- Privacy Policy

Home » Research Paper Abstract – Writing Guide and Examples

Research Paper Abstract – Writing Guide and Examples
Table of Contents

Research Paper Abstract
Research Paper Abstract is a brief summary of a research pape r that describes the study’s purpose, methods, findings, and conclusions . It is often the first section of the paper that readers encounter, and its purpose is to provide a concise and accurate overview of the paper’s content. The typical length of an abstract is usually around 150-250 words, and it should be written in a concise and clear manner.
Research Paper Abstract Structure
The structure of a research paper abstract usually includes the following elements:
- Background or Introduction: Briefly describe the problem or research question that the study addresses.
- Methods : Explain the methodology used to conduct the study, including the participants, materials, and procedures.
- Results : Summarize the main findings of the study, including statistical analyses and key outcomes.
- Conclusions : Discuss the implications of the study’s findings and their significance for the field, as well as any limitations or future directions for research.
- Keywords : List a few keywords that describe the main topics or themes of the research.
How to Write Research Paper Abstract
Here are the steps to follow when writing a research paper abstract:
- Start by reading your paper: Before you write an abstract, you should have a complete understanding of your paper. Read through the paper carefully, making sure you understand the purpose, methods, results, and conclusions.
- Identify the key components : Identify the key components of your paper, such as the research question, methods used, results obtained, and conclusion reached.
- Write a draft: Write a draft of your abstract, using concise and clear language. Make sure to include all the important information, but keep it short and to the point. A good rule of thumb is to keep your abstract between 150-250 words.
- Use clear and concise language : Use clear and concise language to explain the purpose of your study, the methods used, the results obtained, and the conclusions drawn.
- Emphasize your findings: Emphasize your findings in the abstract, highlighting the key results and the significance of your study.
- Revise and edit: Once you have a draft, revise and edit it to ensure that it is clear, concise, and free from errors.
- Check the formatting: Finally, check the formatting of your abstract to make sure it meets the requirements of the journal or conference where you plan to submit it.
Research Paper Abstract Examples
Research Paper Abstract Examples could be following:
Title : “The Effectiveness of Cognitive-Behavioral Therapy for Treating Anxiety Disorders: A Meta-Analysis”
Abstract : This meta-analysis examines the effectiveness of cognitive-behavioral therapy (CBT) in treating anxiety disorders. Through the analysis of 20 randomized controlled trials, we found that CBT is a highly effective treatment for anxiety disorders, with large effect sizes across a range of anxiety disorders, including generalized anxiety disorder, panic disorder, and social anxiety disorder. Our findings support the use of CBT as a first-line treatment for anxiety disorders and highlight the importance of further research to identify the mechanisms underlying its effectiveness.
Title : “Exploring the Role of Parental Involvement in Children’s Education: A Qualitative Study”
Abstract : This qualitative study explores the role of parental involvement in children’s education. Through in-depth interviews with 20 parents of children in elementary school, we found that parental involvement takes many forms, including volunteering in the classroom, helping with homework, and communicating with teachers. We also found that parental involvement is influenced by a range of factors, including parent and child characteristics, school culture, and socio-economic status. Our findings suggest that schools and educators should prioritize building strong partnerships with parents to support children’s academic success.
Title : “The Impact of Exercise on Cognitive Function in Older Adults: A Systematic Review and Meta-Analysis”
Abstract : This paper presents a systematic review and meta-analysis of the existing literature on the impact of exercise on cognitive function in older adults. Through the analysis of 25 randomized controlled trials, we found that exercise is associated with significant improvements in cognitive function, particularly in the domains of executive function and attention. Our findings highlight the potential of exercise as a non-pharmacological intervention to support cognitive health in older adults.
When to Write Research Paper Abstract
The abstract of a research paper should typically be written after you have completed the main body of the paper. This is because the abstract is intended to provide a brief summary of the key points and findings of the research, and you can’t do that until you have completed the research and written about it in detail.
Once you have completed your research paper, you can begin writing your abstract. It is important to remember that the abstract should be a concise summary of your research paper, and should be written in a way that is easy to understand for readers who may not have expertise in your specific area of research.
Purpose of Research Paper Abstract
The purpose of a research paper abstract is to provide a concise summary of the key points and findings of a research paper. It is typically a brief paragraph or two that appears at the beginning of the paper, before the introduction, and is intended to give readers a quick overview of the paper’s content.
The abstract should include a brief statement of the research problem, the methods used to investigate the problem, the key results and findings, and the main conclusions and implications of the research. It should be written in a clear and concise manner, avoiding jargon and technical language, and should be understandable to a broad audience.
The abstract serves as a way to quickly and easily communicate the main points of a research paper to potential readers, such as academics, researchers, and students, who may be looking for information on a particular topic. It can also help researchers determine whether a paper is relevant to their own research interests and whether they should read the full paper.
About the author
Muhammad Hassan
Researcher, Academic Writer, Web developer
You may also like

Chapter Summary & Overview – Writing Guide...

Research Objectives – Types, Examples and...

Research Contribution – Thesis Guide

How to Publish a Research Paper – Step by Step...

Research Methodology – Types, Examples and...

Significance of the Study – Examples and Writing...

- Our History
- The Council
- Verna Wright Prize
- The Secretariat
- Key Documents and Policies
- 2024 Conference
- Abstract Submission Guidance 2024
- Past Conferences
- Past Keynote Speakers
- Courses and Lectures
- Co-Hosted Events
- External Events
- Research – Presenting Abstracts
- Research Projects
- Research Links
- Research Councils
- Qualitative Research Abstracts
- Fellowships, Studentships and Awards
- Published Abstracts
- Training Awards
- General Links
- Professional Organisations
- University and Research Vacancies
- Newsletters
- Council Reports and Society Forms
- SRR Membership
- Symposia Presentations
- Members Newsletter
- Business Minutes
- Search for:
GUIDANCE ON SUBMISSION OF QUALITATIVE RESEARCH ABSTRACTS
General guidance
Authors should refer to the general information and guidelines contained in the Society’s “Guidance for Submission of Abstracts”. The general guidance therein applies to qualitative research abstracts. This includes the maximum permitted limit of 250 words, and the instruction that abstracts should be structured. In keeping with all submissions to the Society, subsequent presentation must reflect and elaborate on the abstract. Research studies or findings not referred to in the abstract should not be presented.
This document contains specific guidance on the content of qualitative research abstracts.
How guidance on content is to be applied by authors and Council.
Council recognises that the nature of qualitative research makes its comprehensive communication within short abstracts a challenge. Therefore, whilst the key areas to be included within abstracts are set out below, it is recognised that emphasis on each area will vary in different cases, and that not every listed sub-area will be covered. Certain elements are likely to receive greater attention at the time of presentation than within the abstract. In particular, presentation of the paper should include sufficient empirical data to allow judgement of the conclusions drawn.
Content of abstracts
- Research question/objective and design: clear statement of the research question/objective and its relevance. Methodological or theoretical perspectives should be clearly outlined.
- Population and sampling: who the subjects were and what sampling strategies were used .
- Methods of data collection: clear exposition of data collection: access, selection, method of collection, type of data, relationship of researcher to subjects/setting (what data were collected, from where/whom, by whom)
- Quality of data and analysis: strategies to enhance quality of data analysis e.g. triangulation, respondent validation; and to enhance validity e.g. attention to negative cases, consideration of alternative explanations, team analysis, peer review panels
- Application of critical thinking to analysis: attention to the influence of the researcher on data collected and on analysis. Critical approach to the status of data collected
- Theoretical and empirical context: evidence that design and analysis take into account and add to previous knowledge
- Conclusions: justified in relation to data collected, sufficient original data presented to substantiate interpretations, reasoned consideration of transferability to groups/settings beyond those studied
Username or email address *
Password *
Remember me Log in
Lost your password?
Abstraction and interpretation during the qualitative content analysis process
Affiliations.
- 1 Department of Nursing, Umeå University, SE-90187, Umeå, Sweden. Electronic address: [email protected].
- 2 Department of Nursing, Umeå University, SE-90187, Umeå, Sweden.
- 3 Department of Nursing, Umeå University, SE-90187, Umeå, Sweden; Department of Health Sciences, University West, Trollhättan, Sweden.
- PMID: 32505813
- DOI: 10.1016/j.ijnurstu.2020.103632
Qualitative content analysis and other 'standardised' methods are sometimes considered to be technical tools used for basic, superficial, and simple sorting of text, and their results lack depth, scientific rigour, and evidence. To strengthen the trustworthiness of qualitative content analyses, we focus on abstraction and interpretation during the analytic process. To our knowledge, descriptions of these concepts are sparse; this paper therefore aims to elaborate on and exemplify the distinction and relation between abstraction and interpretation during the different phases of the process of qualitative content analysis. We address the relations between abstraction and interpretation when selecting, condensing, and coding meaning units and creating categories and themes on various levels. The examples used are based on our experiences of teaching and supervising students at various levels. We also highlight the phases of de-contextualisation and re-contextualisation in describing the analytic process. We argue that qualitative content analysis can be both descriptive and interpretative. When the data allow interpretations of the latent content, qualitative content analysis reveals both depth and meaning in participants' utterances.
Keywords: Abstraction; De-contextualisation; Interpretation; Qualitative content analysis; Re-contextualisation.
Copyright © 2020. Published by Elsevier Ltd.
Publication types
- Abstracting and Indexing / methods*
- Data Analysis*
- Qualitative Research
Writing an Abstract for Your Research Paper
Definition and Purpose of Abstracts
An abstract is a short summary of your (published or unpublished) research paper, usually about a paragraph (c. 6-7 sentences, 150-250 words) long. A well-written abstract serves multiple purposes:
- an abstract lets readers get the gist or essence of your paper or article quickly, in order to decide whether to read the full paper;
- an abstract prepares readers to follow the detailed information, analyses, and arguments in your full paper;
- and, later, an abstract helps readers remember key points from your paper.
It’s also worth remembering that search engines and bibliographic databases use abstracts, as well as the title, to identify key terms for indexing your published paper. So what you include in your abstract and in your title are crucial for helping other researchers find your paper or article.
If you are writing an abstract for a course paper, your professor may give you specific guidelines for what to include and how to organize your abstract. Similarly, academic journals often have specific requirements for abstracts. So in addition to following the advice on this page, you should be sure to look for and follow any guidelines from the course or journal you’re writing for.
The Contents of an Abstract
Abstracts contain most of the following kinds of information in brief form. The body of your paper will, of course, develop and explain these ideas much more fully. As you will see in the samples below, the proportion of your abstract that you devote to each kind of information—and the sequence of that information—will vary, depending on the nature and genre of the paper that you are summarizing in your abstract. And in some cases, some of this information is implied, rather than stated explicitly. The Publication Manual of the American Psychological Association , which is widely used in the social sciences, gives specific guidelines for what to include in the abstract for different kinds of papers—for empirical studies, literature reviews or meta-analyses, theoretical papers, methodological papers, and case studies.
Here are the typical kinds of information found in most abstracts:
- the context or background information for your research; the general topic under study; the specific topic of your research
- the central questions or statement of the problem your research addresses
- what’s already known about this question, what previous research has done or shown
- the main reason(s) , the exigency, the rationale , the goals for your research—Why is it important to address these questions? Are you, for example, examining a new topic? Why is that topic worth examining? Are you filling a gap in previous research? Applying new methods to take a fresh look at existing ideas or data? Resolving a dispute within the literature in your field? . . .
- your research and/or analytical methods
- your main findings , results , or arguments
- the significance or implications of your findings or arguments.
Your abstract should be intelligible on its own, without a reader’s having to read your entire paper. And in an abstract, you usually do not cite references—most of your abstract will describe what you have studied in your research and what you have found and what you argue in your paper. In the body of your paper, you will cite the specific literature that informs your research.
When to Write Your Abstract
Although you might be tempted to write your abstract first because it will appear as the very first part of your paper, it’s a good idea to wait to write your abstract until after you’ve drafted your full paper, so that you know what you’re summarizing.
What follows are some sample abstracts in published papers or articles, all written by faculty at UW-Madison who come from a variety of disciplines. We have annotated these samples to help you see the work that these authors are doing within their abstracts.
Choosing Verb Tenses within Your Abstract
The social science sample (Sample 1) below uses the present tense to describe general facts and interpretations that have been and are currently true, including the prevailing explanation for the social phenomenon under study. That abstract also uses the present tense to describe the methods, the findings, the arguments, and the implications of the findings from their new research study. The authors use the past tense to describe previous research.
The humanities sample (Sample 2) below uses the past tense to describe completed events in the past (the texts created in the pulp fiction industry in the 1970s and 80s) and uses the present tense to describe what is happening in those texts, to explain the significance or meaning of those texts, and to describe the arguments presented in the article.
The science samples (Samples 3 and 4) below use the past tense to describe what previous research studies have done and the research the authors have conducted, the methods they have followed, and what they have found. In their rationale or justification for their research (what remains to be done), they use the present tense. They also use the present tense to introduce their study (in Sample 3, “Here we report . . .”) and to explain the significance of their study (In Sample 3, This reprogramming . . . “provides a scalable cell source for. . .”).
Sample Abstract 1
From the social sciences.
Reporting new findings about the reasons for increasing economic homogamy among spouses
Gonalons-Pons, Pilar, and Christine R. Schwartz. “Trends in Economic Homogamy: Changes in Assortative Mating or the Division of Labor in Marriage?” Demography , vol. 54, no. 3, 2017, pp. 985-1005.
![abstract of qualitative research example “The growing economic resemblance of spouses has contributed to rising inequality by increasing the number of couples in which there are two high- or two low-earning partners. [Annotation for the previous sentence: The first sentence introduces the topic under study (the “economic resemblance of spouses”). This sentence also implies the question underlying this research study: what are the various causes—and the interrelationships among them—for this trend?] The dominant explanation for this trend is increased assortative mating. Previous research has primarily relied on cross-sectional data and thus has been unable to disentangle changes in assortative mating from changes in the division of spouses’ paid labor—a potentially key mechanism given the dramatic rise in wives’ labor supply. [Annotation for the previous two sentences: These next two sentences explain what previous research has demonstrated. By pointing out the limitations in the methods that were used in previous studies, they also provide a rationale for new research.] We use data from the Panel Study of Income Dynamics (PSID) to decompose the increase in the correlation between spouses’ earnings and its contribution to inequality between 1970 and 2013 into parts due to (a) changes in assortative mating, and (b) changes in the division of paid labor. [Annotation for the previous sentence: The data, research and analytical methods used in this new study.] Contrary to what has often been assumed, the rise of economic homogamy and its contribution to inequality is largely attributable to changes in the division of paid labor rather than changes in sorting on earnings or earnings potential. Our findings indicate that the rise of economic homogamy cannot be explained by hypotheses centered on meeting and matching opportunities, and they show where in this process inequality is generated and where it is not.” (p. 985) [Annotation for the previous two sentences: The major findings from and implications and significance of this study.]](https://writing.wisc.edu/wp-content/uploads/sites/535/2019/08/Abstract-1.png)
Sample Abstract 2
From the humanities.
Analyzing underground pulp fiction publications in Tanzania, this article makes an argument about the cultural significance of those publications
Emily Callaci. “Street Textuality: Socialism, Masculinity, and Urban Belonging in Tanzania’s Pulp Fiction Publishing Industry, 1975-1985.” Comparative Studies in Society and History , vol. 59, no. 1, 2017, pp. 183-210.
![abstract of qualitative research example “From the mid-1970s through the mid-1980s, a network of young urban migrant men created an underground pulp fiction publishing industry in the city of Dar es Salaam. [Annotation for the previous sentence: The first sentence introduces the context for this research and announces the topic under study.] As texts that were produced in the underground economy of a city whose trajectory was increasingly charted outside of formalized planning and investment, these novellas reveal more than their narrative content alone. These texts were active components in the urban social worlds of the young men who produced them. They reveal a mode of urbanism otherwise obscured by narratives of decolonization, in which urban belonging was constituted less by national citizenship than by the construction of social networks, economic connections, and the crafting of reputations. This article argues that pulp fiction novellas of socialist era Dar es Salaam are artifacts of emergent forms of male sociability and mobility. In printing fictional stories about urban life on pilfered paper and ink, and distributing their texts through informal channels, these writers not only described urban communities, reputations, and networks, but also actually created them.” (p. 210) [Annotation for the previous sentences: The remaining sentences in this abstract interweave other essential information for an abstract for this article. The implied research questions: What do these texts mean? What is their historical and cultural significance, produced at this time, in this location, by these authors? The argument and the significance of this analysis in microcosm: these texts “reveal a mode or urbanism otherwise obscured . . .”; and “This article argues that pulp fiction novellas. . . .” This section also implies what previous historical research has obscured. And through the details in its argumentative claims, this section of the abstract implies the kinds of methods the author has used to interpret the novellas and the concepts under study (e.g., male sociability and mobility, urban communities, reputations, network. . . ).]](https://writing.wisc.edu/wp-content/uploads/sites/535/2019/08/Abstract-2.png)
Sample Abstract/Summary 3
From the sciences.
Reporting a new method for reprogramming adult mouse fibroblasts into induced cardiac progenitor cells
Lalit, Pratik A., Max R. Salick, Daryl O. Nelson, Jayne M. Squirrell, Christina M. Shafer, Neel G. Patel, Imaan Saeed, Eric G. Schmuck, Yogananda S. Markandeya, Rachel Wong, Martin R. Lea, Kevin W. Eliceiri, Timothy A. Hacker, Wendy C. Crone, Michael Kyba, Daniel J. Garry, Ron Stewart, James A. Thomson, Karen M. Downs, Gary E. Lyons, and Timothy J. Kamp. “Lineage Reprogramming of Fibroblasts into Proliferative Induced Cardiac Progenitor Cells by Defined Factors.” Cell Stem Cell , vol. 18, 2016, pp. 354-367.
![abstract of qualitative research example “Several studies have reported reprogramming of fibroblasts into induced cardiomyocytes; however, reprogramming into proliferative induced cardiac progenitor cells (iCPCs) remains to be accomplished. [Annotation for the previous sentence: The first sentence announces the topic under study, summarizes what’s already known or been accomplished in previous research, and signals the rationale and goals are for the new research and the problem that the new research solves: How can researchers reprogram fibroblasts into iCPCs?] Here we report that a combination of 11 or 5 cardiac factors along with canonical Wnt and JAK/STAT signaling reprogrammed adult mouse cardiac, lung, and tail tip fibroblasts into iCPCs. The iCPCs were cardiac mesoderm-restricted progenitors that could be expanded extensively while maintaining multipo-tency to differentiate into cardiomyocytes, smooth muscle cells, and endothelial cells in vitro. Moreover, iCPCs injected into the cardiac crescent of mouse embryos differentiated into cardiomyocytes. iCPCs transplanted into the post-myocardial infarction mouse heart improved survival and differentiated into cardiomyocytes, smooth muscle cells, and endothelial cells. [Annotation for the previous four sentences: The methods the researchers developed to achieve their goal and a description of the results.] Lineage reprogramming of adult somatic cells into iCPCs provides a scalable cell source for drug discovery, disease modeling, and cardiac regenerative therapy.” (p. 354) [Annotation for the previous sentence: The significance or implications—for drug discovery, disease modeling, and therapy—of this reprogramming of adult somatic cells into iCPCs.]](https://writing.wisc.edu/wp-content/uploads/sites/535/2019/08/Abstract-3.png)
Sample Abstract 4, a Structured Abstract
Reporting results about the effectiveness of antibiotic therapy in managing acute bacterial sinusitis, from a rigorously controlled study
Note: This journal requires authors to organize their abstract into four specific sections, with strict word limits. Because the headings for this structured abstract are self-explanatory, we have chosen not to add annotations to this sample abstract.
Wald, Ellen R., David Nash, and Jens Eickhoff. “Effectiveness of Amoxicillin/Clavulanate Potassium in the Treatment of Acute Bacterial Sinusitis in Children.” Pediatrics , vol. 124, no. 1, 2009, pp. 9-15.
“OBJECTIVE: The role of antibiotic therapy in managing acute bacterial sinusitis (ABS) in children is controversial. The purpose of this study was to determine the effectiveness of high-dose amoxicillin/potassium clavulanate in the treatment of children diagnosed with ABS.
METHODS : This was a randomized, double-blind, placebo-controlled study. Children 1 to 10 years of age with a clinical presentation compatible with ABS were eligible for participation. Patients were stratified according to age (<6 or ≥6 years) and clinical severity and randomly assigned to receive either amoxicillin (90 mg/kg) with potassium clavulanate (6.4 mg/kg) or placebo. A symptom survey was performed on days 0, 1, 2, 3, 5, 7, 10, 20, and 30. Patients were examined on day 14. Children’s conditions were rated as cured, improved, or failed according to scoring rules.
RESULTS: Two thousand one hundred thirty-five children with respiratory complaints were screened for enrollment; 139 (6.5%) had ABS. Fifty-eight patients were enrolled, and 56 were randomly assigned. The mean age was 6630 months. Fifty (89%) patients presented with persistent symptoms, and 6 (11%) presented with nonpersistent symptoms. In 24 (43%) children, the illness was classified as mild, whereas in the remaining 32 (57%) children it was severe. Of the 28 children who received the antibiotic, 14 (50%) were cured, 4 (14%) were improved, 4(14%) experienced treatment failure, and 6 (21%) withdrew. Of the 28children who received placebo, 4 (14%) were cured, 5 (18%) improved, and 19 (68%) experienced treatment failure. Children receiving the antibiotic were more likely to be cured (50% vs 14%) and less likely to have treatment failure (14% vs 68%) than children receiving the placebo.
CONCLUSIONS : ABS is a common complication of viral upper respiratory infections. Amoxicillin/potassium clavulanate results in significantly more cures and fewer failures than placebo, according to parental report of time to resolution.” (9)
Some Excellent Advice about Writing Abstracts for Basic Science Research Papers, by Professor Adriano Aguzzi from the Institute of Neuropathology at the University of Zurich:

Academic and Professional Writing
This is an accordion element with a series of buttons that open and close related content panels.
Analysis Papers
Reading Poetry
A Short Guide to Close Reading for Literary Analysis
Using Literary Quotations
Play Reviews
Writing a Rhetorical Précis to Analyze Nonfiction Texts
Incorporating Interview Data
Grant Proposals
Planning and Writing a Grant Proposal: The Basics
Additional Resources for Grants and Proposal Writing
Job Materials and Application Essays
Writing Personal Statements for Ph.D. Programs
- Before you begin: useful tips for writing your essay
- Guided brainstorming exercises
- Get more help with your essay
- Frequently Asked Questions
Resume Writing Tips
CV Writing Tips
Cover Letters
Business Letters
Proposals and Dissertations
Resources for Proposal Writers
Resources for Dissertators
Research Papers
Planning and Writing Research Papers
Quoting and Paraphrasing
Writing Annotated Bibliographies
Creating Poster Presentations
Thank-You Notes
Advice for Students Writing Thank-You Notes to Donors
Reading for a Review
Critical Reviews
Writing a Review of Literature
Scientific Reports
Scientific Report Format
Sample Lab Assignment
Writing for the Web
Writing an Effective Blog Post
Writing for Social Media: A Guide for Academics
University Library, University of Illinois at Urbana-Champaign

Qualitative Data Analysis: Find Methods Examples
- Atlas.ti web
- R for text analysis
- Microsoft Excel & spreadsheets
- Other options
- Planning Qual Data Analysis
- Free Tools for QDA
- QDA with NVivo
- QDA with Atlas.ti
- QDA with MAXQDA
- PKM for QDA
- QDA with Quirkos
- Working Collaboratively
- Qualitative Methods Texts
- Transcription
- Data organization
- Example Publications
- Find Methods Examples
Locating Methods Examples
Find dissertations that cite a core methods work.
You can conduct a cited reference search in the ProQuest Dissertations & Theses database.
Example Two Heading
Example Two Body
Example Three Heading
Example Three Body
- << Previous: Example Publications
- Last Updated: Jun 6, 2024 9:59 AM
- URL: https://guides.library.illinois.edu/qualitative
Vignettes: an innovative qualitative data collection tool in Medical Education research
- Open access
- Published: 05 June 2024
Cite this article
You have full access to this open access article

- Sylvia Joshua Western ORCID: orcid.org/0000-0002-4397-6746 1 ,
- Brian McEllistrem 1 ,
- Jane Hislop 1 ,
- Alan Jaap 1 &
- David Hope 1
This article describes how to make use of exemplar vignettes in qualitative medial education research. Vignettes are particularly useful in prompting discussion with participants, when using real-life case examples may breach confidentiality. As such, using vignettes allows researchers to gain insight into participants’ thinking in an ethically sensitive way.
Avoid common mistakes on your manuscript.
Vignettes are written, visual, or oral stimuli portraying realistic events in a focussed manner, purposefully aligned with the research objectives and paradigms to elicit responses from research participants [ 1 ]. They have been used in qualitative research to explore physical, social, and mental health–related topics. Although clinical vignettes are widely used in teaching and assessment, vignettes are under-utilised as a research tool in medical education. In this article, we outline the ways in which we found vignettes to be helpful in addressing our research aims prompting a conversation on how they might be used in other medical education research contexts, particularly when working with sensitive issues.
We used vignettes within individual semi-structured interviews, to explore how medical educators interpreted different test-wise behaviours (“ skills and strategies that are not related to the construct being measured on the test but that facilitate an increased test score ”[ 2 ]). We opted to use vignettes for the following reasons:
Akin to clinical vignettes, they enable usage of anonymised and fictionalised version of real-life case studies, protecting the identity and confidentiality of the original individuals [ 3 ]. Vignettes retained the essence of the event but potential identifiers or personal information from the original were redacted or anonymized.
Realistic scenarios support the exploration of sensitive topics which can generate authentic ethical dilemmas. Instead of asking “Have you ever tried to trick your examiner into giving you more marks”? - a question which might cause distress or harm to participants, we could posit a vignette and ask our participants for a third-person perspective. Vignettes therefore promote participants’ psychological safety by providing an alternative non-confronting and safer avenue to discuss value-laden constructs [ 1 ].
When discussing complex ambiguous topics, they provide a focus to help participants orient to the specific matter at hand [ 3 ]. Vignettes help define and communicate the context, setting, character, and situation succinctly.
Using an established framework of Skilling & Stylianides [ 1 ], we constructed five vignettes portraying a spectrum of test-wise behaviours. We drew on informal conversations with stakeholders, online forums, our professional experience, academic literature, and knowledge of the local context to draft the vignettes. Our aim was to understand how people make meaning, what guided their decisions and reactions to test-wise behaviours. Following feedback from experts and several pilot interviews, we revised the vignettes. As such we found that the process of building vignettes was iterative, collaborative, and continuously evolving.
Using previous case studies employing vignettes for data collection, we reflected on the iterative process of constructing, peer and expert reviewing, piloting, and deploying vignettes to eight participants. Participants were staff and students at Edinburgh Medical School. By contemplating the decision-making pathway that aided vignette construction, studying the reflective notes of the interviewer, thematically analysing interview transcripts, and engaging in an ongoing discussion and feedback loops with our expert and supervisory panel, we identified eight factors making vignettes especially useful:
By controlling the age, sex, and ethnicity of subjects, we could explore how participants interpreted and reacted to different test-wise behaviours of different students.
Following discussion, participants commented on the realism of the vignettes, allowing for iteration of the vignettes over time.
Vignettes facilitated subjective interpretation of complex situations and allowed for intentional reflection on thoughts and actions.
Participants had the agency to discuss their own attitudes in relation to the vignettes and used them to explore their real-life experiences.
We tailored the frequency and type of vignette based on the participant’s role, and selected vignettes to explore issues under-discussed in previous interviews.
Criticising real actions and guidelines can be challenging. Discussing hypothetical vignettes allowed for openness, honesty, and pragmatic answers.
Exposing participants to novel vignettes helped the researchers compare their expectations and beliefs to participant views. Participants found the vignettes plausible, which suggested the researchers had a defensible understanding of the topic.
We can compare the interpretation of the same vignette by different individuals in different roles to understand the underlying rationale for their differing perspectives. Follow-up interviews allow for the exploration of changes over time.
Figure 1 shows an exemplar vignette with excerpts of participant responses. Rather than ask how they would feel if an exam candidate used false empathy to conceal their lack of content knowledge, we used Nat vignette (in Fig. 1 ) as a realistic case study to facilitate discussion. The broader themes in the left side of the infographic (Fig. 1 ) speak to some of the factors identified previously, acting as a teaser facilitating the readers to think through the participant responses. For example, the snippet “I can think of it happening to me at least once” connects to plausibility and realism - the participant thinks that this is a plausible scene in their context, and it seems real to them.
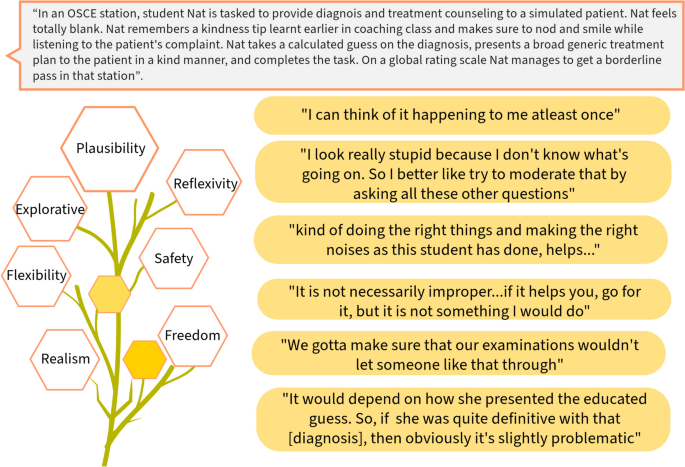
Example vignette with excerpts of participant responses
Firstly, a challenge we faced pertained to participant engagement. While all participants found the example vignette (in Fig. 1 ) both plausible and relatable, the pattern of engagement varied among them. Some used it as a springboard to delve into their own real-life stories, while others found it challenging to reconcile the artificial and hypothetical nature of the vignette. The effectiveness of vignettes hinges on participant engagement. Drawing from our experience and the supporting literature, we found that vignettes must be relatable [ 3 ], plausible [ 3 ], and situated in context [ 1 ]. Participants must be oriented to the vignette method before interview and be given the vignettes at appropriate times during the interview. It is essential when using vignettes to gauge and promote engagement during the interview. Tailored questions and prompts are helpful strategies to promote such engagement. Secondly, we agree that however realistic vignettes are, they are “not real”, therefore participants’ responses to hypothetical vignettes might not perfectly align with their reactions to real-life situations, for instance, considering their underlying motivational relevance to the different contexts - research environment and real-life [ 3 ]. Researchers should remain aware of these challenges and interpret their findings with caution [ 3 ].
In conclusion, our use of vignettes was an innovative alternative to using high-stakes, confidential real-life case examples in qualitative research. Usage of vignette opens new possibilities in medical education research: they can be used within questionnaire surveys, individual and focus group interviews, or as ethnographic field notes. They offer a versatile approach to allow exploration of high-stakes, sensitive, and ethically contentious issues with participants in a safe way. Therefore, researchers can benefit significantly from applying vignettes in their own research.
Data Availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Skilling K, Stylianides GJ. Using vignettes in educational research: a framework for vignette construction. Int J Res Method Educ. 2020;43(5):541–56. https://doi.org/10.1080/1743727X.2019.1704243 .
Article Google Scholar
American Psychological Association. Testwise. APA Dictionary of Psychology. https://dictionary.apa.org/testwise . Updated April 19, 2018. Accessed 20 May 2024.
Jenkins N, Bloor MJ, Fischer J, Berney L, Neale J. Putting it in context: the use of vignettes in qualitative interviewing. Qual Res. 2010;10(2):175–98.
Download references
Author information
Authors and affiliations.
College of Medicine & Veterinary Medicine, The University of Edinburgh, Edinburgh, UK
Sylvia Joshua Western, Brian McEllistrem, Jane Hislop, Alan Jaap & David Hope
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Sylvia Joshua Western .
Ethics declarations
Conflict of interest.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Western, S.J., McEllistrem, B., Hislop, J. et al. Vignettes: an innovative qualitative data collection tool in Medical Education research. Med.Sci.Educ. (2024). https://doi.org/10.1007/s40670-024-02074-0
Download citation
Accepted : 10 May 2024
Published : 05 June 2024
DOI : https://doi.org/10.1007/s40670-024-02074-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Qualitative research
- Medical education
- Data collection
- Find a journal
- Publish with us
- Track your research
- Open access
- Published: 06 June 2024
Flemish critical care nurses’ experiences regarding the influence of work-related demands on their health: a descriptive interpretive qualitative study
- Lukas Billiau ORCID: orcid.org/0009-0009-9563-0999 1 ,
- Larissa Bolliger 2 ,
- Els clays 2 ,
- Kristof Eeckloo 1 , 2 &
- Margo Ketels 2
BMC Nursing volume 23 , Article number: 387 ( 2024 ) Cite this article
Metrics details
Critical care nurses (CCNs) around the globe face other health challenges compared to their peers in general hospital nursing. Moreover, the nursing workforce grapples with persistent staffing shortages. In light of these circumstances, developing a sustainable work environment is imperative to retain the current nursing workforce. Consequently, this study aimed to gain insight into the recalled experiences of CCNs in dealing with the physical and psychosocial influences of work-related demands on their health while examining the environments in which they operate. The second aim was to explore the complex social and psychological processes through which CCNs navigate these work-related demands across various CCN wards.
A qualitative study following Thorne’s interpretive descriptive approach was conducted. From October 2022 to April 2023, six focus groups were organised. Data from a diverse sample of 27 Flemish CCNs engaged in physically demanding roles from three CCN wards were collected. The Qualitative Analysis Guide of Leuven was applied to support the constant comparison process.
Participants reported being exposed to occupational physical activity, emotional, quantitative, and cognitive work-related demands, adverse patient behaviour, and poor working time quality. Exposure to these work-related demands was perceived as harmful, potentially resulting in physical, mental, and psychosomatic strain, as well as an increased turnover intention. In response to these demands, participants employed various strategies for mitigation, including seeking social support, exerting control over their work, utilising appropriate equipment, recognising rewards, and engaging in leisure-time physical activity.
Conclusions
CCNs’ health is challenged by work-related demands that are not entirely covered by the traditional quantitative frameworks used in research on psychologically healthy work. Therefore, future studies should focus on improving such frameworks by exploring the role of psychosocial and organisational factors in more detail. This study has important implications for workplace health promotion with a view on preventing work absenteeism and drop-out in the long run, as it offers strong arguments to promote sufficient risk management strategies, schedule flexibility, uninterrupted off-job recovery time, and positive management, which can prolong the well-being and sustainable careers of the CCN workforce.
Peer Review reports
Globally, the nursing profession is a strenuous occupation with high levels of work-related demands, leading to adverse health outcomes for nurses [ 1 ], reduced marital and life satisfaction [ 2 ], absenteeism, and high costs for society [ 3 ]. In addition, the nursing workforce has to address staffing shortages due to the reduced number of individuals entering the nursing profession [ 4 ], the ageing working population [ 5 ], and the increased number of nurses in premature retirement [ 6 , 7 ].
Especially critical care nurses (CCNs), who specialise in managing life-threatening diseases across all age groups, work in an exceptionally demanding environment [ 8 ]. Increasing evidence suggests that CCNs’ health is mainly challenged by five work-related demands, namely, occupational physical activity (OPA) [ 1 ], shiftwork [ 9 ], and quantitative [ 10 ], cognitive [ 11 ], and emotional work-related demands [ 12 ]. Among CCNs, OPA involves various physically demanding tasks, such as forward bending and isometric neck postures, heavy lifting, prolonged standing, and long-distance walking [ 1 , 9 ]. With continued exposure to OPA, musculoskeletal disorders can arise in terms of pain-related complaints of the wrists, back, thigh, knees, and feet [ 1 ]. However, many studies have reported that engaging in regular leisure-time physical activity has a beneficial influence on health, while OPA may have no beneficial, or even adverse, influence on health [ 13 ]. These conflicting health influences are indicated as the “physical activity health paradox” [ 13 ] and might be explained by differences in duration, intensity, recovery opportunities, and physiological responses [ 14 , 15 ].
In addition to OPA is shift work, which is the amount of time an individual works outside the typical nine AM to five PM schedule, known to impact CCNs’ health through circadian rhythm disruption, fatigue, and social isolation [ 16 , 17 , 18 ]. First, circadian rhythm disruption induces the proliferation of dysfunctional immune cells and is likely to cause cancer [ 19 ], coronary heart disease [ 20 ], diabetes mellitus [ 21 ], and gastrointestinal disorders [ 18 , 22 ]. Second, fatigue may contribute to the development of cancer [ 16 ], coronary heart disease, diabetes mellitus, gastrointestinal disorders [ 23 ], and psychological stress [ 18 , 24 ]. Finally, CCNs report experiencing social isolation because shift work makes it difficult for them to participate in leisure-time activities or family time, which can lead to depression [ 25 , 26 ].
Furthermore, CCNs face quantitative work-related demands regarding high workload, time pressure, and workflow interruptions [ 10 , 27 ]. These demands impair CCNs’ mental focus and increase the likelihood of developing prolonged fatigue and stress [ 10 ]. In addition, CCNs need to deal with high levels of cognitive work-related demands, which can be defined as: “burdens placed on the brain processes involved in information processing” [ 28 , p.1574]. These cognitive work-related demands above the acceptable threshold contribute to attention narrowing, psychological stress, and burnout [ 29 , 30 , 31 ]. Moreover, CCNs are exposed to emotional work-related demands that require them to exert effort to deal with the desired emotional responses [ 28 ]. These demands involve workplace violence and end-of-life care issues and can cause anxiety, fatigue, and depression [ 12 , 32 ].
Given the number of studies having postulated the adverse health effects of work-related demands, there is an increasing need for developing mitigating strategies to guarantee extended healthy working lives [ 33 ]. From a theoretical perspective, the Job Demand-Control-Support model [ 34 ] hypothesises job control and workplace social support as psychosocial moderators to mitigate the strenuous impact of work-related demands on health [ 35 ]. In particular, job control refers to: “a working individual’s potential control over his task and his conduct during the working day” [ 36 , pp. 289–290]. It has been argued that job control can reduce the physiological impact of work-related demands on employees’ health by allowing them to take a break if necessary [ 35 ]. Likewise, workplace social support can be considered as interpersonal relationships at work to cope with stressful situations by putting them into another perspective, thereby leading to less psychological stress [ 37 ]. Additionally, the Effort-Reward Imbalance model [ 38 ] considers the prevention of adverse health outcomes by providing sufficient rewards in line with the performed efforts at work [ 39 ].
Numerous correlational studies are available which research the impact of work-related demands on nurses’ health [ 40 , 41 , 42 ]. To our knowledge, no qualitative studies have comprehensively investigated how exposure to multiple work-related demands influences CCNs’ health, or the complex social and psychological processes through which CCNs navigate these work-related demands across various CCN wards. However, it is essential to identify new factors in the research of CCNs’ work-related health and to create a policy that prevents health complaints and their associated costs.
The aims and design of the study
This qualitative study was based on Thorne’s interpretive descriptive approach [ 43 ] and was part of the Flemish Employees’ Physical Activity study [ 44 ]. Thorne’s interpretive descriptive approach embraces the concept that reality is shaped by social constructs, acknowledging the existence of diverse constructed realities [ 43 ]. Thus, this approach was appropriate to gain insight into the recalled experiences of CCNs in dealing with the physical and psychological influence of work-related demands on their health, while also examining the environments in which they operate [ 43 ]. In addition, this approach was well suited to explore the complex social and psychological processes through which CCNs navigate these work-related hazards across various CCN wards [ 43 ].
Setting and participants
This study was conducted in a local hospital in Flanders (Belgium) with a capacity of 1046 beds. First, 18 CCNs were recruited between October 2022 and January 2023 by means of convenience sampling to ensure a wide range of experiences by posting recruitment flyers in the CCNs’ lockers and placing posters in the CCN wards. Moreover, an invitation mail with informed consent was sent to the head nurses, who then delivered this mail to their CCNs. However, the CCNs could also participate by directly expressing their willingness to engage by email to the research team. Eligibility criteria required CCNs to be employed for more than 50% in the emergency department (ED), intensive care unit (ICU), stroke unit, or the critical care mobile nursing team and to be Dutch speaking. Nurses of the critical care mobile nursing team were employed simultaneously in the ED, ICU, and stroke unit. CCNs in management positions were not included due to their potential impact on the reporting of their subordinates’ experiences [ 45 ].
According to the insights that emerged after the intermediate analysis of the first four focus groups, nine CCNs were purposively selected between January 2023 and April 2023 via a snowball sampling technique to deepen the understanding of the discussed topics from earlier focus groups [ 46 ]. For example, CCNs reported the detrimental influence of prehospital physician-staffed emergency care interventions on their health. Therefore, CCNs with similar and diverse experiences in prehospital physician-staffed emergency care interventions were recruited.
Data collection
Data collection methods.
Thorne’s interpretive descriptive approach was applied by conducting focus groups, which refer to a guided discussion with several people to explore ideas and perceptions about a specific topic from a multiplicity of views [ 47 ]. Conducting focus groups has several benefits, such as stimulating group dynamics, revealing deeper expressions of genuine feelings and beliefs, and enabling the acquisition of rich information in a cost-effective manner. Furthermore, the multiplicity of views during focus groups is useful to deepen the understanding of the complex social and psychological processes through which CCNs navigate their work-related demands, as these views could generate new ideas and perspectives that yield unexpected insights into the recalled experiences.
The research team consisting of experts in occupational health (EC, MK, and LBo), emergency nursing (LBi), and qualitative research (LBo) developed a semi-structured focus group guide (Table 1 ). This guide sought to explore the recalled experiences of CCNs in dealing with the physical and psychological influence of their work-related demands on their health and to identify strategies in which CCNs could mitigate this influence. The focus group guide used a deductive approach because of the preliminary exploration of the Job Demand-Control-Support model [ 34 ], the Effort-Reward Imbalance model [ 38 ], and the Sixth European Working Conditions Survey (EWCS) [ 48 ]. However, the focus groups were conducted with an open mind to identify new topics and to stimulate further questions that could contribute to the in-depth understanding of the CCNs’ recalled experiences [ 43 ]. As a result, the focus group guide became more focused when the transcripts were coded and preliminary ideas of the research team emerged [ 49 ].
Data collection procedure
Between October 2022 and April 2023, six focus groups were held in a comfortable meeting room after lunchtime at the local hospital in Flanders (Belgium). Each focus group consisted of four to five CCNs from the same CCN ward and lasted uninterrupted for a maximum of 90 minutes, with an average duration of 68.75 minutes. The first 60 minutes were during working time, and the rest could be accounted as overtime. All focus groups were conducted by one master’s student in nursing science (LBi). The data collection process was supervised by an experienced qualitative researcher in occupational health (LBo) who provided feedback on the interview style. The master’s student was known superficially at the ED in the local hospital due to his previous nursing student work, which helped in understanding and contextualising the complexities and subtleties of the CCNs’ experiences. The interviewer wore clothes from the hospital to reduce the risk of interviewer bias. No observer was present during the focus groups. Because the participants were encouraged to share their experiences freely, the focus group guide was only implemented when the participants discussed topics irrelevant to this study, when a participant was too dominant, or when the discussion needed stimulation [ 45 ]. The interviewer sought to obtain input from all participating CCNs by asking open-ended and probing questions to introvert participants to elicit in-depth views. All focus groups were audiotaped with a smartphone and tablet.
Data analysis
The audiotapes were transcribed verbatim and deleted afterwards. The data analysis process was based on the Qualitative Analysis Guide of Leuven, which guaranteed a cyclic process between data collection and data analysis to propose a conceptual framework [ 50 ]. The Qualitative Analysis Guide of Leuven consists of two crucial phases, namely, the preparation of the coding process by paper and pencil work and the actual coding process by using qualitative software [ 50 ].
First, two members of the research team (LBi and LBo) read the transcripts several times to obtain an in-depth understanding of the intricate details [ 18 ]. Second, both researchers wrote down memos and then developed a narrative focus group report for each focus group [ 50 ]. Third, concepts were drawn up to replace tangible or concrete experiences, which allowed the development of a conceptual scheme for each focus group. During this process, the same two researchers discussed and cross-checked the identified analytical and contextual concepts and sought to obtain a detailed understanding of the data [ 50 ]. This constant comparison process through inductive and interpretative reasoning allowed a within-case and across-case analysis to compare new concepts with earlier coded data so that similarities and differences in data could be identified and analysed [ 51 , 52 , 53 ]. Subsequently, the concepts were linked to relevant focus group fragments by using the QSR NVivo 12 software program. During this phase, data were further coded by combining concepts into groups of concepts based on emerging ideas and comparable meanings. These groups of concepts resulted in certain categories and were then divided into subcategories and main categories. The main categories were tested in the existing literature and rooted in the practical and theoretical knowledge of the research team after several intermediate meetings. Finally, the main categories were outlined in a conceptual framework, which represented the essential structure of the results. Data saturation was reached when no new dimensions or relationships emerged during the analysis, which was confirmed by conducting an additional focus group [ 52 ].
Trustworthiness
The confirmability of the data was improved by applying different strategies. During the iterative process, the interview style and the questions arising from the focus group guide that could contribute to the in-depth understanding of the CCNs’ recalled experiences were peer-reviewed by the research team. Next, investigator triangulation was applied by two researchers with prior experience in the nursing profession (LBi and LBo) who analysed the transcripts independently and discussed the inductive code tree continuously. These transcripts and inductive code tree were then peer-reviewed by the entire research team at several intermediate meetings.
In addition, an audit trail with detailed information about the decisions made by the research team throughout the research process was documented to enhance the dependability and confirmability of the study [ 45 ]. This audit trail included descriptive interview notes, reflexive notes, methodological notes, and analytical notes. The development of reflexive notes was encouraged by sustaining transparent communication with the research team, which was stimulated because one research member was not familiar with occupational health, two research members were not a nurse, and one research member only had experience in the nursing profession in Switzerland [ 52 ]. Furthermore, the interviewer with experience in emergency nursing reflected on his personal values, opinions, and experiences, which cultivated awareness [ 43 ]. The audit trail also included a thick description of the setting, sample, and observations, supporting the transferability of the results. The Standards for Reporting Qualitative Research were implemented to enhance the quality of the reported data [ 54 ].
Participants
The sample consisted of 37 CCNs, of which 27 CCNs participated in one of the six focus groups and ten CCNs could not participate due to organisational difficulties. Of those 27 CCNs, six were male and 21 were female, with a mean age of 36.07 years. Most CCNs worked in the ED (55.55%), with 77.78% of all included CCNs working full-time. Further sociodemographic characteristics of the CCNs are shown in Table 2 .
The interrelated categories
During iterative development, the influence of work-related demands on the participants’ health and mitigating strategies were identified. While being employed at a CCN ward, participants were continuously exposed to OPA, emotional, cognitive, and quantitative work-related demands, adverse patient behaviour, and poor working time quality. Exposure to such work-related demands was perceived as harmful and could lead to physical, mental, and psychosomatic complaints and increased turnover intention. Participants sought to mitigate the influence of work-related demands on their health by relying upon social support, job control, work equipment, rewards, and leisure-time physical activity. The results are outlined in the conceptual framework (Fig. 1 ). The central hexagon symbolises the consequences on CCNs’ health by surrounding work-related demands. The outer circle illustrates the applied strategies to mitigate adverse health outcomes.
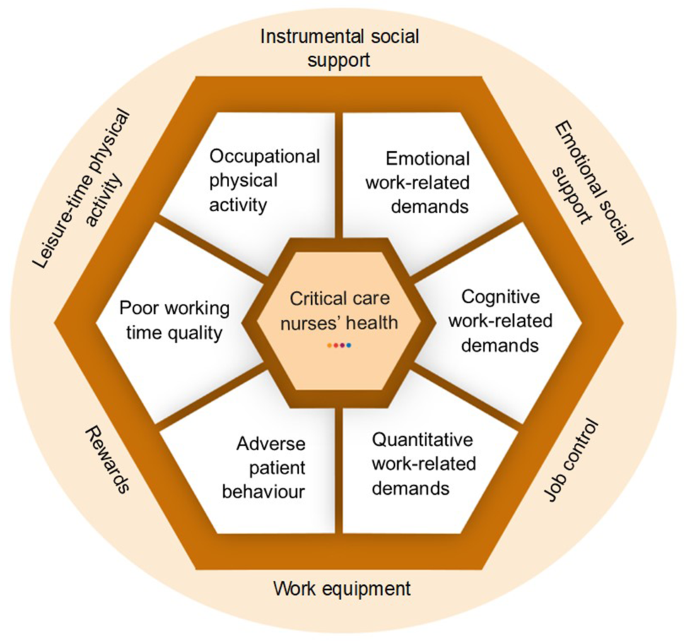
Conceptual framework inspired by the Job Demand-Control-Support model [ 34 ], Effort-Reward Imbalance model [ 38 ], and EWCS [ 48 ]
The structuring of the results was inspired by the Job Demand-Control-Support model [ 34 ], the Effort-Reward Imbalance model [ 38 ], and the EWCS [ 48 ], and supported with exemplar citations referring to the specific participants along with the focus groups they belonged to (FG-P) [ 46 ].
- Work-related demands
Participants experienced continuous exposure to OPA inside the hospital and during prehospital physician-staffed emergency care interventions. The included ED nurses were exposed to less OPA during the morning shift than ICU and stroke unit nurses. The most reported types of OPA were forward bending and isometric neck postures, prolonged standing, and long-distance walking. Forward bending and isometric neck postures were frequently required in various tasks performed, such as resuscitating, plastering, carrying heavy emergency coffers, tilling heavy patients in ambulance stretchers, and caring for intubated patients:
For example applying a plaster, holding up a leg with one arm and your back being curved, I have already had instances where the day after I thought: ‘I had to hold up a leg of 50 kilos which made my arm hurt the day after’. (FG3-P3)
Emotional work-related demands
Participants indicated the resuscitation of a child or family member, severe trauma victims, the announcement of cancer diagnosis to patients, and the high mortality rate as emotionally demanding:
I have seen things during the COVID that I never want to see again. I found that terrible… Yes (…), that feeling of powerlessness. You had to go through it. How many people died alone? I held their hands, but I stood there alone in my alien outfit. Then you have to call the family and tell them that you didn’t leave them alone. Those family members started to cry and I cried with them. I have apologised for that… I found that a very heavy period, those first two months of COVID. In addition, those older persons who arrived and said: ‘You do not have to give the oxygen to us, give it to the younger persons’, and after two hours they were dead. (FG4-P4)
In addition, the quality of management by supervisors was identified as a significant work-related demand among participants, as they reported feeling undervalued and unsupported, as well as experiencing a lack of empathy of their supervisors. Multiple CCNs claimed that the high number of telephone calls from their supervisors to provide shift coverage during off-job time contributed to this perceived poor management quality. FG1 and FG2 participants added that they felt the sense of being controlled by their supervisors via electronic patient records or checklists. The need for resilience, the changing work environment, and the lack of decision authority were further mentioned as significant demands in their role:
They ask for your opinion when it has already been determined. That is something that often happens to us. They already decided on something and then asked us for the show like: ‘How do you think about it?’, but our opinion does not matter anymore. (FG3-P3)
Furthermore, the adverse social behaviour from colleagues was cited as emotionally demanding by several participants. In particular, participating CCNs reported that interpersonal conflicts, such as working with nursing students, inexperienced colleagues or colleagues with whom the participants had a less good connection, contributed to an increased interdependency and the need to control the delivered care:
You have colleagues you get completely stressed out by… Yes, because the way of working is completely different, that you cannot relate to them, that you cannot do anything right for them, whereas you have other colleagues where you feel each other. (FG4-P1)
Finally, participants experienced a demand to perform without the ability to schedule a break and to be present at work during an illness because of their loyalty to colleagues:
Recently, a colleague arrived with a kidney stone. She sat in the kitchen with an infusion of analgesics and started to work an hour and a half later. (FG1-P4)
Cognitive work-related demands
Participants reported feeling highly vigilant throughout their shifts, especially when attending to unplanned care for critically ill patients. This required hypervigilance, combined with a lower presence of physicians, increasing their sense of responsibility. In addition, FG3 participants expressed being overwhelmed by the high amount of auditory stimulation they were exposed to:
In the ICU, I do have more stress because of the responsibility in comparison with the ED. In the ED, the emergency physicians will do many things by themselves, whereas in the ICU, I am expected to do it by myself. In the ICU, you also have a lot more critical patients than in the ED, because in the ED, sometimes you have a lot of geriatrics, but there is nothing critical about it. Whereas in the ICU, if you have an unstable patient, you have to think and reason continuously. Then, again, that is tougher, the psychological aspect. (FG4-2)
Quantitative work-related demands
Participants perceived the high work pace combined with telephone-related workflow interruptions, caused by managing the chaotic CCN ward and processing the high amount of medical orders, as harmful to their health. Furthermore, participating CCNs considered the need to carry out double work and inefficient work as significant demands in their role. As a consequence, multiple CCNs stated that more OPA was performed due to a lack of instrumental social support from colleagues:
Sometimes you feel like you are behind the times. You have to do this and that and that and that. You have continuously, you are faced with something that is not feasible of care as you have been taught. In practice, that is not feasible. This is then shifted on a maximum of pressure (…). (FG4-P3)
Adverse patient behaviour
Participants reported experiencing feelings of incongruence and dissatisfaction while providing care to self-referred non-urgent, dissatisfied, disrespectful, or aggressive patients:
I sometimes feel unsafe, yes. Especially in the ED, very unsafe… Yes, I am roused and stressed. I put it away. I do not show it externally because I do not want the patient to realise this. Internally, this is something that eats you up. I feel I am tachycardic then. (FG4-P2)
Poor working time quality
Participants highlighted the atypical working times as demanding due to working full-time in rotating shifts, on holidays, and during weekends:
Those mixed evening shifts, morning shifts, night shifts, and day shifts… Yes, I stopped working full-time here because I could no longer cope with it. (FG4-P3)
Furthermore, the highly commanded flexibility and poor working time arrangements were mentioned as significant work-related demands due to keeping up with all the refresher courses during off-job time, assisting in other nursing wards, dealing with unpredictable work schedules, and providing shift coverage when colleagues call in sick:
I got a call an hour later from my nursing supervisor asking if I could work another night shift. However, I said: ‘It is my non-working weekend and again it is during my non-working weekend that I have to do a night shift’. Again, I was justifying myself and I thought: ‘Why am I doing that?’. They know my weaknesses and you gave in to one [supervisor], but the other one [supervisor] is also trying because maybe you will also give in to him. (FG5-P1)
Consequences of work-related demands
Physical complaints.
Participants reported experiencing musculoskeletal disorders, particularly after increased exposure to OPA during busy shifts. Multiple CCNs mentioned the most intense pain in the lower and upper back, neck, shoulders, knees, hips, or bilateral wrists. FG2 and FG3 participants also experienced inflammation in their feet, lateral epicondylitis, and restless legs at a young age:
I have never, in the beginning, I did not suffer so much from that, but recently, I started having such restless legs from time to time <<< laughs>>>. In addition, then I think: ‘Oh so embarrassing because you are only 25 or 26 years old’. (FG3-P4)
However, several participants suggested that they had developed musculoskeletal disorders more easily due to OPA compared to leisure-time physical activity. This distinction was attributed to the fact that OPA involves prolonged exposure to less intense physical activity and leisure-time physical activity involves shorter exposure to more intense physical activity:
The physical work is more chronic (…), walking (…), or your arms or your back being strained… Whereas when you exercise that is very intense (…), your arms or your legs that you are training. (FG2-P3)
Furthermore, FG4 participants experienced an increased risk of developing urinary disorders in terms of urinary tract infections and kidney stones. This increased risk was attributed to the lack of opportunities to drink while working and unhealthy toileting behaviours, such as delayed voiding while facing a high work pace. Moreover, participants stated that their rotating shift work and atypical working times led to irregular and unhealthy eating patterns, resulting in unintentional weight gain:
I eat chips with a mandarin and a sandwich with chocolate, and minced meat. (FG3-P4)
Last, participants reported that they had developed impaired sleep quantity in terms of insomnia, shortened or prolonged sleep duration, and increased sleep disturbances, which were probably caused by circadian rhythm disruption due to shift work:
Yeah, especially if I had to switch from night to day rhythm. I was nauseous, intolerant, restless, rushed, unable to sleep, lying awake, not finding rest, being hungry when not being hungry. (FG4-P3) .
Mental complaints
Participants mentioned experiencing challenges in detaching mentally from patient-related stressful situations, particularly when children or family members were involved. Further difficulties in detaching from work were attributed to the high number of consecutive working days, the changing work environment, the challenging weekend schedule/shift, and the considerable level of flexibility required of CCNs. Participating CCNs expressed that this lack of detachment contributed to their impaired sleep health, emotional exhaustion, concentration disorders, work-family interference, and alcohol consumption:
I often need something like alcohol to just, truly, detach for a while <<< sighs>>>. My partner shares in the blows, but you are so overwhelmed at work and you come home with nine emails, a message from that one and a message from that one. On your day off again those emails, again those telephone calls, again… (FG5-P2)
In addition, participants reported that they experienced work-related stress and more intense perceptions of OPA due to poor management quality, adverse social behaviour from colleagues, and working with nursing students. Multiple CCNs added that the refresher courses during off-job time, adverse patient behaviour, and the reported shortcomings in providing the best possible care to patients contributed to their perceived work-related stress, likely resulting in personal dissatisfaction, moral distress, carry over into their personal lives, and increased turnover intention:
That satisfaction is completely overshadowed by the workload and the unsafe atmosphere at the ED. A stroke patient is located in the hallway and a person with epilepsy is located in the hallway, I am not satisfied when I come home. I just think: ‘No one died because of me in my care zone’. (FG5-P2)
Furthermore, participants tended to experience feelings of agitation during exclusion from the multidisciplinary decision-making processes and due to the lack of social support from physicians and the confrontation with dissatisfied patients:
We also do not understand why nurses were never involved in the development of patient rooms. I was part of the project group and when I measured everything and said it would not work for that, I got the reply: ‘Sorry, but it is too late, the rooms are already made and you cannot change that anymore’. (FG6-P4)
In addition, participants perceived emotional exhaustion, which could lead to personality changes and reduced marital and life satisfaction:
I do not know what all of you think about that, but everyone is sad at work. I feel that about myself too. (FG6-P2)
Moreover, participants reported experiencing work-family interference and attributed this to the considerable level of flexibility required, the nature of shift work, and the presence of patient-related stressors. Because of this continuous interference, the included CCNs were not able to take care of their children, perform tasks at home, and spend time with family. This work-family interference caused work-related stress, emotional exhaustion, concentration disorders, impaired marital satisfaction, and a reduced perceived work ability among participants:
So I also stopped working night shifts because of the work-life imbalance. From the moment I had my third child, I said: ‘This is no longer possible’. This caused tension in all possible areas, and then you have to make a choice and say that your private life comes first. It is almost not feasible to work full-time at the pace we work and in the circumstances we work. It is almost not feasible. (FG3-P1)
Finally, participants expressed being subject to social isolation as a result of their demanded flexibility, shift work, and unpredictable work schedules:
Yes, for example, I can no longer take dance classes because it is at a particular hour, and due to irregular shifts, I cannot guarantee that I can follow the class every week. So yes, too bad, but I cannot do my hobby anymore that I love to do. (FG3-P2)
Psychosomatic complaints
Participants stated that the experienced emotional exhaustion and work-related stress led to unintentional weight loss, increased muscle tension, and migraine:
I notice from myself that due to the emotional burden at work, I am starting to have physical complaints. For example, migraine, um yes, always being so tired, extremely losing weight, not being able to gain weight. (FG5-P1)
Moreover, multiple participants expressed the physical effort of OPA and leisure-time physical activity as comparable, but the lack of decision authority and satisfaction that comes with OPA increased their risk of developing prolonged fatigue and emotional exhaustion, contributing to physical exhaustion:
I can spend a whole day in my garden doing heavy work, then I come in [inside home] and I feel so energetic, fulfilled, and relaxed. However, when I come home from work, I feel so empty and drained of energy… The mindset here is already different. It [gardening] is also not an obligation. The work in the ED is an obligation… I can also feel that [physical activity during gardening] in my back and muscles, but still, I am not tired. (FG4-P3)
Furthermore, repetitive exposure to work-related stress was seen by the participants as a main factor in developing heart palpitations and tachycardia:
The moment I had tachycardia at triage due to enormous stress, no one cared from the physicians, except my two colleagues who then did take care of me. (FG5-P1)
Additionally, participants experienced reduced sleep quality, which was attributed to work-related stress, emotional exhaustion, and lack of detachment. In particular, the participating CCNs faced excessive daytime sleepiness and nightmares:
I went for a blood draw last week because my girlfriend said: ‘You should go for a blood draw because you are always tired, you always sleep around the clock and you would take another afternoon nap’. However, yes, everything was normal so the cause is probably my work. (FG5-P2)
Last, participants reported that they had developed concentration disorders likely caused by work-related stress, prolonged fatigue, emotional exhaustion, and lack of detachment, increasing their risk of traffic accidents:
I also nearly drove through a red light once. I had three to four prehospital physician-staffed emergency care interventions during one night and I was thinking of (…), anyways, I had to hit my brakes suddenly. (FG1-P1)
Turnover intention
Participants stated that they tended to leave their CCN ward due to the high work pace, unsafe working conditions, work-family interference, and lack of social support from their supervisors:
I have been in it [CCN profession] for more than 20 years now and I always said: ‘If it works out, I will stay in it until my retirement’… That you can stay employed until your retirement, I do not think that is possible anymore because of the current workload. (FG5-P5)
Mitigating strategies
Social support.
Participants reported instrumental social support from colleagues as a strategy to prevent the physical burden when dealing with OPA and to alleviate cognitive overload when coordinating a chaotic CCN ward:
If I know it is a severely affected patient or someone who is somewhat corpulent and obese, I usually do go and ask the colleague: ‘Do you want to help me with turning this patient so I can wash his back?’. (FG2-P4)
Moreover, the included CCNs indicated that emotional social support from supervisors and colleagues reduced their work-related stress by putting work-related demands into another perspective. As a result, participants carried less emotional and cognitive work-related demands over into their personal life, improving their mental well-being and marital satisfaction. Multiple CCNs added that ventilating to a self-employed psychologist or a family member who also works in healthcare helped them prevent emotional exhaustion and burnout:
Listening, giving advice, helping you, cheering you up, coming to help you unasked (…). Just asking if they can do something, for instance. Often they cannot do anything, but just the question they ask does wonders. (FG4-P1)
Job control
Participants emphasised a high amount of skill discretion due to accommodative access to refresher courses, which contributed to their sense of safety and resulted in less work-related stress and more job satisfaction. Concerning decision authority, multiple CCNs considered the perceived amount of control to schedule their holidays and take up overtime as an important motivator to cope with work-related demands. Additionally, participants stated that the authority to schedule a break at work was needed to recover mentally and physically during periods of high work pace:
It feels good if you can recuperate for once. If you now say like, for example, in certain night shifts, you have finished your patient care, and at midnight or 1 AM, you say: ‘Come, let us drink a coffee’. That you can <<< blows out>>>. This is just for 15 minutes because you still have to do… (FG1-P5)
Work equipment
Participants expressed that work equipment to transfer patients, such as the HoverMatt®, sliding sails, and patient lifts, alleviated the physical burden of OPA. Nevertheless, several CCNs reported shortcomings in ergonomic work equipment to address OPA during prehospital physician-staffed emergency care interventions. In addition to these shortcomings, work equipment to transfer patients was not used to its full potential while facing a high work pace. Furthermore, participants disclosed that adjustable hospital stretchers, ergonomic shoes, and chairs with adaptability for taking blood samples were beneficial in preventing physical complaints. Participants in FG1 and FG3 added the benefits of compression stockings, analgesics, and magnesium to avoid restless legs:
And especially if you work night shifts, the restless legs that you have when you get into your bed. Now, I no longer have that <<< looks at compression stockings>>>. (FG1-P4)
Participants perceived the patients’ gratitude, wages, job security, equal social benefits, career prospects, and off-job time as helpful to cope with the required efforts at work:
That you have been able to do your job the way you want and if you build up a good relationship with your patient who you feel you have been able to help him both physically and mentally through the difficult period, then this does give you satisfaction, uhm. (FG2-P3)
Leisure-time physical activity
Participants indicated leisure-time physical activity as a strategy to detach mentally from work:
I exercise every day and that just helps me more, I am more relaxed compared to when I do not exercise. (FG1-P2)
Participants were exposed to OPA, emotional, cognitive, and quantitative work-related demands, adverse patient behaviour, and poor working time quality. In response to these work-related demands, participants employed various strategies for mitigation, including seeking social support, exerting control over their work, utilising appropriate equipment, recognising rewards, and engaging in leisure-time physical activity. Throughout the following discussion, the results were compared with traditional quantitative frameworks used in research on psychologically healthy work to investigate if these frameworks still comprise all essential factors influencing CCNs’ work-related health.
A key finding of this study was the continuous exposure to a high amount of OPA. However, contrary to Aleid et al. [ 55 ], this study sample identified differences in exposure to OPA between the different participating CCN occupations. This result could be attributed to two organisational factors of the local hospital. First, the hospital’s patient occupancy rate is normally lower during the morning at the ED compared to the ICU and stroke unit. Second, the participating ICU and stroke unit nurses had their work equipment to deal with OPA more closely available in the patient room, while ED nurses did not [ 9 ]. In contrast to Clays et al. [ 56 ], however, this study also emphasised the psychosocial work environment as an influencer of exposure to OPA. This result could be explained by the participating CCNs experiencing adverse social behaviour from colleagues with whom they had a less good connection, resulting in them receiving less instrumental social support and having to perform more OPA alone. Another possible explanation could be that these CCNs were subject to more OPA due to the lack of authority to question medical orders given by physicians. This may be attributed to the experienced patriarchal physician-nurse relationship and the financial incentive of diagnostic tests for physicians due to the fee-for-service payment system in Belgium. Because of the exposure to OPA, the CCNs in this study reported experiencing musculoskeletal disorders, which corroborates the results of previous studies among CCNs [ 1 , 57 ]. Despite several risk management strategies across the nursing profession to reduce the risk of developing musculoskeletal disorders, exposure to side-bending postures during prehospital physician-staffed emergency care interventions is not decreasing [ 58 , 59 ]. From a theoretical perspective, OPA is widely covered by the physical job demands subscale of the Job Demand-Control-Support model [ 34 ], the effort subscale of the Effort-Reward Imbalance model [ 38 ], and the physical environment index of the EWCS [ 48 ].
Exposure to emotional work-related demands related to exclusion from multidisciplinary decision-making processes and providing inappropriate care to patients and their relatives resulted among the participants in moral distress and emotional exhaustion. Consistent with Azoulay et al. [ 40 ], this mental burden can be considered an important factor in developing burnout. As a consequence, participants tended to experience unintentional weight loss, migraines, personality changes, job dissatisfaction, and increased turnover intention. Concerning personality changes, previous research has noted that 38.6% of South Korean ICU nurses were characterised by a Type D personality in terms of anxiety, depression, and inappropriate worrying [ 60 ]. However, CCNs in this study also experienced less empathy towards their patients, and remarkably less empathy towards their partners and friends. Despite the major influence of emotional work-related demands on CCN’s health, these demands are solely covered by the EWCS [ 48 ].
Our results indicate that exposure to cognitive work-related demands during employment at a CCN ward is essential to consider when evaluating CCNs’ health. Previous research has indicated that the continuous solving of unforeseen problems can contribute to self-development at work [ 48 ]. However, consistent with Bolliger et al. [ 46 ], the included CCNs perceived this continuous problem-solving as stress-inducing. An increasing amount of evidence suggests that the required cognitive hypervigilance of CCNs can increase the risk of concentration disorders and may lead to medical errors [ 10 , 11 ]. This increased risk of medical errors was not demonstrated by this study, which could be due to socially desirable answers during the focus groups. Cognitive work-related demands are part of the effort subscale of the Effort-Reward Imbalance model [ 38 ] and the skills and discretion index of the EWCS [ 48 ].
Participants underscored that exposure to quantitative work-related demands in terms of high work pace, workflow interruptions, and inefficient work reduced their attention and sleep health due to work-related stress, which is well supported by evidence [ 10 ]. Multiple participating CCNs experienced reduced subjective sleep quality, disrupted sleep duration, and increased sleep disturbances, which were associated with an increased risk of traffic accidents, and are in line with Smyth’s [ 61 ] Pittsburgh Sleep Quality Index. According to the theoretical models, quantitative work-related demands are covered by the demands subscale of the Job Demand-Control-Support model [ 34 ], the effort subscale of the Effort-Reward Imbalance model [ 38 ], and the work intensity index of the EWCS [ 48 ].
Consideration is required concerning the influence of working time quality on CCNs’ health. Regarding the working time quality index of the EWCS [ 48 ], the combination of atypical working times and family role demands was perceived by participants as detrimental to their health and marital life. A possible explanation for this might be that most participating CCNs were aged between 25 and 35 years, which is seen as the most interesting period for career development, marriage, and raising children [ 31 , 62 , 63 ]. Furthermore, in line with the EWCS [ 48 ], participants who were informed at short notice of adaptations in their work schedule tended to experience a lack of detachment, work-family interference, and social isolation. However, previous research has shown that male workers are more likely to develop low back pain due to work-related demands when they experience work-family interference [ 64 ]. Given these results, nursing supervisors should give more consideration to the risk factors for work-family interference in risk management strategies to prevent the development of musculoskeletal disorders. The dimensions of the working time quality index are not considered by the Job Demand-Control-Support model [ 34 ] or by the Effort-Reward Imbalance model [ 38 ].
This study identified workplace social support as a psychosocial moderator of the development of emotional exhaustion due to stress-inducing work-related demands. In line with Sampei et al. [ 65 ], participants reported that they had developed emotional exhaustion when they faced high exposure to work-related demands with low levels of social support. In contrast to Clays et al. [ 35 ], however, no evidence of the buffering potential of social support on the development of coronary heart diseases due to OPA was detected. From a theoretical perspective, workplace social support is widely mentioned in the Job Demand-Control-Support model [ 34 ], the Effort-Reward Imbalance model [ 38 ], and the EWCS [ 48 ].
Concerning skill discretion, access to training opportunities among the European workforce improved by 12% in 2015 compared to 2005 [ 48 ]. This finding is consistent with this study, in which accommodative access to refresher courses contributed to the participants’ sense of safety at work. However, the amount of flexibility required to be present in the refresher courses during off-job time was likely to induce work-related stress and work-family interference. Regarding decision authority, participants experienced exclusion from multidisciplinary decision-making processes and had fewer opportunities to schedule a break at work. This result is consistent with the EWCS [ 48 ] stating that only a scarce 33% of European subordinates were involved by their supervisors in decision-making processes influencing their work [ 46 ]. Surprisingly, the Job Demand-Control-Support model [ 34 ] was found to measure job control solely on positively perceived decision authority [ 46 ].
The included CCNs expressed the mitigating influence of wages, career prospects, and job security in regard to coping with work-related demands. According to the earnings index of the EWCS [ 48 ], 39% of the European workforce agreed that their employment offers prospects that are beneficial for career advancement. This is in line with this study, in which participants perceived that being employed at a CCN ward contributed to their professional development. From a theoretical perspective, the Effort-Reward Imbalance model [ 38 ] includes the rewards subscale in terms of money, esteem, and security/career opportunities.
In light of the discussed theoretical models, some show additional shortcomings. Although the participants’ health was influenced by patient-related stressful situations, poor management quality, and the experienced demand to perform, these emotional work-related demands are not considered by the Job Demand-Control-Support model [ 34 ] or by the Effort-Reward Imbalance model [ 38 ]. In addition, the Job Demand-Control-Support model [ 34 ] does not pay attention to the work-family interference concept caused by the considerable level of required flexibility, the nature of shift work, and the presence of patient-related stressors. However, the Effort-Reward Imbalance model partially conceptualises work-family interference as overcommitment [ 46 , 48 ]. Finally, the Job Demand-Control-Support model [ 34 ] does not include the rewards subscale in terms of patients’ gratitude, wages, job security, equal social perks, career prospects, or off-job time. Thus, solely the EWCS [ 48 ] covers a wide range of work-related demands that are perceived as harmful according to this study sample.
Limitations
The inclusion of only one hospital may have provoked selection bias and might hinder the transferability of the results to other CCNs employed in similar work environments. Furthermore, the scheduled focus groups with the ICU nurses were frequently cancelled at short notice due to seasonal epidemics and changing work schedules. In addition, the stroke unit’s nursing team is characterised by a limited number of nurses, and therefore, it was only possible to organise one focus group. As a consequence, the subgroup of ICU and stroke unit nurses was small, and data saturation concerning sampling remains debatable. Another limitation is the possible occurrence of healthy worker effect bias [ 66 ], as nurses on sick leave may have felt impeded from participating. During each focus group, essential observations could have been missed due to the absence of an observer. Additionally, interviewer bias may have occurred due to the moderator’s pre-existing superficial relationship with the ED nurses. However, the research team is convinced that the CCNs employed in the local hospital were not hampered from engaging and that this relationship stimulated them to share their deep-rooted feelings and perceptions.
Implications for practice
The results of this study include several recommendations for practice, structured by the developed conceptual framework. In particular, the identified and assessed physical and psychosocial risk factors can be integrated into the current risk management strategies. This is crucial as existing risk management strategies often overlook the consideration of multiple risk factors. Concerning OPA, more ergonomic emergency coffers could be provided to prevent side-bending postures during prehospital physician-staffed emergency care interventions. To tackle emotional work-related demands, nursing supervisors should provide vertical trust, job security, transparent communication, decision authority, and social support to their employees, thereby mitigating the perceived influence of work-related demands [ 46 ]. Addressing job security, the meta-analysis of Kim and von dem Knesebeck [ 67 ] demonstrated that employees without job security had 29% more risk of developing depressive symptoms compared to employees with job security. Moreover, Mazzetti et al. [ 68 ] underscored the need for organisations to provide a leadership programme in which supervisors learn appropriate coaching strategies, enhancing proximal factors such as job satisfaction and commitment. In reference to cognitive and quantitative work-related demands, greater efforts are needed to ensure a sufficient and uninterrupted recovery time between shifts, to provide breaks without interruptions and to reduce the demand to perform [ 69 ]. With respect to adverse patient behaviour, the risk of mental complaints and work-related stress can be reduced by assigning a psychologist who educates CCNs on how to cope with patient-related stressful situations. Furthermore, nursing supervisors can improve poor working time quality by implementing forward and rapidly rotating work schedules to impede the development of circadian rhythm disruption [ 25 ]. In addition, schedule flexibility should be guaranteed by introducing the principles of self-scheduling to provide more control over working time, prevent work-family interference, and reduce the risk of circadian rhythm disruption [ 25 ].

Implications for research
Considerably more work will need to be done to determine the long-term moderating effects of psychosocial job resources by implementing longitudinal research designs. Additionally, further studies need to be carried out to establish the modernisation of traditional quantitative frameworks used in research on psychologically healthy work, in which they explore the role of psychosocial and organisational factors in more detail. Concerning the modernisation of these frameworks, the influence of individual work-related demands on CCNs’ health is well-known according to recent evidence. However, research on the influence of multiple intertwined work-related demands on the health of CCNs remains scarce. As increasing research employs latent profile analyses, the interdependence of job factors becomes evident. Therefore, future research should investigate how multiple work-related demands interact or manifest in certain combinations on CCNs’ health.
This qualitative study identified that the participants’ health was challenged by work-related demands that are not entirely covered by the traditional quantitative frameworks used in research on psychologically healthy work. In particular, CCNs included in this study were exposed to OPA, emotional, cognitive, and quantitative work-related demands, adverse patient behaviour, and poor working time quality. In response to these demands, these CCNs employed various strategies for mitigation, including seeking social support, exerting control over their work, utilising appropriate equipment, recognising rewards, and engaging in leisure-time physical activity. Therefore, future studies should explore the role of psychosocial and organisational factors in more detail. In conclusion, this study recommends the development of an employee-centric work environment by providing sufficient risk management strategies, schedule flexibility, uninterrupted off-job recovery time, and positive management to guarantee extended healthy working lives among the CCN workforce.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
Critical Care Nurses
European Working Conditions Surveys
Emergency Department
Intensive Care Unit
Occupational Physical Activity
Qualitative Analysis Guide of Leuven
Bazazan A, Dianat I, Bahrampour S, Talebian A, Zandi H, Sharafkhaneh A, Maleki-Ghahfarokhi A. Association of Musculoskeletal Disorders and workload with work schedule and job satisfaction among emergency nurses. Int Emerg Nurs. 2019;44:8–13. https://doi.org/10.1016/j.ienj.2019.02.004 .
Article PubMed Google Scholar
Wu Y, Xuan Z, Yanhong G, Nan J, Mengge T, Jiali Z, Xiaoxv Y, Chuanzhu L. Work-family conflict of emergency nurses and its related factors: a National Cross-sectional Survey in China. Front Public Health. 2021;9. https://doi.org/10.3389/fpubh.2021.736625 .
Briggs AM, Woolf AD, Dreinhöfer K, Homb N, Damian GH, Kopansky-Giles D, Åkesson K, March L. Reducing the global burden of musculoskeletal conditions. Bull World Health Organ. 2018;96(5):366–68. https://doi.org/10.2471/blt.17.204891 .
Article PubMed PubMed Central Google Scholar
Liebermann SC, Müller A, Weigl M, Wegge J. Antecedents of the expectation of remaining in nursing until Retirement Age. J Adv Nurs. 2015;71(7):1624–38. https://doi.org/10.1111/jan.12634 .
Bell L. The ageing of the nursing workforce: what lies ahead and what we can do. Int Nurs Rev. 2013;60(3):277–78. https://doi.org/10.1111/inr.12049 .
De Vries N, Boone A, Godderis L, Bouman J, Szemik S, Matranga D, de Winter P. The race to Retain Healthcare Workers: a systematic review on factors that Impact Retention of nurses and Physicians in hospitals. Inquiry. 2023;60. https://doi.org/10.1177/00469580231159318 .
Flinkman M, Leino-Kilpi H, Salanterä S. Nurses’ intention to leave the Profession: integrative review. J Adv Nurs. 2010;66(7):1422–34. https://doi.org/10.1111/j.1365-2648.2010.05322.x .
Western Governors University. Critical Care Nurse Career Guide. https://www.wgu.edu/career-guide/healthcare/critical-care-nurse-career.html#close (2023). Accessed 20 Feb 2023.
Yu F, Narayanan A, Mackay L, Ward K, King A, Smith M. Describing objectively measured Intensive Care nurses’ physical work activity behavioural patterns during a 12-hr shift. J Clin Nurs. 2020;29(21–22):4331–42. https://doi.org/10.1111/jocn.15470 .
Weigl M, Beck J, Wehler M, Schneider A. Workflow interruptions and stress atwork: a mixed-methods study among Physicians and nurses of a Multidisciplinary Emergency Department. BMJ Open. 2017;7(12). https://doi.org/10.1136/bmjopen-2017-019074 .
Weaver AL, Stutzman SE, Supnet C, Olson DM. Sleep quality, but not quantity, is Associated with Self-Perceived Minor Error Rates among Emergency Department nurses. Int Emerg Nurs. 2016;25:48–52. https://doi.org/10.1016/j.ienj.2015.08.003 .
An Y, Yang Y, Wang A, Li Y, Zhang Q, Cheung T, Ungvari GS, Qin M, An F, Xiang Y. Prevalence of Depression and its impact on quality of life among Frontline nurses in Emergency Departments during the COVID-19 outbreak. J Affect Disord. 2020;276:312–15. https://doi.org/10.1016/j.jad.2020.06.047 .
Article CAS PubMed PubMed Central Google Scholar
Merkus SL, Coenen P, Forsman M, Knardahl S, Veiersted KB, Mathiassen SE. An exploratory study on the physical activity Health Paradox—Musculoskeletal Pain and Cardiovascular load during work and leisure in construction and Healthcare Workers. Int J Environ Res Public Health. 2022;19(5):2751. https://doi.org/10.3390/ijerph19052751 .
Holtermann A, Krause N, Van Der Beek AJ, Straker L. The Physical Activity Paradox: six reasons why Occupational Physical activity (OPA) does not Confer the Cardiovascular Health benefits that leisure time physical activity does. Br J Sports Med. 2017;52(3):149–50. https://doi.org/10.1136/bjsports-2017-097965 .
Johansson MS, Holtermann A, Marott JL, Prescott E, Schnohr P, Korshøj M, Søgaard K. The physical activity Health Paradox and Risk factors for Cardiovascular Disease: a Cross-sectional Compositional Data Analysis in the Copenhagen City Heart Study. PLoS ONE. 2022;17(4). https://doi.org/10.1371/journal.pone.0267427 .
Bolino MC, Kelemen TK, Matthews SH. Working 9-to‐5? A review of Research on Nonstandard Work schedules. J Organizational Behav. 2020;42(2):188–211. https://doi.org/10.1002/job.2440 .
Article Google Scholar
Moreno CRC, Marqueze EC, Sargent C, Wright KP Jr, Ferguson SA, Tucker P. Working Time Society Consensus statements: evidence-based effects of Shift Work on Physical and Mental Health. Ind Health. 2019;57(2):139–57. https://doi.org/10.2486/indhealth.sw-1 .
Suleiman AO, Decker RE, Garza JL, Laguerre RA, Alicia GD, Jennifer MC. Worker perspectives on the impact of Non-standard workdays on Worker and Family Well-Being: a qualitative study. BMC Public Health. 2021;21(1). https://doi.org/10.1186/s12889-021-12265-8 .
Yong M, Blettner M, Emrich K, Nasterlack M, Oberlinner C, Hammer GP. A retrospective cohort study of Shift Work and Risk of Incident Cancer among German Male Chemical workers. Scand J Work Environ Health. 2014;40(5):502–10. https://doi.org/10.5271/sjweh.3438 .
Chellappa SL, Vujovic N, Williams JS, Scheer FAJL. Impact of circadian disruption on Cardiovascular function and disease. Trends Endocrinol Metabolism. 2019;30(10):767–79. https://doi.org/10.1016/j.tem.2019.07.008 .
Article CAS Google Scholar
Shan Z, Li Y, Zong G, Guo Y, Li J, Manson JE, Hu FB, Willett WC, Schernhammer ES, Bhupathiraju SN. Rotating Night Shift Work and Adherence to Unhealthy Lifestyle in Predicting Risk of type 2 diabetes: results from two large US cohorts of female nurses. BMJ. 2018;k4641. https://doi.org/10.1136/bmj.k4641 .
Pryce C, Impact of Shift Work on Critical Care Nurses. Can J Crit care Nurs. 2016;27(4):17–21. https://pubmed.ncbi.nlm.nih.gov/29786977 .
PubMed Google Scholar
Letvak S, Ruhm C, Lane S. The impact of nurses’ Health on Productivity and Quality of Care. J Nurs Adm. 2011;41(4):162–67. https://doi.org/10.1097/nna.0b013e3182118516 .
Drake DA, Luna M, Georges JM, Steege LMB. Hospital Nurse Force Theory. Adv Nurs Sci. 2012;35(4):305–14. https://doi.org/10.1097/ans.0b013e318271d104 .
Jensen HI, Larsen JW, Thomsen TD. The impact of Shift Work on Intensive Care nurses’ lives outside work: a cross-sectional study. J Clin Nurs. 2017;27:3–4. https://doi.org/10.1111/jocn.14197 .
Kalmbach DA, Pillai V, Cheng P, Arnedt JT, Drake CL. Shift work disorder, Depression, and anxiety in the transition to rotating shifts: the role of Sleep Reactivity. Sleep Med. 2015;16(12):1532–38. https://doi.org/10.1016/j.sleep.2015.09.007 .
Sonnentag S, Binnewies C, Mojza EJ. Staying well and engaged when demands Are High: the role of psychological detachment. J Appl Psychol. 2010;95(5):965–76. https://doi.org/10.1037/a0020032 .
Gevers J, van Erven P, de Jonge J, Maas M, de Jong J. Effect of Acute and Chronic Job demands on effective individual teamwork Behaviour in Medical emergencies. J Adv Nurs. 2010;66(7):1573–83. https://doi.org/10.1111/j.1365-2648.2010.05314.x .
Liu S, Duan X, Han P, Shao H, Jiang J, Zeng L. Occupational Benefit Perception of Acute and critical care nurses: a qualitative Meta-synthesis. Front Public Health. 2022. https://doi.org/10.3389/fpubh.2022.976146 .
Schooley B, Hikmet N, Tarcan M, Yorgancioglu G. Comparing burnout across Emergency Physicians, nurses, technicians, and Health Information technicians Working for the same Organization. Medicine. 2016;95(10). https://doi.org/10.1097/md.0000000000002856 .
Wu H, Sun W, Lie W. Factors Associated with Occupational stress among Chinese female emergency nurses. Emerg Med J. 2011;29(7):554–58. https://doi.org/10.1136/emj.2010.094391 .
Bardhan R, Heaton K, Davis M, Chen P, Dickinson DA, Lungu CT. A Cross Sectional Study evaluating psychosocial job stress and health risk in Emergency Department nurses. Int J Environ Res Public Health. 2019;16(18):3243. https://doi.org/10.3390/ijerph16183243 .
Ketels M, Belligh T, De Bacquer D, Clays E. Are Psychosocial resources buffering the relation between physical work behaviors and need for recovery? Int J Public Health. 2022;67. https://doi.org/10.3389/ijph.2022.1604787 .
Karasek R, Theorell T, Healthy Work. Stress, Productivity, and the Reconstruction of Working Life. Choice Reviews Online. 1990;28(01):28–0381. https://doi.org/10.5860/choice.28-0381 .
Clays E, Casini A, Van Herck K, De Bacquer D, Kittel F, De Backer G, Holtermann A. Do psychosocial Job resources buffer the relation between physical work demands and Coronary Heart Disease? A prospective study among men. Int Arch Occup Environ Health. 2016;89(8):1299–307. https://doi.org/10.1007/s00420-016-1165-z .
Karasek R, Job Demands. Job decision latitude, and Mental strain: implications for job redesign. Adm Sci Q. 1979;24(2):285. https://doi.org/10.2307/2392498 .
Hornstein EA, Eisenberger NI. Unpacking the Buffering Effect of Social Support figures: Social Support attenuates Fear Acquisition. PLoS ONE. 2017;12(5). https://doi.org/10.1371/journal.pone.0175891 .
Siegrist J. Adverse Health effects of High-Effort/Low-Reward conditions. J Occup Health Psychol. 1996;1(1):27–41. https://doi.org/10.1037/1076-8998.1.1.27 .
Article CAS PubMed Google Scholar
Tian M, Yang H, Yin X, Wu Y, Zhang G, Lv C, Mu K, Gong Y. Evaluating effort-reward imbalance among nurses in Emergency departments: a cross-sectional study in China. BMC 2021; Psychiatry 21 (1). https://doi.org/10.1186/s12888-021-03344-6 .
Azoulay E, De Waele J, Ferrer R, Staudinger T, Borkowska M, Póvoa P, Iliopoulou K. Symptoms of Burnout in Intensive Care Unit specialists facing the COVID-19 outbreak. Ann Intensiv Care. 2020;10(1). https://doi.org/10.1186/s13613-020-00722-3 .
Bernal D, Campos-Serna J, Tobias A, Vargas-Prada S, Benavides FG, Serra C. Work-related psychosocial risk factors and Musculoskeletal disorders in Hospital nurses and nursing aides: a systematic review and Meta-analysis. Int J Nurs Stud. 2015;52(2):635–48. https://doi.org/10.1016/j.ijnurstu.2014.11.003 .
Zare A, Choobineh A, Hassanipour S, Malakoutikhah M. Investigation of psychosocial factors on Upper Limb Musculoskeletal disorders and the prevalence of its Musculoskeletal disorders among nurses: a systematic review and Meta-analysis. Int Arch Occup Environ Health. 2021;94(5):1113–36. https://doi.org/10.1007/s00420-021-01654-6 .
Burdine JT, Thorne S, Sandhu G. Interpretative description: a flexible qualitative methodology for medical education research. Med Educ. 2021;55:336–43. https://doi.org/10.1111/medu.14380 .
Ketels M, Rasmussen CL, Korshøj M, Gupta N, De Bacquer D, Holtermann A, Clays E. Int J Environ Res Public Health. 2020;17(21):7929. https://doi.org/10.3390/ijerph17217929 . The Relation between Domain-Specific Physical Behaviour and Cardiorespiratory Fitness: A Cross-Sectional Compositional Data Analysis on the Physical Activity Health Paradox Using Accelerometer-Assessed Data.
Bolliger L, Lukan J, Colman E, Boersma L, Luštrek M, De Bacquer D, Clays E. Sources of Occupational Stress among Office Workers—A Focus Group Study. Int J Environ Res Public Health. 2022;19(3):1075. https://doi.org/10.3390/ijerph19031075 .
Heckathorn DD. Snowball versus respondent-driven sampling. Sociol Methodol. 2011;41:355–66. https://doi.org/10.1111/j.1467-9531.2011.01244.x .
Holloway I, Wheeler S. Qualitative Research in Nursing and Healthcare. 4th edition. Oxford: Wiley-Blackwell; 2016.
Eurofound. The multiple dimensions of job quality. In: Sixth European Working Conditions Survey – Overview report. (2017 update). Publications Office of the European Union. 2017. https://www.eurofound.europa.eu/en/publications/2016/sixth-european-working-conditions-survey-overview-report . Accessed 10 Okt 2022.
Higginbotham K, Jones I, Johnson M. A grounded theory study: Exploring Health Care professionals decision making when managing end stage heart failure care. J Adv Nurs. 2021;77(7):3142–55. https://doi.org/10.1111/jan.14852 .
Dierckx de Casterlé B, Gastmans C, Bryon E, Denier Y. QUAGOL: a guide for qualitative data analysis. Int J Nurs Stud. 2012;49(3):360–71. https://doi.org/10.1016/j.ijnurstu.2011.09.012 .
Metelski FK, Guedes Dos Santos JL, Cechinel-Peiter C, Fabrizzio GC, Schmitt MD, Heilemann M. Teoria Fundamentada Construtivista: Características E Aspectos Operacionais para a Pesquisa em Enfermagem. Revista Da Escola De Enfermagem Da Usp. 2021;55. https://doi.org/10.1590/s1980-220x2020051103776 .
Polit DF, Beck CT. Nursing Research - Generating and assessing evidence for nursing practice. 10th ed. Wolters Kluwer; 2016.
Hudon E, Chouinard M, Ellefsen E, Beaudin J, Hudon C. The experience of pregnant women in contexts of vulnerability of prenatal primary nursing care: a descriptive interpretative qualitative study. BMC Pregnancy Childbirth. 2023;23(1):187. https://doi.org/10.1186/s12884-023-05474-z .
O’Brien BC, Harris IB, Beckman TJ, Reed DA, Cook DA. Standards for reporting qualitative research. Acad Med. 2014;89(9):1245–51. https://doi.org/10.1097/acm.0000000000000388 .
Aleid AA, Eid Elshnawie HA, Ammar A. Assessing the work activities related to Musculoskeletal disorder among critical care nurses. Crit Care Res Pract. 2021;1–10. https://doi.org/10.1155/2021/8896806 .
Clays E, Hallman D, Oakman J, Holtermann A. Objectively measured Occupational Physical Activity in Blue-Collar workers: what is the role of job type, gender and Psychosocial resources? Appl Ergon. 2020;82. https://doi.org/10.1016/j.apergo.2019.102948 .
Ameri M, Mirhosseini S, Basirinezhad MH, Ebrahimi H. Prevalence of restless legs syndrome and its relationship with fatigue in critical care nurses. Indian J Crit Care Med. 2021;25(11):1275–79. https://doi.org/10.5005/jp-journals-10071-24010 .
Arial M, Benoît D, Wild P. Exploring implicit preventive strategies in Prehospital Emergency Workers: a Novel Approach for preventing back problems. Appl Ergon. 2014;45(4):1003–9. https://doi.org/10.1016/j.apergo.2013.12.005 .
Liu Q, Liu X, Lin H, Sun Y, Geng L, Lyu Y, Wang M. Occupational low back Pain Prevention Capacity of nurses in China: a Multicenter cross-sectional study. Front Public Health. 2023;11. https://doi.org/10.3389/fpubh.2023.1103325 .
Cho G, Kang J, Type D, Personality, Post-Traumatic Stress Disorder Symptoms among Intensive Care Unit Nurses. The Mediating Effect of Resilience. PLoS ONE. 2017;12(4). https://doi.org/10.1371/journal.pone.0175067 .
Smyth C. The Pittsburgh Sleep Quality Index (PSQI). In: Best Practices in Nursing Care to Older Adults. 2012. https://andreasbjerregaard.files.wordpress.com/2015/01/try_this_6_1.pdf . Accessed 15 Jan 2023.
Adkins CL, Premeaux SF. Spending time: the impact of hours worked on work–family conflict. J Vocat Behav. 2012;80(2):380–89. https://doi.org/10.1016/j.jvb.2011.09.003 .
Pool IA, Poell RF, Berings MGMC, ten Cate O. Strategies for Continuing Professional Development among younger, Middle-Aged, and older nurses: a Biographical Approach. Int J Nurs Stud. 2015;52(5):939–50. https://doi.org/10.1016/j.ijnurstu.2015.02.004 .
Weale V, Oakman J, Clays E. Does work–family conflict play a role in the relationship between work-related hazards and Musculoskeletal Pain? Am J Ind Med. 2021;64(9):781–91. https://doi.org/10.1002/ajim.23280 .
Makiko S, Okubo R, Sado M, Piedvache A, Mizoue T, Yamaguchi K, Morisaki N. Emotional exhaustion of Burnout among Medical Staff and its Association with Mindfulness and Social Support: a single Center Study during the COVID-19 pandemic in Japan. Front Psychiatry. 2022;13. https://doi.org/10.3389/fpsyt.2022.774919 .
Li CY, Sung FC. A review of the healthy worker effect in Occupational Epidemiology. Occup Med. 1999;49(4):225–29. https://doi.org/10.1093/occmed/49.4.225 .
Kim TJ, von dem Knesebeck O. Perceived job insecurity, unemployment and depressive symptoms: a systematic review and meta-analysis of prospective observational studies. Int Arch Occup Environ Health. 2016;89(4):561–73. https://doi.org/10.1007/s00420-015-1107-1 .
Mazzetti G, Robledo E, Vignoli M, Topa G, Guglielmi D, Schaufeli WB. Work Engagement: a meta-analysis using the job demands-resources Model. Psychol Rep. 2023;126(3):1069–107. https://doi.org/10.1177/00332941211051988 .
Ghanayem M, Srulovici E, Zlotnick C. Occupational strain and job satisfaction: the Job demand–resource moderation–mediation model in Haemodialysis units. J Nurs Adm Manag. 2020;28(3):664–72. https://doi.org/10.1111/jonm.12973 .
Download references
Acknowledgements
Not applicable.
The open-access grant for this study was funded by the Department of Public Health and Primary Care of Ghent University and by the Strategic Policy Cell of the Ghent University Hospital.
Author information
Authors and affiliations.
Strategic Policy Cell, Ghent University Hospital, Corneel Heymanslaan 10, Ghent, 9000, Belgium
Lukas Billiau & Kristof Eeckloo
Faculty of Medicine and Health Sciences, Department of Public Health and Primary Care, Ghent University, Corneel Heymanslaan 10, Ghent, 9000, Belgium
Larissa Bolliger, Els clays, Kristof Eeckloo & Margo Ketels
You can also search for this author in PubMed Google Scholar
Contributions
LBi, MK, EC, KE, and LBo contributed to the conceptualisation and design of the study. LBi acquired the data, while LBi and LBo undertook the formal analysis of the data. Data curation was taken up by LBi. Resources were provided by EC and KE. LBi developed the original draft preparation, while MK, EC, LBo, and KE critically reviewed and edited the manuscript. Supervision was ensured by MK, EC, KE, and LBo. KE and EC performed the funding acquisition. All authors have read the final draft and agreed to publish this version.
Corresponding author
Correspondence to Lukas Billiau .
Ethics declarations
Ethical approval and consent to participate.
Ethical approval was granted for this study by the Ethics Committee of the Ghent University Hospital (THE-2022-0152) and by the Commission of Medical Ethics of the local hospital in Flanders, Belgium (AZGT2022023). All participants received written and verbal information and gave their written informed consent before enrollment. All methods were carried out in accordance with relevant guidelines and regulations.
Consent for publication
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Billiau, L., Bolliger, L., clays, E. et al. Flemish critical care nurses’ experiences regarding the influence of work-related demands on their health: a descriptive interpretive qualitative study. BMC Nurs 23 , 387 (2024). https://doi.org/10.1186/s12912-024-02032-6
Download citation
Received : 28 October 2023
Accepted : 21 May 2024
Published : 06 June 2024
DOI : https://doi.org/10.1186/s12912-024-02032-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Critical care
- Psychosocial
- Qualitative research
- Sustainable employment
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]
- USC Libraries
- Research Guides
Organizing Your Social Sciences Research Paper
- 3. The Abstract
- Purpose of Guide
- Design Flaws to Avoid
- Independent and Dependent Variables
- Glossary of Research Terms
- Reading Research Effectively
- Narrowing a Topic Idea
- Broadening a Topic Idea
- Extending the Timeliness of a Topic Idea
- Academic Writing Style
- Applying Critical Thinking
- Choosing a Title
- Making an Outline
- Paragraph Development
- Research Process Video Series
- Executive Summary
- The C.A.R.S. Model
- Background Information
- The Research Problem/Question
- Theoretical Framework
- Citation Tracking
- Content Alert Services
- Evaluating Sources
- Primary Sources
- Secondary Sources
- Tiertiary Sources
- Scholarly vs. Popular Publications
- Qualitative Methods
- Quantitative Methods
- Insiderness
- Using Non-Textual Elements
- Limitations of the Study
- Common Grammar Mistakes
- Writing Concisely
- Avoiding Plagiarism
- Footnotes or Endnotes?
- Further Readings
- Generative AI and Writing
- USC Libraries Tutorials and Other Guides
- Bibliography
An abstract summarizes, usually in one paragraph of 300 words or less, the major aspects of the entire paper in a prescribed sequence that includes: 1) the overall purpose of the study and the research problem(s) you investigated; 2) the basic design of the study; 3) major findings or trends found as a result of your analysis; and, 4) a brief summary of your interpretations and conclusions.
Writing an Abstract. The Writing Center. Clarion University, 2009; Writing an Abstract for Your Research Paper. The Writing Center, University of Wisconsin, Madison; Koltay, Tibor. Abstracts and Abstracting: A Genre and Set of Skills for the Twenty-first Century . Oxford, UK: Chandos Publishing, 2010;
Importance of a Good Abstract
Sometimes your professor will ask you to include an abstract, or general summary of your work, with your research paper. The abstract allows you to elaborate upon each major aspect of the paper and helps readers decide whether they want to read the rest of the paper. Therefore, enough key information [e.g., summary results, observations, trends, etc.] must be included to make the abstract useful to someone who may want to examine your work.
How do you know when you have enough information in your abstract? A simple rule-of-thumb is to imagine that you are another researcher doing a similar study. Then ask yourself: if your abstract was the only part of the paper you could access, would you be happy with the amount of information presented there? Does it tell the whole story about your study? If the answer is "no" then the abstract likely needs to be revised.
Farkas, David K. “A Scheme for Understanding and Writing Summaries.” Technical Communication 67 (August 2020): 45-60; How to Write a Research Abstract. Office of Undergraduate Research. University of Kentucky; Staiger, David L. “What Today’s Students Need to Know about Writing Abstracts.” International Journal of Business Communication January 3 (1966): 29-33; Swales, John M. and Christine B. Feak. Abstracts and the Writing of Abstracts . Ann Arbor, MI: University of Michigan Press, 2009.
Structure and Writing Style
I. Types of Abstracts
To begin, you need to determine which type of abstract you should include with your paper. There are four general types.
Critical Abstract A critical abstract provides, in addition to describing main findings and information, a judgment or comment about the study’s validity, reliability, or completeness. The researcher evaluates the paper and often compares it with other works on the same subject. Critical abstracts are generally 400-500 words in length due to the additional interpretive commentary. These types of abstracts are used infrequently.
Descriptive Abstract A descriptive abstract indicates the type of information found in the work. It makes no judgments about the work, nor does it provide results or conclusions of the research. It does incorporate key words found in the text and may include the purpose, methods, and scope of the research. Essentially, the descriptive abstract only describes the work being summarized. Some researchers consider it an outline of the work, rather than a summary. Descriptive abstracts are usually very short, 100 words or less. Informative Abstract The majority of abstracts are informative. While they still do not critique or evaluate a work, they do more than describe it. A good informative abstract acts as a surrogate for the work itself. That is, the researcher presents and explains all the main arguments and the important results and evidence in the paper. An informative abstract includes the information that can be found in a descriptive abstract [purpose, methods, scope] but it also includes the results and conclusions of the research and the recommendations of the author. The length varies according to discipline, but an informative abstract is usually no more than 300 words in length.
Highlight Abstract A highlight abstract is specifically written to attract the reader’s attention to the study. No pretense is made of there being either a balanced or complete picture of the paper and, in fact, incomplete and leading remarks may be used to spark the reader’s interest. In that a highlight abstract cannot stand independent of its associated article, it is not a true abstract and, therefore, rarely used in academic writing.
II. Writing Style
Use the active voice when possible , but note that much of your abstract may require passive sentence constructions. Regardless, write your abstract using concise, but complete, sentences. Get to the point quickly and always use the past tense because you are reporting on a study that has been completed.
Abstracts should be formatted as a single paragraph in a block format and with no paragraph indentations. In most cases, the abstract page immediately follows the title page. Do not number the page. Rules set forth in writing manual vary but, in general, you should center the word "Abstract" at the top of the page with double spacing between the heading and the abstract. The final sentences of an abstract concisely summarize your study’s conclusions, implications, or applications to practice and, if appropriate, can be followed by a statement about the need for additional research revealed from the findings.
Composing Your Abstract
Although it is the first section of your paper, the abstract should be written last since it will summarize the contents of your entire paper. A good strategy to begin composing your abstract is to take whole sentences or key phrases from each section of the paper and put them in a sequence that summarizes the contents. Then revise or add connecting phrases or words to make the narrative flow clearly and smoothly. Note that statistical findings should be reported parenthetically [i.e., written in parentheses].
Before handing in your final paper, check to make sure that the information in the abstract completely agrees with what you have written in the paper. Think of the abstract as a sequential set of complete sentences describing the most crucial information using the fewest necessary words. The abstract SHOULD NOT contain:
- A catchy introductory phrase, provocative quote, or other device to grab the reader's attention,
- Lengthy background or contextual information,
- Redundant phrases, unnecessary adverbs and adjectives, and repetitive information;
- Acronyms or abbreviations,
- References to other literature [say something like, "current research shows that..." or "studies have indicated..."],
- Using ellipticals [i.e., ending with "..."] or incomplete sentences,
- Jargon or terms that may be confusing to the reader,
- Citations to other works, and
- Any sort of image, illustration, figure, or table, or references to them.
Abstract. Writing Center. University of Kansas; Abstract. The Structure, Format, Content, and Style of a Journal-Style Scientific Paper. Department of Biology. Bates College; Abstracts. The Writing Center. University of North Carolina; Borko, Harold and Seymour Chatman. "Criteria for Acceptable Abstracts: A Survey of Abstracters' Instructions." American Documentation 14 (April 1963): 149-160; Abstracts. The Writer’s Handbook. Writing Center. University of Wisconsin, Madison; Hartley, James and Lucy Betts. "Common Weaknesses in Traditional Abstracts in the Social Sciences." Journal of the American Society for Information Science and Technology 60 (October 2009): 2010-2018; Koltay, Tibor. Abstracts and Abstracting: A Genre and Set of Skills for the Twenty-first Century. Oxford, UK: Chandos Publishing, 2010; Procter, Margaret. The Abstract. University College Writing Centre. University of Toronto; Riordan, Laura. “Mastering the Art of Abstracts.” The Journal of the American Osteopathic Association 115 (January 2015 ): 41-47; Writing Report Abstracts. The Writing Lab and The OWL. Purdue University; Writing Abstracts. Writing Tutorial Services, Center for Innovative Teaching and Learning. Indiana University; Koltay, Tibor. Abstracts and Abstracting: A Genre and Set of Skills for the Twenty-First Century . Oxford, UK: 2010; Writing an Abstract for Your Research Paper. The Writing Center, University of Wisconsin, Madison.
Writing Tip
Never Cite Just the Abstract!
Citing to just a journal article's abstract does not confirm for the reader that you have conducted a thorough or reliable review of the literature. If the full-text is not available, go to the USC Libraries main page and enter the title of the article [NOT the title of the journal]. If the Libraries have a subscription to the journal, the article should appear with a link to the full-text or to the journal publisher page where you can get the article. If the article does not appear, try searching Google Scholar using the link on the USC Libraries main page. If you still can't find the article after doing this, contact a librarian or you can request it from our free i nterlibrary loan and document delivery service .
- << Previous: Research Process Video Series
- Next: Executive Summary >>
- Last Updated: May 30, 2024 9:38 AM
- URL: https://libguides.usc.edu/writingguide
- Open access
- Published: 27 May 2024
Understanding patient-related barriers to hydroxyurea use among adolescent and adult patients with sickle cell disease in Mulago and Kiruddu hospitals, Uganda, a qualitative study
- Priscilla Namaganda 1 ,
- Patience Nantume 2 ,
- Kelvin Roland Mubiru 3 ,
- Adelliine Twimukye 2 &
- Christine Sekaggya Wiltshire 2
BMC Health Services Research volume 24 , Article number: 666 ( 2024 ) Cite this article
195 Accesses
Metrics details
In 2016, Uganda added Hydroxyurea (HU) to the list of essential drugs to treat sickle cell disease SCD. However, Hydroxyurea utilization has been low for several countries in sub-Saharan Africa. This study examined patient-related barriers to hydroxyurea use among adolescent and adult patients with sickle cell disease in Mulago and Kiruddu hospitals, in Uganda.
To understand the patient-related barriers to hydroxyurea use among adolescent and adult patients with sickle cell disease, we conducted a parallel convergent mixed methods study at outpatient departments of two national referral hospitals in Uganda from October 2022 to January 2023. The cross-sectional mixed-methods study employed both quantitative and qualitative methods. We collected survey data from a systematic sample of 259 participants and conducted individual interviews with a purposive sample of 40 participants (20 adolescents or their caregivers and 20 adult patients with SCD) and interviewed them individually on their knowledge, perceptions, barriers, and facilitators of HU utilization. Descriptive data were analyzed using Stata 16, whereas qualitative data were analyzed thematically using an inductive approach supported by NVivo 12 software. We triangulated data to determine the concordance of qualitative and quantitative data.
The study enrolled 40 participants for qualitative interviews and 259 patients for quantitative, with an average age of 16, over half being female, 46% having secondary education, and 96% unmarried. The prevalence of HU use was 78%. The study identified three themes as follows: Patient barriers at the individual including Inadequate knowledge about HU, Persistent pain, Poor adherence to HU, Poor communication with health care workers, and Psychosocial and emotional challenges. At the facility level, long queues and poor quality of care, drug-related side effects that affect HU, and drug stock-outs were reported. Myths, rumors, and misconceptions about HU, and gender-related barriers were reported to affect HU utilization at a community level. Facilitators for the use of HU and recommendations for improvement. Facilitators included perceived benefits, long duration on HU, information sharing by healthcare workers, availability of complementary drugs, confirmation of diagnosis, and availability of medication at public health facilities or private pharmacies. Patients suggested continuous adherence support, encouragement from healthcare workers, sensitization about benefits and risks, a peer-to-peer approach, and financial support for adolescents and women to start businesses to resolve financial problems.
Implementing the use of HU has been challenging in Uganda and needs improvement. Facilitators to hydroxyurea use have been highlighted, though Patient-identified barriers at individual, facility, and community levels that need to be resolved. The experiences and insights shared by our participants provide invaluable guidance for increasing the uptake of HU. Further studies are needed to establish validated instruments to assess patients’ pain communication and adherence to the HU regimen.
Peer Review reports
In Africa, sickle cell disease (SCD) contributes substantially to mortality in children younger than 5 years. The global burden has been quantified, with SCD accounting for 6.4% of the under-5 mortality across all of Africa [ 1 ]. However, in countries with greater sickle allele frequencies and lower childhood mortality rates, such as Uganda, SCD may account for up to 15% of under-5 mortality [ 2 ]. The mortality rate in adult patients with SCD is not known presumably because of a lack of accurate data but is thought to be high as more children with SCD survive into adolescence and adulthood, they are faced with poor access to comprehensive sickle cell care with a continuing risk of complications or death [ 2 ].
Hydroxyurea is one of the approved drugs for treating sickle cell disease [ 3 ]. The mechanism by which hydroxyurea works is rather unknown although its efficacy in the treatment of SCD is generally attributed to its ability to boost the levels of fetal hemoglobin (Hb F, α 2 γ 2 ) hence lowering the concentration of HbS. HbF is protective against clinical severity, and low-percentage HbF is associated with a higher risk of developing Vaso-occlusive complications, organ damage, and early death. Systemic review studies have documented the efficacy of hydroxyurea in adult patients with SCD [ 3 ]. In Uganda, the NOHARM and REACH studies reported a reduction in SCD-related complications with the use of hydroxyurea and appeared to be safe for children with SCD without increased severe malaria, infections, or adverse events [ 4 , 5 ].
Hydroxyurea was added to the list of essential drugs in Uganda in 2016 but it is not readily available [ 6 ].
The number of patients with SCD currently taking hydroxyurea is about 33%; this is undocumented data from patient charts. This low percentage of use could be due to limited access and availability of drugs, practitioners’ low knowledge of HU use, and patients’ fear of drug toxicities. Therefore, this study sought to assess barriers to HU treatment among this cohort of patients and document them. This study focused on knowledge, perceptions, barriers, and facilitators of adolescent and adult patients with sickle cell disease regarding HU because there is minimal data and even the data that is available focuses on children, not adults. Reasons reported by authors in studies done included fear of cancer and other side effects, not wanting to take a medication, not wanting to have required laboratory monitoring, or not thinking the medication would work [ 7 ]. The primary goal and benefit of patient-centered care is to improve individual health outcomes, not just population health outcomes, although population outcomes may also improve [ 8 ]. Not only do patients benefit, but providers and healthcare systems benefit as well, through (a) Improved satisfaction among patients and their families, (b) Enhanced reputation of providers among healthcare consumers, (c) Better morale and productivity among clinicians and ancillary staff, (d) Improved resource allocation, (e) Reduced expenses and increased financial margins throughout the continuum of care [ 8 ].
With greater use of HU for eligible patients, it is expected that fewer patients will be hospitalized for complications of SCD, resulting in a net reduction of national healthcare costs for patients with SCD [ 9 ]. In addition, the broader appropriate use of HU in patients with SCD should improve their quality of life and productivity [ 9 ]. With this information, we can lobby the government and/or donors to avail recourses for continued supply of HU and other resources like laboratory capacity that aid us in giving comprehensive care to patients with SCD. Therefore, we conducted a mixed methods study to identify the knowledge, perceptions, barriers, and facilitators of adolescent and adult patients with sickle cell disease regarding HU and suggest interventions to facilitate HU uptake in Uganda. We hypothesized that there was a relationship between patient-related barriers and hydroxyurea use among patients with SCD.
Study design
From October 2022 to January 2023, we conducted a cross-sectional mixed-methods study (parallel convergent) with qualitative components using a phenomenological approach.
Study setting
The study was conducted at the Sickle cell clinic in Mulago Hospital sickle cell clinic and Kiruddu Hospital, hematology. The Sickle Cell Clinic is an innovation for treating children with SCA with acute pain and other medical complications as outpatients. The Mulago sickle cell clinic attends to children, adolescents, and adult patients with SCD. The Kiruddu clinic attends to adolescent and adult patients with SCD in addition to other hematological conditions. Both Mulago and Kiruddu are national referral hospitals in Uganda and are teaching hospitals for Makerere University, College of Health Sciences. The Mulago SCD clinic cares for more than 300 patients with SCD. The hematology clinic at Kiruddu Hospital cares for 100 to 150 patients with SCD.
Sample size estimation
We purposively selected 40 participants to participate in the qualitative interviews. The actual sample size (40) was determined by how many participants were required to explore all the research questions and to achieve thematic saturation. It was difficult to determine the ideal sample size for achieving these objectives at the early stage of the research. Therefore, the process of participant selection was iterative, involving several rounds of selection and interviews as will be necessary to achieve thematic saturation. Data was collected until no new themes or patterns emerged from participants interviewed participants selected from each study site. 20 individual interviews were carried out in each selected site, making a total of 40 Individual interviews from two study sites. Patients were interviewed to identify the barriers to the use of hydroxyurea through In-depth interviews using an in-depth interview form developed for the study with 20 purposively selected patients per site. The criteria for the selection of patients for in-depth interviews were 10 adults (5 males and 5 females), and 10 adolescents (5 males and 5 females) who have ever missed appointments or drugs from each clinic. Also, their understanding, experiences, and what they had heard regarding using Hydroxyurea were assessed. All the interviews were conducted from the hospital premises and in a language preferred by the participants and audio recorded. All adolescents were interviewed with their caretakers and each caretaker signed a parent-guardian consent form in addition to the adolescent signing an assent form.
Eligibility for HU use was (a) Three or more sickle cell-associated moderate to severe pain crises in 12 months, requiring hospitalization or management at a health facility, (b) Sickle cell-associated pain that interferes with daily activities and quality of life, (c) History of severe and/or recurrent acute chest syndrome, (d) Severe symptomatic chronic anemia that interferes with daily activities or quality of life(severe symptomatic anemia criteria was assessed based on the need for blood transfusion). if participants responded yes to any of the above criteria, they were eligible for HU use. Patients with other sickle cell syndromes – e.g., Hb SC disease, S/ß thalassemia, pregnant, severely ill study, and declined to participate in the study were excluded.
The sample size for quantitative was estimated using Leslie Kish’s (1964) formula for sample size calculation. With a prevalence of HU use at 33.7% as reported by a study done in Oman [ 10 ] and at a 0.05 level of significance, the sample was estimated at 260 participants. The sickle cell clinic at Mulago Hospital runs daily and that at Kiruddu on Thursday of every week. Patients with SCD who came for assessment were screened using a questionnaire developed for the study and each one of them was informed about the study with the help of a research assistant. Patients who are taking HU or have taken HU were recorded. Patients who are not taking HU were assessed to determine if they fit the criteria for starting HU as described above. If participants responded to any of the above criteria, they were enrolled in the study after obtaining informed consent from research assistants. Patients enrolled were asked to fill out a standardized questionnaire with the help of research assistants. Information obtained included (a) demographic i.e. age, gender, address, level of education, religion, and occupation, (b) time when patient joined the clinic, past and current medications, history of SCD-associated complications and history of admissions, (c) status of HU use and reasons for not initiating HU and possible solutions to these challenges.
Study variables
Independent variables.
We collected data on; age, gender, address, level of education, religion, occupation, commonest complications of SCD experienced, indications for HU use, and the common medications used.
Dependent variables
Our outcomes were willingness to use HU, perceptions about HU use, reasons for not initiating HU and possible solutions to these challenges.
Procedures for data collection and instruments
Quantitative data.
We used a systematic sampling method for the survey. For the quantitative objective, all patients with SCD were screened and those who met the inclusion criteria were enrolled in the study. We therefore included every 4th participant in the survey beginning with the 4th adult until the sample size was attained. We used maximum variation purposive sampling to select the participants for the in-depth interviews. For the survey, we used an interviewer-administered semi-structured questionnaire to collect data on the 259 participants using a questionnaire administered by a research assistant. For the 40 individual interviews, we used an interview guide which was used to collect perceptions on HU. Interviews lasted approximately 10–20 min. Data collection occurred over three months and transcription began as data collection was ongoing.
Data quality control
The questionnaire was pre-tested on 5 participants from the same community to ensure that the questions were clear and understandable to participants. The Questionnaires and Interview guide were translated into the local language and then back-translated to English as part of standard operating procedures such that they have retained their meaning. The research assistants were adequately trained for 7 days and routinely supervised while in the field and the data they were collecting by the principal investigator to ensure the correct use of data collection tools and adherence to ethical principles.
To ensure reliability, we set clear research questions to expand on responses. Qualitative data was collected separately from quantitative data (parallel convergence). Codes and qualitative findings were crosschecked to improve reliability. Consensus between two or more observers was done to establish reliability. We used NVivo version 12 software to manage narrative data.
To ensure validity, all transcripts were checked for accuracy and completeness by the interviewers to enhance data validity. Feedback from research participants (member check) after analysis and interpretation was obtained in an organized results dissemination workshop. Documentation of member checks and interpretations that were changed because of member feedback was done. Triangulation combined quantitative (survey) and qualitative data collection methods (in-depth interviews) in this single study. Triangulation of various data collection methods was used. These included questionnaires, Topic guides (In-depth interviews), transcripts, field notes, and Literature review. This was aimed at verifying information, or facts obtained from using other methods.
Data management and analysis
Quantitative data collected were double-entered into the computer using EPI-DATA (version 3.1) software to minimize data entry errors. Data was exported to STATA version 15 for data cleaning and analysis. Data was then backed up and archived using codes to ensure confidentiality. The descriptive characteristics were presented using frequencies and percentages or proportions in tables. Numerical data was summarized using means and standard deviations for normally distributed continuous data or medians and interquartile ranges for continuous but skewed variables. The prevalence of hydroxyurea use among adult patients was calculated as a proportion of adult patients with SCD who have ever used hydroxyurea out of the total number of participants who are eligible for HU use with its 95% confidence intervals.
The Qualitative study was guided by the ethical principles of the Association of Social Anthropologists. These principles included protecting research participants, anticipating harm, avoiding undue intrusion, rights to confidentiality and anonymity, intellectual property rights, and participant involvement in research. Recording and storing participants’ information was done in a manner that facilitated greater confidentiality and anonymity, including the use of pseudonyms to describe participants during interviews, separation of participants’ ID information from their transcripts, storage of participant information in secured locations and password-protected hard drives, removal of participants names in all research dissemination outputs. Research assistants obtained informed consent prior to start of individual interviews. The Individual interviews were conducted in one-to-one and face-to-face format to provide greater privacy and assure participants of confidentiality. We conducted an inductive thematic analysis collected from individual interviews with different respondent categories such as (20 adolescents or their caregivers and 20 adult patients with SCD). The analysis examined meanings, themes, and patterns that manifested texts from the interviews regarding HU use in two hospitals in Uganda. All audio recordings from open-ended questions based on interview guides were transcribed verbatim. Two coders Individually read each transcript line by line and identified key concepts to develop a coding framework. A coding framework based on eight transcripts that were manually reviewed and coded to generate the initial set of codes that were crosschecked iteratively between two coders (AT & PN) for consensus and to improve reliability. All transcripts were imported into NVivo version 12 software for open coding and management of data. An initial codebook was developed, and the revised codes were grouped into categories and identified themes. Illustrative quotations for each emergent theme were selected for the results narration.
283 participants were assessed and 259 were enrolled in the study as shown in the flow chart, Fig. 1 .
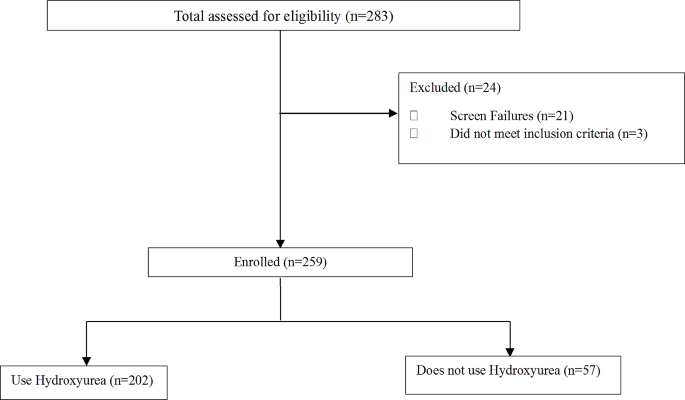
Flow chart showing enrolment profile
Characteristics of adults and adolescents
The total sample size was 259, 221 participants were recruited from the Mulago Hospital sickle cell clinic and 38 from Kiruddu Hospital. At the Mulago sickle cell clinic, the average age was 16 years, with 58.5% being female, and 46% having an education level of secondary. At Kiruddu Hospital, the median age was 24, with 71.1% being female, and 48.1% having an education level of secondary. The average cost of transport to and from the hospital was 11,000 Ugx. The average duration of HU use was 24 months. All this is summarized in Table 1 .
Eligibility for HU use
259 participants met the criteria for HU, 202(78.0%) were taking HU, and 57 participants met the criteria for HU use but were not taking HU. Of those that use HU, 92.1% were current users and 7.9% were past users. HU use among eligible patients is shown in Table 2 .
Patient-related barriers to HU use
Painful crisis was the most common indication for HU use reported in 94.6% of participants, followed by chest syndrome (28%), anemia, 19.4%, and avascular necrosis, 24.7%. indication for HU use is summarized in Table 3 above.
Indications for initiating HU use
The study identified three themes as follows: Patient barriers at the individual, facility, and community level as shown in Tables 4 , 5 and 6 , and 7 . Facilitators for the use of HU and recommendations for improvement as displayed in Table 8 .
Individual barriers
Financial constraints.
The most common reason for stopping HU use was lack of affordability reported by 81.2% of participants. This information is summarised in Table 5 below. The major challenge among 19 (48%) participants from qualitative interviews was financial constraints to buy medication, and food and meet the transport costs to access care.
“There are times when I skipped my medicine doses… Sometimes it was due to money; if I didn’t have the money to buy the tablets. Because we are supposed to buy the tablets—sometimes you go to the pharmacy, and they are expensive, yet you don’t have money. You use the little money you must buy some tablets and they get finished, and I have no money to buy more. So, I first miss some days, and a few times I depend on Panadol and Ibuprofen for emergencies. I take it in case I don’t have the medicine not daily—they told me I could take it occasionally if I am constrained financially and unable to buy the medicine”.
-- IDI, 18, female, adult, Mulago.
Most adults and adolescents were not able to pay for prescribed sickle cell drugs and other ailments because they were expensive.
“… There was no money to buy it because a packet is shs.15,000; just one packet… yet buying it is expensive and I have no money. Now I no longer stay with my father; my mother stays home; she does not work. If my father goes to work and takes a long time there, my mother is suffering to buy the medicine. She buys it for shs. 15,000 but it gets finished in a week, so she must look for more shs. 15,000 to buy another dose”. -- IDI, 19, Male, adolescent, Mulago.
Most of the adolescents said they were unemployed and were mainly dependent on their parent’s support, which was sometimes limited:
“If there is transport because I am always at home. Ever since they fired me from my job, I have been at home”. -- IDI, 3 1, female, adolescent, Mulago.
Inadequate knowledge
Inadequate knowledge about HU among adolescents and adults by few participants. Generally, most individual participants from qualitative (27, 68%) and quantitative (231 (88.2%) across all age categories had a high level of awareness about hydroxyurea and its related benefits as shown in Table 5 below. For the few adult participants who lacked awareness about Hydroxyurea, it was because health workers did not inform them about it, and some had never started on it.
Because I didn’t know about it [Hydroxyurea]; they had never told me about it. So, the doctors asked me, “Have you ever used hydroxyurea?” and I told them, “I don’t know about it . -- IDI, 22, male, adult, Mulago.
Among adolescents, there was low knowledge about HU due to limited sensitization as they did not receive enough health education. Moreover, they reported rumors, myths, and misconceptions about sickle cell in the community.
“Most times what scares them, they say, “Once you start taking the drug and then stop you die”, it scares them as well—okay, the rumors are so many”. -- IDI, 11, Male, youth, Mulago.
Some participants said there was a lack of awareness about Hydroxyurea in the community because they were not sensitized and had not come across people who swallowed it:
“Community people have not been well oriented about Hydroxyurea benefits by the doctors… they have not heard anyone on it so far”. -- IDI, 16_ adult, Mulago.
Persistent pain affected the use of HU
Nearly half (38%) of the participants who participated in individual interviews reported persistent pain despite taking painkillers as a major challenge that hindered proper adherence.
They used to administer painkillers to me since I had a lot of pain! And if the pain comes, it is so strong; it is severe because at school there is a health facility they would do their best with the painkillers but they had no effect. So, they would bring me here” . -- IDI, 28, female, youth, Mulago.
Some participants said they could hardly walk to the health facility due to severe pain, hence missed appointments and picking drugs.
I missed my appointment because I was sick and bedridden, admitted to the hospital. Huh! I feel pain. There are times I could hardly walk…. -- IDI, 10, female, adult, Mulago.
Poor adherence to HU
43% (17, 43%), mainly adolescents from qualitative interviews reported Poor treatment adherence. They missed taking sickle cell medication on time or stopped it for a month or more. The major reasons for missing drugs were pain, running out of drugs, missed appointments to pick drug refills, and lack of funds to buy drugs when they ran out:
“So, when I swallow it in the morning, it takes like 30 minutes, then I go back to normal. But sometimes I miss doses because the medicine is finished before the people at home bring for me more, because I am not near home. They bring it within one week because they also must look for the money to buy it. -- IDI, 28, female, adolescent, Mulago.
Another reason for poor adherence to sick cell medication was forgetfulness. Some participants said they came back from school tired and slept off while others could be distracted by television:
“We leave preps at around 9 pm and I must wash my uniform, I must do this or that. So after, you are exhausted and you just fall on the bed; maybe you say, “Let me read this and swallow the medicine, then I sleep” but before you realize it, they are ringing the bell to wake students up. So that is when I have forgotten and then I remember”. --IDI, 28, female, adolescent, Mulago.
One participant said they had poor access to medication when traveling due to the loss of a loved one and suffered too much pain. They also missed appointments due to illness and admission.”
“I had lost someone. Sometimes, I would be ill and have a lot of pain. I felt too much pain. I missed a dose… Still, I have ever missed taking a dose that was because of my illness. I was admitted”. --IDI, 9, male, adult, Mulago.
Some participants missed drugs due to academic reasons. They could not leave school during the exam period to pick treatment refills.
“There is a time I missed some appointments that in turn made me miss drugs…I am in boarding school and my appointment was due during my examination period, so I was unable to come”. -- IDI, 19, Male, adolescent, Mulago).
One caretaker said adolescent was tired of swallowing several tablets daily hence missed taking drugs on some days.
“Talking about being fed up with the medicine; sometimes I say[caregiver], “I will give you shs.500 if you[adolescent] swallow the medicine”. So personally, when I noticed that on the weekend, she swallows 2000 mg, I said, “Okay, let us leave Monday” and we went against the doctor’s instructions. So honestly, we gave Monday a break; we don’t swallow medicine because she swallowed 2 tablets on Sunday and 2 tablets on Saturday, so we rested on Monday. We resume swallowing it on Tuesday till Sunday, then we rest on Monday. But eh! She totally didn’t like it! So, we discussed and came to that agreement, so that is how we do it”. -- IDI, 30, female, caregiver, Mulago.
Missed routine clinic visits or appointments affected adherence.
Most participants [ 11 ] missed routine clinic visits or appointments mainly because they lacked money for transport to the health facility. The cost of transport for some participants was Ugx 20,000.
“I have never missed a clinic appointment and you said yes…I missed because my mother did not have money for transport, yet she had debts—she had to work so that she could pay the debt she had”. --IDI, 21, female, adolescent, Mulago.
Missed appointments hindered participant’s access to medical care and routine sickle cell monitoring.
“Ever since we started this medication, they told us not to miss any appointments because she must come back and monitor her progress ever since she started hydroxyurea. I believe we won’t miss it again. Previously, we could buy our own medicine but this time round, we won’t miss clinic appointments again”. -- IDI, 14, caregiver, female, Mulago.
Transport constraints were the major reasons for missed appointments. Some participants said they lived at far-off distances from health facilities.
“Since sometimes I live far away and sometimes there is no money for the transport fare… Because there are times when I am suffering symptoms of the illness and I have no transport to bring me to the health Centre for instance now, I just borrowed the money to bring me here. So, I fall sick and swallow the medicine, then I feel better”. -- IDI, 31, female, adult, Mulago.
Only one participant reported that a busy work schedule hindered appointment-keeping.
“I miss appointments because sometimes I am weak, or sometimes I might be busy. I am healthy, but the work I am doing keeps me busy. That is what usually happens”. -- IDI, 22, male, adult, Mulago.
Psychosocial, and emotional challenges
Some participants said they lacked a positive outlook on life. They emphasized they lacked motivation, zeal, and interest to continue taking HU drugs because they had lost hope for a complete cure for sickle cell:
“Sometimes, we lack the zeal to come since we do not have the hope to get completely cured but if the doctor tells you to keep coming and follows you up and encourages you” --IDI, 10, female, adult, Mulago.
Some participants (n = 11, 28%) were anxious and worried to take drugs for life without stopping as they worried could cause undesirable side effects:
“For us that have used it, we experience the benefits, but also worry about the risks like kidney, failure because those are the crucial body organs! So, we worry about all that” --. IDI, 30, female, adult, Mulago.
Some participants (38%) from individual interviews suffered stress due to severe pain especially when they missed medication. They felt bad when missed sickle cell drugs because it would result in painful episodes.
“What I know is that it [hydroxyurea] prevents the painful episodes or controls it but now if you don’t swallow it, the pain returns and this time it is severe. That is what I’m scared of”. --IDI, 20, male, youth, Mulago.
Perceived drug-related side effects affected
Some participants [ 10 ] experienced drug-related side effects that affected adherence to HU, such as headache, dizziness, Painful erections at night, frequent urination, and eyes turned yellow.
“I would have headaches every single day without a break. So, there was a health worker we asked while I was admitted, and he said this drug does not cause headaches and we ignored the issue. But it was a severe headache; they first stopped me from taking it for some time… And they [doctors] told her to stop taking it for 2 weeks and that’s what she did”. --IDI, 24, female, adolescent, and caregiver, Mulago.
Some participants were anxious and worried about taking drugs for life without stopping as they worried could cause undesirable side effects:
“For us that have used it, we experience the benefits, but also worry about the risks like kidney, failure because those are the crucial body organs! So, we worry about all that”. --. IDI, 30, female, adult, Mulago.
Facility-related barriers
Long queues.
Long queues that led to poor quality of care were also reported in the hospital. Some participants were concerned about doctors who left without attending to them, yet they were in severe pain.
“ Anha! Sometimes you go and they tell you, “The time is up; the doctor is leaving, the patients’ queue was long”, sometimes you go and there is no medicine”. -- IDI, 5, female, adult, Mulago.
Some participants said there was no counseling support at the health facility regarding sickle cell at the health facility:
“Uh, they [doctors] did not support me when I missed my appointment. When I came, I was registered and given treatment. They did not do anything else or give me any form of counseling”. --IDI, 9, male, adult, Mulago .
Drug stock-outs
Drug stock-outs were mainly reported by adults. lack of sickle cell medication and other drugs in public health facilities leads patients to run out of drugs. They were told to buy the prescribed drugs from other private pharmacies to resolve issues of drug stock-outs, yet they could not afford them.
“About a month. Initially, they would give us three or six sachets of medicine. They can give you medicine for a two months or three months dose. Then, I buy the rest in the pharmacy. The challenge is some pharmacies do not have it in stock”. -- IDI, 10, female, adult, Mulago.
Some participants reported a lack of free medication in public hospitals.
“…Because even if you find someone and say, “Please help me with shs. 30,000 to buy medicine” they tell you, “Go to Mulago, medicine is there free of charge!” But they don’t know the problem is you will get there and fail to get it”. -- IDI, 5, female, adult, Mulago.
Poor communication with health providers
One participant said they did not report drug-related side effects they experienced to healthcare workers due to forgetfulness.
“I forgot to tell the health workers about the side effects I suffered. Sometimes I simply forget all about it and ignore it and say, “As long as it [side effect] is over, I continue swallowing…Now these health workers initiated me into that medicine and told me to swallow it. I would never skip a dose. They told me to swallow it from Monday to Friday, then I take a different dose for the weekend, and then it is the same for the following week”. -- IDI, 19, Male, Youth, Mulago.
Community-based barriers
Some participants reported that rumors, myths, and misconceptions were the major concerns about sickle cell in the community.
“Most times what scares them, they say, “Once you start taking the drug and then stop you die”, it scares them as well—okay, the rumors are so many” -- IDI, 11, Male, youth, Mulago.
Some participants said there was limited access to sickle cell medication in their nearby community health facilities:
“One time my leg was in severe pain; I had not yet seen the doctor. So, if the health facility was nearby—at that time I would go to Nakaseke, and they work on me. But now, there are no health workers who handle sickle cell cases in Namuwogga”. -- IDI, 27, female, adult Mulago.
Family disagreements or conflict arises from lack of financial provision by man for woman to take child to hospital:
“Sometimes we get challenges, and it affects the family. We even get disagreements between the mother and father; sometimes you are supposed to take the child and he says, “I have no money! If you can go, then go. If you are unable to go, you will go some other time” yet the appointment date is due. So, those are some of the challenges we experience” -- IDI, 26, female, caregiver Mulago.
Facilitators for the use of HU
Facilitators reported by participants were mainly at the Individual and facility level as displayed in Table 7 .
Individual level
Positive perception of HU among adolescents and adults facilitated its utilization. Hydroxyurea use was described as effective pain relief, symptom control, and good and helpful treatment among most of the qualitative participants (n = 28, 70%). This was because it mainly relieved and prevented painful sickle cell episodes, stroke, and malaria. One participant said she received pain relief having taken hydroxyurea, she also read via a Google search about weight gain benefits related to hydroxyurea’s use.
“I suffered severe pain before you started taking it [Hydroxyurea]. The pain was severe! It was so strong that sometimes I could faint because the pain was overwhelming…So far, it is not a bad medicine; it has helped us to decrease the pain so that it is not severe”. -- IDI, 3, female, adolescent, Kiruddu.
Patients reported that Hydroxyurea use improves quality of life as it reduces opportunistic infection and frequenting of hospitals by patients.
“The medicine can make you not go to the hospital every day because the day I began taking the medicine, I stopped going to the hospital. I stopped having infections. The medicine can protect you from getting sick in the cold. You can do anything even when you do not put on a sweater. You feel better. Even if you feel pain, it is not so much”- . - IDI, 15, adult male, Mulago.
Some participants illustrated the ability to do daily activities or tasks very well after using hydroxyurea. They said they had the energy to wash, cook, and perform house chores. Hydroxyurea uses enhanced mobility as one participant said could travel on long journeys having taken it.
“Initially, my back would hurt whenever I would walk a distance such as from this place to home which is no longer the case. I am better. I can perform my tasks very well. I wash, cook, and do everything very well”. --IDI, 9, male, adult, Mulago.
Participants said hydroxyurea use regulated the blood levels and reduced the level of the disease in the body or the blood.
“It seems when we had just gotten initiated onto hydroxyurea, the body was not yet used to it, so the blood levels were a bit unstable. Because when we initiated her onto hydroxyurea, they first checked her blood levels and all that. When we had just initiated her, her blood levels went down, and they initiated her back onto the drug around 2018 in December. And ever since that time, we have not had challenges with her blood levels, expect just eating lots of avocado to supplement”. -- IDI, 30, female, caregiver, Mulago.
Patients reported that Hydroxyurea use prevents a child from anemia, stroke, and other complications.
“Those [patients in waiting area] I have heard them say that it has worked for them; those I have heard especially while we are seated. They say it was effective for them; if the child had many pain episodes, they reduced. Or if the blood levels were reduced—even my brother; he used to have anemia and the pain was severe but when he started swallowing it, it started to reduce”. --IDI, 24, female, caregiver, Mulago.
Long duration on HU, enhanced patient confidence. Most of the participants were aware of hydroxyurea because they had experienced taking it for more than a year which enhanced their confidence. Duration on medication among most participants was between one to eleven years, few took it for less than a year.
“I started hydroxyurea this year in January; we came for a check-up after I went to school because I’m in boarding. Now usually when you take hydroxyurea—remember it is daily, every day I must— “ . --IDI, 28, female, adolescent, Mulago.
Facility level
Information shared by healthcare workers about HU enhanced its uptake. Health providers prescribed hydroxyurea and shared information about it through health education and seminars. They taught about the benefits and risks, the importance of hydroxyurea, and the need for patients to alert doctors in case they experienced unusual Side effects.
“…for us, we got to learn about the side effects from the doctors. But while we were at the seminar, they taught us that it is under the supervision of the doctors, who check frequently. But when we gather as women, those who know and those who don’t know, they say, “It burns the liver and the kidneys”, others say, “It is expensive”. But since you have some knowledge about it, you are firm and whatever you notice about it, you inform the doctor, “Doctor, I notice my fingers are turning” and they counsel you. Because even if we are taking it, as parents we are worried”. -- IDI, 30, female, adult, Mulago.
Healthcare workers performed testing to confirm the diagnosis of sickle cell before treatment initiation that enhanced treatment prescription. There was only one participant who said was started on treatment after symptom identification such as joint and leg swelling.
“I was then diagnosed with sickle cells. So, they asked them, “What signs have you noticed?” Then they said that they saw my joints and legs swelling. So, they got to understand and prescribe medication”. -- IDI, 10, female, adult, Mulago.
The availability of HU drugs enhanced its uptake. Some participants said they bought sickle cell medication from private pharmacies or clinics whenever drugs were not available at public health facilities.
“They [doctors from public facility] gave me the prescription and told me to buy it. So, I bought and took it from the private pharmacy, it was finished. So, after a while, I bought more medicine, but they told us we had to swallow it every day”. -- IDI, 5, female, adult, Mulago.
Recommendations from participants on how to alleviate barriers to SCD care
The major recommendation to patients was for patients to receive continuous advice and encouragement from healthcare workers. They particularly desired health workers to remind them about perfectly adhering to Hydroxyurea because it reduced the constant attacks and kept them healthy. They could advise them to set up reminders such as alarms for perfect adherence.
“We need to receive advice from the health workers. Sometimes, we lack the zeal to come since we do not have the hope to get completely cured but if the doctor tells you to keep coming and follows you up and encourages you” --IDI, 10, female, adult, Mulago.
Patients need to be told about the benefits of hydroxyurea, so that they may accept its early initiation and follow the doctor’s instructions.
“In order to accept the drug; we must tell them about the advantages of hydroxyurea. And I think we should also give them examples; I don’t know if you the health workers see that—personally, my child; I know that when she started taking hydroxyurea, her health condition became better. I regretted why they didn’t tell me earlier, but I feared it because I heard them say, “Once she gets initiated onto it, she takes it for life” and I would say, “Argh!” I was quite afraid of it. But I realized that in this life, many people are taking medicine daily and it helps them. [Hmmm] Maybe Musawo, the question I want to ask you today is, if the person grows up and gets to the child-bearing age, does she stop taking hydroxyurea”. -- IDI, 26, female, caretaker, Mulago.
Continuous sensitization about the benefits and risks of hydroxyurea, to create awareness.
“Other people need more teaching about the thing, and telling them, “If the child takes it, it will reduce the number of times you come here due to the child’s severe health condition” -. - IDI, 28, female, Youth, Mulago.
Counseling hydroxyurea should be done as well as counseling patients to value life.
“A way of encouraging people is to educate them about how important their health is; he shouldn’t be discouraged because he is neither the first nor last because there are many people out there who are ill, but everyone must believe in themselves so that they are healthy. So, if my parent cares, I also must care for myself to make sure I am healthy for the sake of my parent, instead of saying, “I don’t want to swallow medicine” one must sacrifice! --IDI, 18, female, adult, Mulago.
A peer-to-peer approach using experienced patients encourages patients to support each other and testify about the benefits of adhering to sickle cell treatment.
“…there is a school with children who suffer from sickle cell who are about 10. So, they asked me for advice, “Should we swallow hydroxyurea?” because I have spent 7 years. And I told them, “You swallow it, I also swallow it” I don’t discourage them because I have grown up without hydroxyurea. But I said the young ones know that it is helpful to them, so I cannot tell them about the fingernails turning black. Because I see their fingernails; they are not as black as I teach them different vocational skills in their school and they ask me, “Do you also swallow this medicine?” and I tell them I swallow it. But I do notice them. -- IDI, 27, female, adult Mulago.
Need financial support to start up a business as a source of income for medication to meet transport, food, and other needs.
“I was thinking, since she has finished Senior 6, maybe I could start up a small business for her so that she earns some money. Even if she gets shs. 2000, she saves it for clinic appointments and buying medicine” --IDI, 24, female, youth, Mulago.
Urge patients to drink plenty of water and mind their diet and clothing.
“They [patients] should be cautious of the cold weather by wearing a scarf. You should take water instead of Soda, minute maid [ soft drink] because that is not recommended. You would rather buy passion fruits and make your juice since the other drinks contain acids that are not good. I would rather drink water instead of drinking those other drinks. [Okay! ] You must wear a sweater when it is cold and desist from drinking cold water in the cold weather. You must mix it with hot water to become warm”. -- IDI, 17, female, Mulago.
Health facility based
Healthcare workers should address the fears and rumors about sick cell disease and treatment.
“You should address their fears and the rumors because personally, that is what made me afraid at first” -- IDI, 4, male, adult, Mulago.
Healthcare workers should advise/encourage patients to adhere to sickle cell medication:
“You must encourage the patient just like you would say, “You have to swallow folic acid because it increases the blood in the body, if you miss, then the blood levels reduce yet these cells need blood”. So even for that medicine, he/she must swallow it—so one must swallow it daily just as one did for folic acid” –. - IDI, 22, male, adult, Mulago.
There should be free drugs availed at the health facilities:
“Another thing is medicine is expensive! So, what will encourage us to come is, we should get free medicine if it is there. But the one we used to take was easy to access; if they bring us that medicine and at least we get it, find it here, then I am certain that we won’t miss any clinic appointment. Because when you come, you expect to go back with medicine, all you must do is invest in the transport”. -- IDI, 14, female, caretaker, Mulago.
Healthcare managers should ensure a consistent and sufficient drug supply.
Doctors should do follow-ups of patients and set up reminder mechanisms to adhere to treatment and keep routine clinic visits.
“Now there is a certain lady, they gave it to her and after it got finished, she stopped there claiming, “I thought you must give it to us. It is expensive in the pharmacies, and I thought I had to get it from here. Why would I buy it?” She was like, “Who is buying the medicine? Me? It is expensive! If you are giving it to us, give it to us consistently”. Other people need more teaching about the thing, and telling them, “If the child takes it, it will reduce the number of times you come here due to the child’s severe health condition” -- IDI, 28, female, Youth, Mulago.
Healthcare facilities should plan to offer transport refunds to sickle cell patients, “Support us by giving us money for the transport fare. Sometimes we are unable to afford it”.
“Apart from the government supplying the medicine; maybe about the transport as well. If they can, they could organize for us some transport when we are bringing them here because these children—sometimes we get challenges, and it affects the family. We even get disagreements between the mother and father; sometimes you are supposed to take the child and he says, “I have no money! If you can go, then go. If you are unable to go, you will go some other time” yet the appointment date is due. So, those are some of the challenges we experience”. -- IDI, 26, female, youth, Mulago.
Health facilities should allow credit options for patients who lack funds to buy drugs.
“What I think—okay, is it possible to give the people the drugs today and they pay for it another time; you record it down. I want them [doctors] to give us patients] the medicine on credit then they pay later”. --IDI, 20, male, youth, Mulago.
Financial empowerment for women to support sickle cell children at the family level should be done. Work opportunities or Income generation activity (IGA) for caregivers or sickle cell patients should be identified.
“So, we [women] must hustle even more than men—sometimes we come and there is no medicine completely! …for our children, we should be assisted in that regard, train us in income generation activities to support our children’’ -.
-- IDI, 30, female, adult, Mulago.
Community-based
Extension of sickle cell health services to the communities and local districts should be done to resolve the issue of transport.
“We need health facilities in every district because sickle cell patients are quite a number. In my village I was the only one and the whole world knew that I had the ‘virus’ as they used to call it. [Hmmm] and it hindered the boy who almost married me; they told him, “Don’t bother! That one is going to die”. But now… we need those health facilities”. -- IDI, 27, female, adult Mulago. “…they could put up health facilities in communities with health workers who handle sickle cells because you leave the place in severe pain—one time my leg was in severe pain; I had not yet seen the doctor. So, if the health facility was nearby—at that time I would go to Nakaseke, and they work on me. But now, there are no health workers who handle sickle cell cases in Namuwogga” -. -IDI, 27, female, adult Mulago.
Sensitization of patients and community people about Hydroxyurea should be done.
“Patients should be intensively sensitized about it [hydroxyurea] so that they can understand it very well. They should sensitize them so that they understand very well how effective it is”. -- IDI, 32, female, adult, Mulago.
Government should reduce the price of sickle cell medicine to enhance access for all patients.
“If it is possible—because most times the drugs are not in stock here, so they should reduce on the price or cost of the medicine…reduce the cost of that medicine. Some people cannot even start taking it; they live far away, from where they get the medicine, yet it is also expensive. So, it would hinder him or her from accessing it”. -- IDI, 11, Male, youth, Mulago.
The government should put up sickle cell health facilities in rural areas:
“Government should supply the medicine to the health facilities in the rural areas. Supply the medicine for sickle cell disease because even in the government health facilities; if you want medicine, they tell you it is out of stock because I have ever gone there when my drugs were over”. -- IDI, 13, female, youth, Mulago.
The government could support patients by providing more drugs in the health facility or in our clinic here:
“Government should supply the medicine to the health facilities in the rural areas. Supply the medicine for sickle cell disease because even in the government health facilities; if you want medicine, they tell you it is out of stock because I have ever gone there when my drugs were over” -- IDI, 13, female, youth, Mulago.
There is a need for a collaborative partnership with international or non-governmental organizations to support sickle cell patients:
Now, the government; because I have ever been NTV, talking about this issue. Just like they support our friends with HIV, they should also find international organizations to support us as well. Because HIV is serious, these patients are difficult! At least they could get for us only the capsules. -- IDI, 24, female, youth, Mulago.
The overall prevalence of HU use among participants who qualify for its use was high at 78%. This is the first study in Uganda to document the prevalence of HU use among patients with SCD. A literature search didn’t yield any studies documenting the prevalence of HU use among eligible patients. A Nigerian study that assessed Hydroxyurea utilization as a lesson in Public Health found that 65% of patients assessed were eligible for HU use and zero were using it, 5% of patients had been informed of or were aware of hydroxyurea as a treatment option for sickle cell disease [ 12 ]. In our study, though 88.2% of patients knew HU as treatment for SCD.
The high prevalence use of HU found in our study is unlike what other studies found in Africa, this is not uncommon given the high prevalence of SCD in these regions of the world. The high prevalence of use is explained by policies that encourage treatment of SCD e.g., HU is listed on the essential medicine list informed by the high prevalence of SCD hence it is procured and made available up to national referral hospitals. Patients are reviewed by healthcare workers in national referral hospitals who are experts in their field, and such are up to date with the latest management protocols for SCD, this is a key driver in the high prescription rate of HU.
In this study, patient-related barriers to HU use included financial constraints, poor adherence to sickle cell medication, missed routine clinic visits or appointments, psychosocial and emotional challenges, poor communication with health providers, and drug-related side effects (headaches, dizziness, frequent urination and yellowing of eyes).
To the best of our knowledge, this is the first study to document patient-related barriers to HU use among patients with SCD in Uganda. These barriers are like those reported by a cross-sectional survey done in Nigeria. Among patients and caregivers, barriers included lack of knowledge; perceived side effects; cost; religious beliefs of disease causation; and lack of pediatric formulation [ 13 ]. Another study done in Chicago, USA, looked at barriers to hydroxyurea adherence and health-related quality of life in adolescents and young adults with sickle cell disease, they found participants reported negative beliefs/motivational barriers (32%), recall barriers/forgetfulness (44%), and access barriers/paying for hydroxyurea and/or getting refills on time (32%) [ 14 ]. Another study looked at barriers to the use of hydroxyurea in the management of sickle cell disease in Nigeria, reported side effects profiles as the commonest barrier, reported concern for infertility (52.0%), and safety profile of HU in pregnancy and lactation (48.2%) [ 15 ]. A U.S. regional collaborative report on barriers to hydroxyurea use from the perspectives of providers, individuals with sickle cell disease, and families found providers and patient/caregiver reports about hydroxyurea use were inconsistent with one another; adults 26 years and older were least likely to be on hydroxyurea; and the likelihood of being on hydroxyurea decreased with one or more barriers, they also found that, even for patients on hydroxyurea, challenges to taking the medicine at the right time and forgetting were crucial unintentional barriers to adherence. Intentional barriers such as worry about side effects and “tried and it did not work” were important barriers for young adults and adults [ 16 ].
These barriers are not uncommon or unique since SCD is a chronic disease that requires daily medication. Similar challenges are experienced by other patients with chronic conditions [ 17 ]. Patients are bound to get treatment fatigued leading to poor adherence and missed appointments, get depressed, and sometimes suicidal. SCD is prevalent in the black population most of whom are residing in resource-limited settings like sub-Saharan Africa where finances are a major factor in accessing health care. Even in the US, SCD is prevalent among the black population [ 14 ] and most of these populations experience socioeconomic inequalities in developed countries.
These challenges are correlated in that financial constraints coupled with treatment fatigue led to poor adherence to treatment missed appointments, and psychosocial and emotional intrigue.
Other barriers reported were categorized as facility and these included drug stockouts, poor quality of care (referred as few health personnel to attend to them, and lack of counseling services). Community barriers included knowledge gaps and poor access to sickle cell medication in nearby health centers.
These barriers have been reported by other studies, in Nigeria, among clinicians, barriers included limited knowledge of the drug, as well as low self-efficacy to prescribe among physicians and to counsel among nurses; perceived side effects; perceived patient preference for traditional medicine; cost for patient and expense of accompanying laboratory monitoring; and limited availability of the drug and equipment for laboratory monitoring [ 18 ]. Another study in Nigeria reported barriers to hydroxyurea utilization identified by practitioners included safety and toxicity profile (100%), patient compliance (100%), effective follow-up (100%), drug availability (100%), affordability (100%) and specifically concern for reactivation of latent tuberculosis (50%) and carcinogenesis (100%) and teratogenicity (100%) [ 12 ].
In Africa, drug stockouts are a commonality, it is especially more pronounced if the medicine is used for chronic care like HU for SCD as opposed to an acute illness. Government programs support access to life-saving medications for human immunodeficiency virus (HIV), Tuberculosis (TB), and malaria; however, this is not the case for SCD. Advocacy efforts to sustain the continued availability of HU in the SCD treatment program are necessary.
Suggested recommendations by participants included; continuous advice and encouragement from health care workers, continuous sensitization about the benefits and risks of hydroxyurea to create awareness, peer to peer approach using experienced patients to support each other, the need for financial support to start up a business as a source of income for medication to meet transport, food, and other needs, self-motivation and self-love is needed among patients and urge patients to drink plenty of water and mind their diet and clothing.
These recommendations have been suggested by other studies i.e., prospective evaluation of patient’s perceptions of SCD and hydroxyurea in relation to adherence, HRQOL domains, and clinical outcomes is warranted [ 11 ].
Training of sickle cell care providers to attain and maintain competence in the use of hydroxyurea for the treatment of SCD was recommended by the researchers of the study on the level of utilization and provider-related barriers to hydroxyurea use in the treatment of SCD in Jos, Nigeria [ 19 ]. Researchers from an Irish study on the Irish SCD population reported that the smartphone app was expressed by the majority, with daily medication reminders being the most popular feature [ 11 ].
The suggested recommendations by participants are like interventions already in play in other public health programs such as comprehensive HIV treatment and care programs [ 20 ]. Such programs include social economic empowerment activities that equip them with skills for independent income generating for the sustenance of basic care. This allows patients to afford complementary medication, and nutrition and facilitates adherence to clinic appointments [ 21 ]. Such can be adapted into the SCD management program to offset challenges related to finances. With financial empowerment, all the other correlated challenges will be lessened.
Patients recognize the importance of medical information in advancing compliance with treatment. Programs geared towards increasing healthcare knowledge on novel SCD treatments like HU should be promoted. This will trickle down to more quality medication counseling provided to patients which will then lead to medication compliance. Expert patients could be trained to be peer influencers, by equipping them with information, educational, and communication material necessary to empower fellow patients psychosocially. This strategy has been successfully implemented in other public health challenges e.g., HIV and TB [ 22 ].
Other recommendations were health facility-based and these included; Healthcare workers should advise and encourage patients to adhere to sickle cell medication, There should be free drugs availed at the health facilities, Health managers should ensure consistent and sufficient drug supply, Health care workers should create awareness to patients about benefits of sickle cell treatment, Health care workers should offer continuous advice, health education to patients, Health care facilitates should plan to offer transport refund to sickle cell patients, Health facilities should allow credit options for patients who lack funds to buy drugs.
Community-based recommendations included the extension of sickle cell health services to the communities and local districts should be done to resolve the issue of transport, and Sensitization of patients and community people about Hydroxyurea.
Task shifting in terms of personnel and medication is necessary for grassroots accessibility. Such models have been implemented to improve life-saving therapy like ART for HIV-infected patients and disseminated drug delivery models [ 23 ].
National-based recommendations included the government reducing the price of sickle cell medicine to enhance access for all patients, the Government putting up sickle cell health facilities in rural areas, and there is need for a collaborative partnership with international or non-governmental organizations to support sickle cell patients.
Study limitations
This study was carried out at national referral hospitals which have a better supply of medicines and health care experts in the management of SCD, this created selective bias because the quality of care is not generalizable to other health centers in the country. Future research directions should include national surveys to understand the magnitude of the barriers to better government planning in the allocation of resources.
Because of the Cross-sectional nature, of the quantitative section, we were not able to determine causation but could only determine the association between HU use and patient-related barriers to HU use.
Study strengths
The study was conducted at two national referral hospitals that are in the central region of Uganda. This region has one of the highest prevalence of SCD The central region of Uganda is metropolitan with individuals coming in from different parts of Uganda so the SCD population may be representative. The findings of this study are therefore representative of the sickle cell population in Kampala which is the capital city of Uganda.
This is a mixed-method study, so the qualitative aspects of the study helped to explain the results of the quantitative findings. For example, in this study, we now know that lack of affordability is the reason why most patients have never been on HU even if it is indicated or stop using it when they need it.
Implementing the use of HU has been challenging in Uganda and needs improvement. Facilitators to hydroxyurea use have been highlighted, though Patient-identified barriers at individual, facility, and community levels that need to be resolved. The experiences and insights shared by our participants provide invaluable guidance for increasing the uptake of HU. Further studies are needed to establish validated instruments to assess patients’ pain communication and adherence to the HU regimen. The prevalence of HU use among eligible patients is high at 78%.
Data availability
The datasets used and/or analyzed during the current study are available at https://github.com/PNamaganda/Sickle-cell-Data-in-Uganda. Deidentified data and analyzed data for this manuscript are available from the corresponding author upon request.
Modell B, Darlison M. Global epidemiology of hemoglobin disorders and derived service indicators. Bull World Health Organ. 2008;86:480–7.
Article PubMed PubMed Central Google Scholar
Lanzkron S, Carroll CP, Haywood C Jr. Mortality rates and age at death from sickle cell disease: U.S., 1979–2005. Public Health Rep. 2013;128(2):110–6.
Lanzkron S, Strouse JJ, Wilson R, Beach MC, Haywood C, Park H, Segal JB. Systematic review: Hydroxyurea for the treatment of adults with sickle cell disease. Ann Intern Med. 2008;148(12):939–55.
Opoka RO, Ndugwa CM, Latham TS, Lane A, Hume HA, Kasirye P, et al. Novel use of Hydroxyurea in an African Region with Malaria (NOHARM): a trial for children with sickle cell anemia. Blood. 2017;130:2585–93.
Article CAS PubMed Google Scholar
Tshilolo L, Tomlinson G, Williams TN, Santos B, Olupot-Olupot P, Lane A et al. Hydroxyurea for children with sickle cell anemia in sub-saharan Africa. N Engl J Med. 2019; 380:121 – 31.6.
Olupot-Olupot P, Wabwire H, Ndila C, Adong R, Ochen L, Amorut D, ... & Williams, TN. Characterizing demographics, knowledge, practices, and clinical care among patients attending sickle cell disease clinics in Eastern Uganda. Wellcome Open Res. 2020. https://www.health.go.ug/2019/12/02/use-of-hydroxyurea-approved-for-sickle-cell-patients/ .
Brandow AM, Panepinto JA. Hydroxyurea use in sickle cell disease: the battle with low prescription rates, poor patient compliance and fears of toxicities. Expert Rev Hematol. 2010;3(3):255–60. https://doi.org/10.1586/ehm.10.22 .
Article CAS PubMed PubMed Central Google Scholar
Robinson JH, Callister LC, Berry JA, Dearing KA. Patient-centered care and adherence: definitions and applications to improve outcomes. J Am Acad Nurse Pract. 2008;20(12):600–7.
Article PubMed Google Scholar
Kang HA, Barner JC, Lawson KA, Rascati K, Mignacca RC. Impact of adherence to hydroxyurea on health outcomes among patients with sickle cell disease. Am J Hematol. 2023;98(1):90–101.
10, Jose J, Elsadek RA, Jimmy B, George P, Hydroxyurea. Pattern of Use, Patient Adherence, and Safety Profile in patients with Sickle Cell Disease in Oman. Oman Med J. 2019;34(4):327–35. https://doi.org/10.5001/omj.2019.64 . PMID: 31360322; PMCID: PMC6642718.
Article Google Scholar
Fogarty H, Gaul A, Syed S, et al. Adherence to hydroxyurea, health-related quality of life domains, and attitudes towards a smartphone app among Irish adolescents and young adults with sickle cell disease. Ir J Med Sci. 2022;191:809–16. https://doi.org/10.1007/s11845-021-02588-1) .
Aliyu ZY, Babadoko A, Mamman A. Hydroxyurea utilization in Nigeria, a Lesson in Public Health. Blood. 2007;110(11):80.
Okocha EC, Gyamfi J, Ryan N, Babalola O, Etuk EA, Chianumba R, Nwegbu M, Isa H, Madu AJ, Adegoke S, Nnebe-Agumandu U, Brown B, Peprah E, Nnodu OE. Barriers to therapeutic use of Hydroxyurea for Sickle Cell Disease in Nigeria: a cross-sectional survey. Front Genet. 2022;12:765958. https://doi.org/10.3389/fgene.2021.765958 . PMID: 35126450; PMCID: PMC8807646).
Badawy SM, Thompson AA, Penedo FJ, Lai JS, Rychlik K, Liem RI. Barriers to hydroxyurea adherence and health-related quality of life in adolescents and young adults with sickle cell disease. Eur J Hematol. 2017;98(6):608–14.
Article CAS Google Scholar
Adeyemo TA, Diaku-Akinwunmi IN, Ojewunmi OO, Bolarinwa AB, Adekile AD. Barriers to the use of hydroxyurea in the management of sickle cell disease in Nigeria. Hemoglobin. 2019;43(3):188–92. Epub 2019 Aug 29. PMID: 31462098).
Treadwell MJ, Du L, Bhasin N, Marsh AM, Wun T, Bender MA, Nugent D. Barriers to hydroxyurea use from the perspectives of providers, individuals with sickle cell disease, and families: report from a US regional collaborative. Front Genet. 2022;13:921432.
Foo KM, Sundram M, Legido-Quigley H. Facilitators, and barriers of managing patients with multiple chronic conditions in the community: a qualitative study. BMC Public Health. 2020;20:273. https://doi.org/10.1186/s12889-020-8375-8) .
Adimora I, Akingbola TS, Lansigan F, van Hoff J. Pharmacotherapy interventions and barriers to treatment of Sickle Cell Disease in Ibadan, Nigeria. Blood. 2018;132:3523.
Ofakunrin AOD, Adekola K, Okpe ES, Oguche S, Afolaranmi T, Kanhu P, Sagay AS. Level of utilization and provider-related barriers to hydroxyurea use in the treatment of sickle cell disease in Jos. Nigeria Blood. 2019;134:1029.
Ford N, Ball A, Baggaley R, Vitoria M, Low-Beer D, Penazzato M, Hirnschall G. The WHO public health approach to HIV treatment and care: looking back and looking ahead. Lancet Infect Dis. 2018;18(3):e76–86.
Kennedy CE, Fonner VA, O’Reilly KR, Sweat MD. A systematic review of income generation interventions, including microfinance and vocational skills training, for HIV prevention. AIDS Care. 2014;26(6):659–73. Epub 2013 Oct 9. PMID: 24107189; PMCID: PMC3943565.
Medley A, Kennedy C, O’Reilly K, Sweat M. Effectiveness of peer education interventions for HIV prevention in developing countries: a systematic review and meta-analysis. AIDS Educ Prev. 2009;21(3):181–206. https://doi.org/10.1521/aeap.2009.21.3.181 . PMID: 19519235; PMCID: PMC3927325.
Fulton BD, Scheffler RM, Sparkes SP, et al. Health workforce skill mix and task shifting in low-income countries: a review of recent evidence. Hum Resource Health. 2011;9:1. https://doi.org/10.1186/1478-4491-9-1 .
Download references
Acknowledgements
We acknowledge the patients of Mulago Hospital SCD clinic and Kiruddu Hospital who gave us consent to obtain this information.
This study was funded with funds from Novartis Pharmaceuticals. The funding project had no role in the design of the study and collection, analysis, and interpretation of data and no role in writing the manuscript.
Author information
Authors and affiliations.
Kiruddu National Referral Hospital, P.O. Box 6553, Kampala, Uganda
Priscilla Namaganda
Infectious Disease Institute, Makerere University, Kampala, Uganda
Patience Nantume, Adelliine Twimukye & Christine Sekaggya Wiltshire
Uganda Cancer Institute, Kampala, Uganda
Kelvin Roland Mubiru
You can also search for this author in PubMed Google Scholar
Contributions
PN– conception, design of work, acquisition, analysis, interpretation of data, drafted and substantively revised the manuscript, PN– data collection, data entry, data cleaning KM – Quantitative data analysis. AT– Qualitative data analysis, CS- design of work, acquisition, analysis, interpretation of data, drafted and substantively revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Priscilla Namaganda .
Ethics declarations
Ethics approval and consent to participate.
Written informed consent/ assent was obtained from all participants or their parent/guardian or legally authorized representative to participate in the study. Ethical approval was obtained from the Infectious Disease Institute Research Ethic Committee, IDIREC REF 037/2021. All methods and procedures were carried out in accordance with relevant guidelines and regulations.
Consent for publication
Not applicable
Human protection
All data collection methods and analysis were carried out in accordance with relevant Good clinical care practice (GCP) guidelines and regulations.
Conflict of interest
The authors declare that they have no competing interests. The findings and conclusions in this report are those of the author(s) and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Namaganda, P., Nantume, P., Mubiru, K.R. et al. Understanding patient-related barriers to hydroxyurea use among adolescent and adult patients with sickle cell disease in Mulago and Kiruddu hospitals, Uganda, a qualitative study. BMC Health Serv Res 24 , 666 (2024). https://doi.org/10.1186/s12913-024-11125-6
Download citation
Received : 24 November 2023
Accepted : 20 May 2024
Published : 27 May 2024
DOI : https://doi.org/10.1186/s12913-024-11125-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Sickle cell disease
- Hydroxyurea
- Patient-related barriers.
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
Have a language expert improve your writing
Run a free plagiarism check in 10 minutes, automatically generate references for free.
- Knowledge Base
- Dissertation
- How to Write an Abstract | Steps & Examples
How to Write an Abstract | Steps & Examples
Published on 1 March 2019 by Shona McCombes . Revised on 10 October 2022 by Eoghan Ryan.
An abstract is a short summary of a longer work (such as a dissertation or research paper ). The abstract concisely reports the aims and outcomes of your research, so that readers know exactly what your paper is about.
Although the structure may vary slightly depending on your discipline, your abstract should describe the purpose of your work, the methods you’ve used, and the conclusions you’ve drawn.
One common way to structure your abstract is to use the IMRaD structure. This stands for:
- Introduction
Abstracts are usually around 100–300 words, but there’s often a strict word limit, so make sure to check the relevant requirements.
In a dissertation or thesis , include the abstract on a separate page, after the title page and acknowledgements but before the table of contents .
Instantly correct all language mistakes in your text
Be assured that you'll submit flawless writing. Upload your document to correct all your mistakes.

Table of contents
Abstract example, when to write an abstract, step 1: introduction, step 2: methods, step 3: results, step 4: discussion, tips for writing an abstract, frequently asked questions about abstracts.
Hover over the different parts of the abstract to see how it is constructed.
This paper examines the role of silent movies as a mode of shared experience in the UK during the early twentieth century. At this time, high immigration rates resulted in a significant percentage of non-English-speaking citizens. These immigrants faced numerous economic and social obstacles, including exclusion from public entertainment and modes of discourse (newspapers, theater, radio).
Incorporating evidence from reviews, personal correspondence, and diaries, this study demonstrates that silent films were an affordable and inclusive source of entertainment. It argues for the accessible economic and representational nature of early cinema. These concerns are particularly evident in the low price of admission and in the democratic nature of the actors’ exaggerated gestures, which allowed the plots and action to be easily grasped by a diverse audience despite language barriers.
Keywords: silent movies, immigration, public discourse, entertainment, early cinema, language barriers.
Prevent plagiarism, run a free check.
You will almost always have to include an abstract when:
- Completing a thesis or dissertation
- Submitting a research paper to an academic journal
- Writing a book proposal
- Applying for research grants
It’s easiest to write your abstract last, because it’s a summary of the work you’ve already done. Your abstract should:
- Be a self-contained text, not an excerpt from your paper
- Be fully understandable on its own
- Reflect the structure of your larger work
Start by clearly defining the purpose of your research. What practical or theoretical problem does the research respond to, or what research question did you aim to answer?
You can include some brief context on the social or academic relevance of your topic, but don’t go into detailed background information. If your abstract uses specialised terms that would be unfamiliar to the average academic reader or that have various different meanings, give a concise definition.
After identifying the problem, state the objective of your research. Use verbs like “investigate,” “test,” “analyse,” or “evaluate” to describe exactly what you set out to do.
This part of the abstract can be written in the present or past simple tense but should never refer to the future, as the research is already complete.
- This study will investigate the relationship between coffee consumption and productivity.
- This study investigates the relationship between coffee consumption and productivity.
Next, indicate the research methods that you used to answer your question. This part should be a straightforward description of what you did in one or two sentences. It is usually written in the past simple tense, as it refers to completed actions.
- Structured interviews will be conducted with 25 participants.
- Structured interviews were conducted with 25 participants.
Don’t evaluate validity or obstacles here — the goal is not to give an account of the methodology’s strengths and weaknesses, but to give the reader a quick insight into the overall approach and procedures you used.
The only proofreading tool specialized in correcting academic writing
The academic proofreading tool has been trained on 1000s of academic texts and by native English editors. Making it the most accurate and reliable proofreading tool for students.

Correct my document today
Next, summarise the main research results . This part of the abstract can be in the present or past simple tense.
- Our analysis has shown a strong correlation between coffee consumption and productivity.
- Our analysis shows a strong correlation between coffee consumption and productivity.
- Our analysis showed a strong correlation between coffee consumption and productivity.
Depending on how long and complex your research is, you may not be able to include all results here. Try to highlight only the most important findings that will allow the reader to understand your conclusions.
Finally, you should discuss the main conclusions of your research : what is your answer to the problem or question? The reader should finish with a clear understanding of the central point that your research has proved or argued. Conclusions are usually written in the present simple tense.
- We concluded that coffee consumption increases productivity.
- We conclude that coffee consumption increases productivity.
If there are important limitations to your research (for example, related to your sample size or methods), you should mention them briefly in the abstract. This allows the reader to accurately assess the credibility and generalisability of your research.
If your aim was to solve a practical problem, your discussion might include recommendations for implementation. If relevant, you can briefly make suggestions for further research.
If your paper will be published, you might have to add a list of keywords at the end of the abstract. These keywords should reference the most important elements of the research to help potential readers find your paper during their own literature searches.
Be aware that some publication manuals, such as APA Style , have specific formatting requirements for these keywords.
It can be a real challenge to condense your whole work into just a couple of hundred words, but the abstract will be the first (and sometimes only) part that people read, so it’s important to get it right. These strategies can help you get started.
Read other abstracts
The best way to learn the conventions of writing an abstract in your discipline is to read other people’s. You probably already read lots of journal article abstracts while conducting your literature review —try using them as a framework for structure and style.
You can also find lots of dissertation abstract examples in thesis and dissertation databases .
Reverse outline
Not all abstracts will contain precisely the same elements. For longer works, you can write your abstract through a process of reverse outlining.
For each chapter or section, list keywords and draft one to two sentences that summarise the central point or argument. This will give you a framework of your abstract’s structure. Next, revise the sentences to make connections and show how the argument develops.
Write clearly and concisely
A good abstract is short but impactful, so make sure every word counts. Each sentence should clearly communicate one main point.
To keep your abstract or summary short and clear:
- Avoid passive sentences: Passive constructions are often unnecessarily long. You can easily make them shorter and clearer by using the active voice.
- Avoid long sentences: Substitute longer expressions for concise expressions or single words (e.g., “In order to” for “To”).
- Avoid obscure jargon: The abstract should be understandable to readers who are not familiar with your topic.
- Avoid repetition and filler words: Replace nouns with pronouns when possible and eliminate unnecessary words.
- Avoid detailed descriptions: An abstract is not expected to provide detailed definitions, background information, or discussions of other scholars’ work. Instead, include this information in the body of your thesis or paper.
If you’re struggling to edit down to the required length, you can get help from expert editors with Scribbr’s professional proofreading services .
Check your formatting
If you are writing a thesis or dissertation or submitting to a journal, there are often specific formatting requirements for the abstract—make sure to check the guidelines and format your work correctly. For APA research papers you can follow the APA abstract format .
Checklist: Abstract
The word count is within the required length, or a maximum of one page.
The abstract appears after the title page and acknowledgements and before the table of contents .
I have clearly stated my research problem and objectives.
I have briefly described my methodology .
I have summarized the most important results .
I have stated my main conclusions .
I have mentioned any important limitations and recommendations.
The abstract can be understood by someone without prior knowledge of the topic.
You've written a great abstract! Use the other checklists to continue improving your thesis or dissertation.
An abstract is a concise summary of an academic text (such as a journal article or dissertation ). It serves two main purposes:
- To help potential readers determine the relevance of your paper for their own research.
- To communicate your key findings to those who don’t have time to read the whole paper.
Abstracts are often indexed along with keywords on academic databases, so they make your work more easily findable. Since the abstract is the first thing any reader sees, it’s important that it clearly and accurately summarises the contents of your paper.
An abstract for a thesis or dissertation is usually around 150–300 words. There’s often a strict word limit, so make sure to check your university’s requirements.
The abstract is the very last thing you write. You should only write it after your research is complete, so that you can accurately summarize the entirety of your thesis or paper.
Avoid citing sources in your abstract . There are two reasons for this:
- The abstract should focus on your original research, not on the work of others.
- The abstract should be self-contained and fully understandable without reference to other sources.
There are some circumstances where you might need to mention other sources in an abstract: for example, if your research responds directly to another study or focuses on the work of a single theorist. In general, though, don’t include citations unless absolutely necessary.
The abstract appears on its own page, after the title page and acknowledgements but before the table of contents .
Cite this Scribbr article
If you want to cite this source, you can copy and paste the citation or click the ‘Cite this Scribbr article’ button to automatically add the citation to our free Reference Generator.
McCombes, S. (2022, October 10). How to Write an Abstract | Steps & Examples. Scribbr. Retrieved 7 June 2024, from https://www.scribbr.co.uk/thesis-dissertation/abstract/
Is this article helpful?
Shona McCombes
Other students also liked, how to write a thesis or dissertation introduction, thesis & dissertation acknowledgements | tips & examples, dissertation title page.

IMAGES
VIDEO
COMMENTS
Qualitative Research Abstracts Authors Joan Ostaszkiewicz, PhD, RN, MNurs Donna Z. Bliss, PhD, RN, FGSA, FAAN ... Table 1 provides examples of the types of research question that could be addressed using these different approaches. Sample sizes in qualitative research are typically small (10-20 subjects), and the participants or sites ...
Step 2: Methods. Next, indicate the research methods that you used to answer your question. This part should be a straightforward description of what you did in one or two sentences. It is usually written in the past simple tense, as it refers to completed actions.
This example showcases how to write an abstract for a qualitative study. Qualitative studies also have clearly defined research methods. Therefore, it is important to keep in mind the general principles of informative abstract writing. ... but it does let the reader know what the overall subject matter was and the methods used to conduct the ...
Research Paper Abstract Examples could be following: Example 1: ... A Qualitative Study" Abstract: This qualitative study explores the role of parental involvement in children's education. Through in-depth interviews with 20 parents of children in elementary school, we found that parental involvement takes many forms, including volunteering ...
General guidance. Authors should refer to the general information and guidelines contained in the Society's "Guidance for Submission of Abstracts". The general guidance therein applies to qualitative research abstracts. This includes the maximum permitted limit of 250 words, and the instruction that abstracts should be structured.
Cite. Ajit Singh. Writing an abstract for a qualitative research study involves summarizing the key aspects of the study in a concise and informative manner. Here is a sample abstract: Title ...
aspects of reporting that are unique to qualitative research. They describe the general elements that should be reported in qualitative papers and can assist authors in devel-oping comprehensive reports that will support their review. Guidance is provided for how to best present qualitative research, with rationales and illustrations.
The book aims at achieving e ects in three domains: (a) the. personal, (b) the scholarly, and (c) the practical. The personal goal. is to demystify qualitative methods, give readers a feel for ...
Cochrane Abstracts: a guide to style and content 4 In each section of the abstract, standard words and phrases should be used as much as possible. This will ensure that is easier to translate abstracts accurately. A specific phrase or word can be translated in a way that has been agreed by native language speakers.
Qualitative Research Abstract Sample. Background Heart failure affects nearly 6-million Americans and is associated with frequent and costly acute care hospitalizations. Although current guidelines emphasize the importance of implementing systems to coordinate and deliver effective care, hospital readmission rates in the heart failure ...
The sample of the research consisted of 98 doctoral dissertations. Document analysis, a qualitative research method, was employed in the research. According to the findings of the research, most ...
Abstract . Qualitative research is experiencing a resurgence within the field of psychology. This study aimed to explore the range of attitudes toward qualitative research in psychology held by students and academics, using the model of attitudes by Eagly and Chaiken (1993; 2007) as a framework.
In the research methodology section, it is essential to mention the kind of research you conducted; for instance, qualitative research or quantitative research ... Be sure that your statements reflect the actual results and the methods you used to conduct your research. Good Abstract Examples Abstract Example #1.
Denise Blanchard, University of Wollongong Sharon Bourgeois, University of Wollongong Katherine Nelson, Victoria University of Wellington. Qualitative methods may be boundless and may push boundaries. At the end of the day, methods progress research. This includes accounting for participants taking part in the research.
Abstract. Qualitative content analysis and other 'standardised' methods are sometimes considered to be technical tools used for basic, superficial, and simple sorting of text, and their results lack depth, scientific rigour, and evidence. To strengthen the trustworthiness of qualitative content analyses, we focus on abstraction and ...
A qualitative approach was employed using in-depth interviewing with a purposive sample ( N = 30, 17 male, 13 female) of currently abstinent drug abusers and health professionals from the three rehabilitation centers in Tehran. Data analysis was conducted by using the constant comparative method.
A purposive sample of 19 patients were interviewed and transcripts were analyzed using an interpretative, hermeneutic method. ... All titles and abstracts were assessed for inclusion criteria and 62 articles were selected for full-text reading. ... Qualitative research provides an important perspective for evidence-based decision makers in ...
Abstracts, Oral Presentations for Qualitative Methods Conference, May 2016 Doing Collaborative Research: The Good, the Bad, and the Politics ... approaches to using critical incidents in research will be pro-vided. Next, an example of a study in professional education will be highlighted. Examples of critical incidents show how
The qualitative nature of this study reveals insights into teaching and learning through its focus on emerging themes and patterns that developed over time. Methods used included participation-observation; collection of field notes and documents; administration of a pre/post-survey; interviews with teacher and students; and analysis of analytic ...
Definition and Purpose of Abstracts An abstract is a short summary of your (published or unpublished) research paper, usually about a paragraph (c. 6-7 sentences, 150-250 words) long. A well-written abstract serves multiple purposes: an abstract lets readers get the gist or essence of your paper or article quickly, in order to decide whether to….
Locating Methods Examples. Find Dissertations that Cite a Core Methods Work. You can conduct a cited reference search in the ProQuest Dissertations & Theses database. ... qualitative data, qualitative data analysis, qualitative research, taguette. Main Library Information Desk (217) 333 -2290. 1408 W. Gregory Dr. Urbana, IL 61801. Make a Gift ...
This article describes how to make use of exemplar vignettes in qualitative medial education research. Vignettes are particularly useful in prompting discussion with participants, when using real-life case examples may breach confidentiality. As such, using vignettes allows researchers to gain insight into participants' thinking in an ethically sensitive way.
The aims and design of the study. This qualitative study was based on Thorne's interpretive descriptive approach [] and was part of the Flemish Employees' Physical Activity study [].Thorne's interpretive descriptive approach embraces the concept that reality is shaped by social constructs, acknowledging the existence of diverse constructed realities [].
1. Qualitative research is a method of inquiry that develops understanding on human. and social sciences to find the way p eople think. 2. Qualitative research is holistic in nature; this is ...
An abstract summarizes, usually in one paragraph of 300 words or less, the major aspects of the entire paper in a prescribed sequence that includes: 1) the overall purpose of the study and the research problem(s) you investigated; 2) the basic design of the study; 3) major findings or trends found as a result of your analysis; and, 4) a brief summary of your interpretations and conclusions.
Abstract. Background. ... We purposively selected 40 participants to participate in the qualitative interviews. The actual sample size (40) was determined by how many participants were required to explore all the research questions and to achieve thematic saturation. It was difficult to determine the ideal sample size for achieving these ...
How to Write an Abstract | Steps & Examples. Published on 1 March 2019 by Shona McCombes.Revised on 10 October 2022 by Eoghan Ryan. An abstract is a short summary of a longer work (such as a dissertation or research paper).The abstract concisely reports the aims and outcomes of your research, so that readers know exactly what your paper is about.
In their classic accounts, anthropological ethnographers developed causal arguments for how specific sociocultural structures and processes shaped human thought, behavior, and experience in particular settings. Despite this history, many contemporary ethnographers avoid establishing in their work direct causal relationships between key variables in the way that, for example, quantitative ...