventions targeted youth and adults were eligible if the primary studies included people between the ages of 10–19 years.
Intervention: Reviews of interventions developed in school-setting (school-based), digital (digital platforms) or blended learning programs were included. Interventions based on multiple settings or targeted multiple health-related issues were only considered for inclusion if any primary studies were linked to school-based, digital or blended learning interventions, as well as targeting Sexual and Reproductive Health (SRH).
Comparison groups: Randomized controlled trials (RCTs) and studies using a quasi-experimental design (including non-randomized trials—nRCTs). Single group, pre- and post-test research designs, group exposed to sexual education (SE) program (school-based, digital platforms or blended learning) compared with non-exposed control group or another intervention.
Outcomes: Primary outcomes: (1) Sexual behavior and (2) Health and social outcomes related to sexual health. Secondary outcomes: (1) Knowledge and understanding of sexual health and relationship issues and (2) Attitudes, values and skills.
2.5. Exclusion Criteria
Reviews were excluded if:
- Their primary focus was adult people and adolescents were not included.
- Their primary focus was sexual-health screening, sexual abuse or assault or prevention of sexual abuse or rape.
- The studies targeted specific populations (e.g., pre-pubertal children, children with developmental disorders, migrant and refugee, or sexual minorities).
- The interventions focused on low- and middle-income countries or if high income countries were not included in the study.
- Recipients were professionals, teachers, parents or a combination of the latter.
2.6. Risk of Bias and Assessment of Study Quality
Review quality was assessed by the first author using the AMSTAR II checklist [ 42 ]. This is an updating and adaptation of AMSTAR [ 43 , 44 ] which allows a more detailed assessment of systematic reviews that include randomized or non-randomized studies of healthcare interventions, or both. It consists of a 16-item tool (including 5 critical domains) assessing the quality of a review’s design, its search strategy, inclusion and exclusion criteria, quality assessment of included studies, methods used to combine the findings, likelihood of publication bias and statements of conflict of interest. The maximum quality score is 16.
2.7. Data Synthesis
After manually coding the papers and extracting relevant data, we used a narrative/descriptive approach for data synthesis to summarize characteristics of the studies included. Considering the heterogeneity of outcomes, their measures and research designs, meta-analysis of all the studies included was not carried out. Two researchers were involved in data synthesis. Discrepancies were resolved through discussion, and a third researcher was consulted to resolve any remaining discrepancies. For the classification of the information and presentation of the effects of the interventions reported, data was separated (school setting, digital platforms or blended learning) and structured around population, intervention, comparison, and outcome. To address the main review questions, data was synthesized in two phases. Phase 1 addressed the first question, the description of sex education/sexual health interventions. Phase 2 addressed the second question, the effectiveness and benefit of the interventions; studies with a low risk of bias were highlighted, so as to strengthen the reliability of findings (AMSTAR II) [ 42 ].
3.1. Results of Search
Our searches yielded 1476 unique citations. After excluding 776 records based on title and abstract screening, we reviewed 217 full-text articles for eligibility, of which 20 ultimately met inclusion criteria, and proceeded to data extraction. Of the 197 studies that we excluded after full-text review, 82 were carried out in low- and middle-income countries, 47 targeted exclusively adults, 56 dealt with minority groups, and 12 targeted exclusively pre-teen students.
3.2. Risk of Bias in Included Studies
According to the AMSTAR II quality assessment tool’s developers [ 42 ] scores may range from 1 to 16: in this case only 2 reviews scored 16 out of 16: 1 in a school setting [ 45 ], and 1 on a digital platform [ 46 ]. 6 of the 20 systematic reviews were of high quality: 5 in school settings [ 45 , 47 , 48 , 49 , 50 ], and 1 in digital platforms [ 46 ]; there was one study of medium quality in a school setting [ 51 ]. The remaining studies were of low or very low quality (N = 13). It is possible that low quality reviews may not provide reliable evidence, so those scoring in low and critically low quality should be regarded skeptically.
3.3. Reviews Included
Key information regarding the 20 reviews included is shown in Table A2 and Table A3 .
3.3.1. Setting
Ten studies (50%) dealt with school-based interventions [ 45 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 ], 9 (45%) referred to online interventions [ 46 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 63 ] and 1 (5%) was a review of blended learning programs [ 64 ]. In total 491 studies were included in the 20 reviews covered by the present RoR. The 10 reviews of school setting interventions include a total of 266 studies (54%), the 9 reviews of online interventions cover a total of 216 (44%) studies, and the only review of blended learning interventions includes a total of 9 studies (2%). All studies were conducted in high-income economies following the World Bank classification [ 65 ], including US samples in 16 of the 20 studies, although there are two studies in which the country of the sample is not identified [ 51 , 52 ]. Most of the studies evaluating interventions in school settings also include developing countries (low- and middle-income economies) [ 45 , 47 , 50 , 52 , 53 , 55 ], as is also the case in three reviews of online interventions [ 46 , 61 , 62 ] (see Table A2 ).
3.3.2. Population
The targeted age for reviews in school settings, as shown in Table A2 , is the period of adolescence, from 10 to 19 years of age, though one of the studies covers ages from 7 to 19 years [ 53 ]. All the online studies also include young adults (20–24 years old), alongside the adolescent sample [ 46 , 56 , 57 , 59 , 60 , 61 , 62 , 63 ], whilst the review by DeSmet et al. [ 58 ] extends the upper limit to 29 years of age. Along with the sample of adolescents and young adults, the blended learning studies review also incorporates adults of over 25 years of age [ 64 ].
3.3.3. Interventions/Types of Study
All the studies included in this review of reviews used randomized controlled trials (RCTs), non-randomized controlled trials (non-RCT), and a quasi-experimental design or a pre-test/post-test design to examine program effects.
3.3.4. Outcomes
The term “sexual outcomes” refers to the attitudes, behaviors, and experiences of adolescents consequent to their sex education [ 14 ] (p. 1), and an extensive range of variables was included (see Table A2 ): knowledge (e.g., knowledge of contraceptive effectiveness or effective method use); attitudes (e.g., about sex and reproductive health); beliefs (e.g., self-efficacy); skills (e.g., condom skills); intentions/motivation (e.g., use of birth control methods; condom use); behaviors (e.g., sexual debut; condom use; contraception use; intercourse; initiation of sexual activity) and; other outcomes related to sexual behavior (e.g., pregnancy prevalence; number of partners; rates of sexually transmissible infections (STIs); cervical screening; appreciation of sexual diversity; dating and intimate partner violence prevention; sexual violence).
3.3.5. Country of Review
Of the 10 reviews of interventions in school settings, the authors are from the USA in 7 reviews [ 47 , 48 , 49 , 50 , 53 , 54 , 55 ], from the United Kingdom in 1 [ 45 ], from Australia in 1 [ 51 ], and from Thailand in 1 [ 52 ]. Of the 9 reviews of interventions in digital settings, the authors are from the United States in 3 reviews [ 59 , 60 , 63 ], from the United Kingdom in 2 [ 46 , 56 ], from Australia in 1 [ 62 ], from Belgium in 1 [ 58 ], from France in 1 [ 61 ] and from Turkey in 1 [ 57 ]. The authors of the blended learning review are from the USA [ 64 ].
3.3.6. Year of Last Paper Included
The studies cited in the reviews that met the inclusion criteria for this review were published over a wide range of years (between 1981–2019), although only one [ 61 ], with articles published up to and including 2019 was published later than 2017. Of these, 3 were carried out in school settings [ 49 , 51 , 53 ], and 1 on digital platforms [ 46 ].

3.3.7. Search Tools
All reviews include more than 2 tools to carry out the search, in a range of 3–12, and in 7 of them the review of gray literature was included.
3.3.8. Multicenter Studies and Number of Studies Included
All reviews from school settings are multicenter, except that of Mirzazadeh et al. [ 49 ], which includes only one North American sample. The same is true for the blended learning review [ 64 ] and for the reviews of digital platforms, except for the reviews by Bailey et al. [ 56 ], L´Engle et al. [ 60 ], and Widman et al. [ 63 ]. Regarding the number of countries included in the reviews, the range in the school-setting reviews is from 1 to 11, in digital platforms reviews from 1 to 16, and in the only review of blended learning, 3. As for the range of studies included, in the reviews in school setting the range is between 8 and 80, in digital platforms, between 5 and 60, and in the only review of reviews of blended learning 9 studies were included.
3.3.9. Number of Reviews Covered That Include Meta-Analysis
As for the number of reviews that carry out a meta-analysis, there are 8 in total: 4 in school settings [ 45 , 48 , 49 , 55 ] and 4 on digital platforms [ 43 , 46 , 56 , 58 ], while in the only review of blended learning there is no meta- analysis.
3.4. Effectiveness
3.4.1. school settings.
Half of the reviews conclude that interventions are not effective in promoting healthy sexual behaviors and/or reducing risks [ 45 , 47 , 48 , 49 , 50 ]. These reviews are of high quality and with a reduced risk of bias (see Table A4 ), so that the results are highly reliable, even though in most of the studies cited the risk of bias was judged to be high and the quality of evidence was low or very low. These reviews include those of the Marseille et al. [ 48 ] and Mirzazadeh et al. [ 49 ] team, who in two studies—each led by one of the two authors—analyze, on the one hand, the effectiveness of school-based teen pregnancy prevention programs [ 48 ], and, on the other hand, the effectiveness of school-based programs prevent HIV and other sexually transmitted infections in North America [ 49 ]. The results of the studies question the usefulness of interventions carried out in schools to prevent both unwanted pregnancies and the incidence of HIV and other sexual transmitted infections in adolescents in North America. In addition to these results, those of Lopez et al. [ 47 ] focus on analyzing the effectiveness of programs implemented in schools to promote the use of contraceptive methods and conclude that many trials reported contraceptive use as an outcome but did not take into consideration whether contraceptive methods and their relative effectiveness were part of the content. For its part, the review by Mason-Jones et al. [ 45 ] also concludes that the educational programs covered had no significant effect as regards the prevalence of HIV or other STIs (herpes simplex virus, moderate evidence and syphilis, low evidence), nor was there any apparent effect in terms of the number of pregnancies at the end of the trial (moderate evidence). Finally, the review by Oringanje et al. [ 50 ] finds only limited evidence for program effects on biological measures, and inconsistent results for behavioral (secondary) outcomes across trials and concludes that it was only the interventions which combined education and contraception promotion (multiple interventions) that led to a significant reduction in unintended pregnancies over the medium- and long-term follow-up period.
In contrast to these negative results in terms of the effectiveness of the programs implemented in the school environment (identified in 5 of the 10 reviews included), 3 of the 10 reviews concluded that the programs evaluated were mostly effective in promoting knowledge, attitudes and/or in reducing risk behaviors [ 51 , 52 , 53 ] whilst programs were effective in terms of some of the primary outcomes in the reviews by Haberland et al., [ 54 ], and Peterson et al. [ 55 ]. However, these data must be taken with caution since the level of bias in these reviews—excepting that of Kedzior et al. [ 51 ] with a medium quality level—is at a low or critically low-quality level. In the review by Chokprajakchad et al. [ 52 ], 22 programs reviewed were effective in changing targeted adolescent psychosocial and/or behavioral outcomes, in 12 of 17 studies evaluating delay in the initiation of sexual intercourse, the programs were effective and many of the reviewed studies demonstrated impacts on short-term outcomes, such as knowledge, attitudes, perception and intention. The review by Goldfarb et al. [ 53 ] identifies changes in appreciation of sexual diversity, dating and intimate partner violence prevention, healthy relationships, child sex abuse prevention and additional outcomes. According to the review by Kedzior et al. [ 51 ], focused on studies promoting social connectedness with regard to sexual and reproductive sexual health, the programs reviewed improved condom use, delayed initiation of sex, and reduced pregnancy rates. Additionally, in this review, program effectiveness was influenced by ethnicity and gender: greater improvements in condom use were often reported among African American students. For its part, in the study by Peterson et al. [ 55 ] the meta-analysis of three randomized trials provided some evidence that school-environment interventions may contribute to a later sexual debut while their narrative synthesis of other outcomes offered only mixed results.
Finally, the review by Haberland et al. [ 54 ], which focused on studies analyzing whether addressing gender and power in sexuality education curricula is associated with better outcomes, concluded that where interventions addressed gender or power (N = 10/22) there was a fivefold greater likelihood of effectiveness than in those that did not.
3.4.2. Online Platforms
The reviews included show a very diverse panorama of digital platforms used to carry out educational interventions (e.g., websites, social media, gaming, apps or text messaging and mailing), which makes it difficult to compare the results. Of the 9 reviews of studies included, only one—in which the effects of TCCMD (Targeted Client Communication delivered via Mobile Devices) are evaluated [ 46 ]—meets the quality criteria according to the AMSTAR II quality assessment tool [ 42 ] (see Table A4 ); the rest include biases that limit the reliability of the results so that these must be taken with caution. In the studies reviewed by Palmer et al. [ 46 ] among adolescents nine programs were delivered only via text messages; four programs used text messages in combination with other media (for example, emails, multimedia messaging, or voice calls); and one program used only voice calls.
When compared with more conventional approaches, interventions that use TCCMD may increase sexual health knowledge (low certainty evidence), and may modestly increase contraception use (low certainty evidence) while the effect on condom use remains unclear given the very low certainty evidence. Additionally, when compared with digital non-targeted communication, the effects TCCMD on sexual health knowledge, condom and contraceptive use are also unclear, again given the very low-certainty evidence. The review finds evidence of a modest beneficial intervention effect on contraceptive use among adolescent (and adult) populations, but that there was insufficient evidence to demonstrate that this translated into a reduction in contraception.
Most of the reviews included refer to changes to a greater or lesser extent [ 56 , 57 , 59 , 60 , 62 , 63 ], while no changes determined by the intervention were identified in the study by DeSmet et al. [ 58 ]. Finally, the review by Martin et al. [ 61 ] does not include details about changes as a result of the programs.
The review by L´Engle et al. [ 60 ] assesses mHealth mobile phone interventions for ASRH (almost all of which were carried out via SMS platforms, with the notable exception of only four of the programs covered which used other media formats instead of or as well as SMS). The interventions reviewed set out to foster positive and preventive SRH behaviors, augment take-up and continued use of contraception, support medication adherence for HIV-positive young people, support teenage parents, and encourage use of health screening and treatment services. Results from the studies covered in the review offer support for diverse uses of mobile phones in order to help further ASRH. The health promotion programs that made use of text messaging demonstrated robust acceptability and relevance for young people globally and contributed to improved SRH awareness, less unprotected sex, and more testing for STIs. However, the review also found that improved reporting on essential mHealth criteria is necessary in order to understand, replicate, and scale up mHealth interventions. Holstrom’s [ 59 ] review, focused on evaluations of internet-based sexual health interventions, finds that these were associated with greater sexual health knowledge and awareness, lower rates of unprotected sex and higher rates of condom use, as well as increased STI testing. Moreover, the review explores young people’s continuing use of and trust in internet as a source of information about sexual health, as well as the particular themes that interest them. Specifically, the study finds that young people want to know not only about STIs, but also about sexual pleasure, about how to talk with partners about their sexual desires, as well as about techniques to better pleasure their partners.
The review by Widman et al. [ 63 ] reveals a significant weighted mean effect of technology-based interventions on condom use and abstinence, the effects of which were not affected by age, gender, country, intervention, dose, interactivity, or program tailoring. The effects were more significant when evaluated with short-term (one to five months) follow-ups than with longer term (over six months) ones. Moreover, digital programs were more effective than control programs in contributing to sexual health knowledge and safer sex norms and attitudes. This meta-analysis, drawing on fifteen years of research into youth-oriented digital interventions, is clear evidence of their ability to contribute to safer sex behavior and awareness. In the review by Wadham et al. [ 62 ] the majority of studies used a web-based platform for their programs (16 out of 25). These web-based programs varied between complex, bespoke multimedia interventions to more simplified educational modules. Five studies employed SMS platforms both via mobile phone messaging and web-based instant message services. Three of the programs used social networking sites, either for live chat purposes or alongside a web-based platform. Several studies showed that variety in terms of media and platforms was associated with stronger positive responses among participants and improved outcomes. Eleven of the twenty-five studies focused specifically on HIV prevention, with seven finding a statistically significant effect of the program with regard to knowledge levels about prevention of HIV and other STIs, as well as about general sexual health knowledge. However, only twenty percent of the programs that assessed intended use of condoms reported significant effects due to the intervention.
The review by Bailey et al. [ 56 ] (p. 5) assesses interactive digital interventions (IDIs), defined as “digital media programs that provide health information and tailored decision support, behavioral-change support and/or emotional support” and focuses on the sexual well-being of young people between the ages of thirteen and twenty four in the United Kingdom. IDIs have significant though small effects on self-efficacy and sexual behavior, although there is not sufficient evidence to ascertain the effects on biological outcomes or other longer-term impacts. When comparing IDIs with in-person sexual health programs, the former demonstrate significant, moderate positive effects on sexual health knowledge, significant small effects on intention but no demonstrable effects on self-efficacy. The review by Celik et al. [ 57 ] looks at digital programs (the majority internet- and computer-based with only six making use of mobile phone-based applications) and sets out to understand their effectiveness in changing adolescents’ health behaviors. Findings from the studies ( n = 9) suggest that the digital interventions carried out with the adolescents generally had a positive effect on health-promoting behaviors. However, in another study focused on fostering HIV prevention [ 66 ], there was a statistically significant increase in health-promoting behavior in only one of the four studies reviewed.
In the review by DeSmet et al. [ 58 ], no significant behavioral changes as a result of the interventions for sexual health promotion using serious digital games are identified, although the interventions did have significant though small positive effects on outcomes. The fact that so few studies both met the inclusion criteria and also analyzed behavioral effects suggests the need to further investigate the effectiveness of this kind of game-based approach.
Finally, in the review by Martin et al. [ 61 ] 60 studies were covered, detailing a total of 37 interventions, though only 23 of the reviews included effectiveness results. A majority of the interventions were delivered via websites ( n = 20) while online social networks were the second most favored medium ( n = 13), mostly via Facebook ( n = 8). The programs under review favored online interaction, principally amongst peers ( n = 23) but also with professionals ( n = 16). The review concludes that ASHR programs promoting these kinds of online participation interventions have demonstrated feasibility, practical interest, and attractiveness, though their effectiveness has yet to be determined, given that they are still in the early stages of design and evaluation.
3.4.3. Blended Learning
In the only blended learning review included in our study [ 64 ], the authors conclude that blended learning approaches are being successfully applied in ASHR interventions, including in school-based programs, and have led to positive behavioral and psychosocial changes. However, these results should be treated with caution as the review does not follow the guidelines recommended in the AMSTAR II quality assessment tool [ 44 ] (see Table A4 ) and only includes nine studies.
4. Discussion
The present review of reviews assesses, for the first time jointly to our knowledge, the effectiveness of sexual education programs for the adolescent population (ASRH) developed in school settings, digital platforms and blended learning. Of the twenty reviews included (comprising a total of 491 programs, mostly from the USA), ten correspond to reviews of programs implemented in school settings, nine to those dealing with interventions via digital platforms and only one deals with studies relating to blended learning. Twelve (60%) of the reviews included (6 out of 10 in school settings, 5 out of 9 on digital platforms, and the only blended learning review) have been published in the last 3 years (between 2018 and 2020). Thus, the present study constitutes the most up-to-date and recent review of reviews incorporating several contemporary studies not covered by earlier reviews [ 19 , 27 , 33 , 35 , 36 , 37 , 38 , 39 ].
4.1. Interventions Reviewed
The interventions included in the reviews covered by our study were largely focused on reducing risk behaviors (e.g., VIH/STIs and unwanted pregnancies), and envisaging sex as a problem behavior. Programs reviewed often focused on the physical and biological aspects of sex, including pregnancy, STIs, frequency of sexual intercourse, use of condom, and reducing adolescents´ number of sexual partners. One exception is Golfard’s et al. [ 53 ] review about comprehensive sex education, which is centered on healthy relationships and sexual diversity, though it also makes reference to prevention of violence (dating and intimate partner violence prevention and sex abuse prevention). However, Golfard’s et al.’s [ 53 ] rejects more than 80% of the studies initially reviewed because they were focused solely on pregnancy and disease prevention. In the reviews of interventions on digital platforms and via blended learning all the outcomes focused on behaviors related to sexual health (focused on the prevention of risk behaviors), and in several cases also addressed perceived satisfaction and usability. These results are in line with other studies that confirm the over-attention given to risk behaviors, to the detriment of other more positive aspects of sexuality [ 67 , 68 ]. Teachers continue to perceive their responsibility as combating sexual risk, whilst viewing young people as immature and oversexualized [ 69 ], even as adolescents themselves express a preference for sex education with less emphasis on strictly negative sexual outcomes [ 16 ], and more emphasis on peer education [ 70 ].
As for more positive views of sexuality, only on rare occasions do interventions address issues such as sexual pleasure, desire and healthy relationships. Desire and pleasure were not included in the outcome evaluations for school settings, nor for digital and blended learning programs included in this review: again this is in line with the position of other authors cited in the present study, who advocate the need to also embrace the more positive aspects of sexuality [ 53 , 56 ]. Specifically, Bailey and colleagues [ 56 ] (p. 73) suggest as “optimal outcomes” social and emotional well-being in sexual health. Young people want to know about more than STIs, they also “want information about sexual pleasure, how to communicate with partners about what they want sexually and specific techniques to better pleasure their partners” [ 59 ] (p. 282). Similarly, Kedzior et al. [ 51 ] also argue for the need to move beyond a risk-aversion approach and towards one that places more emphasis on positive adolescent sexual and reproductive health.
Pleasure and desire are largely absent within sex and relationship education [ 71 ] and, when they are included, they are often proposed as part of a discourse on safe practice, where pleasure continues to be equated with danger [ 72 ]. The persistent absence of a “discourse of desire” in sex education [ 73 , 74 ] is especially problematic for women, for whom desire is still mediated by (positive) male attention, and for whom pleasure is derived from being found desirable and not from sexual self-expression or from their own desires [ 75 ]. Receiving sexualized attention from men makes women “feel good” by increasing their self-esteem and self-confidence [ 76 ]. However, it is still men who decide what is sexy and what is not, based on the attention they pay to women “girl watching”, [ 77 ] (p. 386), which leads the latter to self-objectify [ 78 ] with all the attendant negative consequences for their overall and sexual health [ 79 ]. In fact, women experience “pushes” and “pulls” [ 80 ] (p.393) with regard to sexualized culture. In one sense, the sexualization of culture has placed women in the position of subjects who desire, not just that of subjects who are desired, but at the same time it becomes a form of regulation in which young women are forced to assume the current sexualized ideal [ 81 , 82 ] in order to position themselves as “modern, liberated and feminine,” and avoid being seen as “outdated or prudish” [ 83 ] (p. 16). Koepsel [ 84 ] provides a holistic definition of pleasure as well as clear recommendations for how educators can overcome these deficits by incorporating pleasure into their existing curricula. At present, sexual education is still largely centered on questions of public health, and there is as yet no consensus on criteria for defining sexual well-being and other aspects of positive sexuality [ 85 ]. Patterson et al. [ 86 ] argue for the need to mandate “comprehensive, positive, inclusive and skills-based learning” to enhance people´s ability to develop healthy positive relationships throughout their lives.
The absence of desire and pleasure in the outcomes of the evaluated reviews is connected with the absence of gender-related outcomes. Only one of the reviews addresses the issue of gender and power in sexuality programs [ 54 ], illustrating how their inclusion can bring about a five-fold increase in the effectiveness of risk behavior prevention. Nonetheless, men are far less likely than women to sign up for a sexuality course, and as a result of masculine ideologies many young males experience negative attitudes towards sex education [ 87 ]. To date we still have little idea as to what are the “active ingredients” that can contribute to successfully encouraging men to challenge gender inequalities, male privilege and harmful or restrictive masculinities so as to help improve sexual and reproductive health for all [ 88 ] (p.16). Schmidt et al.’s [ 89 ] review looks at 10 evidence-based sexual education programs in schools: the majority discuss sexually transmitted diseases and unplanned pregnancy, abstinence, and contraceptive use, while very few address components related to healthy dating relationships, discussion of interpersonal violence or an understanding of gender roles.
The International Guidance on Sexuality Education [ 90 ], and the International Technical Guidance on Sexuality Education [ 17 ] promote the delivery of sexual education within a framework of human rights and gender equality to support children and adolescents in questioning social and cultural norms. The year 2020 marked the anniversaries of several path breaking policies, laws and events for women’s rights: the 100th anniversary of women´s suffrage in the United States; the 25th anniversary of the Beijing Platform for Action, a global roadmap for women´s empowerment; and, the 20th anniversary of the United Nations Security Council Resolution for a Women, Peace and Security agenda. Although there have been important advances in recent years in research relating to the inclusion of gender equality and human rights interventions in ASRH policies and programming still “fundamental gaps remain” [ 40 ] (p.14). Gender equality, and to an even greater extent human rights, have had very little presence in sexual and reproductive health programs and policies, and there is a pressing need to do more to address these issues systematically. Specifically, issues such as abortion and female genital mutilation, with clear repercussions in terms of gender equality and human rights, are rarely dealt with [ 40 ].
Furthermore, sexual education that privileges heterosexuality reinforces hegemonic attributes of femininity and masculinity, and ignores identities that distance themselves from these patterns. Our collective heteronormative legacy marginalizes and harms LGB families [ 91 ] and LGBTQ+-related information about healthy relationships is largely absent from sexual and reproductive health programs [ 92 ]. Students want a more LGBTQ+ inclusive curriculum [ 92 ]: in the present RoR one review [ 53 ] addresses the issue of non-heteronormative identity in sexuality programs with significant results; and other authors are exploring promising initiatives which are also challenging this lack of inclusivity [ 93 ] and rectifying heterosexual bias [ 94 ]. However, unfortunately, the underlying neoliberal focus of the majority of contemporary sexuality education militates to assimilate LGBTQ+ people into existing economic and social normative frameworks rather than helping disrupt them [ 95 ].
4.2. Effectiveness
This present review of reviews shows a variety of types of sexual health promotion initiatives across the three settings (school-based, digital and blended learning), with inconsistent results. The reviews with lower risk of bias are those carried out in school settings and those that are most critical regarding the effectiveness of programs promoting ASRH, both in the prevention of pregnancies and of HIV/STIs. Reviews dealing with digital platforms and blended learning show greater effectiveness in terms of promoting adolescent sexual health: however, these are also the studies that incorporate the highest risks of bias. Specifically, in digital platforms programs the great variety of alternatives makes comparability difficult. Moreover, these programs, along with blended learning, are in a more incipient state of evaluation, compared to school-setting evaluations, and present greater risks of lower quality than reviews in school settings.
The results of the present RoR are in line with those of previous RoRs [ 19 , 32 ]. The review of reviews by Denford et al.s´ [ 19 ] RoR covered 37 reviews up to 2016 and summarized 224 primary randomized controlled trials: whilst it concludes that school-based programs addressing risky sexual behavior can be effective, its reviews of exclusively school-based studies offer mixed results as to effectiveness in relation to attitudes, skills and behavioral change. Some of those studies report positive effects while others find there are no effects, if not even negative effects, in terms of the aforementioned outcomes [ 19 ]. As regards pregnancy, programs appear to be effective at increasing awareness regarding STIs and contraception but overall the findings suggest that the impact of these interventions on attitudes, behaviors and skills variables are mixed, with some studies leading to improvements whilst others show no change. Moreover, the fact that community-based programs were also taken into consideration might have led to the effectiveness of school-based programs being exaggerated [ 19 ].
However, although in our RoR the higher quality/lower bias studies—in keeping with the findings of previous reviews [ 19 , 33 ]—fail to show a clear pattern of effectiveness, the interventions could nevertheless be generating changes as Denford et al. [ 19 ] suggest, though not in the measured outcomes, bearing in mind the low incidence of sexual intercourse and pregnancy in school-going adolescents.
With regard to school settings, Peterson et al. [ 55 ] conclude that further, more rigorous evidence is necessary to evaluate the extent to which interventions addressing school-related factors are effective and to help better understand the mechanisms by which they may contribute to improving adolescent sexual health. With regard to digital platform programs, Wadham et al. [ 62 ] (p. 101) argue that “although new media has the capacity to expand efficiencies and coverage, the technology itself does not guarantee success.” An interesting observation in their review was that interventions which were either web-based adaptations of prior prevention programs, or were theory-based or had been developed from models of behavioral change appeared effective independently of the chosen digital media mode. However, digital programs are still in the early stages of design and evaluation, especially in terms of the effects of peer interaction and often diverge from existing theoretical models [ 61 ] (p. 13). The expert opinion-based proposal of the European Society for Sexual Medicine [ 96 ] argues that e-sexual health education can contribute to improving the sexual health of the population it seems the future of CSHE is moving towards smartphone apps [ 97 ].
However, “despite clear and compelling evidence for the benefits of high-quality curriculum-based CSE, few children and young people receive preparation for their lives that empowers them to take control and make informed decisions about their sexuality and relationships freely and responsibly” [ 17 ] (p. 12), and during “the current public health crisis, the sexual and reproductive health of adolescents and young adults must not be overlooked, as it is integral to both their and the larger society’s well-being” [ 28 ] (p. 9). In the light of these challenges, Coyle et al.’s [ 64 ] suggestion that the blended learning model may end up achieving a far more dominant role in the future of sexual education acquires even more relevance.
4.3. Limitations
This study represents the first review of reviews, as far as we are aware, in which the effectiveness of sex education programs in different settings (school-based, digital and blended learning) is evaluated, using a rich methodology and providing interesting conclusions. However, the present review of reviews is not without its limitations.
While systematic reviews and reviews of reviews can offer a way synthesizing large amounts of data, the great heterogeneity and diversity of measured outcomes make it difficult to establish a synthesis of the results, even more so in cases where it is not possible to apply meta-analysis. Furthermore, the quality of reviews of reviews is limited by that of the reviews they include and RoRs do not necessarily represent the leading edge research in the field.
In addition, although we searched for a wide range of keywords on the most commonly used databases in the field of health (namely ERIC, Web of Science, PubMed, and PsycINFO) to identify relevant papers, it is possible that the choice of keywords and database may have resulted in our omitting some relevant studies. Moreover, our review has focused on articles in international journals published in English, allowing us access to the most rigorous peer-reviewed studies and to those with greater international diffusion, given that English is the most frequently used language in the scientific environment: notwithstanding, this has also limited the scope of our review by precluding research published in other languages and contexts. Nor have documents that could have been found in the gray literature been included, given that only peer-reviewed studies have been considered for inclusion.
It is worth remembering moreover that most of the data on the outcomes of the studies included are self-reported, with mention of only occasional biological outcomes, which may limit the reliability of the effectiveness results. This represents another interesting reflection on the way in which the evaluation of the effectiveness of programs on sexual education is being carried out, and alerts us to the need for change.
Finally, it should be noted that this review of reviews is focused on adolescents from high-income countries, and our results show that studies carried out in the United States are largely overrepresented, since it is the country that provides the highest number of samples, especially in school settings: this may give rise to bias when it comes to generalizing from these results. Once again, this raises another necessary reflection on the capitalization that studies focused on American samples are having in the construction of the body of scientific knowledge on sexual and reproductive behavior, when in reality sexuality is conditioned by socio-economic variables that require a far-more multicultural and world-centric approach.
5. Conclusions
This review of reviews is the first to assess jointly the effectiveness of school-based, digital and blended learning interventions in ASRH in high-income countries. The effectiveness of the sex education programs reviewed mostly focused on the reduction of risky behaviors (e.g., STI or unwanted pregnancies) as public health outcomes; however, pleasure, desire and healthy relationships are outcomes that are mostly conspicuous by their absence in the reviews we have covered. Nonetheless, the broad range of studies included in this RoR, with their diversity of settings and methods, populations and objectives, precludes any easily drawn comparisons or conclusions. The inconsistent results and the high risk of bias reduce the conclusiveness of this review, so a more rigorous assessment of the effectivity of sexual education programs is pending and action needs to be taken to guarantee better and more rigorous evaluations, with sufficient human and financial resources. Schools and organizations need technical assistance to build the capacity for rigorous program planning, implementation and evaluation [ 98 ]. To this end, there are already examples of interesting proposals, such as that of the Working to Institutionalize Sex Education (WISE) Initiative, a privately funded effort to help public school districts develop and deliver comprehensive sexuality programs in the USA [ 99 ].
The extent of the risks of bias identified in the reviews and studies covered by this RoR points to an important conclusion, allowing us to highlight the precariousness that characterizes the evaluation of sexual education programs and the consequent undermining of public policy oriented to promoting ASRH. Public policies that promote ASRH are of vital importance when it comes to minimizing risks related to sexual behavior, and maximizing healthy relations and sexual well-being for the youngest members of our society.
Above all it is important to recognize the opportunities afforded by new technologies, so ubiquitous in the lives of young people, since they allow for programs that are far more cost-effective than traditional, in-person interventions. Finally, blended learning programs are perhaps even more promising, given their combination of the best of face-to-face and digital interventions, meaning they provide an excellent educative tool in the new context of the COVID-19 pandemic, and may even become the dominant teaching model in the future.

Flow diagram Preferred reporting items for systematic reviews and meta-analysis, PRISMA).
Search Terms Used.
Description of studies.
Characteristics and main results of the studies included.
Evaluation of the studies included (AMSTAR II).
1 1. Did the research questions and inclusion criteria for the review include the components of PCIO?; 2. Did the report of the review contain an explicit statement that the review methods were established prior to the conduct of the review and did the report justify any significant deviations from the protocol?; 3. Did the review authors explain their selection of the study designs for inclusion in the review?; 4. Did the review authors use a comprehensive literature search strategy?; 5. Did the review authors perform study selection in duplicate?; 6. Did the review authors perform data extraction in duplicate?; 7. Did the review authors provide a list of excluded studies and justify the exclusions?; 8. Did the review authors describe the included studies in adequate detail?; 9. Did the review authors use a satisfactory technique for assessing the risk of bias (RoB) in individual studies that were included in the review?; 10. Did the review authors report on the sources of funding for the studies included in the review?; 11. If meta-analysis was performed, did the review authors use appropriate methods for statistical combination of results?; 12. If meta-analysis was performed, did the review authors assess the potential impact of RoB in individual studies on the results of the meta-analysis or other evidence synthesis?; 13. Did the review authors account for RoB in primary studies when interpreting/discussing the results of the review?; 14. Did the review authors provide a satisfactory explanation for, and discussion of, any heterogeneity observed in the results of the review?; 15. If they performed quantitative synthesis did the review authors carry out an adequate investigation of publication bias (small study bias) and discuss its likely impact on the results of the review?; 16. Did the review authors report any potential sources of conflict of interest, including any funding they received for conducting the review? 2 H = Hight; M = Media; C = Low; CL = Critically Low. N = No; Y = Yes.
Author Contributions
Conceptualization, M.L.-F. and R.M.-R.; methodology, M.L.-F.; R.M.-R.; Y.R.-C. and M.V.C.-F.; formal analysis, M.L.-F.; R.M.-R.; Y.R.-C. and M.V.C.-F.; investigation, M.L.-F.; R.M.-R.; Y.R.-C. and M.V.C.-F.; writing—original draft preparation, M.L.-F. and R.M.-R.; writing—review and editing, M.L.-F.; R.M.-R., and Y.R.-C. and.; supervision, M.L.-F.; R.M.-R.; Y.R.-C. and M.V.C.-F. All authors have read and agreed to the published version of the manuscript.
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Data availability statement, conflicts of interest.
The authors declare that they have no conflicts of interest.
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Sex Ed in Schools: What Parents Need to Know
Comprehensive sex education can help reduce rates of sexually transmitted infections and promote healthy relationships.
What to Know About Sex Ed in K-12 Schools

Getty Images
Sex education in schools can be taught by a classroom teacher, school nurse or an outside speaker, and often begins in fifth grade.
For some parents, the term "sex ed" conjures memories of dated videos and cringe-inducing lessons on puberty or how babies are made.
But a good school-based sex education curriculum should be much more than that, encompassing multiple issues related to human growth and development, experts say. In addition to basic facts about puberty, sex and contraception, lessons can cover topics like healthy relationships, sexual violence prevention, body image, sexual orientation and gender identity.
"Just because you teach a young person about how to stay safe and what sex and sexuality is, you're not encouraging them to become sexually active," says Michelle Slaybaugh, director of social impact and strategic communications at SIECUS: Sex Ed for Social Change , a national group that advocates for inclusive sex education. "You're giving them the tools to make decisions about their bodies and their lives that best suit them as individuals."
Why Sex Education Matters
Research shows that comprehensive, culturally responsive and inclusive sex education programs help prevent intimate partner violence and help young people develop healthy relationships. These programs have also been shown to reduce rates of sexual activity, sexual risk behaviors, adolescent pregnancy and sexually transmitted infections.
Sex ed "promotes healthy behaviors," says Laurie Dils, associate director of content, health and sexual health education at the Washington Office of Superintendent of Public Instruction. "That's really what we are aiming for as educators, equipping young people with education and skills so that they can make healthy decisions that fit with their own values and their family's values."
But in public school, the quality of sex education your child will receive – or whether they will receive any at all – depends largely on the state and district you live in. There are no federal guidelines for sex education, and currently only 18 states require program content to be medically accurate, according to recent data from the Guttmacher Institute, a research and policy organization focused on sexual health and reproductive rights.
"Most young people have access to the internet," Slaybaugh says. "So if we are not providing them instruction that is medically accurate and age-appropriate, we are leaving it to chance for them to find something on the internet, i.e., porn, and then they think that's what sex and sexuality is."
Sex Education Requirements by State
Sex education standards vary by state – with some not having any curriculum requirements in schools. As of June 2022, 39 states plus Washington, D.C., mandate sex education, HIV education or both, according to Guttmacher Institute data.
Unlike sex education, HIV and STI instruction only focus on concepts like pregnancy prevention and risk reduction. "But sexuality touches our lives in so many other ways, especially when it comes to being inclusive to diverse people, families and experiences," Slaybaugh says.
Thirty-nine states and D.C. either stress or require abstinence to be covered when sex education is taught. Meanwhile, only 20 states require provision of information on contraception, Guttmacher Institute research found.
Slaybaugh says that abstinence-only teachings, sometimes referred to as sexual risk avoidance, are often "rooted in shame." For example, she points to one common lesson in which youth are asked to chew up gum and spit it out, then told the chewed up gum is a representation of a person who had sex before marriage.
"Abstinence-only programs do not teach communication and negotiation for consent," she adds. "It does not teach about what healthy relationships should look like and what they don't look like. They do not include affirming lessons around LGBTQIA+ individuals. They're ostracizing a large part of the youth population."
Health experts including the American Academy of Pediatrics and the American College of Obstetricians and Gynecologists recommend that sex education include information about gender and sexual orientation. But only a small handful of states – 10 plus D.C. – require inclusive content with regard to sexual orientation.
Meanwhile, five states – Alabama, Louisiana, Oklahoma, South Carolina and Texas – allow only negative information to be shared about homosexuality and place a positive emphasis on heterosexuality, according to Guttmacher Institute data. And recently, some states have banned or are seeking to ban the discussion of sexual orientation and gender identity in school, especially in the younger grades.
Florida Governor Ron DeSantis, for example, signed a bill in March 2022 prohibiting instruction about sexual orientation or gender identity in K-3 classrooms. Chris Sprowls, speaker of the Florida House of Representatives, said in a press release that such instruction "does not belong in the classroom where 5- and 6-year-old children are learning. It should be up to the parent to decide if and when to introduce these sensitive topics."
But "not seeing yourself reflected at any time is always detrimental to young people. Certainly seeing yourself negatively portrayed would be devastating," says Stephanie Hull, president and CEO of Girls Inc., a nonprofit youth development organization. "When we don't have an LGBTQ inclusive health curriculum, then we don't reduce homophobic attitudes, we don't reduce the bullying and we don't reduce harassment. Those students are already unsafe, so it increases their lack of safety."
Curriculum by Age
Sex education in schools can be taught by a classroom teacher, school nurse or an outside speaker, and often begins in fifth grade, according to Dils.
But some experts say age-appropriate instruction should begin earlier. For instance, the National Sex Education Standards developed by SIECUS: Sex Ed for Social Change, Answer and Advocates for Youth, a group that works to advance sex education, say that sex education should begin in kindergarten . Based on those standards, early conversations are not about the act of sex, but cover basic information about male and female anatomy and concepts like consent and personal boundaries.
From kindergarten to third grade, curricula may also include lessons to help children understand their own emotions and develop good communication skills, boundaries and respect for others, Dils says.
Then, in third to fifth grade, curriculum can shift to discussing what healthy friendships look like. "If a young person doesn't know how to identify an unhealthy friendship, how can we assume that they will be able to identify and find a healthy romantic relationship later on?" says Slaybaugh.
Additionally, schools should start preparing students for puberty, to help them understand what's going to happen as they get older. The first questions that typically arise from children are: Am I normal? Are these changes that are happening to me normal?
"A big part of sex education, if it's done well, is just helping to normalize what they're going through and to give them enough understanding and tools so that they can manage whatever they're going through," Dils says. "It's different for every young person."
As students enter middle school and high school, discussions should dive deeper into puberty, romantic relationships, partner violence, STIs, gender orientation and sexual identity, experts advise.
Parent Involvement in Sex Education
Currently 40 states plus D.C. require school districts to involve parents in sex education and/or HIV education. Thirty-six states and D.C. give parents the option to remove their child from instruction, while five states require parental consent for students to participate in a program, according to recent data from the Guttmacher Institute.
Critics claim that comprehensive sex education oversexualizes children and is not age-appropriate. American Life League, a Catholic pro-life organization, states on its website that "because of sex education programs, schools have been taking away the parents’ responsibilities of teaching their child about human sexuality."
But proponents of comprehensive sex say parents should be involved. "Parents are the most influential people in an adolescent's decisions about sexuality, and we encourage family discussions about their values related to sexuality," Tazmine Weisgerber, training and technical assistance manager at Answer, a national nonprofit housed within Rutgers University that aims to promote access to comprehensive sex education for youth, wrote in an email.
Experts advise parents to find out what's being taught in the classroom and express any concerns about their child's program to administrators at the school or within the district. Issues can also be brought up during their local school board meetings.
Additionally, start having conversations around sex education with your children at home at an early age. Familiarize yourself with the subject by reading the National Sex Ed Standards, Slaybaugh says. There are many other resources parents can refer to, including:
- Planned Parenthood
- SEICUS: Sex Ed for Social Change
- Talk With Your Kids
"At the end of the day, I think all sex educators want parents to be involved," Slaybaugh says. "We want to help parents understand that this is not a scary subject and it's just as important as math, science or reading. It takes all of us to participate in the process to be successful at seeing sex ed as an important lesson."
See the 2022 Best Public High Schools

Tags: K-12 education , sex education , students , teachers , sexual health
2024 Best Colleges

Search for your perfect fit with the U.S. News rankings of colleges and universities.
Popular Stories
Best Colleges

College Admissions Playbook

You May Also Like
Choosing a high school: what to consider.
Cole Claybourn April 23, 2024

Map: Top 100 Public High Schools
Sarah Wood and Cole Claybourn April 23, 2024

States With Highest Test Scores
Sarah Wood April 23, 2024

Metro Areas With Top-Ranked High Schools
A.R. Cabral April 23, 2024

U.S. News Releases High School Rankings

See the 2024 Best Public High Schools
Joshua Welling April 22, 2024

Explore the 2024 Best STEM High Schools
Nathan Hellman April 22, 2024

Ways Students Can Spend Spring Break
Anayat Durrani March 6, 2024

Attending an Online High School
Cole Claybourn Feb. 20, 2024

How to Perform Well on SAT, ACT Test Day
Cole Claybourn Feb. 13, 2024

The effectiveness of sex education and HIV education interventions in schools in developing countries
Affiliation.
- 1 ETR Associates, 4 Carbonero Way, Scotts Valley, CA 95061, USA. [email protected]
- PMID: 16921919
Objective: To review the impact of sex education and HIV education interventions in schools in developing countries on both risk behaviours for HIV and the psychosocial factors that affect them.
Methods: We conducted a systematic review. Searches identified studies in developing countries that evaluated interventions using either experimental or strong quasi-experimental designs and measured the impact of the intervention on sexual risk behaviours. Each study was summarized and coded, and the results were tabulated by type of intervention.
Findings: Twenty-two intervention evaluations met the inclusion criteria: 17 were based on a curriculum and 5 were not, and 19 were implemented primarily by adults and 3 by peers. These 22 interventions significantly improved 21 out of 55 sexual behaviours measured. Only one of the interventions (a non-curriculum-based peer-led intervention) increased any measure of reported sexual intercourse; 7 interventions delayed the reported onset of sex; 3 reduced the reported number of sexual partners; and 1 reduced the reported frequency of sexual activity. Furthermore, 16 of the 22 interventions significantly delayed sex, reduced the frequency of sex, decreased the number of sexual partners, increased the use of condoms or contraceptives or reduced the incidence of unprotected sex. Of the 17 curriculum-based interventions, 13 had most of the characteristics believed to be important according to research in developed and developing countries and were taught by adults. Of these 13 studies, 11 significantly improved one or more reported sexual behaviours, and the remaining 2 showed non-significant improvements in reported sexual behaviour. Among these 13 studies, interventions led by both teachers and other adults had strong evidence of positive impact on reported behaviour. Of the 5 non-curriculum-based interventions, 2 of 4 adult-led and the 1 peer-led intervention improved one or more sexual behaviours.
Conclusions: A large majority of school-based sex education and HIV education interventions reduced reported risky sexual behaviours in developing countries. The curriculum-based interventions having the characteristics of effective interventions in the developed and developing world should be implemented more widely. All types of school-based interventions need additional rigorous evaluation, and more rigorous evaluations of peer-led and non-curriculum-based interventions are necessary before they can be widely recommended.
Publication types
- Research Support, Non-U.S. Gov't
- Research Support, U.S. Gov't, Non-P.H.S.
- Systematic Review
- Cost-Benefit Analysis
- Developing Countries*
- Global Health
- HIV Infections / economics
- HIV Infections / prevention & control*
- Health Education / economics
- Health Education / methods*
- Health Education / organization & administration
- Health Knowledge, Attitudes, Practice*
- Program Evaluation
- Risk-Taking
- Sex Education / economics
- Sex Education / methods
- Sex Education / organization & administration
- Sexual Behavior
Proposed changes in rules for school sex ed would stigmatize LGBTQ+ people, expert says

Proposed changes to Oklahoma law would make it harder for students to receive medically accurate and comprehensive sex education, according to experts who reviewed legislation that recently advanced in the Oklahoma House of Representatives.
House Bill 3120 was narrowly approved in a committee hearing last week . Its author, state Rep. Danny Williams, R-Seminole, said his goal is "to put the permissions and the responsibility in the hands of parents or guardians" when it comes to learning about sexually transmitted infections, birth control, consent and the prevention of AIDS.
Under current Oklahoma law, sex education is not required, but schools must provide HIV/AIDS prevention instruction and health education. If a school offers sex education, parents can choose to have their kids skip the class. Williams' bill changes it to "opt-in," meaning that parents would have to provide written approval for their kids to join the class.
"Parents should know what their children are being asked to be involved in," Williams said during a legislative committee hearing where he presented the bill. "I think we've walked away from that. I think the challenges of life sometimes have kept us so busy that we haven't looked at the details.
"But at the same time, I think it should be a quality decision based on education and knowledge, so the parent knows what they're doing when they make the decision for their child," he said.
Prep for the polls: See who is running for president and compare where they stand on key issues in our Voter Guide
Changes to lessons on consent, STIs
In its current form, the bill specifically forbids schools from teaching "consent and negotiation skills for sexual activity." Several members of the committee, including fellow Republicans, questioned why it would be banned. If the bill reaches the House floor, Williams said he would agree to restoring one section of the law that requires students be taught the legal definition of sexual consent.
The bill also wades into defining gender roles in reproductive health, which has become a frequent target for conservative lawmakers.
The Oklahoman has sought to identify which individuals or organizations wrote the legislation. Williams, who acknowledged during the committee hearing that he might not have understood exactly what the bill does, did not return messages left at his office.
Heather Duvall is executive director for Amplify Youth Health Collective, a Tulsa-based organization that works to expand access to sex education, promote healthy relationships and encourage community engagement. Through her organization, she's found that 92% of people agree that comprehensive sex education should be happening in schools.
"It's vitally important for young people to learn this information, and we're doing them a disservice if we don't provide them with the education they need to be healthy and safe," Duvall said.
If signed into law, the bill would put Oklahoma in rare company. As of 2022, only eight states required parents to opt-in to sex education, according to SIECUS, an advocacy organization that promotes comprehensive sex education throughout the nation.
"By creating an opt-in when you already have an opt-out, it just creates an extra barrier," said Michelle H. Slaybaugh, director of programs for SIECUS.
Slaybaugh compared it to other policies that rely on students getting a note signed and brought back to school. For example, she said, it's sometimes a challenge for students to get field trip permission slips back to their teachers.
"So when you have a child who may not have a great relationship with their parents, or is afraid of their parents for some reason, requiring them to get an opt-in for vital information that will impact their long-term health outcomes seems ridiculous," she said.
During the committee hearing, Williams said his bill promotes personal responsibility and encourages more participation from parents and guardians.
"I think there are going to be a lot more parents engaged in their children's education completely, not just sex education, because it's going to challenge them to actually be a part of the decision-making process," he said.
As a grandfather, Williams has taught his grandchildren about sexually transmitted diseases.
"I've been trying to teach them if you make good choices, you typically get good results," Williams said. "If you make bad choices, you're probably going to get bad results."
But even if students receive Oklahoma's version of sex education, Slaybaugh said they're exposed to poor quality information that includes stigmatizing claims about LGBTQ+ people.
While HIV can be transmitted during any activity that involves certain bodily fluids, Oklahoma law prioritizes teaching that "engaging in homosexual activity, promiscuous sexual activity, intravenous drug use or contact with contaminated blood products" is the primary cause, and that avoiding those activities "is the only method of preventing the spread of the virus."
"This further stigmatizes learning about HIV information, which puts students at greater risk of not knowing how to find information on how to protect themselves," she said.
Abstinence-focused sex education
The law also prioritizes teaching that avoiding sex outside of marriage is the expected standard for all school-age students, while also teaching the benefits of monogamous heterosexual marriage. Slaybaugh argues that Oklahoma's version of sex education doesn't acknowledge the real situations faced by modern children, and abstinence-based lessons don't speak to consent or intimate partner violence.
"Teaching young people quality sex ed does not increase their chances of becoming sexually active. It actually can delay initial onset of sexual activity, while simultaneously giving them the skills to be smarter about the decisions they make when they choose to become sexually active," she said.
One trend that could help explain the effectiveness of sex education is the teen birth rate. A study of 55 U.S. counties published in 2022 found that funding for more comprehensive sex education led to an overall reduction in the teen birth rate.
Oklahoma's teen birth rate has been steadily falling over the past three decades. In 1991 there were more than 72 babies born for every 1,000 female teenagers. As of 2023, the rate had fallen to about 21 births.
"We know that has happened alongside the expansion of programs and services that support comprehensive sex education," said Duvall.
While a declining teen birth rate is seen across the United States, Oklahoma still has one of the highest rates in the nation, according to Healthy Teens Oklahoma .
- Investigative Stories
- Entertainment
- Life & Living
- Tech & Startup
- Rising Star
- Star Literature
- Daily Star Books
- Roundtables
- Star Holiday
- weekend read
- Environment
- Supplements
- Brand Stories
- Law & Our Rights

Most Viewed
2 Bangladeshis shot dead in New York
Students back to school even as Met office extends heat alert
Heatwave alert extended for 72 hours
Heatwave: Secondary schools, colleges in 5 districts to remain shut tomorrow
The need for comprehensive sexuality education in our schools
When navigating the tightrope between a carefree childhood and forthcoming adulthood responsibilities, teenagers can never seem to catch a break. All these challenges intensify a million-fold when they hit puberty, as their bodies and brains undergo transformations that often go unexplained and unexplored. Through these turbulent times, the importance of sex education in guiding adolescents cannot be overstated.
There are many commonly-held misconceptions about sex education. To better understand what it really is about, we spoke to Dr Riad Mahmud, a health specialist at UNICEF. He explains, "Contrary to popular belief, comprehensive sexuality education (CSE) isn't exclusively about sexuality. Beyond information on safe sex and pregnancy prevention, CSE teaches people to be aware of their bodies, respect boundaries, and understand consent."
For all latest news, follow The Daily Star's Google News channel.
He elaborates on its importance, stating, "CSE equips adolescents with crucial knowledge, attitudes, and skills, enabling them to protect their health, well-being, and dignity."
Existing academic research echoes Dr Riad's sentiments. The 2015 Global Review by the United Nations connects CSE to improved sexual and reproductive health, leading to the reduction of STIs, HIV, and unplanned pregnancy by encouraging safer sexual practices as well as reducing sexual violence and promoting gender equality.
Despite its importance, Bangladesh lacks specific government policies regarding sex education. "CSE is not officially mentioned by the government," explains Dr Riad, "and very limited components of CSE are being implemented through various adolescent health programmes under multiple ministries like the Ministry of Health and Ministry of Education."
Hence, sex education has only been implemented in bits and pieces, almost exclusively under the National Curriculum and Textbook Board (NCTB) curriculum. The brunt of it has been included in textbooks such Physical Education and Health, Life Skill Education, Wellbeing textbooks, among a few others.
Many out-of-school interventions also exist simultaneously to the NCTB content. Jahura Begum, the principal of Udayan Higher Secondary School, recounts two UNICEF-backed events on menstruation awareness that were conducted on campus involving seminars, visual presentations, and an art competition. Dr Riad also cites the School Based Adolescent Health Program (SBAHP) and Gender Equity Movement in Schools (GEMS) to be active initiatives, particularly in rural contexts.
While sex education is technically a part of the education curriculum, its ineffective implementation leaves much to ask for. Dr Riad provides insight into some of the challenges, "Despite the inclusion of basic reproductive health education in textbooks for grades six to ten, the avoidance of the term 'CSE' stems from societal taboos surrounding sexuality, influenced by religious and cultural considerations."
This leads to crucial conversations being conducted in hushed tones or avoided entirely.
Thus, the sensitivity of certain CSE components requires teachers to have specialised training, which often isn't implemented. Dr Riad also notes, "The absence of CSE in the Teachers Training Curriculum leaves educators unprepared to deliver age-appropriate information."
Regading this, two students, Omar Faruk Saikat, a 10th-grader at UCEP Bangladesh, and Farabi Jaman Shehjadi, an HSC graduate from BAF Shaheen College, spoke of their experience. While Saikat observed many of his teachers feeling hesitant, Shehjadi opines that her teachers were actually quite comfortable teaching sex education components. This a lack of consistency in the expertise of teachers across different institutions.
Ensuring the content is age-appropriate is also important, as Srabon Chowdhury*, a teacher at Viqarunnisa Noon School & College, shares, "We don't explain things in a complicated way to young students. Younger students start out by learning general themes such as family, kindness, and respect for others' boundaries. Later, they're exposed to more mature topics such as gender-based violence, sexual consent, pregnancy, and more."
But even when CSE is internalised by students in the classroom, it's often difficult to implement it at home due to stigma. Shamima Chowdhury, a former consultant at UNICEF, explains, "Parents also need to be provided with CSE because the students otherwise cannot apply what they learn in school at home." She emphasises the importance of community buy-in as well, particularly in rural areas, ensuring students can express what they learned without inhibition.
Privilege also heavily intersects with the lack of access to sexual and reproductive health (SRH) resources. As Dr Riad points out, "Some youth, particularly those in gender diversity clusters, refrain from seeking SRH services due to a fear of identity exposure." Shamima notes, "Out-of-school children are also very vulnerable."
Moreover, CSE is yet to reach alternative streams of education like private schools and madrasas. Thus, nearly four million students remain vulnerable to misinformation and negligence towards their own bodies.
So, what can be done to improve the situation? Shamima, alluding to her work in rural Jaipurhat from 2018 to 2019, suggests that the NCTB should gradually introduce more progressive themes by "piloting" new additions to the curriculum in a select number of institutions and communities, instead of launching it directly. Principal Jahura further emphasises the need to reach more rural corners of Bangladesh where much progress is yet to be made. From the students' perspective, Shehjadi suggests that teachers should foster closer bonds with all students and not be biased, so students can properly internalise the concepts they're exposed to.
Despite the many shortcomings of the implementation of CSE, some tangible progress has still been made. Jahura notes that over the years, her student body has grown to become more open-minded toward issues like menstruation, sexuality, and puberty, crediting much of the progress to the inclusion of sex education in textbooks. "The current curriculum textbook is able to express these topics very nicely as well," she adds.
Yet, progress cannot serve as an excuse for complacency. While current initiatives are a foot through the door, we still have a very long way to go. Our youth have a right to access crucial information about their bodies, and it is our responsibility to ensure that what they're provided with is comprehensive, accurate, and inclusive.
Reference :
The United Nations (2015). Global Review finds Comprehensive Sexuality Education key to gender equality and reproductive health .

Related News
Life through the lens of an electricity pole
Bangladeshi comedian-actor to be on ‘Sex Education’

‘Right Here, Right Now’ project to create awareness on sexual and reproductive health and rights (SRHR)
Are you experiencing testing fatigue?

The inclusion of gender studies in our national curriculum is commendable

তাপপ্রবাহ: শিক্ষাপ্রতিষ্ঠান খোলা-বন্ধ নিয়ে যা বললেন শিক্ষাবিদরা
‘কিন্তু গ্রামের বাচ্চারা অসুস্থ হয়ে পড়ছে। কারণ, লোডশেডিং হচ্ছে। খাবার পানি, লোডশেডিংয়ের মতো বিষয়গুলো মাথায় রেখেই স্কুল-কলেজ খোলা রাখার বিষয়টি মাথায় রাখতে হবে।’
‘ডা. জাফরুল্লাহ মুক্তিযুদ্ধের আদর্শ থেকে কখনো বিচ্যুত হননি’
- Open access
- Published: 24 April 2024
Comparing PrEP initiation rates by service delivery models among high risk adolescent boys and young men in KwaZulu-Natal, South Africa: findings from a population-based prospective study
- Mbuzeleni Hlongwa 1 , 2 ,
- Wisdom Basera 3 , 4 &
- Edward Nicol 3 , 5
BMC Public Health volume 24 , Article number: 1151 ( 2024 ) Cite this article
143 Accesses
Metrics details
Introduction
Pre-exposure prophylaxis (PrEP) is an HIV prevention strategy that can reduce the risk of HIV acquisition by more than 90% if taken consistently. Although South Africa has been implementing PrEP since 2016, initially for selected population groups before expanding access to more people, there is a dearth of research focused on PrEP among adolescent boys and young men (ABYM), despite them experiencing high rates of HIV infection. To address this gap, we compared PrEP initiation rates by service delivery points (SDPs) among ABYM in KwaZulu-Natal, South Africa.
We conducted a population-based prospective study in 22 SDPs from July 2021 to July 2022 in KwaZulu-Natal, South Africa. Sexually active ABYM aged 15–35 years who tested HIV negative were recruited at purposively selected PrEP SDPs (i.e., healthcare facilities, secondary schools and Technical Vocational Education and Training (TVET) colleges, and community-based youth zones). We collected baseline quantitative data from each participant using self-administered electronic questionnaires built into REDCap, including demographic information such as age, sex, employment status and level of education, as well as PrEP initiation outcomes. We extracted data from REDCap and exported it to Stata version 17.0 for analysis, and then eliminated discrepancies and removed duplicates. We described baseline characteristics using summary and descriptive statistics (median, interquartile range [IQR] and proportions) and reported PrEP initiation proportions overall and by SDPs.
The study included 1104 ABYM, with a median age of 24 years (interquartile range (IQR): 21–28)). Almost all participants were black African ( n = 1090, 99%), with more than half aged 15–24 years ( n = 603, 55%) and 45% ( n = 501) aged 25–35 years. The majority ( n = 963; 87%) had attained a secondary level of education. Overall PREP initiation rate among adolescent boys and young men was low: among 1078 participants who were eligible for PrEP, 13% ( n = 141) were started on PrEP. Among the participants who were initiated on PrEP, over three quarters (78%, n = 58) were initiated from high schools, compared with community-based youth zones (40%, n = 37), TVET colleges (26%, n = 16) and healthcare facilities (4%, n = 30).
Conclusions
This study provided evidence suggesting that expanding PrEP services to non-traditional settings, such as high schools, TVET colleges, and community-based organizations, may have a potential to increase PrEP access among ABYM in South Africa.
Peer Review reports
Human immunodeficiency virus (HIV) continues to be a significant public health concern in many parts of the world, consisting of more than 37 million people diagnosed with HIV in year 2020 [ 1 ]. South Africa has a high HIV prevalence, with more than seven million people estimated to be living with HIV [ 2 ]. Adolescent boys and young men (ABYM) are a vulnerable group affected by HIV in South Africa, as they account for a substantial proportion of people newly infected with HIV in South Africa [ 3 ]. In South Africa, ABYM are increasingly getting recognised as a vulnerable population group due to the disproportionately high burden of HIV infection, underscoring the urgent need to address the risk factors, including high-risk sexual behaviours and prioritizing AYBM in HIV prevention strategies. Pre-exposure prophylaxis (PrEP) is an HIV prevention strategy that can reduce the risk of HIV acquisition by more than 90% if taken consistently [ 4 , 5 ]. Although this is the case, ABYM continue to experience high rates of HIV infection in South Africa, despite many efforts designed to address their HIV prevention care and needs [ 6 ]. HIV prevalence is 3.1 among males aged 15–19, 4.0 in 20–24 years, 6.3 in 25–29 years, 10.8 in 30–34 years and 16.9 in 35–39 years [ 7 , 8 ]). Data from the HIV incidence study conducted in uMgungundlovu, and published in 2019 showed that among men aged 15–19, 20–24, 25–29 and 30–35 the HIV incidence rates were 0.24, 1.18, 2.84 and 1.45 per 100 person-years, respectively [ 7 ]. In South Africa, the rollout of oral PrEP started in 2016 with 11 sites in five provinces. An additional site was added in November, to create a total of 12 implementing sites in 2016 [ 9 , 10 ]. Initially, PrEP was implemented among selected key population groups (for example, sex workers) as well as to men who have sex with men; and adolescent girls and young women at primary healthcare facilities, before expanding access to more people, including ABYM. However, there is a dearth of research focused on PrEP among ABYM, despite them experiencing high rates of HIV infection.
In order to improve the rates of PrEP initiation among ABYM, it is imperative that we understand which service delivery models may be effective to ensure that men have appropriate access to PrEP services. It is also important that we understand which service delivery models may contribute to low PrEP initiation rates. One potential factor for PrEP initiation is the service delivery model used to provide PrEP services. For example, traditional facility-based healthcare models may not effectively reach ABYM, due to several barriers men face to accessing healthcare services, including stigma, lack of privacy, long waiting queues, unfriendly healthcare environments and concerns about confidentiality [ 11 , 12 ]. These challenges facing public healthcare facilities have led to the growing appetite for alternative models, including decentralizing models, that are aimed at improving the rates of PrEP initiation, such as community-based service delivery models. Community-based service delivery models may be more acceptable and accessible to AYBM compared to the traditional public healthcare facility-based models [ 13 ]. Research demonstrates that community-based ART service delivery and initiation are successful approaches for increasing HIV treatment access in SSA because they address a number of distinctive barriers related to receiving HIV treatment from clinic settings, including stigma and discrimination, long waiting times, confidentiality concerns, and transport costs [ 11 , 14 , 15 , 16 ].
This study aimed to compare PrEP initiation rates by service delivery models among ABYM in KwaZulu-Natal, South Africa. Our study targeted adolescent boys and young men, a population that is at a greater risk for new HIV infections [ 6 ]. Specifically, this study assessed PrEP initiation rates among ABYM who accessed PrEP through high schools, technical and vocational education and training (TVET) colleges, community-based youth zones (i.e., spaces within communities dedicated to young people providing services focused on sexual and reproductive health and HIV-related services), and public healthcare facilities.
Study setting
This study was conducted in uMgungundlovu district in KwaZulu-Natal province, South Africa (Fig. 1 ). We selected participating facilities in consultation with provincial and district Department of Health. Overall HIV prevalence is high in uMgungundlovu district, accounting for 31% overall among 15–59 years, and 23% among men 15–49 years [ 17 ]. The population of uMgungundlovu is predominantly poor and rural, with the majority using public health services [ 18 ].

Sub-districts of uMgungundlovu District, KwaZulu-Natal, South Africa
Study design
We conducted a population-based prospective study in 22 SDPs over 13 months (July 2021 to July 2022). Adolescent boys and young men were purposively selected (those who visited the SDP while study staff were around) from 22 service delivery points (SDPs) (i.e., healthcare facilities ( n = 11), High schools ( n = 2) and Technical Vocational Education and Training (TVET) colleges ( n = 4), and community-based youth zones( n = 5). We defined PrEP initiation according to national guidelines [ 10 ]. We administered questionnaires and accessed routine healthcare service records at enrolment to obtain and verify HIV test results and PrEP initiation outcomes among participants. The protocol for this study has been previously published [ 19 ].
Population and recruitment
The target population for this study comprised sexually active ABYM aged 15–35 years, who test HIV negative during the routine healthcare facility-based, school-based, and community-based HIV testing services at 22 selected SDPs, in each of the seven sub-districts (strata) (namely, UMshwathi, Umgeni, Mpofana, Impendle, Msunduzi, Mkhambathini and Richmond) in the uMgungundlovu district. Participants were recruited and tracked through surveys using questionnaires and routine pharmaceutical records of PrEP pill collection, and SDP records. The inclusion criteria were: (a) having accepted an HIV test in one of the participating SDPs during the data collection, (b) having access to a cell phone and willingness to provide contact details, (c) be aged 15–35 years, (d) be sexually active and at high risk for HIV (identified by a set of risk assessment questions), (e) be seronegative based on HIV rapid test results on the day of recruitment, and (f) be able and willing to provide informed consent. Potential participants who were diagnosed with TB were excluded in the study.
Data collection and management
Male clients that presented at the 22 SDPs for routine HIV test were approached before the test and recruited into the study. We collected baseline quantitative data from each participant using self-administered electronic questionnaires built into REDCap, including demographic information such as age, sex, employment status and level of education, as well as PrEP initiation outcomes, in addition to a HIV risk assessment test. Participants who had a negative HIV test and were substantially at risk were offered PrEP by staff at the SDPs. The risk assessment tool with the higher HIV risk stated in the parenthesis included a past six [ 6 ] months recall on (a) the number of people one had vaginal or anal sex with (2+), (b) frequency of condom use (no & don’t know), (c) reward based sexual experiences (yes), (d) having a sexually transmitted infection (yes & don’t know), (e) sharing of needles during intravenous drug use (yes) and (f) having a partner who is HIV infected (yes & don’t know). Any higher HIV risk response to one of the questions denoted PrEP eligibility. We also used secondary data sources, including the district health information system to extract information on PrEP initiation in the district and facilities where this project was implemented. Trained and competent facility-based data champions, working together with the project coordinator conducted daily quality checks on completeness of REDCap records on the tablets, before uploading data over 3G or Wi-Fi to the REDCap folder stored securely on the SAMRC’s server. Any data inconsistencies and/or errors were flagged, discussed and rectified at regular quality control meetings.
Data analysis
We extracted data from REDCap and exported it to Stata version 17.0 for analysis, and then eliminated discrepancies and removed duplicates. We dropped 23 participants from our analysis because they did not have PrEP initiation outcomes.
We described baseline characteristics using summary and descriptive statistics (median, interquartile range [IQR] and proportions) and reported PrEP initiation proportions overall and by SDPs.
Ethical considerations
The SAMRC Research Ethics Committee gave its clearance for this project (Ref: EC051-11/2020). Gatekeeper approvals were also obtained from the districts, facilities, and collaborating Provincial Departments of Health (Ref: KZ_202010_033). Prior to their involvement, we sought both verbal and written informed consent from all eligible study participants. Participants were informed throughout recruitment that participation was completely voluntary and that they were free to withdraw their participation at any time without facing any repercussions from the research team or the facilities they use.
The study included 1104 ABYM recruited from 22 SDPs (Fig. 2 ), with a median age of 24 years (interquartile range (IQR): 21–28)) (Table 1 ). Almost all participants were black African ( n = 1090, 99%), with more than half aged 15–24 years ( n = 603, 55%) and 45% ( n = 501) aged 25–35 years. The majority ( n = 963; 87%) had attained a secondary level of education.
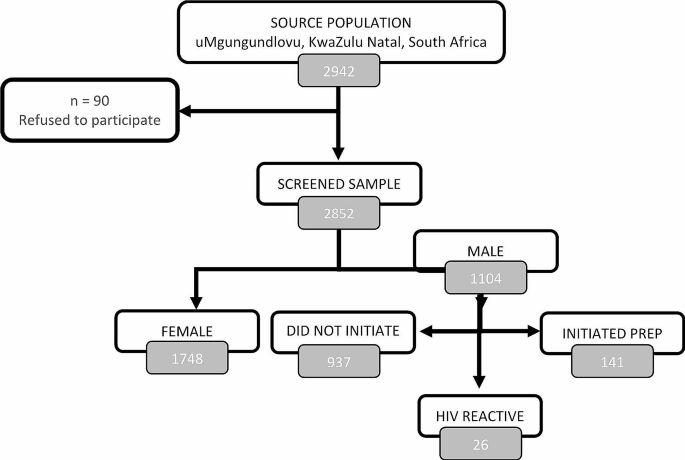
Consort diagram detailing the recruitment of study participants into the PrEP initiation in uMgungundlovu district
PrEP initiation rates among adolescent boys and young men
Overall, PrEP initiation rate among adolescent boys and young men was low: among 1078 participants who were eligible for PrEP, 13% ( n = 141) were started on PrEP (Table 2 ). Twenty-six (2%) participants were diagnosed with HIV, with 89% ( n = 23) reactive participants coming from clinics and 11% ( n = 3) from TVET colleges.
Another notable finding in our study is the disparities in PrEP initiation rates among different types of service delivery points. For example, among the participants who were initiated on PrEP, over three quarters (78%, n = 58) were initiated from high schools, compared with community-based youth zones (40%, n = 37), TVET colleges (26%, n = 16) and healthcare facilities/clinics (4%, n = 30).
Over three quarters (79%, n = 849) of the participants had a high risk profile of HIV infection based on the risk screening tool and were eligible for PrEP. A high proportion (61%, n = 661) of participants self-reported as willing to consider taking PrEP, with 16% ( n = 107) of those who went on to initiate it. Amongst the reasons cited by those at a higher HIV risk profile ( n = 849) for non willingness to consider PrEP, the top three were – I don’t want to be taking drugs for a long time (13%, n = 112), I fear side effects (11%, n = 91) and I do not think I am at risk of acquiring HIV (10%, n = 84).
This study aimed to compare PrEP initiation rates by service delivery models among ABYM in KwaZulu-Natal, South Africa. Similar to our study, PrEP initiation rates among men were reported to be low in Eswatini [ 20 ]. This supports the notion that PrEP access and uptake is a widespread challenge in the region, given the several factors and barriers identified to be affecting men’s access and initiation to PrEP in SSA, including stigma, discrimination, lack of knowledge and awareness of PrEP, inaccessibility of PrEP services, misinformation, fear of side effects and PrEP pill burden [ 21 , 22 , 23 ]. These findings suggest that there is a need for targeted educational interventions aimed to promote PrEP awareness and improve PrEP initiation rates among ABYM in KwaZulu-Natal, and in similar settings elsewhere.
Specifically, our study found that healthcare facilities had lower rates of PrEP initiation compared to high schools and TVET colleges, and community-based youth zones. This result suggests that the traditional facility-based may not be the most effective approach for reaching adolescent boys and young men with PrEP services. Instead, our study findings suggest that the community-based youth zones and high schools and TVET colleges may be promising additional models to traditional healthcare facilities for reaching men through distributing PrEP services.
Our finding reporting low rates of PrEP initiation from healthcare facilities, compared to community-based youth zones and high schools and TVET colleges was not surprising, given the well documented barriers deterring men from accessing services from the healthcare facilities in SSA [ 11 ]. In South Africa, for example, compared with women, men are less likely to access healthcare services, due to many factors including stigma, long waiting queues, masculinity and unfriendly healthcare environments [ 12 ]. However, our findings are consistent with global efforts to decentralize HIV prevention and treatment services to community-based settings in an effort to improve access to HIV treatment.
Evidence shows that community-based HIV services are an effective strategy for improving access to HIV treatment in SSA, as it addresses several distinctive barriers associated with accessing HIV treatment from clinic settings [ 14 , 15 , 16 ]. Therefore, in order to address the low rates of PrEP initiation among ABYM in KwaZulu-Natal, our findings suggest that there may be a need to adopt a multi-pronged approach that may include targeted outreach and education interventions, as well as decentralizing PrEP services to non-traditional healthcare settings. This may include strengthening and expanding partnering with high schools and TVET colleges, as well as community-based organisations to provide education and counselling, as well as improving PrEP access for men. This could involve developing and/or strengthening tailored educational materials, peer-led counselling sessions, and targeted outreach initiatives to increase knowledge of PrEP among males who might not be currently receiving these services.
A key limitation for this study relates to the fact that this paper does not address the factors influencing PrEP initiation rates among ABYM. Instead, these are currently being analyzed qualitatively, and will be discussed in a separate publication.
In conclusion, the findings from this study have important indications for efforts to improve PrEP access among ABYM in KwaZulu-Natal, South Africa. By expanding PrEP services to non-traditional settings, such as high schools, TVET colleges, and community-based organizations, there is potential to increase PrEP access and reduce the burden of HIV among men. These efforts may be particularly important in the context of the ongoing HIV epidemic in South Africa.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
UNAIDS, Global. AIDS update 2021: confronting inequalities: lessons for pandemic responses from 40 years of AIDS. Switzerland: UNAIDS; 2021.
Google Scholar
UNAIDS. South Africa Country factsheets: HIV and AIDS estimates. Switzerland: UNAIDS; 2021.
Simbayi L, Zuma K, Zungu N, Moyo S, Marinda E, Jooste S et al. South African National HIV prevalence, incidence, behaviour and communication survey, 2017: Towards achieving the UNAIDS 90-90-90 targets. 2019.
Baeten JM, Donnell D, Ndase P, Mugo NR, Campbell JD, Wangisi J, et al. Antiretroviral prophylaxis for HIV prevention in heterosexual men and women. N Engl J Med. 2012;367(5):399–410.
Article CAS PubMed PubMed Central Google Scholar
Centers for Disease Control and Prevention. Pre-exposure Prophylaxis (PrEP). Centers for disease control and prevention; 2022.
UNAIDS. A snapshot of men and HIV in South Africa. [press release]. Geneva: UNAIDS; 2017.
Kharsany AB, Cawood C, Lewis L, Yende-Zuma N, Khanyile D, Puren A, et al. Trends in HIV prevention, treatment, and incidence in a hyperendemic area of KwaZulu-Natal, South Africa. JAMA Netw Open. 2019;2(11):e1914378–e.
Article PubMed PubMed Central Google Scholar
Human Sciences Research Council. Summary sheet: the Sixth South African National HIV Prevalence, Incidence, Behaviour and Communication Survey. Pretoria: Human Sciences Research Council; 2023.
SA Department of Health. Guidelines for expanding combination prevention and treatment options for sex workers: oral pre-exposure prophylaxis (PrEP) and test and treat (T&T). Final draft. Pretoria, South Africa. South African National Department of Health; 2016.
SA Department of Health. 2021 Updated guidelines for the provision of Oral Pre-Exposure Prophylaxis (PrEP) to persons at substantial risk of HIV infection. Pretoria: SA National Department of Health; 2021.
Hlongwa M, Mashamba-Thompson T, Makhunga S, Hlongwana K. Barriers to HIV testing uptake among men in sub-saharan Africa: a scoping review. Afr J AIDS Res. 2020;19(1):13–23.
Article PubMed Google Scholar
Leichliter JS, Paz-Bailey G, Friedman AL, Habel MA, Vezi A, Sello M et al. ‘Clinics aren’t meant for men’: sexual health care access and seeking behaviours among men in Gauteng province, South Africa. SAHARA-J: Journal of Social Aspects of HIV/AIDS. 2011;8(2).
Ramraj T, Chirinda W, Jonas K, Govindasamy D, Jama N, Appollis TM, et al. Service delivery models that promote linkages to PrEP for adolescent girls and young women and men in sub-saharan Africa: a scoping review. BMJ open. 2023;13(3):e061503.
Barnabas RV, Szpiro AA, van Rooyen H, Asiimwe S, Pillay D, Ware NC, et al. Community-based antiretroviral therapy versus standard clinic-based services for HIV in South Africa and Uganda (DO ART): a randomised trial. Lancet Global Health. 2020;8(10):e1305–15.
Nachega JB, Adetokunboh O, Uthman OA, Knowlton AW, Altice FL, Schechter M, et al. Community-based interventions to improve and sustain antiretroviral therapy adherence, retention in HIV care and clinical outcomes in low-and middle-income countries for achieving the UNAIDS 90-90-90 targets. Curr HIV/AIDS Rep. 2016;13:241–55.
Eshun-Wilson I, Awotiwon AA, Germann A, Amankwaa SA, Ford N, Schwartz S, et al. Effects of community-based antiretroviral therapy initiation models on HIV treatment outcomes: a systematic review and meta-analysis. PLoS Med. 2021;18(5):e1003646.
HIV Data. South Africa District HIV estimates [Internet]. 2020. https://www.hivdata.org.za/ .
Statistics South Africa. General Household Survey. 2019. Pretoria, South Africa: Statistics South Africa; 2020.
Nicol E, Ramraj T, Hlongwa M, Basera W, Jama N, Lombard C, et al. Strengthening health system’s capacity for pre-exposure prophylaxis for adolescent girls and young women and adolescent boys and young men in South Africa (SHeS’Cap–PrEP): protocol for a mixed methods study in KwaZulu-Natal, South Africa. PLoS ONE. 2022;17(3):e0264808.
Berner-Rodoreda A, Geldsetzer P, Bärnighausen K, Hettema A, Bärnighausen T, Matse S, et al. It’s hard for us men to go to the clinic. We naturally have a fear of hospitals. Men’s risk perceptions, experiences and program preferences for PrEP: a mixed methods study in Eswatini. PLoS ONE. 2020;15(9):e0237427.
Muhumuza R, Ssemata AS, Kakande A, Ahmed N, Atujuna M, Nomvuyo M, et al. Exploring perceived barriers and facilitators of PrEP uptake among young people in Uganda, Zimbabwe, and South Africa. Arch Sex Behav. 2021;50(4):1729–42.
Nabunya R, Karis V, Nakanwagi LJ, Mukisa P, Muwanguzi PA. Barriers and facilitators to oral PrEP uptake among high-risk men after HIV testing at workplaces in Uganda: a qualitative study. BMC Public Health. 2023;23(1):1–13.
Article Google Scholar
Shamu S, Shamu P, Khupakonke S, Farirai T, Chidarikire T, Guloba G, et al. Pre-exposure prophylaxis (PrEP) awareness, attitudes and uptake willingness among young people: gender differences and associated factors in two South African districts. Global Health Action. 2021;14(1):1886455.
Download references
Acknowledgements
Not applicable.
This work was supported by the U.S. President’s Emergency Plan for AIDS Relief (PEPFAR) through the Centers for Disease Control and Prevention, under the terms of Cooperative Agreement Number 1 NU2GGH002193-01-00.
Author information
Authors and affiliations.
Public Health, Societies and Belonging, Human Sciences Research Council, Pretoria, South Africa
Mbuzeleni Hlongwa
School of Nursing and Public Health, University of KwaZulu-Natal, Durban, South Africa
Burden of Disease Research Unit, South African Medical Research Council, Cape Town, South Africa
Wisdom Basera & Edward Nicol
School of Public Health and Family Medicine, University of Cape Town, Cape Town, South Africa
Wisdom Basera
Division of Health Systems and Public Health, Stellenbosch University, Cape Town, South Africa
Edward Nicol
You can also search for this author in PubMed Google Scholar
Contributions
MH drafted the first draft of the manuscript. EN and WB provided critical contributions towards developing and refining the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Mbuzeleni Hlongwa .
Ethics declarations
Ethics approval and consent to participate.
The South African Medical Research Council (SA MRC) Ethics Committee approved this study. Prior to their involvement, we sought both verbal and written informed consent from all eligible study participants. All procedures performed in studies involving human participants adhered to the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from a parent and/or legal guardian for participants below 16 years of age.
Consent for publication
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Hlongwa, M., Basera, W. & Nicol, E. Comparing PrEP initiation rates by service delivery models among high risk adolescent boys and young men in KwaZulu-Natal, South Africa: findings from a population-based prospective study. BMC Public Health 24 , 1151 (2024). https://doi.org/10.1186/s12889-024-18660-1
Download citation
Received : 07 June 2023
Accepted : 18 April 2024
Published : 24 April 2024
DOI : https://doi.org/10.1186/s12889-024-18660-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- PrEP initiation rates
- Service delivery models
- KwaZulu-Natal
- South Africa
BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]
States Direct Districts to Defy New Title IX Rule on Transgender Students

- Share article
In the week since the U.S. Department of Education finalized a rule on the rights of transgender students under Title IX, education leaders in at least five states have urged school districts to ignore it—and activist groups are pressing conservative governors to challenge the directive in federal court.
“We are very proud of our districts that are holding the line, and we will never allow Joe Biden to control our schools and indoctrinate our kids,” said Oklahoma State Superintendent Ryan Walters said at a state board meeting Thursday.
Governors and state education chiefs in Florida , Louisiana , Montana , and South Carolina have also directed districts to defy the rule and signaled potential legal challenges.
The showdown will put district leaders in those five states—and those in other states with legal restrictions on transgender students’ restroom access and pronouns—in a tough but familiar position.
If districts honor the new rule, they risk legal repercussions and political fallout from defying their states. But if they ignore the Education Department’s interpretation of federal law, they risk a civil rights investigation, which comes with the threat of lost federal funding if they cannot reach a resolution.
“It is what I call an untenable position,” said Francisco M. Negrón, Jr., the founder and CEO of K12Counsel, a school law advocacy and policy firm. “It’s clear that, in some jurisdictions at least, schools are going to have to make a decision about which set of rules to follow—with some very consequential outcomes.”
New Title IX rule carries more legal weight
Issued April 19, the Title IX rule, effective Aug. 1, echoes the Biden administration’s long-held position that the law’s prohibition on sex-based discrimination in schools includes protections for sexual orientation and gender identity. A school would violate the law if it “denies a transgender student access to a sex-separate facility or activity consistent with that student’s gender identity.” It also includes directives on how K-12 schools and colleges should handle reports of sexual assault and harassment.
A separate rule related to transgender student athletes is pending.
Civil rights groups praised the rule for asserting protections that transgender students need to attend schools free from harassment and discrimination.
“Today’s rule will be life-changing for so many LGBTQ+ youth and help ensure LGBTQ+ students can receive the same educational experience as their peers: going to dances, safely using the restroom, and writing stories that tell the truth about their own lives,” said a statement from Kelley Robinson, the president of the Human Rights Campaign, an LGBTQ+ advocacy organization.
Conservative state leaders argue the rule violates parental and states’ rights and creates unsafe and uncomfortable conditions for cisgender girls who may be required to share single-sex facilities with transgender classmates.
We will not comply.
“We will not comply,” Florida Gov. Ron DeSantis, a Republican, said in a video posted to X April 24. “We will fight back.”
Moms for Liberty, a conservative activist group, wrote a letter to Republican governors, urging them to “take any and all necessary legal measures to safeguard fundamental parental rights.”
The rule cements a position the Biden administration has held since the president’s first day in office that the U.S. Supreme Court’s 2020 decision in Bostock v. Clayton County, Ga. , which held that Title VII, a law that prohibits sex discrimination in the workplace, bars unequal treatment on the basis of sexual orientation or gender identity. Biden officials argue that legal reasoning should also apply to Title IX.
Because the policy went through a formal rulemaking and public comment process, it carries more legal weight than a similar argument President Barack Obama’s administration detailed in nonbinding guidance it issued in 2016, Negrón said.
The Obama administration later sued North Carolina for passing a “bathroom bill” that violated that guidance. A federal judge later stayed that Title IX interpretation in response to a lawsuit from 13 states, and President Donald Trump’s administration eventually rescinded the Obama-era guidance.
Districts in the middle of state-federal conflict
The new rule, and states’ vows to defy it, could set up a similar legal conflict. At least 11 states have laws that restrict access to restrooms and locker rooms based on sex assigned at birth, the Associated Press reported. Legislatures have also introduced and debated bills that would prohibit schools from using students’ desired names and pronouns, and some have passed laws requiring educators to seek permission from parents or guardians before using them.
Education Department spokesperson Vanessa Harmoush said in a statement that the Title IX regulations were written following “a rigorous process to give complete effect to the Title IX statutory guarantee that no person experiences sex discrimination in federally funded education.”
“As a condition of receiving federal funds, all federally funded schools are obligated to comply with these final regulations, and we look forward to working with school communities all across the country to ensure the Title IX guarantee of nondiscrimination in school is every student’s experience,” that statement said.
It remains to be seen how aggressive the Biden administration will be about investigating violations of the law, or state directives to do so, Negrón said.
“Just because something is enforceable doesn’t mean it will be enforced,” he said.
Sign Up for EdWeek Update
Edweek top school jobs.

Sign Up & Sign In


IMAGES
COMMENTS
Quality sexual health education programs teach students how to: 1. Analyze family, peer, and media influences that impact health. Access valid and reliable health information, products, and services (e.g., STI/HIV testing) Communicate with family, peers, and teachers about issues that affect health. Make informed and thoughtful decisions about ...
School-based sex education is a critical tool for HIV prevention among youth, and research suggests school-based HIV prevention programs are cost-effective when implemented in the context of combination prevention . Intervention evaluations need to go beyond addressing the question of whether school-based sex education increases knowledge and ...
Sex and HIV Education. Beginning in the 1970s, concerns over adolescent pregnancy—and later, HIV/AIDS—galvanized widespread public support for sex education in schools. Most states currently have a policy requiring HIV education, usually in conjunction with broader sex education. Meanwhile, as debate over the relative merits of abstinence ...
Dr Riad also cites the School Based Adolescent Health Program (SBAHP) and Gender Equity Movement in Schools (GEMS) to be active initiatives, particularly in rural contexts. While sex education is technically a part of the education curriculum, its ineffective implementation leaves much to ask for.
school-based HIV prevention and sex education interventions for changing HIV-related knowledge and risk behaviours in low- and middle-income countries (188). The review included 64 interventions presented in 63 articles. Nine interventions were either abstinence-only or emphasized abstinence (also known as the "abstinence-plus approach"); the
The quality and content of sex education in US schools varies widely. There is significant variation in the quality of sex education taught in US schools, leading to disparities in attitudes, health information, and outcomes. ... 26 US states and Washington DC mandate sex education and HIV education. 18 states require that sex education content ...
HIV remains a serious concern among youth, particularly among sexual minority youth (SMY). Risk behaviors including low rates of HIV testing and inconsistent condom use as well as use of substances before sex contribute to these disparities. Therefore, HIV education in schools may be a valuable tool for reducing HIV-related risk behaviors.
Objectives School-based sex education is a cornerstone of HIV prevention for adolescents who continue to bear a disproportionally high HIV burden globally. We systematically reviewed and meta-analyzed the existing evidence for school-based sex education interventions in low- and middle-income countries to determine the efficacy of these interventions in changing HIV-related knowledge and risk ...
According to the 2018 CDC School Health Profiles, fewer than half of high schools and less than a fifth of middle schools teach all 20 topics recommended by the CDC as essential components of sex education. These topics range from basic information on how HIV and other STIs are transmitted — and how to prevent infections — to critical ...
State Profile Highlights. 30 states and the District of Columbia require sex education, either explicitly by law or by proxy via enforced state standards.; 39 states and the District of Columbia specifically require instruction on HIV/AIDS in schools.; 35 states require schools to emphasize the importance of abstinence when sex education or HIV/STI instruction is provided.
As of October 1, 2020: Thirty states and the District of Columbia require public schools teach sex education, 28 of which mandate both sex education and HIV education. Thirty-nine states and the District of Columbia require students receive instruction about HIV. Twenty-two states require that if provided, sex and/or HIV education must be ...
Sex and HIV education programs that are based on a written curriculum and that are implemented among groups of youth in schools, clinics, or other community settings are a promising type of intervention to reduce adolescent sexual risk behaviors. This paper summarizes a review of 83 evaluations of such programs in developing and developed ...
It is widely accepted that young people have a right to sex education because it is a means by which they can protect themselves against unintended pregnancies and sexually transmitted diseases (STDs), including HIV infection. Sex education programs, implemented in diverse venues including schools or medical clinics, typically provide ...
Currently, CDC reaches approximately 2 million students by funding education agencies and a network of leaders in school-based HIV, STD, and pregnancy prevention. These funded partners: Deliver HIV, STD, and pregnancy prevention programs grounded in the latest research. Select and implement effective health education curricula.
and sex characteristics in federally funded education programs, applying the reasoning of the Supreme Court's ruling in Bostock v. Clayton County. Protect people from harm when they are separated or treated differently based on sex in school. The final regulations clarify that a school must not separate or treat people differently based on
This paper reviews 83 studies that measure the impact of curriculum-based sex and HIV education programs on sexual behavior and mediating factors among youth under 25 years anywhere in the world. Two thirds of the programs significantly improved one or more sexual behaviors. The evidence is strong that programs do not hasten or increase sexual behavior but, instead, some programs delay or ...
Objectives: School-based sex education is a cornerstone of HIV prevention for adolescents who continue to bear a disproportionally high HIV burden globally. We systematically reviewed and meta-analyzed the existing evidence for school-based sex education interventions in low- and middle-income countries to determine the efficacy of these interventions in changing HIV-related knowledge and risk ...
2008. Review of Sex, Relationships and HIV Education in SchoolsReview of Sex, Relationships and HIV Education in Schools Prepared for the fi rst meeting of UNESCO's Global Advisory Group meeting 13-14 December 2007 ED.2008/WS/27- cld:2075.8September 2008 3 Acknowledgements This review would not have been possible without the help of many people.
A: High school students, ages 14-18, are most in need of adequate sexual health education. This demographic has a high rate of STDs as compared to other age groups, and, according to the CDC, 44% of males and 43% of females participate in intercourse by age 17. 27, 28 Evidence shows that adequate sex education can increase contraceptive use, decreasing STD and pregnancy rates for teenagers ...
Unfortunately, just 30 states and the District of Columbia require sex education to be taught in schools, ... The program focuses on young people aged 10-19 who are homeless, in or aging out of foster care, living with HIV or AIDS, victims of human trafficking or living in areas with high adolescent birth rates. It also focuses on people ...
Aims. (1) To systematically review existing reviews of Sex Education (SE) of school-based (face-to-face), digital platforms and blended learning programs for adolescent populations in high-income countries. (2) To summarize evidence relating to effectiveness. 2.2.
Evidence consistently shows that high-quality sexuality education delivers positive health outcomes, with lifelong impacts. Young people are more likely to delay the onset of sexual activity - and when they do have sex, to practice safer sex - when they are better informed about their sexuality, sexual health and their rights.
Sex education in schools can be taught by a classroom teacher, school nurse or an outside speaker, and often begins in fifth grade. For some parents, the term "sex ed" conjures memories of dated ...
Decisions about sex education are usually made at the state and local level — no federal laws dictate what sex education should look like or how it should be taught in schools.. Almost every state in the U.S. has some guidance around sex education. Currently, 39 states and the District of Columbia require that HIV and/or sex education is covered in school.
Objective: To review the impact of sex education and HIV education interventions in schools in developing countries on both risk behaviours for HIV and the psychosocial factors that affect them. Methods: We conducted a systematic review. Searches identified studies in developing countries that evaluated interventions using either experimental or strong quasi-experimental designs and measured ...
Under current Oklahoma law, sex education is not required, but schools must provide HIV/AIDS prevention instruction and health education. If a school offers sex education, parents can choose to ...
The importance of sex education in guiding adolescents cannot be overstated. ... HIV, and unplanned pregnancy by encouraging safer sexual practices as well as reducing sexual violence and ...
Pre-exposure prophylaxis (PrEP) is an HIV prevention strategy that can reduce the risk of HIV acquisition by more than 90% if taken consistently. Although South Africa has been implementing PrEP since 2016, initially for selected population groups before expanding access to more people, there is a dearth of research focused on PrEP among adolescent boys and young men (ABYM), despite them ...
Issued April 19, the Title IX rule, effective Aug. 1, echoes the Biden administration's long-held position that the law's prohibition on sex-based discrimination in schools includes ...