An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager

Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Poverty and Health Disparities: What Can Public Health Professionals Do?
Affiliations.
- 1 1 University of Toledo, Toledo, OH, USA.
- 2 2 Ball State University, Muncie, IN, USA.
- 3 3 University of Florida College of Medicine, Jacksonville, FL, USA.
- PMID: 29363333
- DOI: 10.1177/1524839918755143
More than a tenth of the U.S. population (13% = 41 million people) is currently living in poverty. In this population, the socioeconomic, cultural, and environmental conditions have detrimental health effects such as higher rates of chronic diseases, communicable illnesses, health risk behaviors, and premature mortality. People living in poverty are also deprived of social, psychological, and political power, leading to continuation of worsening health and chronic deprivation over generations. The health of individuals living in poverty poses greater challenges from policy, practice, and research standpoints. Public health professionals are poised uniquely to be advocates for the marginalized, be the resource persons for health education, implement health promotion programs, and conduct research to understand health effects of poverty and design tailored and targeted public health interventions. In this article, we summarize the opportunities for public health practice with individuals living in poverty.
Keywords: health disparities; poverty; public health policies; social determinants of health; social policy.
PubMed Disclaimer
Similar articles
- Structural approaches to health promotion: what do we need to know about policy and environmental change? Lieberman L, Golden SD, Earp JA. Lieberman L, et al. Health Educ Behav. 2013 Oct;40(5):520-5. doi: 10.1177/1090198113503342. Health Educ Behav. 2013. PMID: 24048612
- Shaping public policy and population health in the United States: why is the public health community missing in action? Raphael D. Raphael D. Int J Health Serv. 2008;38(1):63-94. doi: 10.2190/HS.38.1.d. Int J Health Serv. 2008. PMID: 18341123
- Reducing Premature Mortality in the Mentally Ill Through Health Promotion Programs. Price JH, Khubchandani J, Price JA, Whaley C, Bowman S. Price JH, et al. Health Promot Pract. 2016 Sep;17(5):617-22. doi: 10.1177/1524839916656146. Epub 2016 Jun 14. Health Promot Pract. 2016. PMID: 27307394
- A Critical Exploration of Migraine as a Health Disparity: the Imperative of an Equity-Oriented, Intersectional Approach. Befus DR, Irby MB, Coeytaux RR, Penzien DB. Befus DR, et al. Curr Pain Headache Rep. 2018 Oct 5;22(12):79. doi: 10.1007/s11916-018-0731-3. Curr Pain Headache Rep. 2018. PMID: 30291549 Review.
- Disparities in health, poverty, incarceration, and social justice among racial groups in the United States: a critical review of evidence of close links with neoliberalism. Nkansah-Amankra S, Agbanu SK, Miller RJ. Nkansah-Amankra S, et al. Int J Health Serv. 2013;43(2):217-40. doi: 10.2190/HS.43.2.c. Int J Health Serv. 2013. PMID: 23821903 Review.
- Miracle friends and miracle money in California: a mixed-methods experiment of social support and guaranteed income for people experiencing homelessness. Henwood BF, Kim BE, Stein A, Corletto G, Suthar H, Adler KF, Mazzocchi M, Ip J, Padgett DK. Henwood BF, et al. Trials. 2024 Apr 29;25(1):290. doi: 10.1186/s13063-024-08109-6. Trials. 2024. PMID: 38685123 Free PMC article.
- Self-reported Impacts of the COVID-19 Pandemic and Economic Inflation on the Well-being of Low-income U.S. Veterans. Tsai J, Hird R, Collier A. Tsai J, et al. J Community Health. 2023 Dec;48(6):970-974. doi: 10.1007/s10900-023-01267-9. Epub 2023 Aug 21. J Community Health. 2023. PMID: 37605100
- Diversity in maintaining health of populations. Nsibandze BS. Nsibandze BS. Health SA. 2022 Dec 13;27:2137. doi: 10.4102/hsag.v27i0.2137. eCollection 2022. Health SA. 2022. PMID: 36570092 Free PMC article. No abstract available.
- Chasing the Youth Dividend in Nigeria, Malawi and South Africa: What Is the Role of Poverty in Determining the Health and Health Seeking Behaviour of Young Women? Mkwananzi S, Baruwa OJ. Mkwananzi S, et al. Int J Environ Res Public Health. 2022 Oct 30;19(21):14189. doi: 10.3390/ijerph192114189. Int J Environ Res Public Health. 2022. PMID: 36361068 Free PMC article.
- Perceptions of Barriers: An Examination of Public Health Practice in Kansas. Eppler M, Brock K, Brunkow C, Mulcahy ER. Eppler M, et al. Int J Environ Res Public Health. 2022 May 1;19(9):5513. doi: 10.3390/ijerph19095513. Int J Environ Res Public Health. 2022. PMID: 35564905 Free PMC article.
- Search in MeSH
Related information
Linkout - more resources, full text sources.
- Ovid Technologies, Inc.
Other Literature Sources
- scite Smart Citations
- MedlinePlus Health Information

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- BMJ Journals
You are here
- Volume 59, Issue 4
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- Center for Research on Population and Health, American University of Beirut, Beirut, Lebanon
- Correspondence to: Dr M Khawaja Center for Research on Population and Health, American University of Beirut, Beirut 1107 2020, Lebanon; mk36aub.edu.lb
This glossary addresses the complex nature of poverty and raises some conceptual and measurement issues related to poverty in the public health literature, with a focus on poor countries.
- community health
- social exclusion
https://doi.org/10.1136/jech.2004.022822
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Linked Articles
- In this issue Is epidemiology popular enough? Carlos Alvarez-Dardet John R Ashton Journal of Epidemiology & Community Health 2005; 59 253-253 Published Online First: 14 Mar 2005.
Read the full text or download the PDF:
Select Your Interests
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
- Download PDF
- Share X Facebook Email LinkedIn
- Permissions
Income, Poverty, and Health Inequality
- 1 Chief population health officer of New York City Health + Hospitals, and clinical associate professor of population health and medicine at the New York University School of Medicine
The health of people with low incomes historically has been a driver of public health advances in the United States. For example, in New York City, cholera deaths during outbreaks in 1832 and 1854 concentrated among the poor helped push forward the Metropolitan Health Law, which allowed for regulation of sanitary conditions in the city. The law was an exemplar for other municipalities across the United States, saving countless lives during subsequent cholera epidemics as well as from typhus, dysentery, and smallpox.
Health inequality persists today, though our public health response—our modern Metropolitan Health Laws—must address more insidious causes and conditions of illness. There is a robust literature linking income inequality to health disparities —and thus widening income inequality is cause for concern. US Census data show a steady increase in summary measures of income inequality over the past 50 years. The association between income and life expectancy, already well established, was detailed in a landmark 2016 JAMA study by Raj Chetty, PhD, of Stanford University, and colleagues. This study found a gap in life expectancy of about 15 years for men and 10 years for women when comparing the most affluent 1% of individuals with the poorest 1%. To put this into perspective, the 10-year life expectancy difference for women is equal to the decrement in longevity from a lifetime of smoking.
Probing the Income-Health Relationship
In an editorial that accompanied the article by Chetty et al, Angus Deaton, PhD, of Princeton University, commented on the study’s geographical findings: “It is as if the top income percentiles belong to one world of elite, wealthy US adults, whereas the bottom income percentiles each belong to separate worlds of poverty, each unhappy and unhealthy in its own way.” Prior research had tried to identify these separate worlds, describing “ Eight Americas ” defined by sociodemographic characteristics, such as low-income white people in Appalachia and the Mississippi Valley, Western Native Americans, and Southern low-income rural black people. To improve health, interventions may need to account for starkly different lived experiences across different geographic contexts.
Educational attainment, sex, and race interact with and complicate the income-health relationship. Two additional dimensions add complexity: thinking beyond income to wealth and thinking beyond mortality to morbidity. Wealth refers to the total value of assets (and debts) possessed by an individual, not just the flow of money defined as income. Wealth is even more unequally divided than income : while the top 10% of the income distribution received a little more than half of all income, the top 10% of the wealth distribution held more than three-quarters of all wealth. This matters because it is one way that inequities persist over time —through, for instance, legacy effects of Jim Crow laws or discriminatory housing policy that affect family wealth and health over generations .
Studies on inequality and mortality may garner the most attention, but disparities in morbidity and quality of life are also evident. Low-income adults are more than 3 times as likely to have limitations with routine activities (like eating, bathing, and dressing) due to chronic illness, compared with more affluent individuals. Children living in poverty are more likely to have risk factors such as obesity and elevated blood lead levels, affecting their future health prospects.
Inequality or Inequity?
Is it the role of physicians and other health professionals to address poverty? Is it a “modifiable” risk factor, or should we focus on more proximate causes of illness, such as health behaviors? Our answers to these questions determine whether wealth gradients lead only to health inequality—or whether they contribute to health inequity , which is inequality that is avoidable and unfair.
Two arguments favor paying attention to income and wealth distributions as part of advancing health equity. First, health care spending—the realm of medical professionals—can worsen income inequality, at both individual and systemic levels. Individually, poor people have to spend a much greater proportion of their income on health care than richer people do. In 2014, medical outlays lowered the median income for the poorest decile of US individuals by 47.6% vs 2.7% for the wealthiest decile. Systemically, medical spending can crowd out other government spending on social services , drawing resources away from education and environmental improvement, for example. Taken together, this supports the case that “first do no harm” must extend to the financial impact of delivering health care. Clinicians who care about the social determinants of health must also pay heed to the cost (and opportunity cost) of health care.
Second, we are in a period when declines in key public health indicators may be wrought by policies that ostensibly have little to do with health—such as tax policy. The Centers for Disease Control and Prevention reported that average life expectancy decreased for the second year in a row in 2016. But mean mortality changes may obscure the full picture , which is more about increasing mortality being concentrated in lower-income groups. Meanwhile, the recent Tax Cuts and Jobs Act is likely to exacerbate income inequality. This is particularly true if the tax cuts trigger cuts in government spending , as Republican leaders have signaled. Medicaid and the Supplemental Nutrition Assistance Program (SNAP, also known as food stamps) are 2 programs for low-income individuals that are likely to be targeted for cuts. Even if Medicare and Social Security are spared, life expectancy differences by income means that more affluent US adults can expect to claim those benefits over a longer lifespan.
What would be today’s analog to the Metropolitan Health Law of 1866? Addressing the root causes of health inequity requires interrupting the vicious cycle of poverty leading to illness leading to poverty—what Jacob Bor, ScD, and Sandro Galea, MD, of Boston University School of Health, have termed a “21st century health-poverty trap.” Although there are many root causes to address, perhaps the place to begin is the health of children. For instance, economic policy like the Earned Income Tax Credit has been associated with decreases in low birth weight.
Congress’ recent reauthorization of the Children’s Health Insurance Program offers a glimmer of hope for such bipartisan paths toward health equity nationally. Focusing on resources to support children—such as nurse home visits to pregnant women, prekindergarten programs, and adolescent mental health care— can directly improve health while influencing intergenerational economic mobility. The city of Philadelphia offers a concrete example of how to do this: a tax on sugary drinks was used to fund prekindergarten, social services in neighborhood schools, and parks and libraries. In this way, health might lead to economic opportunity, leading to better health.
Corresponding Author: Dave A. Chokshi, MD, MSc ( [email protected] ).
Published Online: February 21, 2018, at https://newsatjama.jama.com/category/the-jama-forum/ .
Disclaimer: Each entry in The JAMA Forum expresses the opinions of the author but does not necessarily reflect the views or opinions of JAMA, the editorial staff, or the American Medical Association.
Additional Information: Information about The JAMA Forum, including disclosures of potential conflicts of interest, is available at https://newsatjama.jama.com/about/ .
Note: Source references are available through embedded hyperlinks in the article text online.
See More About
Chokshi DA. Income, Poverty, and Health Inequality. JAMA. 2018;319(13):1312–1313. doi:10.1001/jama.2018.2521
Manage citations:
© 2024
Artificial Intelligence Resource Center
Cardiology in JAMA : Read the Latest
Browse and subscribe to JAMA Network podcasts!
Others Also Liked
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
Advertisement
Climate change, poverty and child health inequality: evidence from Vietnam’s provincial analysis
- Published: 09 September 2024
- Volume 57 , article number 163 , ( 2024 )
Cite this article

- Cong Minh Huynh ORCID: orcid.org/0000-0001-8169-5665 1 &
- Bao Khuyen Tran 1
This paper investigates how climate change and poverty affect child health inequality across 63 provinces in Vietnam from 2006 to 2023. By examining deaths and economic losses from storms and floods, we assess climate change’s impact; while, infant mortality rate (IMR) and under-5 mortality rate (U5MR) serve as indicators of child health inequality. Findings reveal that climate change directly worsens child health inequality and exacerbates it indirectly by increasing poverty. Notably, the effects on U5MR are more pronounced than on IMR. Additionally, child vaccinations, healthcare infrastructure, and access to clean water are vital in reducing health disparities and mitigating climate change’s harmful effects on child health.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Subscribe and save.
- Get 10 units per month
- Download Article/Chapter or eBook
- 1 Unit = 1 Article or 1 Chapter
- Cancel anytime
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
Data availability
The data that supports the findings of this study is available from the corresponding author upon reasonable request.
See more at: http://ccdpc.gov.vn/default.aspx
See more at: https://www.gso.gov.vn/en/homepage/
See more at: https://papi.org.vn/eng/
Ahmed A, Asabere SB, Adams EA, Abubakari Z (2023) Patterns and determinants of multidimensional poverty in secondary cities: implications for urban sustainability in African cities. Habitat Int 134:102775. https://doi.org/10.1016/j.habitatint.2023.102775
Article Google Scholar
Ahmed SA, Diffenbaugh NS, Hertel TW, Lobell DB, Ramankutty N, Rios AR, Rowhani P (2011) Climate volatility and poverty vulnerability in Tanzania. Glob Environ Chang 21(1):46–55. https://doi.org/10.1016/j.gloenvcha.2010.10.003
Alaba OA, Hongoro C, Thulare A, Lukwa AT (2021) Leaving No Child Behind: Decomposing Socioeconomic Inequalities in Child Health for India and South Africa. Int J Environ Res Public Health 18(13):7114. https://doi.org/10.3390/ijerph18137114
Anser MK, Yousaf SU, Usman B, Azam K, Bandar NFA, Jambari H, Sriyanto S, Zaman K (2023) Beyond climate change: Examining the role of environmental justice, agricultural mechanization, and social expenditures in alleviating rural poverty. Sustain Futures 6:100130. https://doi.org/10.1016/j.sftr.2023.100130
Arellano M, Bond S (1991) Some tests of specification for panel data: Monte Carlo evidence and an application to employment equations. Rev Econ Stud 58(2):277–297
Azzarri C, Signorelli S (2020) Climate and poverty in Africa South of the Sahara. World Dev 125:104691. https://doi.org/10.1016/j.worlddev.2019.104691
Bango M, Ghosh S (2023) Reducing infant and child mortality: assessing the social inclusiveness of child health care policies and programmes in three states of India. BMC Public Health. https://doi.org/10.1186/s12889-023-15812-7
Benevolenza MA, DeRigne L (2019) The impact of climate change and natural disasters on vulnerable populations: a systematic review of literature. J Hum Behav Soc Environ 29(2):266–281
Bennett CM, Friel S (2014) Impacts of climate change on inequities in child health. Children 1(3):461–473
Billah MA, Khan MMA, Hanifi SMA, Islam MM, Khan MN (2023) Spatial pattern and influential factors for early marriage: evidence from Bangladesh Demographic Health Survey 2017–18 data. BMC Women’s Health. https://doi.org/10.1186/s12905-023-02469-y
Black RE, Allen LH, Bhutta ZA, Caulfield LE, De Onis M, Ezzati M, Mathers C, Rivera J (2008) Maternal and child undernutrition: global and regional exposures and health consequences. The Lancet 371(9608):243–260
Blank RM (2000) Distinguished lecture on economics in government—fighting poverty: lessons from recent US history. J Econ Perspect 14(2):3–20
Blundell R, Bond S (1998) Initial conditions and moment restrictions in dynamic panel data models. J Econ 87(1):115–143
Bunyavanich S, Landrigan CP, McMichael AJ, Epstein PR (2003) The impact of climate change on child health. Ambul Pediatr 3(1):44–52
Bureau USC (2009) Statistical abstract of the United States. US Government Printing Office, Washington
Google Scholar
Callander EJ, Schofield DJ, Shrestha RN (2012) Multiple disadvantages among older citizens: what a multidimensional measure of poverty can show. J Aging Soc Policy 24(4):368–383. https://doi.org/10.1080/08959420.2012.735177
Cermeño AL, Palma N, Pistola R (2023) Stunting and wasting in a growing economy: biological living standards in Portugal during the twentieth century. Econ Human Biol. https://doi.org/10.1016/j.ehb.2023.101267
Chersich MF, Pham MD, Areal A, Haghighi MM, Manyuchi A, Swift CP, Wernecke B, Robinson M, Hetem R, Boeckmann M et al (2020) Associations between high temperatures in pregnancy and risk of preterm birth, low birth weight, and stillbirths: systematic review and meta-analysis. BMJ. https://doi.org/10.1136/bmj.m3811
Clemens V, von Hirschhausen E, Fegert JM (2020) Report of the intergovernmental panel on climate change: implications for the mental health policy of children and adolescents in Europe—a scoping review. Eur Child Adolesc Psychiatry 31:701–713
Ebaidalla EM (2023) Inequality of opportunity in child health in Sudan: across-region study. J Econ Dev 48(1):59–83
Ebi KL, Vanos J, Baldwin JW, Bell JE, Hondula DM, Errett NA, Hayes K, Reid CE, Saha S, Spector J et al (2021) Extreme weather and climate change: population health and health system implications. Annu Rev Public Health 42(1):293–315
Fagbamigbe AF, Lawal TV, Atoloye KA (2023) Evaluating the performance of different Bayesian count models in modelling childhood vaccine uptake among children aged 12–23 months in Nigeria. BMC Public Health. https://doi.org/10.1186/s12889-023-16155-z
Filho WL, Taddese H, Balehegn M, Nzengya D, Debela N, Abayineh A, Mworozi E, Osei S, Ayal DY, Nagy GJ, Yannick N, Kimu S, Balogun A-L, Alemu EA, Li C, Sidsaph H, Wolf F (2020) Introducing experiences from African pastoralist communities to cope with climate change risks, hazards and extremes: Fostering poverty reduction. Int J Disaster Risk Reduct 50:101738. https://doi.org/10.1016/j.ijdrr.2020.101738
Gentle P, Maraseni TN (2012) Climate change, poverty and livelihoods: adaptation practices by rural mountain communities in Nepal. Environ Sci Policy 21:24–34. https://doi.org/10.1016/j.envsci.2012.03.007
Goldhagen JL, Shenoda S, Oberg C, Mercer R, Kadir A, Raman S, Waterston T, Spencer NJ (2020) Rights, justice, and equity: a global agenda for child health and wellbeing. Lancet Child Adolesc Health 4(1):80–90
Gould W (1993) Quantile regression with bootstrapped standard errors. Stata Tech Bull 2(9):1–28
Göran D, Whitehead M (1991). Policies and strategies to promote social equity in health. Background document to WHO - Strategy paper for Europe, Arbetsrapport 2007:14, Institute for Futures Studies
Hallegatte S, Fay M, Barbier EB (2018) Poverty and climate change: Introduction. Environ Dev Econ 23(3):217–233
Hamilton PB, Hutchinson SJ, Patterson RT, Galloway JM, Nasser NA, Spence C, Palmer MJ, Falck H (2021) Late-Holocene diatom community response to climate driven chemical changes in a small, subarctic lake, Northwest Territories. Canada Holocene 31(7):1124–1137. https://doi.org/10.1177/09596836211003214
Hao Y, Evans GW, Farah MJ (2023) Pessimistic cognitive biases mediate socioeconomic status and children’s mental health problems. Sci Rep. https://doi.org/10.1038/s41598-023-32482-y
Helldén D, Andersson C, Nilsson M, Ebi KL, Friberg P, Alfvén T (2021) Climate change and child health: a scoping review and an expanded conceptual framework. Lancet Planet Health 5(3):e164–e175
Hertel TW, Rosch SD (2010) Climate change, agriculture, and poverty. Appl Econ Perspect Policy 32(3):355–385
Hoang HH, Huynh CM (2020) Climate change, economic growth and growth determinants: Insights from Vietnam’s coastal south central region. J Asian Afr Stud 56(3):693–704
Hoechle D (2007) Robust standard errors for panel regressions with cross-sectional dependence. Stata Journal 7(3):281–312
Hope KR (2009) Climate change and poverty in Africa. Int J Sust Dev World 16(6):451–461
Huynh CM (2023) Climate change and agricultural productivity in Asian and Pacific countries: how does research and development matter? J Econ Stud 51:712–729
Khanal U, Wilson C, Rahman S, Lee BL, Hoang V-N (2021) Smallholder farmers’ adaptation to climate change and its potential contribution to UN’s sustainable development goals of zero hunger and no poverty. J Clean Prod 281:124999. https://doi.org/10.1016/j.jclepro.2020.124999
Kistin EJ, Fogarty J, Pokrasso RS, McCally M, McCornick PG (2010) Climate change, water resources and child health. Arch Dis Child 95(7):545–549
Kota K, Chomienne M-H, Geneau R, Yaya S (2023) Socio-economic and cultural factors associated with the utilization of maternal healthcare services in Togo: a cross-sectional study. Reprod Health. https://doi.org/10.1186/s12978-023-01644-6
Liu M, Ge Y, Hu S, Stein A, Ren Z (2022) The spatial–temporal variation of poverty determinants. Spatial Statistics 50:100631. https://doi.org/10.1016/j.spasta.2022.100631
Magunda A, Ononge S, Balaba D, Waiswa P, Okello D, Kaula H, Keller B, Felker-Kantor E, Mugerwa Y, Bennett C (2023) Maternal and newborn healthcare utilization in Kampala urban slums: perspectives of women, their spouses, and healthcare providers. BMC Pregnancy Childbirth. https://doi.org/10.1186/s12884-023-05643-0
Masson-Delmotte VP, Zhai P, Pirani SL, Connors C, Péan S, Berger N, Caud Y, Chen L, Goldfarb MI, Scheel Monteiro PM (2021). Ipcc, 2021: Summary for policymakers. In: Climate change 2021: The physical science basis. contribution of working group i to the sixth assessment report of the intergovernmental panel on climate change
Memirie ST, Verguet S, Norheim OF, Levin C, Johansson KA (2016) Inequalities in utilization of maternal and child health services in Ethiopia: the role of primary health care. BMC Health Serv Res. https://doi.org/10.1186/s12913-016-1296-7
Mosley LM (2015) Drought impacts on the water quality of freshwater systems; review and integration. Earth Sci Rev 140:203–214
Moyo E, Nhari LG, Moyo P, Murewanhema G, Dzinamarira T (2023) Health effects of climate change in Africa: a call for an improved implementation of prevention measures. Eco-Environ Health 2(2):74–78. https://doi.org/10.1016/j.eehl.2023.04.004
Mujica OJ, Sanhueza A, Carvajal-Velez L, Vidaletti LP, Costa JC, Barros AJD, Victora CG (2023) Recent trends in maternal and child health inequalities in Latin America and the Caribbean: analysis of repeated national surveys. Int J Equity Health 22:1–12. https://doi.org/10.1186/s12939-023-01932-4
Muzindutsi P-F (2018) A comparative analysis of income- and asset-based poverty measures of households in a township in South Africa. Int J Econ Financ Stud 10(1):184–202
Ngu NH, Tan NQ, Non DQ, Dinh NC, Nhi PTP (2023) Unveiling urban households’ livelihood vulnerability to climate change: an intersectional analysis of Hue City. Vietnam Environ Sustain Indic 19:100269. https://doi.org/10.1016/j.indic.2023.100269
Olayide OE, Alabi T (2018) Between rainfall and food poverty: Assessing vulnerability to climate change in an agricultural economy. J Clean Prod 198:1–10. https://doi.org/10.1016/j.jclepro.2018.06.221
Onyimadu CO (2023) Climate change adaptation and wellbeing among smallholder women farmers in Gwagwalada and Kokona. Nigeria Futures 153:103238. https://doi.org/10.1016/j.futures.2023.103238
Pham T (2022) The child education and health ethnic inequality consequences of climate shocks in Vietnam. Econ Educ Rev 90:102311
Pollock EA, Gennuso KP, Givens ML, Kindig D (2021) Trends in infants born at low birthweight and disparities by maternal race and education from 2003 to 2018 in the United States. BMC Public Health 21(1):1117
Reeves R, Rodrigue E, Kneebone E (2016) Five evils: multidimensional poverty and race in America. Econ Stud Brook Rep 1:1–22
Ruggeri Laderchi C, Saith R, Stewart F (2003) Does it matter that we do not agree on the definition of poverty? A comparison of four approaches. Oxf Dev Stud 31(3):243–274. https://doi.org/10.1080/1360081032000111698
Rupasingha A, Goetz SJ (2007) Social and political forces as determinants of poverty: a spatial analysis. J Soc Econ 36(4):650–671. https://doi.org/10.1016/j.socec.2006.12.021
Rylander C, Øyvind Odland J, Manning Sandanger T (2013) Climate change and the potential effects on maternal and pregnancy outcomes: an assessment of the most vulnerable–the mother, fetus, and newborn child. Glob Health Action 6(1):19538
Samanta S, Hazra S, French JR, Nicholls RJ, Mondal PP (2023) Exploratory modelling of the impacts of sea-level rise on the Sundarbans mangrove forest West Bengal India. Sci Total Environ. https://doi.org/10.1016/j.scitotenv.2023.166624
Shiferaw N, Regassa N (2023) Levels and trends in key socioeconomic inequalities in childhood undernutrition in Ethiopia: evidence from Ethiopia demographic and health surveys 2000–2019. Discov Soc Sci Health. https://doi.org/10.1007/s44155-023-00034-4
da Silva ICM, França GV, Barros AJD, Amouzou A, Krasevec J, Victora CG (2018) Socioeconomic inequalities persist despite declining stunting prevalence in low-and middle-income countries. J Nutr 148(2):254–258
Teka AM, Temesgen Woldu G, Fre Z (2019) Status and determinants of poverty and income inequality in pastoral and agro-pastoral communities: household-based evidence from Afar Regional State Ethiopia. World Dev Perspect 15:100123. https://doi.org/10.1016/j.wdp.2019.100123
Trani J-F, Zhu Y, Park S, Khuram D, Azami R, Fazal MR, Babulal GM (2023) Multidimensional poverty is associated with dementia among adults in Afghanistan. Eclin Med 58:101906. https://doi.org/10.1016/j.eclinm.2023.101906
United Nations (1992). United Nations Framework Convention on Climate Change . https://unfccc.int/resource/docs/convkp/conveng.pdf
Wickham S, Anwar E, Barr B, Law C, Taylor-Robinson D (2016) Poverty and child health in the UK: using evidence for action. Arch Dis Child 101(8):759–766
Wooldridge G, Murthy S (2020) Pediatric critical care and the climate emergency: our responsibilities and a call for change. Front Pediatr 8:472
Woronko C, Merry L, Uckun S, Cuerrier A, Li P, Hille J, Van Hulst A (2023) Prevalence and determinants of overweight and obesity among preschool-aged children from migrant and socioeconomically disadvantaged contexts in Montreal Canada. Prev Med Rep 36:102397. https://doi.org/10.1016/j.pmedr.2023.102397
Wossen T, Berger T (2015) Climate variability, food security and poverty: agent-based assessment of policy options for farm households in Northern Ghana. Environ Sci Policy 47:95–107. https://doi.org/10.1016/j.envsci.2014.11.009
Zhou X, Chen J, Li Z, Wang G, Zhang F (2017) Impact assessment of climate change on poverty reduction: A global perspective. Phys Chem Earth Parts a/b/c 101:214–223. https://doi.org/10.1016/j.pce.2017.06.011
Download references
This research is funded by Vietnam National Foundation for Science and Technology Development (NAFOSTED) under grant number 502.01–2021.48. There are no relevant financial or non-financial competing interests to report.
Author information
Authors and affiliations.
Becamex Business School, Eastern International University, Nam Ky Khoi Nghia St, Hoa Phu Ward, Thu Dau Mot, Binh Duong, Vietnam
Cong Minh Huynh & Bao Khuyen Tran
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Cong Minh Huynh .
Ethics declarations
Conflict of interest.
The authors declare that they have no conflict of interest.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Huynh, C.M., Tran, B.K. Climate change, poverty and child health inequality: evidence from Vietnam’s provincial analysis. Econ Change Restruct 57 , 163 (2024). https://doi.org/10.1007/s10644-024-09743-5
Download citation
Received : 01 February 2024
Accepted : 22 August 2024
Published : 09 September 2024
DOI : https://doi.org/10.1007/s10644-024-09743-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Climate change
- Child health inequality
JEL Classification
- Find a journal
- Publish with us
- Track your research
Poverty and Health - The Family Medicine Perspective (Position Paper)
Introduction
Poverty is a complex and insidious determinant of health caused by systemic factors that can persist for generations in a family. Beginning before birth and continuing throughout an individual’s life, poverty can significantly impact health and health outcomes. The vision of the American Academy of Family Physicians (AAFP) is to transform health care to achieve optimal health for everyone. Primary care physicians and public health professionals continue to collaborate on a shared vision of improving population health. As the integration of primary care and public health continues, this shared vision becomes even more relevant, focused, and clear. Success in this new era means achieving better outcomes by transforming health care to overcome obstacles related to the social, environmental, and community determinants of health – including poverty. 1,2,3,4
Family physicians have a unique perspective on local population’s health challenges because we serve generations of families and follow individual patients through different life stages. We are privileged to share the complex stories of individuals and families in sickness and health over long periods and across different care settings. Rather than viewing a single snapshot of a patient during an episode of illness, we know the patient’s whole story. We know the environmental, patient, and family factors that lead to illness and disease – and the patient’s need to manage their condition effectively. As lifelong collaborators in care, family physicians are well-positioned to understand each patient’s unique obstacles to better health and help overcome them.
Call to Action
The AAFP urges its members to become informed about the impact of poverty on health. Achieving the vision of optimal health for everyone requires a culturally proficient care team and a well-resourced medical neighborhood that supplies readily accessible solutions. Family physicians play a critical role in community health and can contribute through bold efforts in many areas. When these solutions are incorporated seamlessly into everyday practice workflows, family physicians and care teams can be true to the AAFP’s vision by achieving positive change for individuals, families, and communities, and improve population health.
The AAFP calls for action in the following areas:
Physician Level
- Become more informed about the impact of the social determinants of health (SDoH) and identify tangible next steps you can take to address and reduce health inequities
- Be aware of, and sensitive to, your patient’s specific circumstances to help them achieve their health goals
Practice Level
- Identify critical factors that impact patient health, leveraging The EveryONE Project and data collection on SDoH in electronic health records (EHRs)
- Understand each patient’s unique challenges and coping strategies and know what community resources are available
Community-Leadership Level
- Promote alignment with other private and public community resources to help advance the integration of primary care and public health
- Partner with other health care and social service organizations to connect directly to resources that mitigate poverty’s effect on health
Educational Level
- Drive change in undergraduate and graduate medical education to ensure future physicians are adequately prepared to prevent and address disparities caused by SDoH
Advocacy Level
- Work with local, state, and national governments to adopt a Health in All Policies approach that prioritizes health within goals and agenda-setting
- Advocate for regulatory frameworks and economic incentives to ensure public health and population health are critical to individual health care efforts
Understanding Poverty and Low-income Status
Poverty occurs when an individual or family lacks the resources to provide life necessities, such as food, clean water, shelter, and clothing. It also includes a lack of access to such resources as health care, education, and transportation. 5 In the United States, federal poverty is expressed as an annual pre-tax income level indexed by the size of household and age of household members. For example, in 2020, the federal poverty income level was $12,760 for an individual younger than 65 years and $26,200 for a family of four. 6 In 2019, approximately 10.5% of Americans were living below the poverty line. While overall poverty rates had been declining in the past several years, inequalities remain by SDoH, including race and racism, ethnicity, educational attainment, and disability status. 7
The term “low income” generally describes individuals and families whose annual income is less than 130-150% of the federal poverty income level. For example, the Supplemental Nutrition Assistance Program (SNAP) is available to individuals with a gross monthly income of 130% of the federal poverty income level. 8 Medicaid is open to families with an income of 138% of the poverty income level. 9
Poverty and low-income status are associated with various adverse health outcomes, including shorter life expectancy, higher infant mortality rates, and higher death rates for the 14 leading causes of death. 10,11 Individual- and community-level mechanisms mediate these effects. 12 For individuals, poverty restricts the resources used to avoid risks and adopt healthy behaviors. 13 Poverty also affects the built environment (i.e., the human-made physical parts of the places where people live, work, and play, including buildings, open spaces, and infrastructure), services, culture, and communities’ reputation, all of which have independent effects on health outcomes. 14
Location matters, and there are often dramatic differences in health care delivery and health outcomes between communities that are only a few miles apart. For example, the Robert Wood Johnson Foundation (RWJF) found a 25-year difference in average life expectancy in New Orleans, LA, between inner city and suburban neighborhoods. Similarly, there is a 14-year difference in average life expectancy between two Kansas City, MO, neighborhoods that are roughly three miles apart. 15
A study by The Commonwealth Fund assessed 30 indicators of access, prevention, quality, potentially avoidable hospital use, and health outcomes. The study found that populations with low-income status suffer disparities in every state. However, it also identified significant differences among states’ performances. For top-performing states, many health care measures of populations with low income were better than average and better than those for individuals with higher income or more education in lagging states. These findings indicate that low-income status does not have to determine poor health or poor care experience. Interventions seen in top-performing states, such as expanded insurance coverage, access, and coordination of social and medical services, can help mitigate poverty’s effects on health. 16
Poverty and Health
SDoH are the conditions under which people are born, grow, live, work, and age, and include factors such as socioeconomic status, education, employment, social support networks, and neighborhood characteristics. 4 These social factors have a more significant collective impact on health and health outcomes than health behavior, health care, and the physical environment. 17,18 SDoH, especially poverty, structural racism, and discrimination, are the primary drivers of health inequities. 19,20
Economic prosperity can provide individuals access to resources to avoid or buffer exposure to health risks. 21 Research shows that individuals with higher incomes consistently experience better health outcomes than individuals with low incomes and those living in poverty. 22 Poverty affects health by limiting access to proper nutrition and healthy foods; shelter; safe neighborhoods to learn, live, and work; clean air and water; utilities; and other elements that define an individual’s standard of living. Individuals who live in low-income or high-poverty neighborhoods are likely to experience poor health due to a combination of these factors. 23,24
Violence is also more prevalent in areas with greater poverty. From 2008 to 2012, individuals in households at or below the poverty level experienced more than double the rate of violent victimization than individuals in high-income households. 25 This pattern of victimization by violent behavior was consistent for both Black and white individuals. It significantly impacts the victim’s family and perpetrator’s family (through incarceration).
Because they intersect with so many SDoH, poverty and low-income status dramatically affects life expectancy. 26 Education and its socioeconomic status correlate to income and wealth. These have powerful associations with life expectancy for both sexes and all races at all ages. Students from families with low income are five times more likely to drop out of high school than students from families with high income. 27 In 2008, the life expectancy among U.S. adult men and women with fewer than 12 years of education was not much better than the life expectancy among all adults in the 1950s and 1960s. 28
Poverty affects individuals insidiously in other ways that we are just beginning to understand. Mental illness, chronic health conditions, and substance use disorders are all more prevalent in populations with low income. 29 Poor nutrition, toxic exposures (e.g., lead), and elevated levels of the stress hormone cortisol are factors associated with poverty that may have lasting effects on children beginning before birth and continuing after birth. These effects, which can influence cognitive development and chronic disease development, are dose-dependent (i.e., the duration of exposure matters). 30,31,32 For example, the greater the number of years a child spends living in poverty, the more elevated the child’s overnight cortisol level and the more dysregulated the child’s cardiovascular response to acute stressors. 31 Impaired development of the nervous system affects cognitive and socioemotional development and increases the risk of behavioral challenges, adverse health behaviors, and poor school performance. 31,32 Recent studies have even identified a strong association between pediatric suicide and county-level poverty rates. 33
However, the effects of poverty are not predictably uniform. Longitudinal studies of health behavior describe positive (e.g., tobacco use cessation) and negative (e.g., decrease in physical activity) health behavior trends in populations with lower and higher socioeconomic status. However, there is a socioeconomic gradient in health improvement. In other words, populations with lower socioeconomic status lag behind populations with higher socioeconomic status in positive gains from health behavior trends. Health behaviors are important in that they account for differences in mortality. 34 The fact that positive changes in health behaviors are possible despite the challenges of poverty points to the importance of developing and implementing interventions that promote healthy behaviors in populations with low income.
Risk Regulators and Intervention
Poverty affects health in many different ways through complex mechanisms that we are just beginning to understand and describe. Living in poverty does not necessarily predetermine poor health. 35 Poverty will not “cause” a disease. Instead, poverty affects both the likelihood that an individual will have risk factors for disease and its ability and opportunity to prevent and manage disease. An individual’s health outcomes (a physiologic expression) ultimately will be influenced by genetic and environmental factors, as well as health behaviors – all of which may be affected by poverty. Material conditions, discriminatory practices, neighborhood conditions, behavioral norms, work conditions, as well as laws, policies, and regulations associated with poverty make it a “risk regulator.” 35 This means that poverty functions as a control parameter at a system level to influence the probability of exposure to key risk factors (e.g., behaviors, environmental risks) that lead to disease (Figure 1).
Figure 1: An Illustration of Risk Regulators in Social and Biological Context
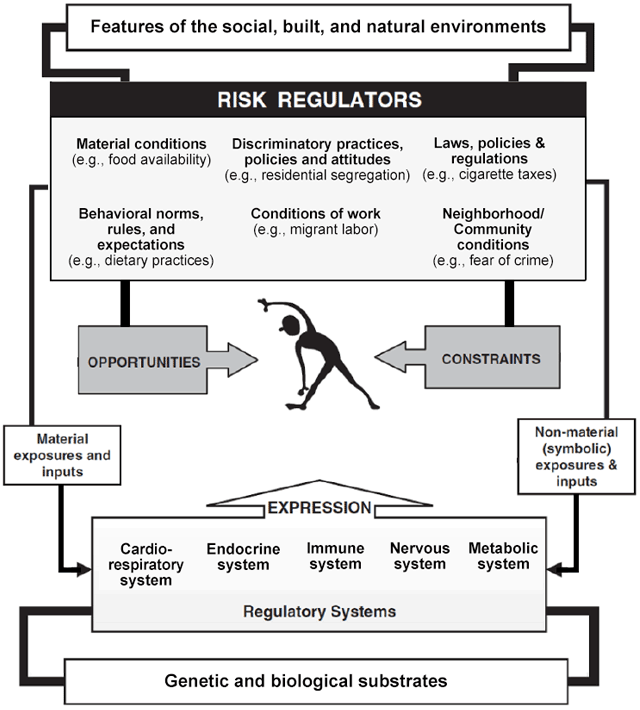
Reprinted with permission from Glass TA, McAtee MJ. Behavioral science at the crossroads in public health: extending horizons, envisioning the future. Soc Sci Med. 2006;62(7):1650-1671.
Thinking of poverty as a risk regulator rather than a rigid determinant of health allows family physicians to relinquish the feeling of helplessness when providing medical care to families and individuals with low income.
Family physicians are uniquely positioned to devise solutions to mitigate the development of risk factors that lead to disease and the conditions unique to populations with low income that interfere with effective disease prevention and management. They can boost an individual or family’s “host resistance” to the health effects of poverty and tap into a growing array of aligned resources that provide patients and families with tangible solutions so that health maintenance can be a realistic goal.
Role of the Family Physician
Community-Oriented Primary Care (COPC)
Strong primary care teams are critical in the care of patients with low income. These populations often have higher rates of chronic disease and difficulty navigating health care systems. They benefit from care coordination and team-based care that addresses medical and socioeconomic needs.
In the United States, there is a move toward increased payment from government and commercial payers to offset the cost of providing coordinated and team-based care. Some payment models provide shared savings or care coordination payments in addition to traditional fee-for-service reimbursement. The practice transformations from COPC and payment models based on targets and meaningful use alter how we approach patient panels and communities. 36 The rationale behind alternative payment models – particularly regarding the care of lower socioeconomic populations – is that significant cost savings can be realized when care moves toward prevention and self-management and away from crisis-driven, fragmented care provided in the emergency department or a hospital setting. By recognizing and treating disease earlier – and actively partnering with local public health services like health educators, community health workers, and outreach services – family physicians can help prevent costly, avoidable complications and reduce the total cost of care.
Community Responsive Care
Care team members can positively affect the health of patients with low income by creating a welcoming, nonjudgmental environment that supports a long-standing therapeutic relationship built on trust. Familiarity with the National Standards for Culturally and Linguistically Appropriate Services (CLAS) in Health and Health Care can prepare practices and institutions to provide care in a manner that promotes health equity. 37
Patients with low income may be unintentionally shamed by the care team when their behaviors are seen as evidence of being “noncompliant” (e.g., missing appointments, not adhering to a medical regimen, not getting tests done). These patients may not be comfortable sharing information about the challenges that lead to their “noncompliant” behaviors. For example, a patient with low income may arrive 15 minutes late to an appointment because they have to rely on someone else for transportation. A patient may not take prescribed medication because it is too expensive. A patient may not get tests done because their employer will not allow time off from work. A patient may not understand printed care instructions because of low-literacy skills. Such patients may be turned away by staff because their tardiness disrupts the schedule, or they may even be dismissed from the practice altogether because of repeated noncompliance. Physicians and care team members should learn why the patient was noncompliant and promote an atmosphere of tolerance and adaptation.
Patients with low socioeconomic status and other marginalized populations rarely respond well to dictation from health care professionals. Instead, interventions that rely on peer-to-peer storytelling or coaching are more effective in overcoming cognitive resistance to positive health behavior changes. 38 Physicians and care team members can identify local groups that provide peer-to-peer support. Such activities are typically hosted by local hospitals, faith-based organizations, health departments, or senior centers.
Screen for Socioeconomic Challenges
Family physicians regularly screen for risk factors for disease. Screening to identify patients’ socioeconomic challenges and other SDoH can be incorporated into practices using EveryONE Project tools. Once socioeconomic challenges are identified, physicians and their care teams can work with patients to design achievable, sustainable treatment plans. The simple question, “Do you (ever) have difficulty making ends meet at the end of the month?” has a sensitivity of 98% and specificity of 60% in predicting poverty. 39 A casual inquiry about the cost of a patient’s medications is another way to start a conversation about socioeconomic obstacles to care.
A patient’s home and neighborhood affect health. 40 The care team should ask the patient whether their home is adequate to support healthy behaviors. For example, crowding, infestations, and lack of utilities are all risk factors for disease. Knowing that a patient is homeless or has poor, inadequate housing will help guide care.
Set Priorities and Make a Realistic Plan of Action
Family physicians direct the therapeutic process by working with the patient and care team to identify priorities so treatment goals are clear and achievable. In many cases, suspending a “fix everything right now” agenda in favor of a treatment plan of small steps that incorporate shared decision making can help this process. It is likely that a patient with low income will not have the resources (e.g., on-demand transportation, forgiving work schedule, available child care) to comply with an ideal treatment plan. Formulating a treatment plan that makes sense for the patient’s life circumstances is vital to success.
For example, for a patient with limited means and multiple chronic conditions – including hypertension and diabetes – start by addressing these conditions. Colon cancer screening or a discussion about beginning statin therapy can come later. It may be easier for this patient to adhere to an insulin regimen involving vials and syringes instead of insulin pens, which are much more expensive. The “best” medication for a patient with low income is the one that the patient can afford and self-administer reliably. Celebrate success with each small step that takes a patient closer to disease control and improved self-management.
Help Newly Insured Patients Navigate the Health Care System
In many states, the expansion of Medicaid has allowed individuals and families with low income to become insured – perhaps for the first time. A newly insured individual with low income will not necessarily know how or when to make, keep, or reschedule an appointment; develop a relationship with a family physician; manage medication refills; or obtain referrals. They may be embarrassed to reveal this lack of knowledge to the care team. Physicians and care team members can help by providing orientation to newly insured patients within the practice. For example, ensure that all patients know where to pick up medication, how to take it and why, when to return for a follow-up visit and why, and how to follow their treatment plan from one appointment to the next. Without this type of compassionate intervention, patients may revert to an old pattern of seeking crisis-driven care often provided by the emergency department or a local hospital.
Provide Material Support to Families with Low Income
Resources that make it easier for busy physicians to provide support to families with low income include the following:
● Reach Out and Read is a program that helps clinicians provide books for parents to take home to read to their children. Studies have shown that Reach Out and Read improve children’s language skills. 41
● 2-1-1 is a free, confidential service that patients or staff can access 24 hours a day by phone. 2-1-1 is staffed by community resource specialists who can connect patients to resources such as food, clothing, shelter, utility bill relief, social services, and even employment opportunities. Follow-up calls are made to ensure clients connect successfully with the resource referrals.
● The National Domestic Violence Hotline is staffed 24 hours a day by trained advocates who provide confidential help and information to patients who are experiencing domestic violence.
Local hospitals, health departments, and faith-based organizations often are connected to community health resources that offer services such as installing safety equipment in homes; providing food resources; facilitating behavioral health evaluation and treatment; and providing transportation, vaccinations, and other benefits to individuals and families with low income.
Practices can make a resource folder of information about local community services that can be easily accessed when taking care of patients in need. This simple measure incorporates community resources into the everyday workflow of patient care, thus empowering the care team.
Participate in Research that Produces Relevant Evidence
Much of the research about the effects of poverty on health is limited to identifying health disparities. This is insufficient. Research that evaluates specific interventions is needed to gain insight into what effectively alleviates poverty’s effects on health care delivery and outcomes. Family physicians can serve a critical role in this research because we have close relationships with patients with low income. 42
Advocate on Behalf of Neighborhoods and Communities with Low Income
Family physicians are community leaders, so we can advocate effectively for initiatives that improve the quality of life in neighborhoods with low income. Some forms of advocacy are apparent, such as promoting a state’s expansion of Medicaid. Other efforts may be specific to the community served. For example, a vacant lot can be converted to a basketball court or soccer field. A community center can expand programs that involve peer-to-peer health coaching. A walking program can be started among residents in a public housing unit. Collaboration with local law enforcement agencies can foster the community’s trust and avoid the potential for oppression. 43
Family physicians have local partners in advocacy, so we do not have to act in isolation. As a result of the Patient Protection and Affordable Care Act (ACA), nonprofit hospitals regularly report community needs assessments and work with local health departments to establish action plans that address identified needs. A Community Health Needs Assessment (CHNA) reflects a specific community’s perception of need, and each action plan outlines multi-sectoral solutions to meet local health needs. Local CHNAs are typically available online, as are the associated action plans. Family physicians can use information in the CHNA to access local health care leadership and join aligned forces in the communities we serve, thereby supporting the AAFP’s vision of achieving optimal health for everyone.
1. Sherin K, Adebanjo T, Jani A. Social determinants of health: family physicians’ leadership role. Am Fam Physician . 2019;99(8):476-477.
2. Commission on Social Determinants of Health. Closing the gap in a generation. Health equity through action on the social determinants of health. World Health Organization (WHO). Accessed March 22, 2021. www.who.int/social_determinants/final_report/csdh_finalreport_2008.pdf
3. Kovach KA, Reid K, Grandmont J, et al. How engaged are family physicians in addressing the social determinants of health? A survey supporting the American Academy of Family Physician’s health equity environmental scan. Health Equity . 2019;3(1):449-457.
4. American Academy of Family Physicians (AAFP). Advancing health equity by addressing the social determinants of health in family medicine (position paper). Accessed March 22, 2021.
5. World Vision. What is poverty? It’s not as simple as you think. Accessed March 22, 2021. www.worldvision.ca/stories/child-sponsorship/what-is-poverty#:~:text=1.-,What%20is%20the%20definition%20of%20poverty%3F,care%2C%20education%20and%20even%20transportation
6. Office of the Assistant Secretary for Planning and Evaluation. 2020 poverty guidelines. Accessed March 22, 2021. https://aspe.hhs.gov/2020-poverty-guidelines
7. United States Census Bureau. Income, poverty and health insurance coverage in the United States: 2019. Accessed March 22, 2021. www.census.gov/newsroom/press-releases/2020/income-poverty.html
8. United States Department of Agriculture. SNAP special rules for the elderly or disabled. Accessed March 22, 2021. www.fns.usda.gov/snap/eligibility/elderly-disabled-special-rules
9. U.S. Centers for Medicare & Medicaid Services. Federal poverty level (FPL). Accessed March 22, 2021. www.healthcare.gov/glossary/federal-poverty-level-fpl/
10. Link BG, Phelan J. Social conditions as fundamental causes of disease. J Health Soc Behav . 1995;Spec No:80-94.
11. Brooks-Gunn J, Duncan GJ. The effects of poverty on children. Future Child . 1997;7(2):55-71.
12. Berkman LF, Kawachi I. A historical framework for social epidemiology. In: Berkman LF, Kawachi I, eds. Social Epidemiology . New York, NY: Oxford University Press; 2014.
13. Phelan JC, Link BG, Tehranifar P. Social conditions as fundamental causes of health inequalities: theory, evidence, and policy implications. J Health Soc Behav . 2010;51 Suppl:S28-S40.
14. Macintyre S, Ellaway A, Cummins S. Place effects on health: how can we conceptualise, operationalise and measure them? Soc Sci Med . 2002;55(1):125-139.
15. Robert Wood Johnson Foundation. Mapping life expectancy. Short distances to large gaps in health. Accessed March 22, 2021. www.rwjf.org/en/library/articles-and-news/2015/09/city-maps.html
16. Schoen C, Radley D, Riley P, et al. Health care in the two Americas. Findings from the Scorecard on State Health System Performance for Low-Income Populations, 2013. Accessed March 22, 2021. www.commonwealthfund.org/sites/default/files/documents/___media_files_publications_fund_report_2013_sep_1700_schoen_low_income_scorecard_full_report_final_v4.pdf
17. Booske BC, Athens JK, Kindig DA, Park H, Remington PL. County health rankings working paper. Different perspectives for assigning weights to determinants of health. University of Wisconsin Population Health Institute. Accessed March 22, 2021. www.countyhealthrankings.org/sites/default/files/differentPerspectivesForAssigningWeightsToDeterminantsOfHealth.pdf
18. County Health Rankings & Roadmaps. County Health Rankings model. Accessed March 22, 2021. www.countyhealthrankings.org/explore-health-rankings/measures-data-sources/county-health-rankings-model
19. Phelan JC, Link BG, Tehranifar P. Social conditions as fundamental causes of health inequalities: theory, evidence, and policy implications. J Health Soc Behav . 2010;51 Suppl:S28-S40.
20. National Academies of Sciences, Engineering, and Medicine. Communities in action. Pathways to health equity. Accessed March 22, 2021. www.nap.edu/catalog/24624/communities-in-action-pathways-to-health-equity
21. Anderson LM, Scrimshaw SC, Fullilove MT, Fielding JE, Task Force on Community Preventive Services. The Community Guide’s model for linking the social environment to health. Am J Prev Med . 2003;24(3 Suppl):12-20.
22. Berkman LF, Kawachi I, eds. Social Epidemiology . New York, NY: Oxford University Press; 2000.
23. Riste L, Khan F, Cruickshank K. High prevalence of type 2 diabetes in all ethnic groups, including Europeans, in a British inner city: relative poverty, history, inactivity, or 21st century Europe? Diabetes Care . 2001;24(8):1377-1383.
24. Healthy People 2030. Social determinants of health. Accessed March 22, 2021. https://health.gov/healthypeople/objectives-and-data/social-determinants-health
25. Bureau of Justice Statistics. Household poverty and nonfatal violent victimization, 2008-2012. Accessed March 24, 2021. www.bjs.gov/index.cfm?ty=pbdetail&iid=5137
26. Chetty R, Stepner M, Abraham S, et al. The association between income and life expectancy in the United States, 2001–2014. JAMA . 2016;315(16):1750-1766.
27. National Center for Education Statistics. Trends in high school dropout and completion rates in the United States: 1972–2009. Accessed March 24, 2021. https://nces.ed.gov/pubs2012/2012006.pdf
28. Olshansky SJ, Antonucci T, Berkman L, et al. Differences in life expectancy due to race and educational differences are widening, and many may not catch up. Health Aff (Millwood). 2012;31(8):1803-1813.
29. Walker ER, Druss BG. Cumulative burden of comorbid mental disorders, substance use disorders, chronic medical conditions, and poverty on health among adults in the United States. Psychol Health Med . 2017;22(6):727-735.
30. Evans GW, Kim P. Childhood poverty and health: cumulative risk exposure and stress dysregulation. Psychol Sci . 2007;18(11):953-957.
31. Lipina SJ, Colombo JA. Poverty and Brain Development During Childhood: An Approach from Cognitive Psychology and Neuroscience . Human Brain Development Series. Washington, DC: American Psychological Association; 2009.
32. Farah MJ, Noble KG, Hurt H. Poverty, privilege, and brain development: empirical findings and ethical implications. In: Illes J, ed. Neuroethics: Defining the Issues in Theory, Practice, and Policy . New York: Oxford University Press; 2005.
33. Hoffmann JA, Farrell CA, Monuteaux MC, et al. Association of pediatric suicide with county-level poverty in the United States, 2007-2016. JAMA Pediatr . 2020;174(3):287-294.
34. Stringhini S, Sabia S, Shipley M, et al. Association of socioeconomic position with health behaviors and mortality. JAMA . 2010;303(12):1159-1166.
35. Glass TA, McAtee MJ. Behavioral science at the crossroads in public health: extending horizons, envisioning the future. Soc Sci Med . 2006;62(7):1650-1671.
36. American Academy of Family Physicians. Integration of primary care and public health (position paper). Accessed March 24, 2021. www.aafp.org/about/policies/all/integration-primary-care.html
37. U.S. Department of Health and Human Services. National CLAS Standards. Accessed March 24, 2021. https://thinkculturalhealth.hhs.gov/clas
38. Houston TK, Allison JJ, Sussman M, et al. Culturally appropriate storytelling to improve blood pressure: a randomized trial. Ann Intern Med . 2011;154(2):77-84.
39. Brcic V, Eberdt C, Kaczorowski J. Development of a tool to identify poverty in a family practice setting: a pilot study. Int J Family Med . 2011;2011:812182.
40. Braveman P, Dekker M, Egerter S, Sadegh-Nobari T, Pollack C. Housing and health. Robert Wood Johnson Foundation. Accessed March 24, 2021. www.dhss.delaware.gov/dhss/dph/mh/files/housingandhealth.pdf
41. Zuckerman B. Promoting early literacy in pediatric practice: twenty years of Reach Out and Read. Pediatrics. 2009;124(6):1660-1665.
42. O’Campo P, Dunn JR, eds. Rethinking Social Epidemiology: Towards a Science of Change . New York, NY: Springer; 2012.
43. President's Task Force on 21st Century Policing. Interim report of the President's Task Force on 21st Century Policing. Office of Community-Oriented Policing Services. Accessed March 21, 2021. https://cdpsdocs.state.co.us/ccjj/meetings/2015/2015-03-13_CCJJ_Presidents-21CentCommPolicingTF-InterimReport.pdf
(2015 COD) (January 2022 COD)
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.
- Open access
- Published: 09 September 2024
Exploring the impact of housing insecurity on the health and wellbeing of children and young people in the United Kingdom: a qualitative systematic review
- Emma S. Hock 1 ,
- Lindsay Blank 1 ,
- Hannah Fairbrother 1 ,
- Mark Clowes 1 ,
- Diana Castelblanco Cuevas 1 ,
- Andrew Booth 1 ,
- Amy Clair 2 &
- Elizabeth Goyder 1
BMC Public Health volume 24 , Article number: 2453 ( 2024 ) Cite this article
Metrics details
Housing insecurity can be understood as experiencing or being at risk of multiple house moves that are not through choice and related to poverty. Many aspects of housing have all been shown to impact children/young people’s health and wellbeing. However, the pathways linking housing and childhood health and wellbeing are complex and poorly understood.
We undertook a systematic review synthesising qualitative data on the perspectives of children/young people and those close to them, from the United Kingdom (UK). We searched databases, reference lists, and UK grey literature. We extracted and tabulated key data from the included papers, and appraised study quality. We used best fit framework synthesis combined with thematic synthesis, and generated diagrams to illustrate hypothesised causal pathways.
We included 59 studies and identified four populations: those experiencing housing insecurity in general (40 papers); associated with domestic violence (nine papers); associated with migration status (13 papers); and due to demolition-related forced relocation (two papers). Housing insecurity took many forms and resulted from several interrelated situations, including eviction or a forced move, temporary accommodation, exposure to problematic behaviour, overcrowded/poor-condition/unsuitable property, and making multiple moves. Impacts included school-related, psychological, financial and family wellbeing impacts, daily long-distance travel, and poor living conditions, all of which could further exacerbate housing insecurity. People perceived that these experiences led to mental and physical health problems, tiredness and delayed development. The impact of housing insecurity was lessened by friendship and support, staying at the same school, having hope for the future, and parenting practices. The negative impacts of housing insecurity on child/adolescent health and wellbeing may be compounded by specific life circumstances, such as escaping domestic violence, migration status, or demolition-related relocation.
Housing insecurity has a profound impact on children and young people. Policies should focus on reducing housing insecurity among families, particularly in relation to reducing eviction; improving, and reducing the need for, temporary accommodation; minimum requirements for property condition; and support to reduce multiple and long-distance moves. Those working with children/young people and families experiencing housing insecurity should prioritise giving them optimal choice and control over situations that affect them.
Peer Review reports
Introduction
The impacts of socioeconomic position in childhood on adult health outcomes and mortality are well documented in quantitative analyses (e.g., [ 1 ]). Housing is a key mechanism through which social and structural inequalities can impact health [ 2 ]. The impact of housing conditions on child health are well established [ 3 ]. Examining the wellbeing of children and young people within public health overall is of utmost importance [ 4 ]. Children and young people (and their families) who are homeless are a vulnerable group with particular difficulty in accessing health care and other services, and as such, meeting their needs should be a priority [ 5 ].
An extensive and diverse evidence base captures relationships between housing and health, including both physical and mental health outcomes. Much of the evidence relates to the quality of housing and specific aspects of poor housing including cold and damp homes, poorly maintained housing stock or inadequate housing leading to overcrowded accommodation [ 6 , 7 , 8 , 9 , 10 , 11 , 12 , 13 ]. The health impacts of housing insecurity, together with the particular vulnerability of children and young people to the effects of not having a secure and stable home environment, continue to present a cause for increased concern [ 7 , 8 , 11 , 14 ]. The National Institute for Health and Care Research (NIHR) Public Health Reviews (PHR) Programme commissioned the current review in response to concerns about rising levels of housing insecurity and the impact of housing insecurity on the health and wellbeing of children and young people in the United Kingdom (UK).
Terminology and definitions related to housing insecurity
Numerous diverse terms are available to define housing insecurity, with no standard definition or validated instrument. For the purpose of our review, we use the terminology and definitions used by the Children’s Society, which are comprehensive and based directly on research with children that explores the relationship between housing and wellbeing [ 15 ]. They use the term “housing insecurity” for those experiencing and at risk of multiple moves that are (i) not through choice and (ii) related to poverty [ 15 ]. This reflects their observation that multiple moves may be a positive experience if they are by choice and for positive reasons (e.g., employment opportunities; moves to better housing or areas with better amenities). This definition also acknowledges that the wider health and wellbeing impacts of housing insecurity may be experienced by families that may not have experienced frequent moves but for whom a forced move is a very real possibility. The Children’s Society definition of housing insecurity encompasses various elements (see Table 1 ).
Housing insecurity in the UK today – the extent of the problem
Recent policy and research reports from multiple organisations in the UK highlight a rise in housing insecurity among families with children [ 19 , 22 , 23 ]. Housing insecurity has grown following current trends in the cost and availability of housing, reflecting in particular the rapid increase in the number of low-income families with children in the private rental sector [ 19 , 22 , 24 ], where housing tenures are typically less secure. The ending of a tenancy in the private rental sector was the main cause of homelessness given in 15,500 (27% of claims) of applications for homelessness assistance in 2017/18, up from 6,630 (15% of claims) in 2010/11 for example [ 25 ]. The increased reliance on the private rented sector for housing is partly due to a lack of social housing and unaffordability of home ownership [ 23 ]. The nature of tenure in the private rental sector and gap between available benefits and housing costs means even low-income families that have not experienced frequent moves may experience the negative impacts of being at persistent risk of having to move [ 26 ]. Beyond housing benefit changes, other changes to the social security system have been linked with increased housing insecurity. The roll-out of Universal Credit Footnote 1 , with its built-in waits for payments, has been linked with increased rent arrears [ 27 , 28 ]. The introduction of the benefit cap, which limits the amount of social security payments a household can receive, disproportionately affects housing support and particularly affecting lone parents [ 29 , 30 , 31 ].
The increase in families experiencing housing insecurity, including those living with relatives or friends (the ‘hidden homeless’) and those in temporary accommodation provided by local authorities, are a related consequence of the lack of suitable or affordable rental properties, which is particularly acute for lone parents and larger families. The numbers of children and young people entering the social care system or being referred to social services because of family housing insecurity contributes further evidence on the scale and severity of the problem [ 32 ].
The COVID-19 pandemic exacerbated housing insecurity in the UK [ 24 ], with the impacts continuing to be felt. In particular, the pandemic increased financial pressures on families (due to loss of income and increased costs for families with children/young people at home). These financial pressures were compounded by a reduction in informal temporary accommodation being offered by friends and family due to social isolation precautions [ 24 ]. Further, the COVID-19 pandemic underscored the risks to health posed by poor housing quality (including overcrowding) and housing insecurity [ 24 , 33 ]. Recent research with young people in underserved communities across the country also highlighted their experience of the uneven impact of COVID-19 for people in contrasting housing situations [ 34 ].
While the temporary ban on bailiff-enforced evictions, initiated due to the pandemic, went some way towards acknowledging the pandemic’s impact on housing insecurity, housing organisations are lobbying for more long-term strategies to support people with pandemic-induced debt and rent-arrears [ 33 ]. The Joseph Rowntree Foundation has warned of the very real risk of a ‘two-tier recovery’ from the pandemic, highlighting the ‘disproportionate risks facing people who rent their homes’ ([ 35 ], para. 1). Their recent large-scale survey found that one million renting households worry about being evicted in the next three months, and half of these were families with children [ 35 ]. The survey also found that households with children, renters from ethnic minority backgrounds and households on low incomes are disproportionately affected by pandemic-induced debt and rent arrears [ 35 ].
The cost-of-living crisis is exacerbating the impact of the COVID-19 pandemic, with many households experiencing or set to experience housing insecurity due to relative reductions in income accompanying increases in rent and mortgage repayments [ 36 ]. People experiencing or at risk of housing insecurity are disproportionately affected, due to higher food and utility costs [ 37 ].
Research evidence on relationships between housing in childhood and health
Housing is a key social determinant of health, and a substantive evidence base of longitudinal cohort studies and intervention studies supports a causal relationship between the quality, affordability and stability of housing and child health [ 38 ]. Evidence includes immediate impacts on mental and physical health outcomes and longer-term life course effects on wider determinants of health including education, employment and income as well as health outcomes [ 39 ].
The negative health impact of poor physical housing conditions has been well documented [ 40 , 41 ]. Housing instability and low housing quality are associated with worse psychological health among young people and parents [ 42 , 43 ]. The UK National Children’s Bureau [ 22 ] draws attention to US-based research showing that policies that reduced housing insecurity for young children can help to improve their emotional health [ 44 ], and that successful strategies for reducing housing insecurity have the potential to reduce negative outcomes for children with lived experience of housing insecurity, including emotional and behavioural problems, lower academic attainment and poor adult health and wellbeing [ 45 ]. A variety of pathways have been implicated in the relationship between housing insecurity and child health and wellbeing, including depression and psychological distress in parents, material hardships and difficulties in maintaining a good bedtime routine [ 38 ]. Frequent moves are also associated with poorer access to preventive health services, reflected, for example, in lower vaccination rates [ 46 , 47 ].
Housing tenure, unstable housing situations and the quality or suitability of homes are inter-related [ 48 ]. For example, if families are concerned that if they lost their home they would not be able to afford alternative accommodation, they may be more likely to stay in smaller or poor-quality accommodation or in a neighbourhood where they are further from work, school or family support. In this way, housing insecurity can lead to diverse negative health and wellbeing impacts relating to housing and the neighbourhoods, even if in the family does not experience frequent moves or homelessness [ 49 ]. Thus, the relationship between housing insecurity and child health is likely to be complicated by the frequent coexistence of poor housing conditions or unsuitable housing with housing insecurity. The relationship between unstable housing situations and health outcomes is further confounded by other major stressors, such as poverty and changes in employment and family structure, which may lead to frequent moves.
The evidence from cohort studies that show a relationship between housing insecurity, homelessness or frequent moves in childhood and health related outcomes can usefully quantify the proportion of children/young people and families at risk of poorer health associated with housing instability. It can, however, only suggest plausible causal associations. Further, the ‘less tangible aspects of housing’ such as instability are poorly understood [ 40 ]. Additional (and arguably stronger) evidence documenting the relationship between housing insecurity and health/wellbeing comes from the case studies and qualitative interviews with children and young people and families that explore the direct and indirect impacts of housing insecurity on their everyday lives and wellbeing. Thus, the current review aimed to identify, appraise and synthesise research evidence that explores the relationship between housing insecurity and the health and wellbeing among children and young people. We aimed to highlight the relevant factors and causal mechanisms to make evidence-based recommendations for policy, practice and future research priorities.
We undertook a systematic review synthesising qualitative data, employing elements of rapid review methodology in recognition that the review was time-constrained. This involved two steps: (1) a single screening by one reviewer of titles and abstracts, with a sample checked by another reviewer; and (2) a single data extraction and quality assessment, with a sample checked by another reviewer) [ 50 , 51 , 52 ]. The protocol is registered on the PROSPERO registry, registration number CRD42022327506.
Search strategy
Searches of the following databases were conducted on 8th April 2022 (from 2000 to April 2022): MEDLINE, EMBASE and PsycINFO (via Ovid); ASSIA and IBSS (via ProQuest) and Social Sciences Citation Index (via Web of Science). Due to the short timescales for this project, searches aimed to balance sensitivity with specificity, and were conceptualised around the following concepts: (housing insecurity) and (children or families) and (experiences); including synonyms, and with the addition of a filter to limit results to the UK where available [ 53 ]. To expedite translation of search strings across different databases, searches prioritised free text search strings (including proximity operators), in order to retrieve relevant terms where they occurred in titles, abstracts or any other indexing field (including subject headings). The searches of ASSIA and IBSS (via ProQuest) and Social Sciences Citation Index (via Web of Science) used a simplified strategy adapted from those reproduced in Additional File 1. Database searching was accompanied by scrutiny of reference lists of included papers and relevant systematic reviews (within search dates), and grey literature searching (see Supplementary Table 1, Additional File 2), which was conducted and documented using processes outlined by Stansfield et al . [ 54 ].
Inclusion criteria
We included qualitative studies, including qualitative elements of mixed methods studies from published and grey literature (excluding dissertations and non-searchable books), that explored the impact of housing insecurity, defined according to the Children’s Society [ 15 ] definition (which includes actual or perceived insecurity related to housing situations), on immediate and short-term outcomes related to childhood mental and physical health and wellbeing (up to the age of 16), among families experiencing / at risk of housing insecurity in the UK (including low-income families, lone-parent families, and ethnic minority group families including migrants, refugees and asylum seekers). Informants could include children and young people themselves, parents / close family members, or other informants with insight into the children and young people’s experiences. Children and young people outside a family unit (i.e., who had left home or were being looked after by the local authority) and families from Roma and Irish Traveller communities were excluded, as their circumstances are likely to differ substantially from the target population.
Study selection
Search results from electronic databases were downloaded to a reference management application (EndNote). The titles and abstracts of all records were screened against the inclusion criteria by one of three reviewers and checked for agreement by a further reviewer. Full texts of articles identified at abstract screening were screened against the inclusion criteria by one reviewer. A proportion (10%) of papers excluded at the full paper screening stage were checked by a second reviewer. Any disagreements were resolved through discussion.
Grey literature searches and screening were documented in a series of tables [ 54 ]. One reviewer (of two) screened titles of relevant web pages and reports against the inclusion criteria for each web platform searched, and downloaded and screened the full texts of potentially eligible titles. Queries relating to selection were checked by another reviewer, with decisions discussed among the review team until a consensus was reached.
One reviewer (of two) screened reference lists of included studies and relevant reviews for potentially relevant papers. One reviewer downloaded the abstracts and full texts of relevant references and assessed them for relevance.
Data extraction
We devised a data extraction form based on forms that the team has previously tested for similar reviews of public health topics. Three reviewers piloted the extraction form and suggested revisions were agreed before commencing further extraction. Three reviewers extracted and tabulated key data from the included papers and grey literature sources, with one reviewer completing data extraction of each study and a second reviewer formally checking a 10% sample for accuracy and consistency. The following data items were extracted: author and year, location, aims, whether housing insecurity was an aim, study design, analysis, who the informants were, the housing situation of the family, reasons for homelessness or housing insecurity, conclusion, relevant policy/practice implications and limitations. Any qualitative data relating to housing insecurity together with some aspect of health or wellbeing in children and young people aged 0–16 years were extracted, including authors’ themes (to provide context), authors’ interpretations, and verbatim quotations from participants. We sought to maintain fidelity to author and participant terminologies and phrasing throughout.
Quality appraisal
Peer-reviewed academic literature was appraised using the Critical Appraisal Skills Programme (CASP) checklist for qualitative studies [ 55 ] and the quality of grey literature sources (webpages and reports) was appraised using the Authority, Accuracy, Coverage, Objectivity, Date, Significance (AACODS) checklist [ 56 ]. Because of concerns about the lack of peer review and/or the absence of a stated methodology, it was decided to use the AACODS tool that extends beyond simple assessment of study design. A formal quality assessment checklist was preferred for journal articles that passed these two entry criteria. One reviewer performed quality assessment, with a second reviewer formally checking a 10% sample for accuracy and consistency.
Development of the conceptual framework
Prior to undertaking the current review, we undertook preliminary literature searches to identify an appropriate conceptual framework or logic model to guide the review and data synthesis process. However, we were unable to identify a framework that specifically focused on housing insecurity among children and young people and that was sufficiently broad to capture relevant contexts, exposures and impacts. We therefore developed an a priori conceptual framework based on consultation with key policy and practice stakeholders and topic experts and examination of key policy documents (see Fig. 1 ).
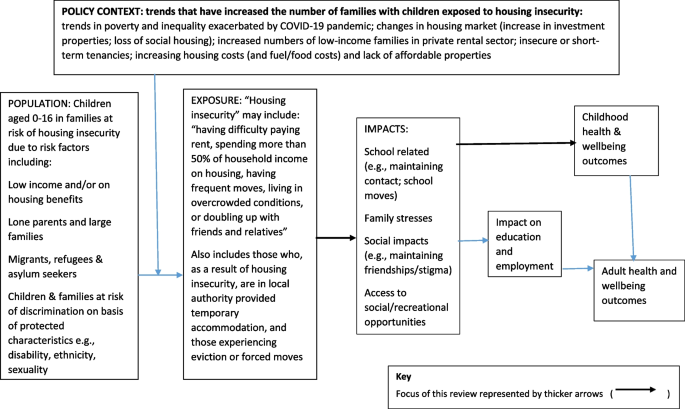
A priori conceptual framework for the relationship between housing insecurity and the health and wellbeing of children and young people
We initially consulted policy experts who identified relevant organisations including research centres, charities and other third sector organisations. We obtained relevant policy reports from organisational contacts and websites, including Child Poverty Action Group (CPAG), Crisis, Joseph Rowntree Foundation (JRF) and HACT (Housing Association Charitable Trust), NatCen (People Living in Bad Housing, 2013), the UK Collaborative Centre for Housing Evidence (CaCHE), and the Centre on Household Assets and Savings Management (CHASM) (Homes and Wellbeing, 2018). We also identified a key report on family homelessness from the Children’s Commissioner (Bleak Houses. 2019) and a joint report from 11 charities and advocacy organisations published by Shelter (Post-Covid Policy: Child Poverty, Social Security and Housing, 2022). We also consulted local authority officers with responsibility for housing and their teams in two local councils and third sector providers of housing-related support to young people and families (Centrepoint). Stakeholders and topic experts were invited to comment on the potential focus of the review and the appropriate definitions and scope for the ‘exposure’ (unstable housing), the population (children and young people) and outcomes (health and wellbeing). Exposures relate to how children and families experience housing insecurity, impacts are intermediate outcomes that may mediate the effects of housing insecurity on health and wellbeing (e.g., the psychological, social, and environmental consequences of experiencing housing insecurity), and outcomes are childhood health and wellbeing effects of housing insecurity (including the effects of the impacts/intermediate outcomes).
The contextual factors and main pathways between housing-related factors and the health and wellbeing of children and young people identified were incorporated into the initial conceptual framework. We then used this conceptual framework to guide data synthesis.
Data synthesis
We adopted a dual approach whereby we synthesised data according to the a priori conceptual framework and sought additional themes, categories and nuance inductively from the data, in an approach consistent with the second stage of ‘best fit framework synthesis’ [ 57 , 58 ]. We analysed inductive themes using the Thomas and Harden [ 59 ] approach to thematic synthesis, but coded text extracts (complete sentences or clauses) instead of coding line by line [ 60 , 61 ].
First, one reviewer (of two) coded text extracts inductively and within the conceptual framework, simultaneously, linking each relevant text extract to both an inductive code based on the content of the text extract, and to an element of the conceptual framework. We assigned multiple codes to some extracts, and the codes could be linked to any single element or to multiple elements of the conceptual framework. During the process of data extraction, we identified four distinct populations, and coded (and synthesised) data discretely for each population. We initially coded data against the ‘exposure’, ‘impacts’ and ‘outcomes’ elements of the conceptual framework, however we subsequently added a further element within the data; ‘protective factors’. One reviewer then examined the codes relating to each element of the conceptual framework and grouped the codes according to conceptual similarity and broader meaning, reporting the thematic structure and relationships between concepts apparent from the text extracts both narratively and within a diagram to illustrate hypothesised causal pathways within the original conceptual framework, to highlight links between specific exposures, impacts and outcomes for each population. While we synthesised the findings by population initially, and present separate diagrams for each population, we present overall findings in this manuscript due to several similarities and then highlight any important differences for the domestic violence, migrant/refugee/asylum seeker, and relocation populations.
Study selection and included studies
Here we report the results of our three separate searchers. First, the database searches generated 3261 records after the removal of duplicates. We excluded 3025 records after title and abstract screening, examined 236 full texts, and included 16 peer-reviewed papers (reporting on 16 studies). The reasons for exclusion of each paper are provided in the Supplementary Table 2, Additional File 3. Second, we examined 726 grey literature sources (after an initial title screen) and included 37 papers. Third, we examined 85 papers that we identified as potentially relevant from the references lists of included papers and relevant reviews, and included six (two of which were peer-reviewed publications). Figure 2 summarises the process of study selection and Table 2 presents a summary of study characteristics. Of the included studies, 16 took place across the UK as a whole, one was conducted in England and Scotland, one in England and Wales and 17 in England. In terms of specific locations, where these were reported, 13 were reported to have been conducted in London (including specific boroughs or Greater London), two in Birmingham, one in Fife, two in Glasgow, one in Leicester, one in Rotherham and Doncaster, and one in Sheffield. The location of one study was not reported (Table 2 ).
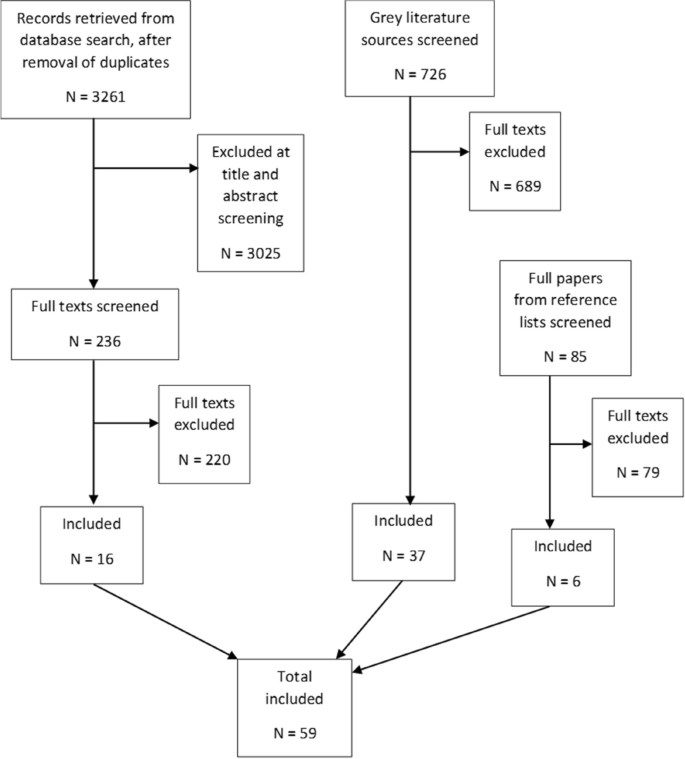
Flow diagram of study selection
We identified four distinct populations for which research evidence was available during the process of study selection and data extraction:
General population (evidence relating to housing insecurity in general) (reported in 40 papers);
Domestic violence population (children and young people experiencing housing insecurity associated with domestic violence) (reported in nine papers);
Migrant, refugee and asylum seeker population (children and young people experiencing housing insecurity associated with migration status) (reported in 13 papers);
Relocation population (evidence relating to families forced to relocate due to planned demolition) (reported in two papers).
Evidence relating to each of these populations was synthesised separately as the specific housing circumstances may impact health and wellbeing differently and we anticipated that specific considerations would relate to each population. Some studies reported evidence for more than one population.
Quality of evidence
The quality of evidence varied across the studies, with published literature generally being of higher quality than grey literature and containing more transparent reporting of methods, although reporting of methods of data collection and analysis varied considerably within the grey literature. All 18 peer-reviewed studies reported an appropriate methodology, addressing the aim of the study with an adequate design. Eleven of the 18 peer-reviewed studies reported ethical considerations, and only two reported reflexivity. Most studies had an overall assessment of moderate-high quality (based on the endorsement of most checklist items) and no studies were excluded based on quality. Most of the grey literature originated from known and valued sources (e.g., high-profile charities specialising in poverty and housing, with the research conducted by university-based research teams). Although methodologies and methods were often poorly described (or not at all), primary data in the form of quotations was usually available and suitable to contribute to the development of themes within the evidence base as a whole. Quality appraisals of included studies are presented in Supplementary Tables 3 and 4, Additional File 4.
Housing insecurity and the health and wellbeing of children and young people
The updated conceptual framework for the impact of housing insecurity on the health and wellbeing of children aged 0–16 years in family units is presented in Fig. 3 for the general population, Fig. 4 for the domestic violence population, Fig. 5 for the refugee/migrant/asylum seeker population, and Fig. 6 for the relocation population (arrows represent links identified in the evidence and coloured arrows are used to distinguish links relating to each element of the model). Table 3 outlines the themes, framework components and studies reporting data for each theme.
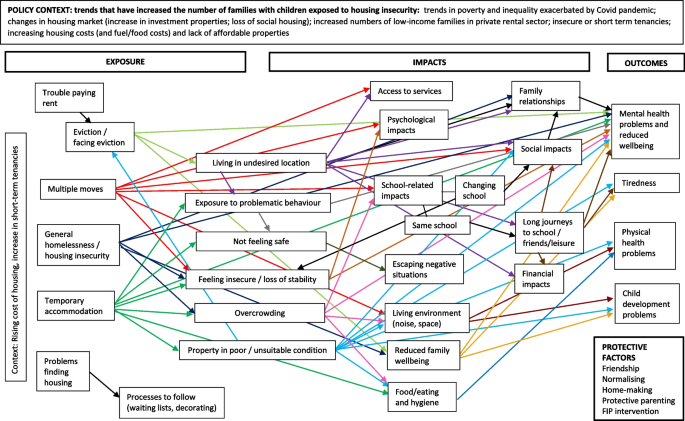
Conceptual framework for the relationship between housing insecurity and health and wellbeing in the general population
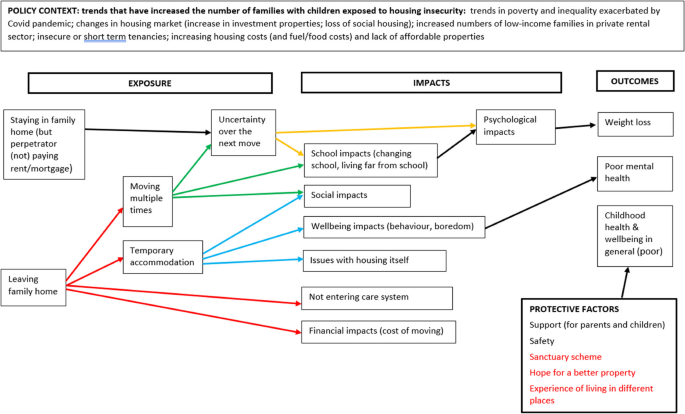
Conceptual framework for the relationship between housing insecurity and health and wellbeing in the domestic violence population
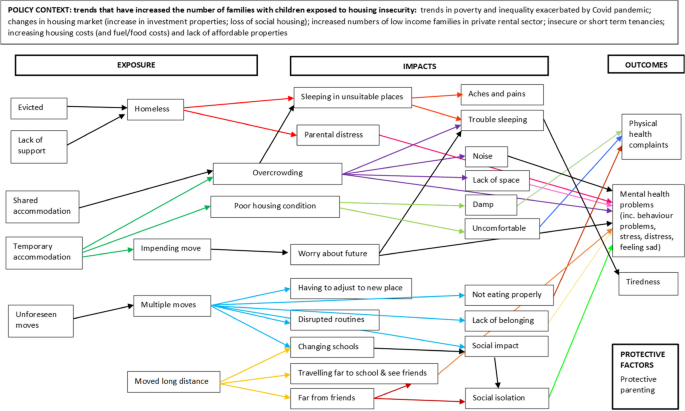
Conceptual framework for the relationship between housing insecurity and health and wellbeing in the migrant, refugee and asylum seeker population
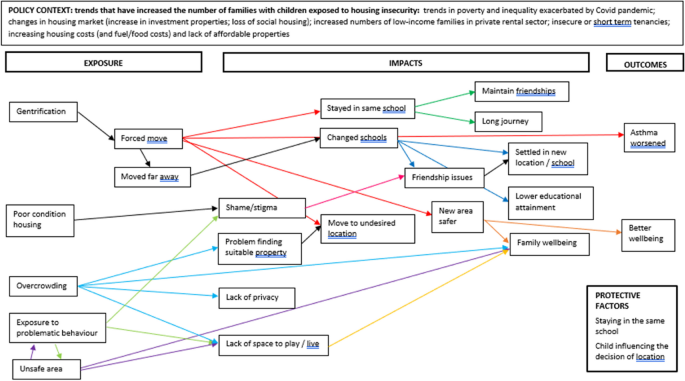
Conceptual framework for the relationship between housing insecurity and health and wellbeing in the relocation population
Exposures are conceptualised as the manifestations of housing insecurity – that is, how the children and young people experience it – and housing insecurity was experienced in multiple and various ways. These included trouble paying for housing, eviction or the prospect of eviction, making multiple moves, living in temporary accommodation, and the inaccessibility of suitable accommodation.
Fundamentally, a key driver of housing insecurity is poverty. Parents and, in some cases, young people cited the high cost of housing, in particular housing benefit not fully covering the rent amount [ 116 ], trouble making housing payments and falling into arrears [ 15 , 92 , 97 ]. Sometimes, families were evicted for non-payment [ 15 , 102 ], often linked to the rising cost of housing [ 109 ] or loss of income [ 102 ]. Some children and young people were not aware of reasons for eviction [ 90 ], and the prospect of facing eviction was also a source of housing insecurity [ 116 ].
The cost of housing could lead to families having to move multiple times [ 116 ], with lack of affordability and the use of short-term tenancies requiring multiple moves [ 109 , 116 ]. Children and young people were not always aware of the reasons for multiple moves [ 15 ]. Multiple moves could impact upon education and friendships [ 77 , 82 ].
Living in temporary housing was a common experience of housing insecurity [ 15 , 71 , 87 , 90 , 94 , 98 , 111 , 112 , 113 , 114 ]. Temporary housing caused worry at the thought of having to move away from school and friends [ 91 ] and acute distress, which manifested as bedwetting, night waking and emotional and behavioural issues at school [ 66 ]. Living in a hostel for a period of time could lead to friendship issues due to not being able to engage in sleepovers with friends [ 102 ].
The inaccessibility of suitable accommodation also contributed to insecurity. Sometimes, when a family needed to move, they had to fulfil certain requirements, for instance, to decorate their overcrowded 3-bedroom accommodation to be eligible for a more suitable property [ 15 ]. Further, some families encountered the barrier of landlords who would not accept people on benefits [ 15 , 85 , 117 ]. Waiting lists for social housing could be prohibitively long [ 97 , 98 , 116 ].
Dual exposures and impacts
Some phenomena were found to be both exposures and impacts of housing insecurity, in that some issues and experiences that were impacts of housing insecurity further exacerbated the living situation, causing further insecurity. These included not feeling safe, exposure to problematic behaviour, living far away from daily activities, overcrowding, and poor or unsuitable condition properties.
Not feeling safe was frequently reported by children and young people, and by parents in relation to the safety of children and young people. Parents and children and young people described being moved to neighbourhoods or localities [ 15 , 69 , 87 , 90 , 103 ] and accommodation [ 87 , 97 , 109 , 112 , 113 , 114 ] that did not feel safe. For one family, this was due to racial abuse experienced by a parent while walking to school [ 69 ]. In one case, a young person’s perception of safety improved over time, and they grew to like the neighbours and area [ 15 ], although this was a rare occurrence.
Often, this experience of being unsafe was due to exposure to problematic behaviour in or around their accommodation, including hearing other children being treated badly [ 112 ], being exposed to violence (including against their parents) [ 111 , 112 , 114 ], witnessing people drinking and taking drugs [ 69 , 83 , 90 , 111 , 112 , 114 ], finding drug paraphernalia in communal areas [ 112 , 114 ] or outside spaces [ 69 ], hearing threats of violence [ 111 ], hearing shouting and screaming in other rooms [ 114 ], witnessing people breaking into their room [ 83 ], and witnessing their parent/s receiving racist abuse and being sworn at [ 83 ].
‘There’s a lot [of] drugs and I don’t want my kids seeing that… One time he said ‘mummy I heard a woman on the phone saying ‘I’m going to set fire to your face’’ She was saying these things and my son was hearing it.’ ( [ 111 ] , p.15)
Another impact related to the family and children and young people being isolated and far away from family, friends, other support networks, work, shops, school and leisure pursuits due to the location of the new or temporary housing [ 15 , 83 , 87 , 97 , 104 , 109 ]. This affected education, friendships, finances and access to services (see ‘ Impacts ’).
Overcrowding was another issue that was both a source or feature of housing insecurity, as this created a need to move, as well as being an impact, in that families moved to unsuitable properties because they had little alternative. Overcrowding was largely a feature of temporary accommodation that was too small for the family [ 67 , 91 ], including hostels/shared houses where whole families inhabited one room and washing facilities were shared [ 100 , 102 ]. In turn, overcrowding could mean siblings sharing a room and/or bed [ 15 , 41 , 64 , 71 , 78 , 109 , 111 , 112 , 113 , 114 , 116 ] (which could lead to disturbed sleep [ 15 ]), children/young people or family members sleeping on the floor or sofa [ 15 , 71 , 102 , 110 ] (which caused aches and pains in children/young people; [ 100 ]), children/young people sharing a room with parents [ 64 , 71 , 94 , 109 , 111 , 112 , 113 , 114 ], a room being too small to carry out day to day tasks [ 112 , 113 , 114 ], a lack of privacy in general (e.g., having to change clothes in front of each other) [ 70 , 111 , 112 , 114 ], living in close proximity to other families [ 114 ], and cramped conditions with little room to move when too many people and possessions had to share a small space [ 15 , 64 , 90 , 97 , 103 , 109 , 114 ].
It’s all of us in one room, you can imagine the tension…. everyone’s snapping because they don’t have their own personal space …it’s just a room with two beds. My little brother has to do his homework on the floor.’ ( [ 97 ] , p..43)
It was thus difficult for children and young people to have their own space, even for a short time [ 98 ], including space to do schoolwork [ 102 , 103 ], play [ 91 ] or invite friends over [ 103 ]. Families sometimes ended up overcrowded due to cohabiting with extended family [ 110 ] or friends [ 91 , 102 ] (‘hidden homelessness’). Other families outgrew their property, or anticipated they would in future, when children grew older [ 70 , 116 ]. Overcrowding sometimes meant multiple families inhabiting a single building (e.g., a hostel or shelter), where single parents had difficulties using shared facilities, due to not wanting to leave young children alone [ 100 ]. Overcrowding could also lead to children feeling unsafe, including being scared of other people in shared accommodation [ 102 ], experiencing noise [ 102 ], and feeling different from peers (due to not having their own room or even bed) [ 102 ]. Living in overcrowded conditions could lead to, or exacerbate, boredom, aggressive behaviour, and mental health problems among children and young people (see ‘ Outcomes ’) [ 72 , 79 , 91 ]. Overcrowded conditions caused a ‘relentless daily struggle’ for families ([ 83 ], p.48).
Similarly, the need to take whatever property was on offer led to families living in properties in poor condition, which in turn could exacerbate housing insecurity, both because families needed to escape the poor condition housing and because they were reluctant to complain and ask for repairs on their current property in case the landlord increased the rent or evicted them [ 86 , 96 ]. Eviction was perceived as a real threat and families described being evicted after requesting environmental health issues [ 74 ] and health and safety issues [ 116 ] be addressed. Families experienced issues relating to poor condition properties, including accommodation being in a poor state of decoration [ 98 ], broken or barely useable fixtures and fittings [ 86 , 90 , 96 ], no laundry or cooking facilities [ 102 ], no electricity [ 67 ], no or little furniture [ 67 , 102 ], broken appliances [ 71 , 96 , 97 ], structural failings [ 97 ], unsafe gardens [ 90 ], mould [ 71 , 90 , 96 , 97 , 104 , 109 ], and bedbugs and/or vermin [ 67 , 76 , 77 ]. Even where the property condition was acceptable, accommodation could be unsuitable in other ways. Many families with young children found themselves living in upper floor flats, having to navigate stairs with pushchairs and small children [ 71 , 74 , 78 , 83 , 87 , 92 , 109 ]. One study reported how a family with a child who had cerebral palsy and asthma were refused essential central heating and so had to request a property transfer [ 75 ]. Lack of space to play was a particular issue in relation to temporary accommodation, often due to overly small accommodation or a vermin infestation [ 80 , 87 , 91 ]. In small children, the effects included health and safety risks [ 87 , 112 ] and challenges keeping them occupied [ 112 ]. In older children and young people, a lack of space meant a lack of privacy [ 63 , 112 ]. School holidays could be particularly challenging, particularly when outside play spaces were unsuitable due to safety concerns (e.g., people selling drugs, broken glass) [ 87 , 106 ], and some temporary accommodation restricted access during the daytime [ 112 ]. With shared temporary accommodation, such as a refuge or hostel, came the threat of possessions being removed by others [ 80 ].
Impacts are defined here as intermediate outcomes that may mediate the effects of housing insecurity on health and wellbeing, for instance, the psychological, social, and environmental consequences of experiencing housing insecurity. According to the evidence reviewed, these were overwhelmingly negative, with only a very small number of positive impacts, and, in many cases, these were offset by other negative impacts. Impacts on friendships, education, family relationships, diet, hygiene, access to services, feelings of being different, feelings of insecurity, parental wellbeing, the financial situation of the family, experiences of noise, leaving negative situations behind, and other impacts, such as leaving pets behind and time costs, were noted. Overlaying all of the above was a lack of choice and control experienced by the children/young people and their families.
A particularly large and disruptive impact of housing insecurity was the effect on friendships and social networks. Over multiple moves, children and young people faced the challenge of building new social networks and reputations each time [ 15 , 90 , 106 ], and worried about maintaining existing friendships [ 90 ]. The beneficial side to this was the potential to have friends all over town, although this was offset by difficulty in forming close friendships due to frequent moves [ 15 ]. Children and young people in temporary, overcrowded or poor condition accommodation often felt ashamed of their housing and concealed it from their friends [ 15 , 73 , 78 , 111 , 112 , 114 , 115 ], and in one case missing out on sleepovers with friends [ 102 ]. Moving far from friends presented difficulties in maintaining friendships and a social life, leading to boredom and isolation [ 102 , 114 ]. The threat of an impending long-distance move could cause sadness and worry [ 114 ] and young people missed the friends they had left behind [ 15 , 90 ]. Other associated social impacts of housing insecurity exacerbated by the wider experience of poverty included turning turn down invitations to go out with friends for financial reasons [ 115 ] or to avoid leaving a parent alone with younger sibling/s [ 114 ], and feeling different from peers, either because of looking unkempt or lacking in confidence [ 115 ].
Another key impact of housing insecurity was the effect on education, and this was closely intertwined with friendship impacts. Faced with moving, often multiple times, sometimes to uncertain locations, families were faced with the decision to keep the same school or to change schools. Multiple moves and/or an unfeasibly long journey to school, led to either a decision to, or anticipating the prospect of having to, change schools [ 15 , 66 , 90 , 91 , 102 , 106 , 108 , 111 , 116 ]. This could in turn impact on the child’s sense of stability, academic performance and friendships [ 90 , 105 , 106 , 111 , 115 , 116 ] and make them feel sad [ 102 ]. In the case of one family, staying at the same school during a move resulted in decreased educational attainment [ 69 ].
Staying at the same school created some stability and allowed for friendships and connections with teachers and the school to be maintained [ 15 , 102 ]. This was, however, quite often the only option, due to the family not knowing their next location, and thus which school they would be near [ 15 , 102 , 113 ], and was not without issues. Those who were unhappy with school were thus effectively prevented from changing schools due to housing insecurity [ 15 , 90 ]. Families were often re-housed at a considerable distance from the school [ 15 , 70 , 93 , 94 , 113 ]. This meant having to get up very early for a long journey by public transport [ 15 , 66 , 70 , 77 , 88 , 90 , 94 , 102 , 105 , 106 , 111 , 113 ], which also caused problems maintaining friendships [ 115 ], increased tiredness and stress [ 15 , 66 , 77 , 102 , 111 , 113 , 114 , 115 ] and left little time for homework and extra-curricular activities [ 113 , 114 , 115 ]. Some children and young people stayed with friends or relatives closer to school on school nights, although these arrangements were not sustainable longer-term [ 15 , 90 ].
Living in temporary housing was associated with practical challenges in relation to schooling, for instance, keeping track of uniform and other possessions, limited laundry facilities, and limited washing facilities [ 112 , 115 ]. Parents noted academic performance worsened following the onset of housing problems [ 111 , 113 , 116 ]. Limited space and time to do homework or revision [ 111 , 112 , 113 , 114 , 115 ], tiredness and poor sleep [ 111 , 113 ], travelling and disrupted routines [ 114 ], disruptions from other families (e.g. in a hostel) [ 114 ], a lack of internet connection [ 114 ], and the general impact of the housing disruption [ 111 , 113 , 116 ] made it challenging for those experiencing housing insecurity to do well at school. Families often had to wake up early to access shared facilities in emergency accommodation before school [ 113 , 114 ]. Some children and young people missed school altogether during periods of transience, due to multiple moves rendering attendance unviable [ 71 , 106 , 111 ], lack of a school place in the area [ 109 ], or not being able to afford transport and lunch money [ 81 ], which in turn affected academic performance [ 106 , 111 ].
‘Their education was put on hold. My daughter was ahead on everything in her class and she just went behind during those two weeks.’ ([ 111 ] , p.15)
Children and young people also experienced an impact on immediate family relationships. Housing insecurity led to reduced family wellbeing [ 82 ], and family relationships becoming more strained, for instance, due to spending more time at friends’ houses that were far away [ 15 ]. In some cases, however, housing insecurity led to improved family relationships, for instance, in terms of a non-resident father becoming more involved [ 15 ], or children feeling closer to their parents [ 106 ].
Some impacts related to the child’s health and wellbeing. Impacts on diet were reported, including refusal of solid food (which affected growth) [ 113 ], stress and repeated moves leading to not eating properly (which resulted in underweight) [ 91 ], insufficient money to eat properly [ 15 , 99 , 106 ], a lack of food storage and preparation space [ 102 , 103 , 112 ], and a hazardous food preparation environment [ 112 ]. Unsuitable temporary accommodation, including converted shipping containers, hostels, B&Bs and poorly maintained houses were particularly likely to be associated with a wide range of other well-being related impacts. Unsuitable accommodation presented various problems, including excessive heat, dripping water, overcrowding, damp, dirt, electrical hazards, vermin, flooding and a lack of washing and laundry facilities [ 41 , 67 , 71 , 74 , 76 , 77 , 81 , 87 , 88 , 102 , 104 , 106 , 109 , 112 , 116 ]. Moving could also impact on access to services and continuity of care, including being unable to register with general practitioners [ 82 ], and difficulty in maintaining continuity of medical care [ 65 ].
Psychological impacts of housing insecurity included feeling different from peers [ 115 ], feeling disappointed in each new property after being initially hopeful [ 15 ], and having trouble fitting in, in a new area [ 15 ]. Feeling insecure (including uncertainty over when and where the next move will be, or if another move is happening) was a further impact of living in insecure housing situations (including temporary housing, making multiple moves, being evicted) [ 15 , 87 , 90 , 114 , 116 ], leading to stress and worry [ 15 , 114 ].
One of the major issues that [she] says affects her mental health is the uncertainty of their situation. She says it is hard to not know where they will be staying one night to the next. It is also difficult to adjust to living without her furniture and clothes ( [ 114 ] , p.17)
Multiple moves, or anticipating a move, disrupted children and young people’s sense of continuity and led to the experience of a loss of security and stability more generally [ 15 , 85 , 87 ]. This led children and young people to feel responsible for helping and providing support to their parents, including hiding their feelings [ 111 , 114 ], or not requesting things be bought [ 15 , 113 ]. Children and young people also felt a sense of displacement and a lack of belonging [ 15 , 115 ]. Loss of stability and security triggered a desire for stability, to be able to settle, have friends over, and not have to worry about moving [ 109 ].
Housing insecurity also had a negative effect on parent-wellbeing, and this impacted the wellbeing of young people both directly [ 15 , 65 , 102 , 106 ] and indirectly through increased arguments and family stress [ 15 , 93 ] and reduced parental ability to care for children with chronic conditions [ 41 ]. Parents also perceived their reduced wellbeing as negatively impacting their children's development [ 41 ]. The threat of sanctions for missed housing payment could lead to reduced well-being among the whole family, characterised by feelings of despair, failure and a loss of hope [ 93 ].
Moving also had a financial impact on families. Moving into much smaller temporary accommodation meant that possessions had to be left behind, with the family having to pay for decorating, carpets, curtains and furniture each time they moved [ 15 , 84 , 98 , 104 , 105 ], incurring considerable debt [ 98 ]. If the new location was far away from school, family, friends and, in some cases, shops, then the family incurred travel costs [ 15 , 87 , 94 , 112 , 114 ]. Because of all this, children and young people’s requests for possessions or experiences (e.g., trips out) were refused [ 113 ].
Excessive noise was another disruption that children and young people experienced in connection with their precarious housing situation. Sources of noise were traffic on a main road [ 15 ] a factory nearby [ 110 ], or from other people in a B&B, hotel, hostel, or neighbouring properties [ 15 , 91 , 102 , 106 , 112 ], and could disrupt sleep and daily activities.
If their current conditions were sufficiently bad, some children and young people felt positively about moving, to leave negative things behind. For instance, a move could take them close to friends [ 15 ] or they may have more space in the new property [ 15 ]. Quite often, however, negative impacts of moving seemed to offset any benefit [ 90 ].
Frequent moves could impact on children and young people’s health and wellbeing in other ways. Space might be even more squeezed by cardboard boxes in preparation for an impending move [ 15 ]. Some children reported having to leave beloved pets behind [ 90 ]. Time costs associated with moving meant less time for other activities [ 15 ]. Multiple moves, particularly across local authority boundaries, could impact the family’s access to services [ 41 , 71 ], including health services [ 90 ], specialist healthcare required to manage children’s health conditions [ 83 ], and social services [ 85 , 93 ].
One key impact that overlaid all of the above but was rarely mentioned was a lack of choice or control [ 109 ]. This was inherent in the families’ and children/young people’s accounts of their experiences of housing insecurity, through talk of not knowing where their next move would be or when, and having to move long distances away from the places they used frequently and the people who supported them. Even the journey into housing insecurity was often outside of families’ control, such as increases in rent, change in income, or eviction notices (see ‘ Exposure ’). Families often could not improve properties in poor condition because they could not afford repairs to properties in poor condition, so felt they had to live with these problems [ 90 ]. Some families avoided reporting problems to the landlord for fear of a rent increase or eviction (see ‘ Exposure ’). Children and young people in particular felt that they lacked control over their housing situation, and in some cases were not aware of reasons for moves [ 15 ].
Several childhood health and wellbeing outcomes have been documented in relation to, and they are overwhelmingly negative. These consisted of mental health problems, physical health problems, tiredness, and stunted child development. Living in temporary housing, making multiple moves, and the instability and insecurity associated with anticipating a move, or being uncertain whether a move would be needed, had an obvious negative impact on the mental health of children and young people [ 41 , 63 , 79 , 107 ], including in terms of self-harm [ 71 , 96 , 97 , 107 , 111 ], thoughts of suicide [ 71 ], anxiety [ 71 , 90 , 103 , 111 , 112 , 115 ], and depression [ 110 , 115 ]. Sometimes these problems manifested as physical pain [ 106 ], nightmares [ 84 ], night waking [ 107 ], or wetting the bed [ 63 , 107 , 111 ]. Stress, anger, isolation, fear, worry about the future (including about having to move again), worry about safety and acute distress were also reported [ 15 , 63 , 73 , 79 , 82 , 84 , 89 , 90 , 96 , 109 , 114 , 115 , 118 ]. One child with distress/mental health problems (as a result of having to make multiple moves) stopped eating properly (resulting in underweight and anaemia), and became socially withdrawn [ 79 ]. Another child reported weight loss and mental health problems due to worry about the future housing situation [ 95 ]. One study reported on stress and anxiety in children due to the trauma of losing their home and the emergency accommodation being unsuitable and temporary [ 111 ].
‘My six year old has been going to the doctors because he’s developed a nervous tick since we’ve been in that room. He was constantly nervous all the time. He’s so unsettled still and he knows that we’re still not settled. He’s really anxious. He’s become violent […]’ ( [ 111 ] , p.13)
Sometimes children and young people’s mental health issues would be displayed through problematic behaviour such as withdrawal, stealing, smoking, drug-taking, aggressive behaviour, and running away [ 68 , 71 , 79 , 84 , 97 , 107 , 114 , 115 ]. Teachers observed that younger children tended to get more withdrawn and older children and young people tended to get more angry and antagonistic, although the same child could cycle between these two states [ 115 ]. Separation anxiety was also reported [ 87 , 111 ].
Children and young people also experienced physical health problems as a result of living in temporary accommodation, poor condition housing, and making multiple moves, including the development or exacerbation of asthma [ 69 , 81 , 90 ] and eczema [ 41 , 81 , 90 , 111 ], stomach bugs [ 71 ], insect bites [ 112 ], infectious diseases [ 41 , 109 , 112 ], headaches [ 113 ], stomach aches [ 109 , 113 ], exacerbation of long-term conditions [ 41 , 75 , 109 ], rashes and asthma as a result of damp [ 100 ], a dermatological condition as a result of living in a hotel [ 91 ], other physical symptoms in young children, such as coughing and vomiting [ 100 ] and musculoskeletal pain from sleeping in unsuitable places [ 102 ]. One study reported illness in a baby following a difficult birth, attributed to housing-related stress in the mother [ 83 ]. Rarer outcomes included weight gain due to a lack of cooking facilities and thus reliance on fast food, weight loss due to stress [ 79 , 95 ] and head lice due to close contact with others [ 115 ]. Some properties presented risk of injury to babies and young children [ 41 ].
Tiredness was also reported, in relation to travelling a long distance to school and to visit family and friends [ 15 , 66 , 77 , 102 , 112 , 115 ]. Tiredness also resulted from poor quality sleep due to the unsuitable nature of the accommodation (e.g., poor state of repair, overcrowded), sleeping on a sofa [ 102 ], and worrying about the housing situation [ 15 , 41 , 87 , 109 , 112 , 114 ].
Impacts on the perceived development of young children were reported, in particular in relation to having no space to play, which impacted standing/walking and emotional development [ 87 , 111 ], and multiple moves, which impacted on potty training and speech development [ 87 , 111 ]. One study reported an impact on growth due refusal of solid food [ 113 ].
Protective factors
Protective factors were not presented in the original conceptual framework. However, we identified specific protective factors that were perceived to lessen the impact of housing insecurity on wellbeing among children and adolescents. These included friendship, keeping the same school, normalising housing insecurity, home-making, having a plan, hope, protective parenting, and some interventions.
Friendship was a key protective factor. Retaining connections with friends and peer networks following moves was important [ 15 , 90 ], and school facilitated this [ 114 ]. Indeed, another related strategy was to keep children and young people enrolled in the same school during and after moves, to retain some stability [ 15 , 70 , 90 , 108 ].
Some sources noted that children and young people tended to normalise and destigmatise their housing insecurity as something to be expected given that the family is poor or receives benefits [ 15 , 62 , 90 ]. This response could be a coping/defence mechanism to try to deal with the negative impacts of being insecurely housed.
Another, more positive, coping strategy was to make the property feel more like a home. For instance, decorating the property could lead to children and young people feeling more settled and ‘at home’, even if the ultimate intention was to move [ 15 ]. Further coping strategies included having a plan of how things could go to keep anxiety at bay and retain some control [ 15 ], seeing the advantages of a location [ 15 ], and hoping for a better house next time, and/or hoping that the family would settle in a permanent home [ 15 ].
Parents also acted to protect children and young people from the negative impacts of housing insecurity, by concealing the full extent of their financial and housing problems [ 113 ], including children and young people in decision-making [ 70 , 90 ] (for instance, allowing children and young people to influence their parents’ decisions on location, where there was a choice [ 70 ]), and presenting their situation as an adventure [ 114 ]. One study also documented parents taking their children out to parks to give them space to run around [ 91 ].
Lastly, some positive findings were reported by an evaluation of the Families Intervention Project (FIP), for families at risk of eviction due to anti-social behaviour [ 118 ]. Families that worked closely with a multi-agency team experienced increased housing security, reduced stress and anxiety, and fewer behavioural problems among the children [ 118 ]. Another study reported positive effects of a peer-led parenting programme on children’s behaviour, although it is unclear how this impacted on their health and wellbeing [ 64 ].
Key findings relating to other populations
Families that have experienced domestic violence.
Domestic violence could be a source of housing insecurity both for families who leave the family home to seek safety and for those who stay. Families that leave can end up moving multiple times (and frequently), perhaps initially to a refuge and then into other forms of temporary housing, with families experiencing uncertainty over when the next move would be [ 90 , 105 ]. One study reported that experience of living in different places was perceived to be beneficial, although little detail was given, and this was offset by difficulty building peer networks [ 90 ]. In one family, the alternative to housing insecurity was for the children to be placed in local authority care, which was avoided through the children and other parent leaving the perpetrator [ 90 ].
Among families who stay in the family home (with the perpetrator leaving), housing insecurity could be created by the perpetrator refusing to pay the mortgage, leaving the family worried and uncertain:
‘ I’ve lost two stone, my son has lost ten pounds – he is only 15 – he is having counselling at school. It has just been a nightmare…He hasn’t paid the mortgage for a year because he wants to get me out so he can have the money… ’ ([ 95 ], p. 68). Friendship was particularly impacted among this population. To prevent the perpetrator from finding them, children were not able to disclose personal information [ 63 ]. This made it difficult to form close friendships.
Parents reported a lack of support offered to children and young people, including services that they needed [ 80 ]. However, where support was offered to parents and children/young people who had moved to escape abuse in their previous home, this support could improve wellbeing [ 63 , 79 , 80 ], acting as a protective factor. Particular forms of useful support included a parenting course [ 79 ] and supportive staff and peers at hostels [ 80 ]. Hostels offered a feeling of safety due to closed-circuit television [ 80 ]. One study reported that refuge and hostel staff were perceived as helpful but powerless to keep families safe in some cases, although children and young people found it helpful to talk and open up to staff about their situation [ 63 ]. One intervention, the Sanctuary scheme, allowed people experiencing/at risk of domestic violence to remain in their own home, with additional security [ 95 ].
Migrant, refugee and asylum seeker families
Migrant, refugee and asylum seeker families experienced similar forms of housing insecurity and similar impacts on everyday life and childhood health/wellbeing as did the general population. However, migrant/refugee families reported having to move suddenly, with very little notice (e.g., 48 h) [ 77 , 82 ]. They also lacked support from services and assistance with housing from the local authority. Consequently, families would end up homeless and have to beg friends to let them sleep on their sofas [ 101 ].
Once homeless, families slept in unsuitable locations, such as on the night bus, in a church, and in the waiting room of the Accident and Emergency (A&E) department. This led to extreme tiredness; in some cases, children were too tired to attend school [ 102 ]. That type of homelessness was a particular feature of the experience of housing insecurity among this population.
‘We had to keep going to McDonalds every night and we would also go to A&E. I would have to wear my school clothes and sleep like that.… They would say we have to sleep where the people wait but it’s just like lights […] The chairs were hard.’ (child aged 9) ( [ 102 ] , p. 22)
Other considerations specific to migrant/refugee/asylum seeker families were language barriers, which compounded the challenge of adjusting to a new area [ 82 ], and pressure to cook British food rather than food from their home country in communal facilities [ 106 ].
Families forced to relocate due to demolition
Two papers identified from the database search examined experiences of relocation; families were living in local authority accommodation in Glasgow and experienced a forced move as the high-rise block of flats they lived in was due to be demolished [ 69 , 70 ]. This forced location creates housing insecurity.
Despite the common source, however, housing insecurity was experienced in different ways by different families. One family reported not wanting to move as the children liked the area and their school and nursery, and one family was offered a flat but needed outdoor space [ 70 ]. Many families experienced the pre-relocation area as unsafe due to problematic behaviour in outdoor shared areas [ 69 ]. Because of this and no access to a private garden children lacked space to play [ 70 ]. Families also reported feeling shame in relation to the local area and the poor condition of their pre-relocation housing (a high-rise block of flats), and were keen to move to a less stigmatising area with better condition housing [ 69 , 70 ].
Most families managed to relocate to areas close enough for their children and young people to attend the same schools. However two families changed schools [ 69 , 70 ]. Children and young people felt shame and stigma relating to the local area and the flats themselves, with many young people reluctant to invite friends over, or others socialising in the corridor without inviting friends inside [ 70 ]. Thus, relocation could have positive impacts on families and children/young people. For three families, moving was a positive experience, with children and young people enjoying having a garden and growing to like their new neighbours and the area [ 69 ].
Although we anticipated potentially different experiences, impacts and outcomes relating to housing insecurity across the four populations, the evidence reviewed suggests many similarities. Some exposures were common to multiple populations, for instance, being evicted or having a forced move, living in temporary accommodation, experiencing overcrowding, exposure to problematic behaviour, poor condition/unsuitable property, and making multiple moves. Common impacts included social, school-related, psychological, financial and family wellbeing impacts, having to travel long distances to attend school and see friends, having to live in a property that was unsuitable or in a poor state of repair, overcrowded and often noisy, all of which could then further exacerbate housing insecurity. Outcomes reported across multiple populations included mental health problems (which could manifest in physical ways, for example, trouble eating and sleeping, or wetting the bed) and physical health problems such as skin complaints and asthma related to poor housing conditions. Protective factors common to multiple populations included friendship and support, staying at the same school, having hope for the future, and parenting practices. Pervasive throughout all populations and accounts was an overall lack of choice or control over the housing situation and poverty as a driving force.
These findings support and build upon previous literature that has examined the impact of housing insecurity on the health and wellbeing of children and young people, in terms of reduced mental and psychological wellbeing [ 21 , 42 , 43 ], ill health relating to homelessness or poor housing conditions [ 40 , 41 ], and disrupted family processes [ 38 ]. Likewise, the findings build upon prior cohort studies that support a causal relationship with child health [ 38 ], by highlighting the details of the hardships faced by children and young people experiencing housing insecurity and exploring relationships between exposures, ‘less tangible’ impacts and health and wellbeing outcomes.
Many elements of the Children’s Society definition of housing insecurity were identifiable in our review findings. A key element of housing insecurity is financial insecurity [ 17 , 19 ]; this was borne out in our findings where families were frequently exposed to high/rising costs of housing or reduced income. Indeed, our review found that families incurred additional costs due to multiple and/or frequent moves and/or moving into temporary accommodation. This could potentially increase financial insecurity, thus creating a vicious circle of housing insecurity and poverty. Having ‘a home that does not provide a sense of safety and security’ ([ 18 ], paragraph 3) was evident when children and young people reported not feeling safe in their accommodation, and relational insecurity was evident in families’ accounts of being moved far from friends, school and support networks.
In addition, we identified certain population-specific considerations. Families experiencing domestic violence faced a difficult choice between choosing to remain in the property and leaving the property, both with insecurity attached. Housing insecurity negatively impacted on friendships for all populations, however this could be potentially more challenging for those escaping domestic violence, due to the need to keep personal information confidential in order to maintain family safety.
Parents and children/young people in migrant, refugee and asylum seeker populations spoke of having very little notice before having to move out of a property, sometimes only 48 h. This created a housing emergency, captured in accounts of families becoming homeless and having to sleep in unsuitable places, such as the Accident and Emergency department waiting room or on a night bus. In some families, parents had no recourse to public funds, so even when children and young people were born in the UK, the family still ended up destitute and homeless, leading to significant worry.
A key factor in relocation was that families were forced to move by a particular date, as the high-rise block they lived in was scheduled for demolition. Many families desired a move, due to a lack of space, overcrowding, and unsafe outdoor spaces. However many did not want to leave behind social networks and schools in the community, and even some who wanted to move had difficulty finding a suitable property (e.g., for their family size).
A key challenge to synthesising the evidence was the complexity of the data, in particular the relationships between exposures and impacts. Factors that families initially experienced as exposures could then become impacts, and particular impacts could then worsen housing insecurity, in a cyclical fashion. For instance, overcrowded conditions could precipitate a move, but then the only property available may be in a poor state of repair, with intolerable living conditions, thus prompting a further move. Another key challenge in synthesising the qualitative evidence was that many elements of the experience of housing insecurity that were experienced simultaneously by children and young people have been artificially separated within the updated conceptual frameworks, making analysis problematic. For instance, those living in poor-condition temporary accommodation may want to move due the poor state of a property, but be worried about where they may end up next and whether children/young people will have to change schools and move far from friends. Such complexity has proved challenging to our overall synthesis. Policymakers and practitioners should be aware that the diagrams illustrating the hypothesised causal pathways simplify the multiple inter-related factors related to housing insecurity that impact on the wellbeing of children and young people. Identifiable common stresses including poverty, financial difficulties and debt, immigration/refugee status and domestic abuse will also exert direct significant effects on family wellbeing that prove difficult to separate from those directly due to housing insecurity.
Limitations
Limitations of the evidence base.
We have identified numerous literature sources, many rich with data relating to the experiences of children and young people, and synthesised these data into diagrams that illustrate hypothesised causal pathways within the original conceptual framework, with accompanying descriptions of the experiences of housing insecurity in children and young people. However, we cannot establish claims for the comprehensiveness of our diagrams that map hypothesised causal pathways from housing insecurity to childhood health/wellbeing based on the original conceptual framework. We mapped associations where they were present in the accounts of children/young people and other informants. However, the evidence base may have missed other potential associations, particularly for populations covered by a small number of studies.
Within the evidence base, accounts from parents or other informants proved extremely useful in examining the impacts of housing insecurity on the health and wellbeing of children and young people, particularly for younger children who are not able to yet articulate their experiences and feelings. Nevertheless, such accounts proved an insufficient substitute for rich and nuanced data directly from the children and young people themselves. Our public involvement group have informed us that children and young people may find it difficult to talk about their housing situation, and noted that we did not identify any research that explicitly examined the perspectives of young people who provide care for a parent.
Likewise, little available information relates to the health and wellbeing of children and young people, and it is difficult to establish whether the evidence we have reviewed has captured all relevant health and wellbeing experiences. The majority of the accounts of young people focused on the impacts (or intermediate outcomes) of housing insecurity, which means that we have been able to present a rich picture of these ‘less tangible’ impacts, but also that the links from these impacts to health and wellbeing outcomes is less well understood. For instance, our public involvement group noted that we had not reported any evidence relating to bullying as a result of experiencing housing insecurity.
Strengths and limitations of the review
Strengths of our review method include the prior use of a conceptual model, developed in consultation with stakeholders and topic experts, and examination of key policy documents, which guided the process of synthesis. Synthesis was thus both deductive (i.e., informed by the a priori conceptual model) and inductive (i.e., conducted using established thematic synthesis methods), which allowed for an organised and yet rich and nuanced picture of the impacts of housing insecurity on health and wellbeing among children and young people in the UK. The review was conducted by an established team of experienced reviewers and a methodologist.
A key limitation is that literature sources were far more plentiful than anticipated, including numerous long and detailed reports identified through grey literature searching. While this enhanced the richness of the dataset, it also expanded the review workload, leading to additional time constraints. Limited time and resource could be allocated for double-checking full texts (in particular in the grey literature) and extractions, and thus only a sample were double-checked. Time constraints also prevented citation searches of key included studies. Nevertheless, such an approach remains consistent with established rapid review methods with minimal consequences for missing or mis-reported evidence [ 50 , 51 , 52 ]. Time and resource constraints also prohibited examination of how experiences may differ according to location within the UK.
Implications for policy
It is important that decisions made about housing at a national and local level reflect the impacts that insecure housing can have on children and young people, and ensures that housing insecurity is prevented in the first place. The current review findings suggest that policies should focus on reducing housing insecurity in its totality among families. One way to do this is to focus on eviction, which is a significant cause of instability and a leading cause of households seeking homelessness assistance [ 25 ]. This could include ending no-fault evictions, as has been done in Scotland for private renters since 2017 and as proposed, but yet to be introduced by the UK government in 2019. Scotland’s introduction of longer tenancy agreements with the removal of no-fault evictions may also facilitate families being able to settle and reduce the need for multiple moves. Similarly, legislating for minimum standards in the private rented sector, as currently being explored [ 119 ], will protect children and young people from being exposed to unhealthy and dangerous conditions.
Other changes could include (1) stipulating minimum requirements for space in family properties and minimum requirements for property conditions; (2) advocating for families living in the private rental sector to improve their housing situation; (3) reducing the use of short-term tenancies so families are not required to make multiple moves; (4) providing affordable housing options that give families more choice; and (5) engaging families in the design of systems and services that meet their housing needs. Addressing poverty more widely should also help to alleviate housing insecurity among families in the UK, as much of the evidence reported on how poverty initiated and/or exacerbated housing insecurity, for instance, by restricting choice and by increasing worry. However, any changes will need adequate support for enforcement, something made clear by the limited effectiveness of policy introduced to protect people from revenge/retaliatory eviction [ 97 , 120 , 121 , 122 ], improve the quality and suitability of temporary accommodation, and, where possible, reduce the need for temporary accommodation through preventative measures.
Among families escaping domestic violence, support systems are needed to avoid destitution caused by the perpetrator (e.g., not paying the mortgage). There should also be systems in place to ensure that families are housed in a permanent residence as soon as possible following the initial placement in emergency temporary accommodation after leaving the family home, with as few moves as possible. Appropriate support with housing should be made available to refugee/asylum seeker/migrant families, including those where the parents have no recourse to public funds, and short-notice and long-distance moves should be avoided, particularly where these take families away from their support systems and communities.
Implications for practice
Where possible, interventions to reduce or eliminate housing insecurity should be implemented. Where this is not possible, interventions should focus on reducing the impact of housing insecurity, for instance, by ensuring long journeys can be avoided, that accommodation is of a decent standard, and by providing adequate support to families and children young people. Practitioners who work to house families should prioritise stable, suitable and good quality housing. Practitioners who interact with children and young people experiencing housing insecurity and homelessness (e.g., clinicians, teachers, social workers) should recognise the complexity of the children and young people’s experiences, including how the situation and circumstances (e.g., escaping domestic violence, migration status) might impact on their health and wellbeing, and that impacts vary on an individual basis, particularly in assessments and family support plans. A multiagency approach should be utilised with families to mitigate the impacts of housing insecurity, poor housing conditions or unsuitable housing. Practitioners should consider the impacts of continuity of school, support and services, and the need for mental health support, parenting and counselling, for instance through providing support with transport to enable children and young people to stay at their current school, and support to maintain friendships. All those working with children/young people and families experiencing housing insecurity should consider ways to offer them optimal choice and control over situations that affect them.
All practitioners and professionals (e.g., teachers) who work with children and young people from families who have escaped domestic violence should ensure that the children and young people are receiving appropriate support from all relevant services, and that appropriate safety measures are in place to protect the family from the perpetrator.
Research recommendations
Future qualitative research could focus explicitly on the health and wellbeing of children and young people experiencing housing insecurity, and how they link with the impacts and outcomes identified in the current review. In particular, research could explore how the health and wellbeing of children and young people are affected by the impacts of housing insecurity on friendships, education, food and hygiene, financial impacts, long journeys, overcrowding, perceived safety, and access to services. Further qualitative research could examine the impact of interventions to address housing insecurity among families in the UK. Interventions with a participatory component that seek to ensure that the voices of children and young people remain central should be prioritised for further research. The voices of specific groups of young people who are likely to be marginalised (e.g., young carers) could be explored in future research. Future qualitative research should report methods of recruitment and data collection and analysis clearly and transparently, and should incorporate meaningful research reflexivity.
Conclusions
Housing insecurity has a profound impact on children and young people in families in the UK. Such housing insecurity can take many forms and result from often inter-related situations that are fundamentally connected to poverty. The resultant housing insecurity can have multiple (often simultaneous) impacts, including those that relate to educational, psychological, financial and family wellbeing impacts, having to travel long distances to attend school and see friends, and having to live in unsuitable, poorly repaired, overcrowded or noisy properties, any of which further exacerbate housing insecurity. Negative experiences can impact on health and wellbeing, in terms of mental health problems (which could manifest in physical ways) and physical health problems, as well as tiredness and developmental issues. Some experiences and situations can lessen the impact of housing insecurity on the health and wellbeing of children and young people. Negative impacts of housing insecurity on health and wellbeing may be further compounded by specific situations and life circumstances, such as escaping domestic violence, being a migrant, refugee or asylum seeker (or having a parent with that status), or experiencing a forced relocation due to housing demolition.
Availability of data and materials
All data presented in this review were already published, either in an academic journal, or a report that is publicly available. Search strings are available in Additional File 1. Data extracted from the published papers and reports included in the current study are available from the corresponding author on request.
the main social security payment in the UK; for more information see https://www.gov.uk/universal-credit

Abbreviations
Accident and Emergency (Department)
Authority, Accuracy, Coverage, Objectivity, Date, Significance
Applied Social Sciences Index and Abstracts
Bed and Breakfast (accommodation)
Critical Appraisal Skills Programme
Coronavirus Disease 2019
Families Intervention Project
United Kingdom
International Bibliography of the Social Sciences
National Institute for Health and Care Research
International prospective register of systematic reviews
Davey Smith G, Hart C, Blane D, Hole D. Adverse socioeconomic conditions in childhood and cause specific adult mortality: Prospective observational study. BMJ. 1998;316:1631–5.
Article Google Scholar
Swope CB, Hernandez D. Housing as a determinant of health equity: A conceptual model. Soc Sci Med. 2019;243: 112571.
Article PubMed PubMed Central Google Scholar
Weitzman M, Baten A, Rosenthal DG, Hoshino R, Tohn E, Jacobs DE. Housing and child health. Curr Probl Pediatr Adolesc Health Care. 2013;43(8):187–224.
PubMed Google Scholar
Kohler L. Child public health: A new basis for child health workers. Eur J Public Health. 1998;8:253–5.
Cresswell T. What is child public health? Curr Paediatr. 2004;14(7):612–8.
Braubach M, Jacobs DE, Ormandy D. Environmental burden of disease associated with inadequate housing. Copenhagen: WHO Regional Office for Europe; 2011.
Google Scholar
Clair A. Housing: an Under-Explored Influence on Children’s Well-Being and Becoming. Child Indic Res. 2019;12:609–26.
Dockery M, Kendall G, Li J, Mahendran A, Ong R, Strazdins L. Housing and children’s development and wellbeing: a scoping study. AHURI Final Report No. 149. Melbourne: Australian Housing and Urban Research Institute Limited; 2010.
Evans GW, Saltzman H, Cooperman JL. Housing quality and children’s socioemotional health. Environ Behav. 2001;33(3):389–99.
Gehrt D, Hafner M, Grollov ST, Christoffersen J, editors. Impacts of the indoor environment in our homes and schools on child health: A novel analysis using the EU-SILC Database. 17th International Healthy Buildings Conference; 2021 21–23 June 2021; Oslo: SINTEF Academic Press.
Mansour A, Bentley R, Baker E, Li A, Martino E, Clair A, et al. Housing and health: an updated glossary. J Epidemiol Community Health. 2022;76(9):833–8.
Article PubMed Google Scholar
World Health Organization. Housing and health guidelines. Geneva: World Health Organization; 2018.
Shaw M. Housing and public health. Ann Rev Public Health. 2004;25:397–418.
Clark WAV. Life events and moves under duress: disruption in the life course and mobility outcomes. Longitudinal Life Course Stud. 2016;7(3):218–39.
The Children’s Society. Moving, Always Moving: The normalisation of housing insecurity among children in low income households in England. London: The Children’s Society; 2020.
Burgard SA, Seefeldt KS, Zelner S. Housing instability and health: findings from the Michigan Recession and Recovery Study. Soc Sci Med. 2012;75(12):2215–24.
Kushel MB, Gupta R, Gee L, Haas JS. Housing instability and food insecurity as barriers to health care among low-income Americans. J Gen Intern Med. 2006;21(1):71–7.
Public Health England. Improving health through the home. 2017. Available from: https://www.gov.uk/government/publications/improving-health-through-the-home/improving-health-through-the-home . Accessed Aug 2022.
Preece J, Bimpson E. Housing and Insecurity and Mental Health in Wales. Glasgow: CaCHE, University of Glasgow; 2019.
Jelleyman T, Spencer N. Residential mobility in childhood and health outcomes: A systematic review. J Epidemiol Community Health. 2008;62(7):584–92.
Article CAS PubMed Google Scholar
Glasheen C, Forman-Hoffman V, Hedden S, Ridenour T, Wang J, Porter J. Residential transience among US adolescents: association with depression and mental health treatment. Epidemiol Psychiatr Sci. 2019;28(6):682–91.
Article CAS PubMed PubMed Central Google Scholar
National Children’s Bureau. Housing and the health of young children: policy and evidence briefing for the VCSE sector. 2016. Available from: https://www.ncb.org.uk/sites/default/files/uploads/files/Housing%2520and%2520the%2520Health%2520of%2520Young%2520Children.pdf . Accessed Aug 2022.
Office of Disease Prevention and Health Promotion. Housing Instability. 2020. Available from: https://wayback.archive-it.org/5774/20220414161055/https://www.healthypeople.gov/2020/topics-objectives/topic/social-determinants-health/interventions-resources/housing-instability . Accessed Aug 2022.
Harris J, McKee J. Health and wellbeing in the private rented sector. Part 1: Literature review and policy analysis. Bristol: UK Collaborative Centre for Housing Evidence (CaCHE); 2021.
Wilson W, Cromarty H. Applying as homeless from an assured shorthold tenancy (England). House of Commons Library Briefing Paper No. 06856; 2020. https://commonslibrary.parliament.uk/research-briefings/sn06856/ . Accessed Aug 2022.
Cheetham M, Moffatt S, Addison M, Wiseman A. Impact of Universal Credit in North East England: a qualitative study of claimants and support staff. Bmj Open. 2019;9:e029611. https://doi.org/10.1136/bmjopen-2019-029611 . Accessed Aug 2022.
Williams R, Bell A, Garratt E, Pryce G. Understanding the effect of universal credit on housing insecurity in England: a difference-in-differences approach. Hous Stud. 2022. https://doi.org/10.1080/02673037.2022.2146066 .
Hardie I. Welfare reform and housing insecurity: the impact of Universal Credit rollout on demand for rent arrears and homelessness advice from Citizens Advice in England. Soc Policy Soc. 2022. https://doi.org/10.1017/S1474746422000379 .
Gov.uk Benefit cap: number of households capped to May 2023. 2023. https://www.gov.uk/government/statistics/benefit-cap-number-of-households-capped-to-may-2023 . Accessed Aug 2022.
Gov.uk Benefit cap: estimated impact on parents, by age of youngest child 2017. https://www.gov.uk/government/statistics/benefit-cap-estimated-impact-on-parents-by-age-of-youngest-child . Accessed Aug 2022.
Department for Work and Pensions (DWP). Benefit Cap Data to February 2018. 2018. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/704234/benefit-cap-statistics-feb-2018.pdf . Accessed Aug 2022.
Hilditch M. One in three councils took children into care due to homelessness. Inside Housing. 2016. Available from: https://www.insidehousing.co.uk/news/news/one-in-three-councils-took-children-into-care-due-to-homelessness-48690 . Accessed Aug 2022.
Child Poverty Action Group. Post-Covid Policy: Child Poverty, Social Security and Housing. London: Child Poverty Action Group; 2021.
Fairbrother H, Woodrow N, Crowder M, Holding E, Griffin N, Er V, et al. “It All Kind of Links Really”: Young People’s Perspectives on the Relationship between Socioeconomic Circumstances and Health. Int J Environ Res Public Health. 2022;19(6):3679.
Joseph Rowntree Foundation. As 400,000 renters face evictions, JRF warns the UK risks a two-tier recovery. 2021. Available from: https://www.jrf.org.uk/news/as-400000-renters-face-eviction-jrf-warns-the-uk-risks-a-two-tier-recovery . Accessed Aug 2022.
Broadbent P, Thomson R, Kopasker D, McCartney G, Meier P, Richiardi M, et al. The public health implications of the cost-of-living crisis: outlining mechanisms and modelling consequences. Lancet Regional Health Eur. 2023; 27:100585. https://doi.org/10.1016/j.lanepe.2023.100585 . Accessed Aug 2022.
Allard M. “I don’t know what the winter’s going to bring:” experiences of homelessness during a cost of living crisis. London: Crisis; 2022.
Bess K, Miller A, Mehdipanah R. The effects of housing insecurity on children’s health: a scoping review. Health Promotion Int. 2022;38(3):daac006. https://doi.org/10.1093/heapro/daac006 . Accessed Aug 2022.
Li Y, Bentley R, Singh A, Fleitas Alfonzo A, editors. Housing disadvantage in childhood and health: a systematic review. Society for Social Medicine Annual Scientific Meeting. J Epidemiol Commun Health. 2021;50(Suppl 1):dyab168.384. https://doi.org/10.1093/ije/dyab168.384 . Accessed Aug 2022.
Rolfe S, Garnham L, Godwin J, Anderson I, Seaman P, Donaldson C. Housing as a social determinant of health and wellbeing: developing an empirically-informed realist theoretical framework. Bmc Public Health. 2020;20(1):1138. https://doi.org/10.1186/s12889-020-09224-0 . Accessed Aug 2022.
Royal College of Paediatrics and Child Health. Poverty and child health: views from the frontline. London: Royal College of Paediatrics and Child Health; 2017.
Rollings KA, Wells NM, Evans GW, Bednarz A, Yang Y. Housing and neighborhood physical quality: Children’s mental health and motivation. J Environ Psychol. 2017;50:17–23.
Suglia SF, Chambers E, Sandel MT. Poor housing quality and housing instability. In: The social determinants of mental health. VA, United States: American Psychiatric Publishing; 2015. p. 171–92.
Cutts DB, Meyers AF, Black MM, Casey PH, Chilton M, Cook JT, et al. US housing insecurity and the health of very young children. Am J Public Health. 2011;101(8):1508–14.
Dong M, Anda RF, Felitti VJ, Williamson DF, Dube SR, Brown DW, et al. Childhood residential mobility and multiple health risks during adolescence and adulthood: the hidden role of adverse childhood experiences. Arch Pediatr Adolesc Med. 2005;159(12):1104–10.
Brown D, Benzeval M, Gayle V, Macintyre S, O’Reilly D, Leyland AH. Childhood residential mobility and health in late adolescence and adulthood: findings from the West of Scotland Twenty-07 Study. J Epidemiol Commun Health. 2012;66(10):942–50.
Article CAS Google Scholar
Pearce A, Elliman D, Bedford H, Law C. Residential mobility and uptake of childhood immunisations: Findings from the UK Millennium Cohort Study. Vaccine. 2008;26(13):1675–80.
Clair A, Reeves A, McKee M, Stuckler D. Constructing a housing precariousness measure for Europe. J Eur Soc Policy. 2019;29(1):13–28.
Bone J. Neoliberal nomads: Housing insecurity and the revival of private renting in the UK. Sociological Research Online. 2014;19(4):1–4.
Kelly S, Moher D, Clifford T. Defining rapid reviews: A modified Delphi consensus approach. Int J Technol Assess Health Care. 2016;32(4):265–75.
Tricco AC, Antony J, Zarin W, Strifler L, Ghassemi M, Ivory J, et al. A scoping review of rapid review methods. BMC Med. 2015;13(1):1–15.
Tricco AC, Zarin W, Antony J, Hutton B, Moher D, Sherifali D, et al. An international survey and modified Delphi approach revealed numerous rapid review methods. J Clin Epidemiol. 2016;70:61–7.
Ayiku L, Levay P, Hudson T, Finnegan A. The NICE UK geographic search filters for MEDLINE and Embase (Ovid): Post-development study to further evaluate precision and number-needed-to-read when retrieving UK evidence. Res Synthesis Methods. 2020;11:669–77.
Stansfield C, Dickson K, Bangpan M. Exploring issues in the conduct of website searching and other online sources for systematic reviews: how can we be systematic? Syst Rev. 2016;5:191. https://doi.org/10.1186/s13643-016-0371-9 . Accessed Aug 2022.
Critical Appraisal Skills Programme. CASP Qualitative Checklist [online]. Critical Appraisal Skills Programme; 2022. Available from: https://casp-uk.net/casp-tools-checklists/ . Accessed Sept 2022.
Tyndall J. AACODS Checklist.: Flinders Univeristy; 2010. Available from: https://dspace.flinders.edu.au/xmlui/bitstream/handle/2328/3326/AACODS_Checklist.pdf?sequence=4&isAllowed=y . Accessed Sept 2022.
Carroll C, Booth A, Cooper K. A worked example of "best fit" framework synthesis: A systematic review of views concerning the taking of some potential chemopreventive agents. BMC Med Res Methodol. 2011;11:29. https://doi.org/10.1186/1471-2288-11-29 . Accessed Aug 2022.
Shaw L, Nunns M, Briscoe S, Anderson R, Thompson CJ. A “Rapid Best-Fit” model for framework synthesis: Using research objectives to structure analysis within a rapid review of qualitative evidence. Res Synt Methods. 2021;12(3):368–83.
Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol. 2008;8:45. https://doi.org/10.1186/1471-2288-8-45 . Accessed Aug 2022.
Gudde CB, Olsø TM, Whittington RSV. Service users’ experiences and views of aggressive situations in mental health care: a systematic review and thematic synthesis of qualitative studies. J Multidisciplinary Healthcare. 2015;3(8):449–62.
Levitt HM. How to conduct a qualitative meta-analysis: Tailoring methods to enhance methodological integrity. Psychother Res. 2018;28(3):367–78.
Backett-Milburn K, Cunningham-Burley S, Davis J. Contrasting lives, contrasting views? understandings of health inequalities from children in differing social circumstances. Soc Sci Med. 2003;57(4):613–23.
Bowyer L, Swanston J, Vetere A. “Eventually you just get used to it”: An interpretative phenomenological analysis of 10–16 year-old girls’ experiences of the transition into temporary accommodation after exposure to domestic violence perpetrated by men against their mothers. Clin Child Psychol Psychiatry. 2015;20(2):304–23.
Bradley C, Day C, Penney C, Michelson D. “Every day is hard, being outside, but you have to do it for your child”: Mixed-methods formative evaluation of a peer-led parenting intervention for homeless families. Clin Child Psychol Psychiatry. 2020;25(4):860–76.
Centre CCL. Growing Up In A Hostile Environment: The rights of undocumented migrant children in the UK. London: Coram Children’s Legal Centre; 2013.
Dexter Z, Capron L, Gregg L. Making Life Impossible: How the needs of destitute migrant children are going unmet. London: The Children’s Society; 2016.
Jolly A. No Recourse to Social Work? Statutory Neglect, Social Exclusion and Undocumented Migrant Families in the UK. Soc Inclusion. 2018;6(3):190–200.
Karim K, Tischler V, Gregory P, Vostanis P. Homeless children and parents: Short-term mental health outcome. Int J Soc Psychiatry. 2006;52(5):447–58.
Lawson L, Kearns A, Egan M, Conway E. “You Can’t Always Get What You Want…”? Prior-Attitudes and Post-Experiences of Relocation from Restructured Neighbourhoods. Housing Studies. 2015;30(6):942–66.
Lawson L, Kearns A. “Power to the (young) people”? Children and young people’s empowerment in the relocation process associated with urban re-structuring. Int J Hous Policy. 2016;16(3):376–403.
Minton A, Jones S. Generation squalor: Shelter’s national investigation into the housing crisis. London: Shelter; 2005.
Moffatt S, Lawson S, Patterson R, Holding E, Dennison A, Sowden S, et al. A qualitative study of the impact of the UK “bedroom tax.” J Public Health. 2016;38(2):197–205.
Nettleton S, Burrows R. When a capital investment becomes an emotional loss: The health consequences of the experience of mortgage possession in England. Hous Stud. 2000;15(3):463–79.
Office of the Deputy Prime Minister. Causes of homelessness amongst ethnic minority populations. London: Office of the Deputy Prime Minister; 2005.
Oldman C, Beresford B. Home, sick home: Using the housing experiences of disabled children to suggest a new theoretical framework. Hous Stud. 2000;15(3):429–42.
Price J, Spencer S. Safeguarding children from destitution: Local authority responses to families with “no recourse to public funds.” Oxford: Centre on Migration, Policy and Society, University of Oxford; 2015.
Rowley L, Morant N, Katona C. Refugees Who Have Experienced Extreme Cruelty: A Qualitative Study of Mental Health and Wellbeing after Being Granted Leave to Remain in the UK. J Immigr Refug Stud. 2020;18(4):357–74.
Thompson C, Lewis DJ, Greenhalgh T, Smith NR, Fahy AE, Cummins S. “I don’t know how I’m still standing” a Bakhtinian analysis of social housing and health narratives in East London. Soc Sci Med. 2017;177:27–34.
Tischler V, Karim K, Rustall S, Gregory P, Vostanis P. A family support service for homeless children and parents: users’ perspectives and characteristics. Health Soc Care Community. 2004;12(4):327–35.
Tischler V, Rademeyer A, Vostanis P. Mothers experiencing homelessness: mental health, support and social care needs. Health Soc Care Community. 2007;15(3):246–53.
Tod AM, Nelson P, De Chavez AC, Homer C, Powell-Hoyland V, Stocks A. Understanding influences and decisions of households with children with asthma regarding temperature and humidity in the home in winter: A qualitative study. BMJ Open. 2016;6(1):e009636.
Warfa N, Bhui K, Craig T, Curtis S, Mohamud S, Stansfeld S, et al. Post-migration geographical mobility, mental health and health service utilisation among Somali refugees in the UK: A qualitative study. Health Place. 2006;12(4):503–15.
Watt P. Gendering the right to housing in the city: Homeless female lone parents in post-Olympics, austerity East London. Cities. 2018;76:43–51.
Wilcox P. Lone motherhood: the impact on living standards of leaving a violent relationship. Social Policy & Administration. 2000;34(2):176–90.
Young Women’s Trust. On the edge: Life for young women on low incomes in London. London: Young Women’s Trust; 2020.
Children’s Commissioner for England. Changing the odds in the early years. London: Children’s Commissioner for England; 2017.
Children’s Commissioner for England. Bleak houses: Tackling the crisis of family homelessness in England. London: Children’s Commissioner for England; 2019.
Children’s Commissioner. “Are we there yet?” Our rights, our say: A report for the UN Committee on the Rights of the Child. London: Children and Young People’s Commissioner Scotland, Children’s Commissioner for Wales, Northern Ireland Commissioner for Children and Young People, and Children’s Commissioner for England; 2020.
Children’s Commissioner for England. The big ask, the big answer. London: Children’s Commissioner for England; 2021.
The Children’s Society. Understanding childhoods: Growing up in hard times. London: The Children’s Society; 2017.
The Children’s Society. A lifeline for all: Children and families with no recourse to public funds. London: The Children’s Society; 2020.
Child Poverty Action Group and Church of England. Poverty in the pandemic: the impact of coronavirus on lowincome families and children. London: Child Poverty Action Group; 2020.
Child Poverty Action Group. The safety net is gone: Understanding the impact of poverty on the lives of children and families in England: a survey of social workers. London: Child Poverty Action Group; 2020.
Hardy K, Gillespie T. Homelessness, health and housing: Participatory action research in East London. The Sociological Review Foundation: Lancaster; 2016.
Jones A, Bretherton J, Bowles R, Croucher K. The effectiveness of schemes to enable households at risk of domestic violence to remain in their homes: Research report. London: Department for Communities and Local Government; 2010. p. 2010.
Joshi P, Wallace E, Williams L. Young children’s and families’ experiences of services aimed at reducing the impact of low-income: Participation work with children and families. London: Office of the Children’s Commissioner; 2015.
Clarke A, Hamilton C, Jones M, Muir K. Poverty, evictions and forced moves. York: Joseph Rowntree Foundation; 2017.
Croucher K, Quilgars D, Dyke A. Housing and life experiences: making a home on a low income. York: Joseph Rowntree Foundation; 2018.
Joseph Rowntree Foundation. UK Poverty 2020/21: The leading independent report. York: Joseph Rowntree Foundation; 2021.
Action M. Maternal health: Exploring the lived experiences of pregnant women seeking asylum. London: Maternity Action; 2022.
Project 17. “In the night we didn’t know where we were going”: Project 17’s Hotel Fund. London: Project 17; 2018.
Project 17. Not seen, not heard: Children’s experiences of the hostile environment. London: Project 17; 2019.
Royal College of Paediatrics and Child Health. Poverty & Us - parents, carers and young people tell us how poverty impacts them. London: Royal College of Paediatrics and Child Health; 2017.
Renters’ Reform Coalition. Safe, secure and affordable homes for all: A renters’ blueprint for reform: Renters’ Reform Coalition. 2022.
Scottish Women’s Aid. Change, justice, fairness: “Why should we have to move everywhere and everything because of him?” Edinburgh: Scottish Women’s Aid; 2015.
Shelter. Listen up: The voices of homeless children. London: Shelter; 2004.
Shelter. Toying with their future: The hidden cost of the housing crisis. London: Shelter; 2004.
Shelter. Policy: Briefing. Homes fit for families? The case for stable private renting. London: Shelter; 2012.
Shelter. A Roof Over My Head: The final report of the Sustain project. London: Shelter; 2014.
Shelter. Sick and tired: The impact of temporary accommodation on the health of homeless families. London: Shelter; 2004.
Shelter. ‘This is no place for a child’: the experiences of homeless families in emergency accommodation. London: Shelter; 2015.
Shelter. Desperate to escape: the experiences of homeless families in emergency accommodation. London: Shelter; 2016.
Shelter. The experiences of people in housing debt. London: Shelter; 2016.
Shelter. ‘We’ve got no home’: The experiences of homeless children in emergency accommodation. London: Shelter; 2017.
Shelter. Impacts of homelessness on children – research with teachers. London: Shelter; 2017.
Shelter. Building our future: A vision for social housing. London: Shelter; 2018.
Shelter. Health of one in five renters harmed by their home. London: Shelter; 2021. Available from: https://england.shelter.org.uk/media/press_release/health_of_one_in_five_renters_harmed_by_their_home . Accessed Aug 2022.
White C, Warrener M, Reeves A, La Valle I. Family Intervention Projects: An Evaluation of their Design, Set-up and Early Outcomes. London: Department for Children, Schools and Families; 2008. Contract No.: DCSF-RW047.
Gov.uk. A Decent Homes Standard in the private rented sector: consultation. 2022. https://www.gov.uk/government/consultations/a-decent-homes-standard-in-the-private-rented-sector-consultation/a-decent-homes-standard-in-the-private-rented-sector-consultation . Accessed Aug 2022.
Marsh A, Gibb K. The private rented sector in the UK. Glasgow: UK Collaborative Centre for Housing Evidence; 2019.
Moore T, Dunning R. Regulation of the private rented sector in England using lessons from Ireland. York: JRF Report, Joseph Rowntree Foundation; 2017.
Walsh E. Repair in the private rented sector: where now? J Property Plann Environ Law. 2021;13(1):46–59.
Download references
Acknowledgements
We wish to thank Katie Lewis and Liz Kitchin from the University of Sheffield for providing administrative support to the project, Karen Horrocks, from the UK Office for Health Improvement and Disparities, for revising the policy and practice implications, anonymous young people who provided PPI feedback on a lay summary and gave us an insight into key omissions from the evidence base, and Mary Crowder from the University of Sheffield for her support in accessing feedback from PPI members at a local youth organisation. We would also like to thank the policy and practice stakeholders and topic experts with whom we consulted to develop the initial conceptual framework.
This study is funded by the National Institute for Health Research (NIHR) Public Health programme (project reference 18/93 PHR Public Health Review Team). The views expressed are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care.
Author information
Authors and affiliations.
Sheffield Centre for Health and Related Research, University of Sheffield, Sheffield, UK
Emma S. Hock, Lindsay Blank, Hannah Fairbrother, Mark Clowes, Diana Castelblanco Cuevas, Andrew Booth & Elizabeth Goyder
Australian Centre for Housing Research, University of Adelaide, Adelaide, Australia
You can also search for this author in PubMed Google Scholar
Contributions
EH led the review, and undertook study selection, grey literature searching and selection, data extraction, quality assessment and coding, drafted the synthesis, and drafted and refined large parts of the manuscript. LB undertook study selection, data extraction, quality assessment and coding, compiled study characteristics, checked and refined the synthesis, and drafted and refined parts of the manuscript. HF undertook study selection, grey literature searching and selection, data extraction and quality assessment, co-ordinated patient and public involvement, provided topic expertise, checked and refined the synthesis, and drafted and refined parts of the manuscript. MC designed the search strategy, undertook database searches and drafted and refined parts of the manuscript. DCC undertook study selection and drafted and refined parts of the manuscript. AB provided methodological support and advice, checked and refined the synthesis, and drafted and refined parts of the manuscript. AC provided topic expertise and drafted and refined parts of the manuscript. EG undertook stakeholder consultation and protocol development, drafted and refined parts of the manuscript, and was the guarantor of the review. All authors reviewed the manuscript.
Corresponding author
Correspondence to Emma S. Hock .
Ethics declarations
Ethical approval and consent to participate.
Ethical approval was not required for this study because no human participants were involved.
Consent for publication
Not applicable.
Competing interests
AB is a Cochrane author and co-convenor of the Cochrane Qualitative and Implementation Methods Group, and was also previously a member of the NIHR Evidence Synthesis Advisory Group from 2018 to 2022 and a member of the NIHR HS&DR Funding Board from 2018 to 2022. No other authors have competing interests to declare.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., supplementary material 2., supplementary material 3., supplementary material 4., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Hock, E.S., Blank, L., Fairbrother, H. et al. Exploring the impact of housing insecurity on the health and wellbeing of children and young people in the United Kingdom: a qualitative systematic review. BMC Public Health 24 , 2453 (2024). https://doi.org/10.1186/s12889-024-19735-9
Download citation
Received : 22 May 2023
Accepted : 08 August 2024
Published : 09 September 2024
DOI : https://doi.org/10.1186/s12889-024-19735-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Systematic review
- Housing insecurity, Housing instability
- Adolescents
- Young people
BMC Public Health
ISSN: 1471-2458
- General enquiries: [email protected]
Search the website
- Sign up for our latest news
- Annual conference tickets
- Digitally enabled care in the community
- New podcast episode
- Health and care services
Illustrating the relationship between poverty and NHS services
- Public health
- Population health
- Health inequalities
- 18 March 2024
- 19-minute read
- Share to twitter
- Share to linkedin
- Share to facebook
- Share to email
- Share to print
)
Saoirse Mallorie
People living in poverty find it harder to live healthy lives, harder to access NHS services, live with greater illness and die earlier than the rest of the population.
Poverty and the effect it has on health and on the NHS is not new, though the recent rise in deep poverty, cost-of-living increases and high pressure on NHS services are all worsening the problem (6 in 10 of people in the most deprived areas report that the cost-of-living squeeze is impacting their health) and adding to the financial cost to the NHS.
Poverty is a complex problem that will affect different groups in different ways. For example, child poverty is rising particularly sharply, negatively impacting children’s health now and throughout their lives.
NHS staff are also impacted by poverty in different ways. They can experience poverty directly themselves, as well as treating patients who are experiencing the effects of poverty.
Poverty makes it harder for people to access services (nearly one in five low-income adults report skipping essential dental care due to the cost), and services do not always reach those in poverty. This lack of access means people living in poverty are getting sicker and accessing services later – accident and emergency (A&E) attendances are nearly twice as high in the most deprived groups, and emergency admissions 68% higher.
Greater illness and less access to care contribute to worse health outcomes – the mortality rate in the lowest Index of Multiple Deprivation (IMD) decile is almost double that of the highest.
The NHS has a role to play in addressing poverty, both as an employer and as a provider of public services. There are examples of good work under way, such as poverty-proofing services (making sure every stage of the patient pathway is accessible to more deprived groups), but more needs to be done to support better access and better outcomes for those living in poverty.
The NHS can only treat the symptoms of poverty; broader government, economic and civic society action is needed to treat the causes.
Introduction
Currently it is estimated that more than one in five people in the UK are living in poverty. Living in poverty has a profound impact on people’s health and how they use NHS services. From greater prevalence of a wide range of diseases and difficulties in accessing health care, to later treatment and worse health outcomes, poverty affects every stage of the patient journey.
As well as taking a significant toll on individuals, poverty also leads to additional costs for the NHS. In 2016, the Joseph Rowntree Foundation (JRF) estimated the cost of poverty on health care (ie, additional public spending due to greater health care need and use) at £29 billion (£34 billion in current prices ) . Since that report, the situation has got worse: the number of people living in poverty has increased since 2015/16, and the proportion of those people living in deep poverty has risen.
This long read looks at the link between poverty and each of the following:
prevalence of ill health
difficulties accessing health care
late or delayed treatment (and higher NHS costs)
poorer health outcomes.
These four issues can be seen across a wide range of NHS services, from emergency care to dentistry. As well as highlighting this breadth, it is hoped that this long read will provide stimulus for local and NHS leaders to consider the role poverty plays when making plans to manage and improve services. To that end, it signposts some existing resources that may help tackle the issues.
Taking action on this is one of the biggest things we can do to influence and shape health outcomes and inequalities. Senior leader in population health, integrated care board
Methodology
This long read draws on four main sources. First, a literature review of work focusing on the relationship between poverty and health. Second, quantitative analysis of secondary data sources, such as NHS England, the Office for National Statistics (ONS), and the Office for Health Improvement and Disparities (OHID). Third, semi-structured interviews with senior NHS staff working in this space to understand how poverty is impacting on services at the local level and what is being done to tackle it. Fourth, expertise from JRF on poverty and how it has changed over time.
Data analysis notes
Poverty is a complex problem with a range of different definitions. Due to the availability of data, different measures are used throughout this report, including the following.
Relative poverty : the number of people whose post-tax household income, standardised to take different household types and ages into account, is below 60% of national current median income (after housing costs). Deep poverty is defined as less than 50% of median income, and very deep poverty less than 40%.
Index of Multiple Deprivation (IMD): an area-based measure of deprivation, combining income, employment, health, education, crime, barriers to housing and services, living environment.
Income deprivation : a subset of IMD, showing the proportion of people in an area who are out of work or on low earnings.
These measures can be presented in different ways:
percentages of people
deciles, where a population is divided into ten equal groups according to, for example, their income level (so the bottom income decile refers to the 10% of the population with the lowest income)
quintiles, where a population is divided into five equal groups (so the bottom income quintile refers to the 20% of the population with the lowest income).
It is important to acknowledge that there are differences in these measures, particularly between income-specific poverty and IMD. People are defined as being in poverty if they lack sufficient income to meet their needs, whereas people are deprived due to a lack of resources of all kinds, not just income. Both poverty and deprivation have an adverse effect on health, and therefore on the NHS.
There are also differences between people-based measures (relative poverty) and area-based measures (IMD, income deprivation) – for example, there may be people living in an area of high-income deprivation who are not income deprived themselves. Or there may be people whose income does not class them as living in poverty but who are in debt so do experience the problems of poverty.
Even within one measure of poverty there are complexities, as poverty is not static. People move in and out of poverty, and the experience of someone in the bottom IMD quintile may differ substantially from someone experiencing deep and persistent poverty, such as those living in destitution or homelessness.
While this analysis aims to show the impact of poverty on individual-level health and on NHS services (generally in England, though some data is for Great Britain or the United Kingdom), it is important to note that poverty does not operate in isolation. Health and health care are affected by a wide range of factors, including age, sex and ethnicity. This analysis presents the association between measures of poverty and health care activity, rather than attempting to isolate any causal relationship between poverty and health care activity.
Both prevalence and activity data show expressed need – need in terms of the services people use. They do not account for those who need medical care but do not seek it or receive it ( unmet need ). More deprived communities and individuals may have greater need for health care services, but the extent to which this translates into actual use of services (or expressed need) will clearly be affected by the access to and availability of services for these communities and individuals.
Finally, this long read focuses on NHS activity, but it is important to remember that the problems of poverty and deprivation also exist in social care , where data is unfortunately less readily available by measures of deprivation or poverty.
Poverty and prevalence of ill health
Living in poverty makes it harder for people to manage their health well. For example, it is more difficult to eat healthily. If money is short, spending on a healthy diet becomes a substantial expense . In addition, there is a negative relationship between income and access to cooking facilities ( 8% of households with an income below £10,000 per year have no cooker and 16% have no freezer), and a positive relationship between deprivation and the availability of fast-food outlets – nearly one in three food outlets in the most deprived areas are fast food, compared to one in five in the least deprived areas.
It is therefore unsurprising to see a strong relationship between deprivation and poor diet. Given the link between diet and ill health, it is also unsurprising to see a strong relationship between deprivation and a range of diet-related health problems, including cardiovascular disease and diabetes .
Other ways in which being poor negatively impacts health include housing, both in terms of unhealthy or dangerous homes , and difficulties in heating homes properly . Poverty or deprivation can also contribute to mental illness, as struggling to pay bills , afford food or find suitable housing are all inherently stressful.
Although these problems predated the cost-of-living crisis, there are signs that the crisis has worsened the situation. Food insecurity is increasing, and in a 2023 survey, 25% of households in the most deprived quintile of areas reported eating less fruit and fewer vegetables because of cost-of-living increases, compared to 8% of the least deprived quintile. Rising energy bills are also a problem.
)
These issues contribute to the recent increase in very deep poverty, with 6 million people in very deep poverty in 2021/22, up from 4.5 million two decades ago. Approximately 3.8 million people experienced destitution in 2022, 64% higher than 2019. The impact of poverty on health will be even more acute for these people.
Another recent change is the rise in zero-hours contracts and less stable employment, which may also affect health, with a 12 percentage point difference in self-reported good health between employees with good job security and those without.
Child poverty
Childhood has an impact on an individual’s health throughout their life and a childhood lived in poverty has a negative impact . For example, Adverse childhood experiences (ACEs) are correlated with poverty, and negatively impact health in later life, increasing the risk of illnesses from cardiovascular diseases to cancer. Children in deprived areas start to experience health inequalities early on, for example, higher obesity rates, greater exposure to tobacco retailing, and poorer mental health.
These issues impact on children’s health (and therefore on the NHS) in childhood and throughout their lives, and can create a self-perpetuating cycle – children in poorer households may experience poorer health, which limits their education or employment opportunities, which continues to trap families in poverty throughout generations . Childhood illness can also be a trigger to send a family into poverty, for example, if parents have to give up work to care for their child.
It is therefore especially concerning that child poverty is rising . Deep poverty has also risen, with a million destitute children in 2022, 88% higher than 2019. This increase can be seen starkly at the international level. Here, the UK has seen the greatest increase in child poverty rates out of the 39 high or upper middle-income countries in the European Union (EU)/Organization for Economic Cooperation and Development (OECD).
)
Complexity of poverty
That deprivation contributes to greater prevalence of illness, which in turn contributes to higher NHS activity, is intuitively understandable, but this association is not always straightforward. For example, people in more deprived areas, despite being substantially less likely to consume alcohol, or to drink risky amounts (more than 14 units a week), are nearly twice as likely to be admitted to hospital due to alcohol-related problems. Why this happens is not clear . This inverse relationship makes the point that the association between deprivation, prevalence and NHS activity can be complex, and that decreasing the prevalence of an illness or risk factors, while good for people, may not decrease NHS activity.
Another complexity of poverty that makes finding solutions harder is that nobody experiences poverty in isolation – everyone experiences a range of influences on their health, such as their location, age and ethnicity. This is especially problematic for people who belong to multiple marginalised groups , as they often experience additional health disadvantages when their different social inequalities intersect .
NHS staff and poverty
Poverty among NHS staff is a large and growing problem. 71% of providers report that staff struggling to afford to travel to work is a significant issue, and 42% report that staff are struggling to afford to eat at work. This affects staff health, which in turn affects the NHS in terms of increased sickness absence. Recruitment and retention are also a problem, with 68% of providers reporting that staff are moving to other sectors due to the cost of living.
As well as being impacted by poverty directly, staff are affected by dealing with the impact of poverty on their patients. Interviews with NHS stakeholders emphasised the moral injury this causes staff, especially as they can generally only treat the symptoms of poverty rather than the underlying causes. This long read cannot explore this issue more fully, but the impact of both treating and experiencing poverty on NHS staff needs to be acknowledged
We all know the stories about nurses using food banks. But how does working with patients who are in poverty affect staff who feel unable to do anything about it? Senior leader, network of NHS trusts
Poverty and difficulties accessing health care
It might be expected that greater prevalence of ill health in poorer or more deprived groups would lead to higher NHS activity around people in these groups. But this is not always the case, especially at the earlier stages of the patient pathway, such as people accessing services that prevent health conditions deteriorating. There are two sides to this lack of access – barriers that prevent people seeking treatment, and a lack of resources to provide this treatment.
Poverty makes it harder for people to access care
The NHS is reactive to its core, you effectively have to knock on the door and say, ‘I want help’. One of the dilemmas of this space is, how likely is that to happen? Chief executive, NHS trust
Poverty creates practical difficulties in seeking treatment. The cost of travelling to hospital, waiting on the phone for a GP appointment, using the internet to access online services ( 14% of the lowest socio-economic grade do not have internet access at home, compared to 2% of the highest), paying NHS charges etc, can all be prohibitive for those living in poverty.
As well as these challenges, the stigma of poverty can lead to a reluctance to come forward for treatment , or to seek help more broadly, for example accessing financial advice . And there is a relationship between deprivation and a lack of trust in public institutions, including the NHS, which again leads to a reluctance to access health care. These make the problem harder to solve for the NHS, as simply improving access to existing services won’t help those people who are reluctant to come forward for help
For a lot of people living, particularly in intergenerational poverty, there’s no expectation that public services will be any good or understand this space. It’s kind of wired in that you’ll be useless. Chief executive, NHS trust
The NHS does not always reach those in poverty
While there is no clear relationship between deprivation and the provision of several NHS services, such as diagnostic waits , there are relationships in other areas – for example, people who live in the most deprived areas of England are twice as likely to wait more than a year for non-urgent treatment. This is a variation of the inverse care law – that those who most need medical care are least likely to receive it.
In primary care, there are fewer GPs per patient in more deprived areas, consultations are shorter , and continuity of GP care is worse. This feeds through to patient satisfaction – for example, in 2023, 80% of patients in the most deprived quintile felt they had enough time at their last GP appointment, compared to 87% in the least deprived quintile.
Finally, NHS systems and administration can be more challenging to navigate for more deprived patients. Interviews with senior NHS staff gave a range of examples, from complex forms to reclaim travel expenses (which assumes people can pay these expenses in the first place) to patients in hospital missing out on social prescribing because this is only available via the GP. All this means that only 61% of people aged 65 and over in more deprived areas are satisfied with being able to access services when needed, compared to 69% in the least deprived areas.
The poorer you are, the more likely you are to be in unstable housing, the more likely you are to be moving around, the less likely it is that your local hospital will actually have contact details for you. Senior leader, network of NHS trusts
It is important to note that while more deprived areas shouldn’t be underserved, even if this was corrected, the impact of poverty on illness and NHS services would not be solved. While there are things the NHS can do in this space (assuming they have the capacity and funding), alleviating the root causes of poverty is not a problem for health services alone.
Impact of access difficulties
[Over-presenting] that’s the bit we talk about, I’m equally worried about the other end of it, which is nobody presents, either because they can’t, because to be honest they’re on £8 a week, they can’t get to services, or because they think they’ll be dismissed. Chief executive, NHS trust
These issues contribute to the lower use of preventive services in more deprived areas, such as lower uptake of cancer screening services and lower child vaccine rates . This association continues in a wide range of community or non-urgent services. A 2022 survey of those aged 65 and over found that those from lower social grades had fewer dentist, GP and non-urgent hospital appointments, despite being more likely to have a long-term health condition.
The cost-of-living crisis is worsening the issue. In 2023, 8% of lower-income adults reported not getting prescriptions or other medicines because they were unable to afford it, and 19% reported skipping essential dental care.
There is a risk that this problem may become even more acute given the current shift towards digital and remote care , which more deprived groups, who are more likely to experience digital exclusion ( a million people cancelled their broadband in the past year as they could not afford it), could struggle to access.
If people cannot access the services they need when they need them, they may either access other NHS services (there is a strong correlation between deprivation and patients reporting that they used other NHS services as they had problems making an appointment with a GP), or they may get sicker and need more costly services.
)
Unmet need, which describes where people who need medical care do not receive it, may be a particular problem for more deprived groups. For example, in 2021 the undiagnosed diabetes rate was double in the bottom IMD quintile compared to the top.
A recent JRF survey found that of those in the bottom income quintile whose health has been negatively impacted by the cost-of-living crisis, only 33% had accessed mental health services, and 39% physical health services, and that there were a range of reasons why they had not accessed care.
This presents a challenge for the NHS in finding those with an unmet need for health care, ensuring treatment is tailored to their needs, and dealing with the short-term increase in demand that may result if people are more able to access the care they need. However, this increase in demand may be offset by a decrease in demand for later-stage services, because if illnesses are caught earlier, they can often be treated more easily and cheaply.
)
Poverty and late or delayed treatment (and higher NHS costs)
Poverty contributes to greater prevalence of poor health, and thereby greater need for NHS services. And poverty contributes to difficulties in accessing these services at the early stages of illness. This leads to an inevitable but costly outcome, both in terms of financial cost to the NHS and worse outcomes for patients – an association between poverty and use of more-acute NHS services.
Dental care is a good illustration of this. The challenges of eating healthily while living in poverty contributes to a higher incidence of tooth decay among people in more deprived areas. Lack of access to NHS dentists has been well documented in the media recently , especially in more deprived areas . Another barrier is NHS dental charges , which vary from £25.80 to £306.80. These factors combine to result in substantially higher tooth extraction rates for people in more deprived areas.
)
A general dentist service attendance costs the NHS an average of £192 . NHS providers cost a major surgical tooth extraction in hospital at £3,915. Facilitating access to dentistry at an earlier stage could therefore save a considerable sum, as well as being better for patients. But this problem is worsening. Between 2018/19 and 2021/22, there was a 47% fall in routine dental examinations for non-paying adults but a 14% increase in urgent treatments.
Looking at a comprehensive measure of admissions to hospital, there are more admissions of patients in more deprived areas than in less deprived – unsurprising given the greater prevalence of ill health with deprivation. However, this difference is entirely driven by emergency admissions – planned admissions are lower for more deprived areas.
)
Later-stage and more costly hospital visits can also be seen in more A&E attendances – people in the most deprived IMD decile are nearly twice as likely to have attended A&E in 2022/23 than the least deprived decile. And it can be seen in higher numbers and longer stays in critical care (one of the most intensive uses of NHS resources, with some of the highest unit costs – more than £2,000 per bed day ).
)
These higher emergency hospital admissions, higher A&E attendances, and higher/longer critical care stays show that people in poverty access care later, access more unplanned care (ie, at the emergency stage), and access more intensive care for longer. This has a negative impact on patients and is more expensive for the NHS than if people had been treated earlier.
There are signs that this problem of late access has worsened in recent years. While this was a problem before the Covid-19 pandemic and remains a problem now, the interruption of service delivery due to Covid-19 did not help matters. Take early diagnosis of cancer – during Covid-19, the proportion of early cancer diagnoses fell more sharply for patients in more deprived areas (from 53% diagnosed early in March 2020 to 41% in May 2020, while the least deprived quintile of areas went from 58% to 52%).
The cost-of-living crisis is also exacerbating the problem; in a 2022 survey of NHS providers, 56% reported an increase in people delaying seeking help due to the cost of living. Another example is an increase in hospital admissions for malnutrition and nutrient deficiencies ( more than 800,000 admissions in 2022/23). This leads to higher costs for the NHS – Future Health estimated that health problems due to malnutrition cost £22.6 billion a year.
Poverty and worse health outcomes
Poverty and deprivation give rise to greater ill health and can make it harder to access NHS services. As well as increasing pressure on late-stage NHS services, this worse health and later treatment leads, inevitably, to worse outcomes for people. Between March 2021 and January 2023, the age-standardised mortality rate in the lowest IMD decile was almost double that of the highest.
Higher mortality rates are found not just in diseases that are more prevalent in more deprived areas, but also in diseases that are less prevalent in more deprived areas. For example, dementia is 1.4 times less prevalent in the most deprived areas compared to the least, but deaths from dementia are 1.6 times higher.
)
Higher mortality rates mean that life expectancy is lower in more deprived areas . Men living in the most deprived areas can expect to live 9.7 years fewer than men in the least deprived areas, and women 7.9 years fewer. These inequalities in life expectancy are increasing; between 2015–2017 and 2018–2020, female life expectancy decreased by 4.8 months in the most deprived decile but rose by 1.2 months in the least.
Not only do people in more deprived areas die sooner, they also live a higher proportion of their lives with health problems. 60-year-old women in the most deprived local areas have a similar level of diagnosed ill health (ie, not including any unmet need) as 76-year-old women in the least deprived.
)
Multimorbidity
Multimorbidity – multiple long-term conditions – is a problem across the whole population ( one in four people have two or more health conditions) but is noticeably worse for people in more deprived areas. In 2018 , 28% of 65–74-year-olds in the most deprived quintile of areas had four or more long-term conditions, compared to 16% in the least deprived quintile. The disparity starts early – in 2019, the median age of multimorbidity onset was eight years younger in the most deprived IMD quintile compared with the least deprived – and is growing.
This high and rising multimorbidity is adding pressure to NHS services. Research from The Health Foundation found that people with four or more conditions had an average of 8.9 outpatient visits and 24.6 GP visits over a two-year period, compared to 2.8 outpatient visits and 8.8 visits to the GP for people with one condition.
Both patient outcomes and NHS pressures are worsened by the challenges that come from managing multiple health conditions. The access difficulties discussed above, plus barriers to health literacy and the ability to navigate the NHS (especially where services are not designed for those with high levels of need), are all compounded by having to attend multiple appointments and navigate multiple systems for multiple conditions. These challenges are often greater for people in more deprived groups, and can lead to a vicious cycle, where the challenges in managing multimorbidity can increase health problems.
Inclusion groups – people who are homeless
All these issues are more severe among inclusion health groups – those who are socially excluded, such as sex workers, Gypsy, Roma and Traveller communities, vulnerable migrants, etc. One such group are people who experience homelessness . 82% of people who are homeless report being diagnosed with a mental health issue, eight times higher than the general population. And 66% of those in temporary accommodation report that their living situation has a negative impact on their health.
As well as causing or exacerbating ill health, homelessness makes it harder to access medical services. Only 37% of women who are homeless were up to date with breast screening in 2018–21, compared to 62% of the general population.
As with deprivation more widely, later-stage NHS activity is higher for people who experience homelessness . 48% of people who are homeless had been to A&E at least once in the previous year. These challenges in seeking and accessing health care mean that men who experience homelessness die at just 45 on average – 35 years earlier than the England average.
What can the NHS do to tackle poverty?
Despite the scale and complexity of the problem, the NHS can make a difference , through raising awareness of poverty in patients among staff, taking action to meet the needs of those experiencing poverty and using its voice to advocate for tackling poverty. The box below provides resources for the sector, including examples of what the NHS is currently doing at the local level to try to mitigate the effects of poverty on health – from providing practical support in accessing services to building trust and removing stigma.
We’re investing quite heavily in neighbourhood-level groups who can do that advocacy work and that support work and that befriending work that doesn’t say, ‘Oh gosh, you’re poor, we’re going to do something to you.' Chief executive, NHS trust
Resources for the NHS in tackling poverty
The NHS’s role in tackling poverty
Poverty and the health and care system: the role of data and partnership in bringing change
Tackling health inequalities on NHS waiting lists
Examples of NHS work
Building trust at the neighbourhood level
Wessex Cancer Alliance’s Communities Against Cancer project: partnering with a voluntary infrastructure body which provides training, support and grant funding to support community groups in raising awareness of cancer within their communities in ways that are appropriate for them. Targeted towards those experiencing health inequalities, including those on low incomes.
Norfolk and Waveney Community Voices : using trusted communicators to speak with communities who may not already engage with the NHS to hear what is important to them in health services and other issues that affect health and wellbeing, such as housing and employment.
Helping people navigate the NHS or access wider support
Southampton Hospital’s Patient support hub : providing a single point of contact for additional support before and after a visit to hospital.
The Warm Home Prescription Scheme : partnering with charities and using the government’s Household Support Fund to pay the energy bills of up to 150 people with cold-sensitive health conditions who are struggling with heating costs.
Using data to find and better understand those in poverty
Tackling fuel poverty in Cheshire and Merseyside : supporting people with respiratory illness who are living in fuel poverty. Drawing on data which identifies the population cohorts at greatest risk of harm, multidisciplinary teams (NHS, voluntary, community and social enterprise organisations, and local authorities) work together to reach out to high-risk groups with targeted interventions.
Poverty proofing services to ensure accessibility
Sale Central Primary Care Network : running drop-in sessions with a community health adviser for those facing barriers to accessing traditional services. This provides advice to improve health and wellbeing, and links to broader support services, such as financial advice.
Children’s Hospital Alliance’s Was Not Brought Programme : using AI to identify children at risk of not attending appointments, and providing tailored support such as free transport or appointments in schools.
Making the most of any contact with deprived groups
Bolton : employing social prescribing link workers in every primary care network to share advice with people in poverty, for example, by directing them to financial and debt advice, housing advice and skills training.
Understanding the complexities of poverty
Providing food for parents of children in hospital : offering free or subsidised meals for parents and carers during their child’s hospital stay. This trial was inspired by the charity Sophie’s Legacy and delivered in partnership with the NHS England food provision team and trust charities.
Supporting NHS staff in poverty
Identifying need and targeting support : using a survey of staff and focus groups to target support to those who need it, such as providing free breakfasts to some employees, offering budget management workshops, and training managers to support their staff.
Tackling poverty can be seen as less urgent than, for example, bringing waiting lists down. In interviews, senior NHS staff stated that while there is widespread agreement that tackling poverty is important, this does not always translate into concrete action or funding.
Fundamentally, what we are held to account on the at the end of the day is waiting lists and the achievement of targets and the delivery of balanced budgets. Senior leader, network of NHS trusts
NHS action to mitigate the effects of poverty is needed both for people and populations and to lessen the long-term pressure on the system – this should not be less of a priority than seemingly more urgent, or more measurable, aims. Previous work from The King’s Fund has shown ways the NHS can embed improvements in access for those in poverty or experiencing other health inequalities. But for sustained change to take place, long-term, multi-agency approaches are needed , as well as a willingness to change or replace current systems – this is not a quick or easy fix.
Poverty has a significant impact on people’s health, their need for health care, and their use of health care services. That people in poverty experience worse health is bad for them, bad for the economy, and bad for the NHS. The NHS needs to do more to deliver services that people living in poverty are more easily able to access and navigate – some good examples already exist at the local level. However, while the NHS can help manage the health consequences of being in poverty, taking action to lift millions of people out of poverty requires sustained investment and prioritisation across national government, public services and wider business and civic society.
About this report
This work was commissioned and funded by the Joseph Rowntree Foundation. JRF provided advice and information, but views expressed and any errors are those of the authors only.
Sources for conditions table/infographic
Mental health: Office for National Statistics (2022) ; NHS Digital (2023); NHS Digital (2022); NHS Digital (2022)
Bowel cancer: CancerData (no date); Office for Health Improvement and Disparities (no date) ; Office for National Statistics (2023)
Covid-19: Office for Health Improvement and Disparities (2023)
)
- Siva Anandaciva et al
Let's talk about social prescribing
What is social prescribing? How does it fit with other health and care services and what does it aim to achieve? Find out in our podcast episode.
- 26 July 2024
- Policy, finance and performance
The King's Fund responds to the King's Speech
Sarah Woolnough, Chief Executive at The King's Fund, responds to the King's Speech.
- 17 July 2024
The King's Fund responds to Wes Streeting's speech at the Future of Britain Conference
Siva Anandaciva, Chief Analyst of The King's Fund, comments on Wes Streeting’s speech at the Tony Blair Institute for Global Change Future of Britain Conference.
- 9 July 2024
The King's Fund responds to Liberal Democrat pledge to provide £1 billion a year to restore the local Public Health Grant
'We warmly welcome this commitment from the Liberal Democrats to restore the Public Health Grant to previous funding levels.' says Sarah Woolnough, Chief Executive at The King's Fund.
- 2 June 2024
PERSPECTIVE article
Perspectives in poverty and mental health.

- 1 Department of Psychiatry and Neurosciences, Charité – Universitätsmedizin Berlin, Corporate Member of Freie Universität Berlin, Humboldt-Universität zu Berlin, and Berlin Institute of Health, Berlin, Germany
- 2 Department of Psychiatry of University Hospital Charité in St. Hedwig Hospital Berlin, Germany
In recent years, different forms of poverty and their interaction with mental illness have been in the focus of research, although the implementation of action in mental health care and policy making so far is scarce. This perspective article offers different perspectives of poverty and its reciprocal association with mental illness and outlines possible future research and policy implications. We will approach the topic of poverty from various levels: On a micro-level, focusing on absolute poverty with precarious housing and malnutrition. On a meso-level, on neighborhood-related poverty as a factor in individuals' mental illness. On a macro-level, on effects of income inequality on mental health. In several studies, it has been shown that on each level, poverty has a profound impact on mental health, though it must be noted that in some fields, research is still scarce. In the future, an inter- and transdisciplinary approach is of considerable importance, since poverty and its impact on mental health should be addressed from different perspectives, reaching from targeted programs for individual groups (e.g., homeless people) up to national policy measures.
Introduction
The Global Burden of Disease study estimated that, in 2017, 792 million people worldwide reported impaired mental health, which represents almost 11% of the global population ( 1 ). According to The World Health Organization, mental health conditions produce economical losses of one trillion USD, with depression being the leading cause of ill health and disability ( 2 , 3 ).
Especially people living in poverty are unequally affected by mental illness ( 4 ). The United Nations (UN) defines poverty as “…a condition characterized by severe deprivation of basic human needs, including food, safe drinking water, sanitation facilities, health, shelter, education and information. It depends not only on income but also on access to social services” ( 5 ). According to the World Bank, the extreme poverty line concerning daily expenses is under 2.15$ based on 15 national poverty lines from some of the poorest countries in the World ( 6 ). National poverty lines vary depending on the respective costs to cover one's basic needs, e.g., in the European Union, someone earning <60% of the median income is “at-risk-of-poverty” ( 7 ). Relative poverty on the other hand, is defined as not having enough material, cultural, and social resources and thus be excluded from a lifestyle, which other individuals from the respective country can maintain ( 8 ).
Poverty has increased globally since the COVID-19 pandemic. The United Nations University reported that after 30 years of decline of poverty, the global pandemic could lead to an increase of global poverty by 8% since 2020, with rates being three times higher in rural compared to urban areas ( 9 ).
In this perspective article, we focus on the impact of poverty on mental health in high-income countries. We discuss effects of poverty on a micro-, meso- and macro-level and outline implications for future research and mental health policies. On the micro-level, we discuss individual characteristics including material, psychosocial, and behavioral risk factors, using the example of precarious housing and malnutrition. On a meso-level, we refer to community- and neighborhood-related circumstances with a focus on local poverty, social exclusion and discrimination, and their respective effects on individual mental health. On a macro-level, we focus on the association between income inequality within a nation and the national mental health burden.
Absolute poverty in high-income countries
Rates of poverty in the Organization for Economic Co-operation and Development (OECD) countries vary between 4.9% in Iceland as the lowest rate up to 19.9% in Costa Rica, whereby the highest poverty rate among high-income countries can be found in the United States with 17.8% ( 10 ). One subgroup affected by poverty in high-income countries are people exposed to homelessness. With an estimation of 1.9 million persons without a home, and increasing numbers in countries like the United States, United Kingdom and Germany ( 11 ), several research and policy initiatives focus on the interrelation between mental health and living conditions in poverty.
In a systematic review and meta-analysis of 39 studies with altogether 8,049 homeless persons in Germany, a pooled prevalence of a current mental illness of 76.2% (95% CI 64.0–86.6) was reported, with alcohol dependence being the most common disorder (pooled prevalence 36.7% [95%CI 27.7–46.2]) ( 12 ). In a systematic review and meta-regression among western countries, 29 studies with 5,684 individuals reported a pooled prevalence of 37.9% (95%CI 27.8–48.0) for alcohol dependence and 24.4% (95%CI 13.2–35.6) for drug dependence ( 13 ). Substance use among homeless people is often heavily stigmatized, and even healthcare professionals have displayed a rather negative attitude toward patients with substance use, which might have an influence of the self-esteem and empowerment of patients and thus affect treatment outcomes such as treatment completion ( 14 ). Beyond drug use, adverse life events, suicidality and mental illness are important predictors of becoming homeless ( 15 ). There is a complex interplay between homelessness and mental illness, with mental health challenges increasing the risk of homelessness, and homelessness promoting poor mental health including depression and suicidality ( 16 ).
Persons with debts and substantial loans represent another group affected by poverty in high-income countries. In Western countries like Germany, 8.6% of the general population have debts that cannot be cleared because of insufficient income and assets ( 17 ). Again, persons with mental health issues are disproportionately affected by debt. In a study with 486 psychiatric patients, 55.1% had outstanding debts, loans, or unpaid bills, of which more than a third (36.3%) reported debts between 10.000 and 99.999 e ( 18 ). Here, binary regression analysis identified younger age and substance use disorders as being significantly associated with outstanding debts [OR 0.98 (95%CI 0.96–1.00) and OR 2.41 (95%CI 1.48–3.92)] ( 18 ).
Another important aspect of absolute poverty is insufficient nutrition. There is an increasing focus on the interaction between food security and mental health as main sources of global mortality and disease ( 19 ). For example, Fang et al. conducted a study during the COVID-19 pandemic among 2,714 low-income participants in the United States and observed that food insecurity was associated with a 257% higher risk of anxiety [as measured by the GAD-7; OR 3.57 (95%CI 3.01–4.23)] and a 253% higher risk of depression [measured by PHQ-9; OR 3.53 (95%CI 2.99–4.17)] ( 20 ). Insufficient nutrition is a risk factor, while income stability was detected as a protective factor for depression [OR 0.77 after adjusting for income stability (95%CI 0.66–0.91)]. Especially respondents with children were identified as the most vulnerable subgroup. This evidence is supported by findings of the Global Burden of Disease Study 2019 ( 21 ), which reported that child and maternal malnutrition was one of the leading risk factors for disability-adjusted life-years. This study emphasizes the pivotal importance of targeted nutritional programs as a part of women's health in the context of mental health care. It also implicates that reaching out to vulnerable groups should not be restricted to mental health care settings, but that including interventions in the general community is essential, where e.g. mothers can be provided with adequate resources.
Poverty in the neighborhood
People living in socially underprivileged and poor city areas suffer more often from mental health conditions like depression, anxiety and psychosis than persons living in high-income neighborhoods ( 22 – 24 ). For example, Fone et al. reported that regional income inequality was significantly associated with more common mental disorders [measured by the Gini coefficient 1 and the Mental Health Inventory MHI-5; Odds Ratio = 1.13 (95%CI 1.04–1.22)] ( 22 ). In addition, more than half of the world's population live in cities, and the continuous urbanization of city areas lead to an aggravation of community-level risk factors for mental health conditions, including physical environmental challenges or chronic stress exposition, even though city residents have more access to education and healthcare ( 25 , 26 ). Accordingly, in a meta-analysis, Vassos et al. reported a 2.37 higher risk for schizophrenia for people living in urban environments compared to rural environments ( 24 ).
During the last decade, the effect of neighborhood-related factors (including social cohesion, income deprivation as well as traffic or air pollution) on the mental health status of residents has gained attention ( 27 ). It has been suggested to interpret data on individual risk factors including income and education with respect to their interaction with the social environment ( 28 , 29 ). The relationship between factors on a neighborhood level and individual outcomes can be complex ( 30 ), with multiple, potentially bidirectional pathways to explain the association between community-level and individual factors. In spite of these potential complexities, there is evidence that poverty in the neighborhood is associated with poor mental health (measured by the General Health Questionnaire GHQ-28) above and beyond the effects of individual education or income ( 31 ). This effect was even more pronounced among persons with a minority status (persons with a Turkish migration background in Berlin, Germany), and again independent of individual factors like age or income (beta = 1.12, Standard Error = 0.26, p < 0.001) ( 31 ). This observation is supported by a longitudinal cohort study with 1,120 participants in New York, which observed that the socioeconomic status (SES) of the neighborhood was associated with the incidence of depression, independently of the individual SES ( 28 ).
Next to economic deprivation, social-interactive aspects of the neighborhood should be taken into account. For example, a longitudinal multilevel analysis with 4,426 participants over the course of 7 years examined quality of life and mental health (36-Item Short Form Survey and Mental Health Inventory-5), neighborhood deprivation (gross household income) and social cohesion, which refers to a sense of belonging and solidarity within a community (Buckner's Neighborhood Cohesion Scale) ( 32 ). This study reported a negative association between neighborhood challenges due to poverty on the one hand and low levels of mental health and quality of life on the other, again after adjusting for individual socio-economic risk factors and transitions in life events. Interestingly, a protective effect of solidarity and social cohesion on this association was found. These findings suggest that individual mental health is substantially influenced by local poverty, and that solidarity and social support is of key importance for mental wellbeing ( 33 – 35 ).
Data on mediating processes between neighborhood poverty and mental wellbeing are rare and may include aspects of family and peer support structures ( 4 , 30 ). Lack of family and neighborhood resources can lead to more stress, social isolation, discrimination and susceptibility for mental disorders ( 31 ). Mental illness, on the other hand, can increase stigmatization, social exclusion and marginalisation ( 4 , 36 ). Also, income in people with mental health conditions is usually decreased, reducing resources and leading to a higher probability to live in a poor neighbourhood ( 4 ). Physical aspects of neighborhoods may also play an important role for mental wellbeing. In Greenwich, UK, it has been shown that physical environment and mental wellbeing are associated with each other on many domains ( 37 ). In this study, living conditions for persons registering in the lowest quartile for mental health were characterized by neighborhood noise [OR 2.71 (95%CI 1.48–4.98)], feeling overcrowded in the home [OR 1.42 (95%CI 1.42–3.48)], being dissatisfied with access to green open spaces [OR 1.69 (95%CI 1.05–2.74)], and feeling unsafe to go out in the day [OR 1.64 (1.02–2.64)].
Prospective studies are required to disentangle the interaction of individual, environmental and community level effects on mental health.
Income inequality and its effects on mental health
Looking at relative poverty on a macro-level, general effects of income inequalities on mental health have to be considered, as numerous studies have shown the effect of income inequality on overall health and mortality in high income countries ( 38 – 41 ). In their list of 17 sustainable development goals, the UN declared reducing income inequalities within and among countries as one aim ( 5 ). In the last decades, income inequality has dramatically increased in Western industrialized countries ( 42 ). According to the epidemiologists Pickett and Wilkinson, income inequality is linearly associated with higher rates of mental illness in high income countries ( 38 , 43 ). Industrialized countries with high income inequality, like the United States (measured by the ratio of income among the wealthiest compared with the poorest 20% in each country) showed a high index of health and social problems (e.g., life expectancy, mental illness, homicides, distrust, social mobility) ( 44 ). In 2022, Tibber et al. included 42 studies with data from 7,744,469 participants and found higher income inequality to be associated with poor general mental health, depression and psychosis in adults ( 45 ). Likewise, a review of 26 studies from mostly high-income countries reported a positive relationship between income inequality and depression, with greater impact for women and low-income subpopulations ( 41 ). Regarding schizophrenia, Burns et al. investigated incidence rates across 26 mostly high-income countries and found a positive relationship between income inequality, measured by the Gini coefficient, and the incidence rate of schizophrenia [beta = 1.02; Z = 2.28; p = 0.02; (95%CI 1.00–1.03)]: for every point in income inequality increase, a two-point increase in incidence rate of schizophrenia followed ( 46 ). After correction for potential confounders like rates of urbanization, Gross Domestic Product per capita, migrant population and unemployment rate, the effect still remained significant ( 46 ).
Regarding mortality caused by mental health conditions, suicide rates among young men in England and Wales increased over the period of 1950–1998, which was associated with an increase in income inequality and divorce and a decline in marriage ( 47 ). A longitudinal study from Canada investigated mental health in 2,461 mothers during pregnancy and after birth and found a significant interaction between income inequality measured by the Gini coefficient and anxiety symptoms, but not depressive symptoms ( 48 ). In a register-based cohort study with 1,354,393 children, mental disorders were three–four times more prevalent in children who had parents in the lowest income percentiles ( 49 ). Differences were detected concerning attention-deficit hyperactivity disorder in boys and depression and anxiety in girls. Wilkinson and Pickett elaborated on the importance of early childhood interventions to reduce developmental risk factors for health ( 50 ).
To explain these findings, several causal hypotheses are discussed. For example, the Social Capital Hypothesis suggests high income inequality affects (mental) health because of a breakdown of social capital, which includes social trust and safety, a sense of belonging, and participation ( 38 , 39 , 51 ). The Status Anxiety Hypothesis states that high income inequality fuels a feeling of inferiority because of high status competition and comparison, which causes chronic stress ( 52 ). In his book, “Status Syndrome,” Marmot states that position in hierarchy, which is linked to control over life and social engagement, is the most important factor for health inequalities, rather than factors like genetics or behaviour ( 53 , 54 ). This hypothesis is supported by a study using data of 34,000 study participants across 31 European countries, conducting multi-level models with the Gini coefficient, several sociodemographic factors, and status anxiety, as assessed by the multi-scale question “some people look down on me because of my job situation or income” ( 52 ). In this latter study, status anxiety was inversely associated with income rank; moreover, status anxiety was also lower in countries with lower income inequality. Beyond status anxiety, perception of unfair income distribution may be particularly pronounced in cities with relatively segregated high and low income neighborhoods and exposure to dramatic differences in resources and privileges ( 55 ). Again, longitudinal studies can help to disentangle complex interactions between individual risk and resilience factors, community resources and environmental challenges.
Discussion: Future policy implications
The reviewed studies suggest that a person's mental health is not only and even not primarily explained by individual risk factors, but includes closely related community and environmental processes that reflect social differences and justice. In this context, Amartya Sen's capability framework emphasizes the responsibility of the society to contribute to each of its members' self-fulfilment ( 56 ). Together with the conceptual work of Michael Marmot ( 54 ), these considerations shift the focus away from stigmatizing socially and economically excluded individuals toward a reflection of multidimensional processes within a society, which steer vulnerable people in the direction of poverty and compromised somatic as well as mental health.
Among many conceptual frameworks, the World Health Organization formulated three levels of policy approaches in their call for action on the social determinants of health, to tackle general health inequities ( 57 ). Based on this, we elaborate on specific mental health and poverty strategies and recommend:
Targeted programs for groups with a low socioeconomic status, including homeless persons with mental illness. Financial inclusion of people with mental illness, especially those in unstable housing, should be in the focus of targeted programs. Indeed, our own research showed that in Berlin Germany, about 10.1% of all patients have no bank account, thus severely restricting access to social aid and limiting participation ( 58 ). Strategies of permanent supportive housing like Housing First have proven to be effective on housing stability as well as health outcomes ( 15 ). Other examples for targeted programs might be nutritional programs for women or young mothers, since child and maternal malnutrition are one of the leading risk factors for disability-adjusted life-years ( 21 ).
Policies for closing the gap of social inequalities. Here, scientists from different disciplines should cooperate to assess the impact of poverty on the general mental health of a community, and to disentangle complex interactions on the level of communities, environments and individuals. Our own research emphasizes the impact of local poverty above and beyond individual income ( 31 ). This observation supports the implementation and examination of effects of anti-poverty programs including Universal Basic Income (UBI) ( 59 ). A study on the effects of basic income provided by cash payments in Finland reported significant improvements in mental wellbeing; mediating factors were associated with a reduction in perceived stigma, more time with family and friends, and a new sense of hope for the future ( 60 ). Interestingly, improvements for children were amplified when the payments were given early during their individual development ( 60 ). Nevertheless, it should be considered that UBI might also be discriminating toward people with different needs and thus higher living expenses, for example for people with chronic diseases and higher health expenditures. Also, UBI might only be offered to people with a certain citizenship, excluding already marginalized people without any citizenship for example. In light of the effects of income inequality on mental health, economic growth per se will not lead to an increased mental wellbeing, and a balanced distribution of wealth should be considered in policy including metal health strategies ( 61 ).
Promoting interdisciplinary and participatory research on social interactions in societies. To date, participatory research and peer involvement is widely underrepresented and should play a much more influential role in scientific studies and policies for mental health ( 62 ). On a neighborhood level, solidarity and mutual support appears to represent important mediators between neighborhood poverty and individual mental health. It should be an inter- as well as transdisciplinary effort including social sciences to disentangle these processes and their complex interactions. We and others have suggested to promote topics relevant for mental health in all aspects of city planning, including exposure to air pollution, traffic noise, also at nights, provision of green spaces, accessible community centers and spaces for social interaction ( 25 , 26 ).
To disentangle the complex impact of absolute and relative poverty on mental health, studies should be designed longitudinally and measurements should be included that address mental as well as somatic health, risk factors such as racism and discrimination and potential resilience factors such as solidarity and mutual support. Facing the increasing digitization of health care, the use of digital tools and digital interventions to collect data can be of help with this endeavour ( 63 , 64 ).
Altogether, an inter- and transdisciplinary approach can promote understanding of the complex and multileveled interactions between individual- and community-based risk factors. The aim is to address mental health in populations with evidence-based public health policies that target social and physical environments and foster solidarity and mutual support. Medical prevention and intervention strategies targeted at the provision of adequate mental health care for persons with mental illness should be complemented by policies that promote social participation and empowerment within societies.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
DM and AH were responsible for drafting and revising the manuscript. DM wrote the first manuscript draft. AH, SS, and SG revised the manuscript. All authors contributed to and approved the final manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The handling editor [WF] declared a shared affiliation with the author(s) at the time of review.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. ^ To objectify income inequality, several measures have been established, of which the Gini index is one of the most commonly used ( 65 ). It ranges from 0 to 1, with higher index indicating greater income inequality. The calculation relates to the Lorenz curve, which is a graphical representation of distribution of income.
1. Saloni Dattani, Hannah Ritchie MR. Mental Health. Our World Data . (2021). Available online at: https://ourworldindata.org/mental-health (accessed May 15, 2022).
Google Scholar
2. WHO. Mental Health . Available online at: https://www.who.int/observatories/global-observatory-on-health-research-and-development/analyses-and-syntheses/mental-health/global-strategic-direction#:~:text=Mental (accessed May 15, 2022).
3. WHO. Mental Health and Substance Abuse . Available online at: https://www.who.int/teams/mental-health-and-substance-use/promotion-prevention/mental-health-in-the-workplace#:~:text=A (accessed May 15, 2022).
4. Ridley M, Rao G, Schilbach F, Patel V. Poverty, depression, and anxiety: causal evidence and mechanisms. Science . (2020) 370:aay0214. doi: 10.1126/science.aay0214
PubMed Abstract | CrossRef Full Text | Google Scholar
5. United Nations. World Summit for Social Development Programme of Action - Chapter 2. (1995). Available online at: https://www.un.org/esa/socdev/wssd/text-version/agreements/poach2.htm (accessed May 15, 2022).
6. Bank TW. Fact Sheet: An Adjustment to Global Poverty Lines (2022). Available online at: https://www.worldbank.org/en/news/factsheet/2022/05/02/fact-sheet-an-adjustment-to-global-poverty-lines (accessed May 15, 2022).
7. Eurostat. Glossary: At-risk-of-poverty rate. (2021). Available online at: https://ec.europa.eu/eurostat/statistics-explained/index.php?title=Glossary:At-risk-of-poverty_rate (accessed May 15, 2022).
8. DIW Berlin. Armut. (2022). https://www.diw.de/de/diw_01.c.411565.de/presse/diw_glossar/armut.html (accessed May 15, 2022).
9. Sumner A, Hoy C, Ortiz-Juarez E. E stimates of the impact of COVID-19 on global poverty . Helsinki (2020). doi: 10.35188/UNU-WIDER/2020/800-9
CrossRef Full Text | Google Scholar
10. OECD. Poverty rate (indicator) . Paris: OECD (2022). doi: 10.1787/0fe1315d-en
11. OECD. “ Better Data and Policies to Fight Homelessness in the OECD”, Policy Brief on Affordable Housing . (2020). Available online at: http:/oe.cd/homelessness-2020 (accessed May 17, 2022).
12. Gutwinski S, Schreiter S, Deutscher K, Fazel S. The prevalence of mental disorders among homeless people in high-income countries: an updated systematic review and meta-regression analysis. PLoS Med. (2021) 18:e1003750. doi: 10.1371/journal.pmed.1003750
13. Fazel S, Khosla V, Doll H, Geddes J. The prevalence of mental disorders among the homeless in Western countries: systematic review and meta-regression analysis. PLoS Med. (2008) 5:e225. doi: 10.1371/journal.pmed.0050225
14. van Boekel LC, Brouwers EPM, van Weeghel J, Garretsen HFL. Stigma among health professionals towards patients with substance use disorders and its consequences for healthcare delivery: systematic review. Drug Alcohol Depend. (2013) 131:23–35. doi: 10.1016/j.drugalcdep.2013.02.018
15. Schreiter S, Speerforck S, Schomerus G, Gutwinski S. Homelessness: care for the most vulnerable – a narrative review of risk factors, health needs, stigma, and intervention strategies. Curr Opin Psychiatry . (2021) 34:400–4. doi: 10.1097/YCO.0000000000000715
16. Padgett DK. Homelessness, housing instability and mental health: making the connections. BJPsych Bull. (2020) 44:197–201. doi: 10.1192/bjb.2020.49
17. Creditreform. Schuldner Atlas Deutschland. (2021). Available online at: https://www.creditreform.de/fileadmin/user_upload/central_files/News/News_Wirtschaftsforschung/2021/SchuldnerAtlas_Deutschland/2021-11-10_AY_OE_Analyse_SchuldnerAtlas_2021.pdf (accessed May 17, 2022).
18. Schreiter S, Heidrich S, Heinz A, Krausz RM, Schouler-Ocak M, Bermpohl F, et al. [Debts, loans and unpaid bills among day patients and inpatients in psychiatric care in Berlin, Germany]. Nervenarzt. (2021) 92:1172–8. doi: 10.1007/s00115-020-01013-9
19. Sparling TM, Cheng B, Deeney M, antoso MV, Pfeiffer E, Emerson JA, et al. Global mental health and nutrition: moving toward a convergent research Agenda. Front Public Health . (2021) 9:722290. doi: 10.3389/fpubh.2021.722290
20. Fang D, Thomsen MR, Nayga RM. The association between food insecurity and mental health during the COVID-19 pandemic. BMC Public Health. (2021) 21:607. doi: 10.1186/s12889-021-10631-0
21. Collaborators GBD 2019 RF. Global burden of 87 risk factors in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet . (2020) 396:1223–49. doi: 10.1016/S0140-6736(20)30752-2
22. Fone D, Greene G, Farewell D, White J, Kelly M, Dunstan F. Common mental disorders, neighbourhood income inequality and income deprivation: small-area multilevel analysis. Br J Psychiatry. (2013) 202:286–93. doi: 10.1192/bjp.bp.112.116178
23. Peen J, Schoevers RA, Beekman AT, Dekker J. The current status of urban-rural differences in psychiatric disorders. Acta Psychiatr Scand. (2010) 121:84–93. doi: 10.1111/j.1600-0447.2009.01438.x
24. Vassos E, Pedersen CB, Murray RM, Collier DA, Lewis CM. Meta-analysis of the association of urbanicity with schizophrenia. Schizophr Bull. (2012) 38:1118–23. doi: 10.1093/schbul/sbs096
25. Gruebner O, Rapp MA, Adli M, Kluge U, Galea S, Heinz A. Cities and mental health. Dtsch Arztebl Int. (2017) 114:121–7. doi: 10.3238/arztebl.2017.0121
26. Adli M, Schöndorf J. [Does the city make us ill? The effect of urban stress on emotions, behavior, and mental health]. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. (2020) 63:979–86. doi: 10.1007/s00103-020-03185-w
27. Heinz A, Deserno L, Reininghaus U. Urbanicity, social adversity and psychosis. World Psychiatry. (2013) 12:187–97. doi: 10.1002/wps.20056
28. Galea S, Ahern J, Nandi A, Tracy M, Beard J, Vlahov D. Urban neighborhood poverty and the incidence of depression in a population-based cohort study. Ann Epidemiol. (2007) 17:171–9. doi: 10.1016/j.annepidem.2006.07.008
29. Visser K, Bolt G, Finkenauer C, Jonker M, Weinberg D, Stevens GWJM. Neighbourhood deprivation effects on young people's mental health and well-being: a systematic review of the literature. Soc Sci Med. (2021) 270:113542. doi: 10.1016/j.socscimed.2020.113542
30. van Ham M, Manley D, Bailey N, Simpson L, Maclennan D. Neighbourhood effects research: New perspectives. In: van Ham M, Manley D, Simpson L, Maclennan D, editors. Neighbourhood Effects Research: New Perspectives . Cham: Springer (2011). p. 1–21. doi: 10.1007/978-94-007-2309-2_1
31. Rapp MA, Kluge U, Penka S, Vardar A, Aichberger MC, Mundt AP, et al. When local poverty is more important than your income: mental health in minorities in inner cities. World Psychiatry. (2015) 14:249–50. doi: 10.1002/wps.20221
32. Fone D, White J, Farewell D, Kelly M, John G, Lloyd K, et al. Effect of neighbourhood deprivation and social cohesion on mental health inequality: a multilevel population-based longitudinal study. Psychol Med. (2014) 44:2449–60. doi: 10.1017/S0033291713003255
33. Kingsbury M, Clayborne Z, Colman I, Kirkbride JB. The protective effect of neighbourhood social cohesion on adolescent mental health following stressful life events. Psychol Med. (2020) 50:1292–9. doi: 10.1017/S0033291719001235
34. Erdem Ö, Prins RG, Voorham TAJJ, van Lenthe FJ, Burdorf A. Structural neighbourhood conditions, social cohesion and psychological distress in the Netherlands. Eur J Public Health. (2015) 25:995–1001. doi: 10.1093/eurpub/ckv120
35. Johns LE, Aiello AE, Cheng C, Galea S, Koenen KC, Uddin M. Neighborhood social cohesion and posttraumatic stress disorder in a community-based sample: findings from the Detroit Neighborhood Health Study. Soc Psychiatry Psychiatr Epidemiol. (2012) 47:1899–906. doi: 10.1007/s00127-012-0506-9
36. Anakwenze U, Zuberi D. Mental health and poverty in the inner city. Health Soc Work. (2013) 38:147–57. doi: 10.1093/hsw/hlt013
37. Guite HF, Clark C, Ackrill G. The impact of the physical and urban environment on mental well-being. Public Health. (2006) 120:1117–26. doi: 10.1016/j.puhe.2006.10.005
38. Pickett KE, Wilkinson RG. Inequality: an underacknowledged source of mental illness and distress. Br J Psychiatry. (2010) 197:426–8. doi: 10.1192/bjp.bp.109.072066
39. De Silva MJ, McKenzie K, Harpham T, Huttly SRA. Social capital and mental illness: a systematic review. J Epidemiol Community Health . (2005) 59:619–27. doi: 10.1136/jech.2004.029678
40. Wilkinson R, Pickett K. Inequality and mental illness. Lancet Psychiatry. (2017) 4:512–3. doi: 10.1016/S2215-0366(17)30206-7
41. Patel V, Burns J, Dhingra M, Tarver L, Kohrt B, Lund C. Income inequality and depression: a systematic review and meta-analysis of the association and a scoping review of mechanisms. World Psychiatry. (2018) 17:76–89. doi: 10.1002/wps.20492
42. Berman Y, Ben-Jacob E, Shapira Y. The dynamics of wealth inequality and the effect of income distribution. PLoS ONE. (2016) 11:e0154196. doi: 10.1371/journal.pone.0154196
43. Pickett KE, James OW, Wilkinson RG. Income inequality and the prevalence of mental illness: a preliminary international analysis. J Epidemiol Community Health. (2006) 60:646–7. doi: 10.1136/jech.2006.046631
44. Pickett K. Income inequality and social dysfunction. Annu Rev Sociol . (2009) 35:493–511. doi: 10.1146/annurev-soc-070308-115926
45. Tibber MS, Walji F, Kirkbride JB, Huddy V. The association between income inequality and adult mental health at the subnational level—a systematic review. Soc Psychiatry Psychiatr Epidemiol. (2022) 57:1–24. doi: 10.1007/s00127-021-02159-w
46. Burns J, Tomita A, Kapadia A. Income inequality and schizophrenia: increased schizophrenia incidence in countries with high levels of income inequality. Int J Soc Psychiatry . (2013) 60:185–196. doi: 10.1177/0020764013481426
47. Gunnell D, Middleton N, Whitley E, Dorling D, Frankel S. Why are suicide rates rising in young men but falling in the elderly?—a time-series analysis of trends in England and Wales 1950–1998. Soc Sci Med. (2003) 57:595–611. doi: 10.1016/S0277-9536(02)00408-2
48. Lowe SA, McDonald S, Senthilselvan A, Nykiforuk CI, Chari R, Pabayo R. Is neighbourhood income inequality associated with maternal mental health? A longitudinal analysis of pregnant and new mothers living in Calgary, Alberta. BMJ Open. (2021) 11:e049220. doi: 10.1136/bmjopen-2021-049220
49. Kinge JM, Øverland S, Flatø M, Dieleman J, Røgeberg O, Magnus MC, et al. Parental income and mental disorders in children and adolescents: prospective register-based study. Int J Epidemiol. (2021) 50:1615–27. doi: 10.1093/ije/dyab066
50. Pickett KE, Wilkinson RG. The ethical and policy implications of research on income inequality and child well-being. Pediatrics . (2015) 135(Suppl):S39–47. doi: 10.1542/peds.2014-3549E
51. Kragten N, Rözer J. The income inequality hypothesis revisited: assessing the hypothesis using four methodological approaches. Soc Indic Res. (2017) 131:1015–33. doi: 10.1007/s11205-016-1283-8
52. Layte R, Whelan CT. Who feels inferior? A test of the status anxiety hypothesis of social inequalities in health. Eur Sociol Rev. (2014) 30:525–35. doi: 10.1093/esr/jcu057
53. De Vogli R. Status syndrome: how your social standing directly affects your health and life expectancy. BMJ Br Med J . (2004) 329:408. doi: 10.1136/bmj.329.7462.408
54. Marmot M. Status syndrome. Significance. (2004) 1:150–4. doi: 10.1111/j.1740-9713.2004.00058.x
55. Heinz A, Zhao X, Liu S. Implications of the association of social exclusion with mental health. JAMA Psychiatry. (2020) 77:113–4. doi: 10.1001/jamapsychiatry.2019.3009
56. Sen A. Development as Freedom (1999). The Globalization and Development Reader: Perspectives on Development and Global Change. New York, NY (1999).
57. Solar O IA. A Conceptual Framework for Action on the Social Determinants of Health. Social Determinants of Health Discussion Paper 2 (Policy and Practice) . Geneva: World Health Organization. (2010).
58. Schreiter S, Bermpohl F, Schouler-Ocak M, Krausz MR, Rössler W, Heinz A, et al. Bank account ownership and access among in-patients in psychiatric care in berlin, germany-a cross-sectional patient survey. Front Psychiatry. (2020) 11:508. doi: 10.3389/fpsyt.2020.00508
59. Bidadanure JU. The political theory of universal basic income. Annu Rev Polit Sci. (2019) 22:481–501. doi: 10.1146/annurev-polisci-050317-070954
60. Wilson N, McDaid S. The mental health effects of a Universal Basic Income: a synthesis of the evidence from previous pilots. Soc Sci Med. (2021) 287:114374. doi: 10.1016/j.socscimed.2021.114374
61. Oishi S, Kesebir S. Income inequality explains why economic growth does not always translate to an increase in happiness. Psychol Sci. (2015) 26:1630–8. doi: 10.1177/0956797615596713
62. Slattery P, Saeri AK, Bragge P. Research co-design in health: a rapid overview of reviews. Heal Res policy Syst. (2020) 18:17. doi: 10.1186/s12961-020-0528-9
63. Heinz A, Kiefer F, Smolka MN, Endrass T, Beste C, Beck A, et al. Addiction research consortium: losing and regaining control over drug intake (ReCoDe)-from trajectories to mechanisms and interventions. Addict Biol. (2020) 25:e12866. doi: 10.1111/adb.12866
64. Tost H, Champagne FA, Meyer-Lindenberg A. Environmental influence in the brain, human welfare and mental health. Nat Neurosci. (2015) 18:1421–31. doi: 10.1038/nn.4108
65. Liberati P, Bellù LG. Inequality Analysis - The Gini Index . Rome (2006).
Keywords: income inequalities, poverty & inequality, mental health, homelessness and mental health, mental illness
Citation: Marbin D, Gutwinski S, Schreiter S and Heinz A (2022) Perspectives in poverty and mental health. Front. Public Health 10:975482. doi: 10.3389/fpubh.2022.975482
Received: 22 June 2022; Accepted: 07 July 2022; Published: 04 August 2022.
Reviewed by:
Copyright © 2022 Marbin, Gutwinski, Schreiter and Heinz. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Derin Marbin, derin.marbin@charite.de
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Front Public Health
The Intertwined Relationship Between Malnutrition and Poverty
Faareha siddiqui.
1 Division of Women and Child Health, Aga Khan University, Karachi, Pakistan
Rehana A. Salam
Zohra s. lassi.
2 Robinson Research Institute, Adelaide Medical School, University of Adelaide, Adelaide, SA, Australia
Despite social and economic development, the burden of malnutrition across the globe remains unacceptably high. A vital relationship exists between nutritional status, human capital, and economic standing. Malnutrition adversely affects the physiological and mental capacity of individuals; which in turn hampers productivity levels, making them and their respective countries more susceptible to poverty. A two-way link exists between malnutrition and poverty, creating a vicious cycle with each fueling the other. Malnutrition produces conditions of poverty by reducing the economic potential of the population and likewise, poverty reinforces malnutrition by increasing the risk of food insecurity. The aim of the paper is to describe the interconnection between malnutrition and poverty, and to highlight how both serve as the cause and consequence of each other. The paper also discusses ways to move ahead to tackle these issues in a parallel manner rather than in separate silos.
Introduction
Malnutrition relates to a deficiency, excess, or imbalance of energy and other macro and micro-nutrients. It comprises of varying degrees of under- or over- nutrition, which leads to changes in body composition, body function, and clinical outcomes. In other words, malnutrition is an all-inclusive term that represents all manifestations of poor nutrition and ranges from extreme hunger and undernutrition to obesity ( 1 , 2 ). Despite social and economic development, the burden of malnutrition across the globe remains unacceptably high ( 2 ), recent data suggests that ~800 million people are undernourished, out of which 780 million reside in low-to-middle income countries, especially in Sub-Saharan Africa and South Asia ( 2 ). In 2015, inadequate food intake and poor dietary quality were responsible directly or indirectly for causing ill-health with six of the top 11 global risk factors being associated with dietary imbalances ( 2 ) and in 2017, 11 million deaths and 255 million disability-adjusted life years (DALYs) were attributable to dietary risk factors ( 3 ). Children under the age of 5 years are highly vulnerable to malnutrition with estimates suggesting that in 2019, globally 144 million children under the age of five were stunted (short for his/her age), 47 million wasted (thin for his/her height) and 38 million overweight (abnormal or excess bodyweight) ( 4 ). In adults, obesity is becoming more prevalent worldwide with ~38.9% of the adult population being either overweight or obese ( 5 ). Paradoxically, even though women have a higher prevalence (15.1%) of obesity than men (11%) ( 5 ); millions of women around the world are still underweight and one-third of women of reproductive age are estimated to have anemia ( 5 ).
Malnutrition has long been linked to poverty as higher rates of malnutrition are found in areas with chronic poverty ( 6 ). The impact of poverty on individuals can be seen through multiple manifestations and includes poor nutritional status, food insecurity, vulnerability to disease, reduced productivity levels, and compromised physical and intellectual development. Additionally, people living in poverty are unable to access necessities including nutritious food, hygienic environment, appropriate shelter, and adequate health care ( 7 ). Therefore, it would not be incorrect to suggest that even though malnutrition is a global phenomenon, those living in poverty face a higher burden. The question that now arises is whether malnutrition is a cause or consequence of poverty. The relationship between the nutritional status and economic standing has been further explored through the course of this paper.
The World Bank has set the International Poverty Line at $1.90 per person per day using 2011 Purchasing Power Parity (PPP) conversion factors ( 8 ). Therefore, households with a per capita income or expenditure less than the standard poverty line are defined as being poor ( 9 ). This makes income level the prime indicator for poverty, however with the passage of time, the need for re-conceptualizing poverty is becoming more evident as poverty is complex and multifaceted. Therefore, the conceptualization of poverty should not be limited to average income and wealth only but should encompass various other deprivations that are often experienced by people living in poverty. The global Multidimensional Poverty Index (MPI) is an international measure of acute poverty covering over 100 developing countries; created by the Oxford Poverty and Human Development Initiative (OPHI) and the United Nations Development Programme (UNDP) in 2010 ( 10 ). The global MPI steps away from the traditional view of poverty being solely limited to average income and wealth; to a more holistic view that highlights the need for using multiple indicators to account for various issues faced by people as a consequence of poverty ( 10 ). Through this index, poverty is portrayed to be a deprivation of basic amenities that restricts individuals from leading a good and healthy life ( 11 ) and takes into account the systemic disparities within a country and stretches the boundaries of poverty beyond the shortage of material assets to a concept that encompasses multiple deprivations, including but not limited to: assets, living standards, education, sanitation and hygiene, health and nutrition ( 10 ).
Since the 1990s, it is estimated that the proportion of the world's population living in extreme poverty has declined by more than a half ( 8 ). In 2015, 10% of the world's population lived under the poverty line; compared to nearly 36% in 1990 ( 8 ). Unfortunately, despite the overall decline in global poverty, progress has been uneven and disproportionate with the majority of the world's poor residing predominantly in Sub-Saharan Africa and South Asia ( 8 ). In 2015, 736 million people lived in extreme conditions of poverty with half of them i.e., 368 million residing only in five countries of India, Nigeria, Democratic Republic of Congo, Ethiopia, and Bangladesh ( 8 ). This illustrates that certain countries especially those afflicted by conflict, poor governance, and natural disasters continue to experience a skewed burden of poverty.
To analyze the vital linkages between poverty and malnutrition; it is important to highlight the growing evidence that health outcomes including malnutrition are driven by social determinants of health i.e., the conditions and circumstances in which people live, learn, work, and even play have a significant impact on their health ( 12 ). This interconnection between people's conditions and circumstances and their health can be displayed using the concept of poverty and food insecurity. The term “food insecurity” refers to a situation in which people do not have adequate physical, social or economic access to sufficient and nutritious food ( 13 ). Broadly, food insecurity is assessed using four dimensions i.e., food availability, access to food, stability of supply and safe, and healthy food utilization ( 14 ). Food insecurity may occur at various levels including regional, national, household, or individual. Poverty and food insecurity are deeply related, as poverty may adversely affect the social determinants of health and may create unfavorable conditions in which people might experience unreliable food supply ( 13 ). Food is a major household expenditure for the poor households ( 15 ). Data from African countries indicate that close to half of household income is spent on food: Nigeria (56.4%) ( 16 ); Kenya (46.7%), Cameroon (45.6%), Algeria (42.5%) ( 17 ). Similarly, within high-income countries, low-income households spend a significant proportion of their income on food: Ireland (14–33%), USA (28.8–42.6%) ( 17 , 18 ). In comparison, the wealthiest households in the USA spend a much lower 6.5–9.2% of household income on food ( 17 ). Despite spending a large proportion of their household income on food, many poor households continue to remain food insecure because of their insufficient, irregular, and fluctuating incomes ( 2 , 13 ).
Poverty, Food Insecurity and Double Burden of Malnutrition
A vital relationship exists between malnutrition and poverty. Poverty creates unstable and unfavorable conditions that may contribute to fueling the problem of malnutrition ( 7 ). People living in poverty often face financial limitations, which hinders their ability to access safe, sufficient, and nutritious food ( 7 ). Food insecurity compromises people's ability to acquire the amount of food needed to fulfill the bodily requirement of calories and without sufficient calorie intake, an individual may not be able to build up energy or strength to carry out everyday life activities and this also hampers the capacity and productivity to earn ( 19 ). While people living in poverty may require a greater quantity of food than they cursrently have, it is important to take into consideration that appropriate intake of nutrients and quality of food is equally important ( 19 ). Poverty can contribute to worsening malnutrition by compromising the quality of food intake and bolstering hidden hunger which is the deficiency of essential vitamins and minerals. The burden of obesity has extended beyond wealthier, developed nations and has now also become a feature of the developing world ( 16 ). Poverty leads to financial constraints that in turn lead to the consumption of cheap, high-energy staple foods, primarily carbohydrates, and fats rather than nutritionally dense food. Through the consumption of carbohydrates and fats, energy levels spike; but nutritional quality becomes compromised. The consequence of this is reduced nutritional quality and nutrient deficiencies. Poverty plays a significant role in regulating access and preference of foods ( 13 , 16 ), and this is evident in studies that showcase that when people living in poverty get a chance to spend relatively more on food; they often prefer to buy better tasting food, rather than good quality food ( 19 ).
The deficiency of micronutrients or “hidden hunger” is an important component of malnutrition ( 13 ). Micronutrient deficiencies can exists in all age groups and in any socioeconomic bracket. Iron, folate, vitamin A, iodine, and zinc deficiencies are among the most common and widespread micronutrient deficiencies among women and children in low- and middle- income countries and many of these micronutrient deficiencies co-exist. Assessing the relationship between malnutrition and poverty, requires consideration of micronutrient deficiencies. While macro- and micro- nutrient deficiencies may cause suboptimal mental and physical development, recurrent infections and growth retardation ( 20 , 21 ); micro-nutrient deficiencies may also result in adverse birth outcomes including low birth weight babies ( 22 , 23 ). To date, ~20 million babies are born with low birth weight each year and there is growing evidence of the connections between slow growth in height early in life and impaired health and educational and economic performance later in life ( 5 , 24 ). Low birth weight in babies can contribute to the vicious cycle of malnutrition since maternal nutrition status especially maternal stature has been reported to be inversely associated with offspring mortality, underweight, and stunting in infancy and childhood ( 22 , 23 ). Moreover, the importance of adequate intake of micronutrients can be noted in children born to mothers with sufficient amounts of iodine during pregnancy ( 19 ), as these children tend to complete one-third or one-half a year more schooling than children born to mothers with inadequate amount of iodine during pregnancy ( 19 ). It has been suggested that if every mother took iodine capsules during pregnancy then this could improve educational attainment among children in Central and Southern Africa ( 19 ).
Briefly put, the double burden of malnutrition and the importance of micro-nutrients should be recognized when analyzing the malnutrition-poverty cycle. There is a growing need to reimagine the concept of malnutrition and development experts and policy makers should make strides to account for the inherent complexities of both concepts in order to develop successful and sustainable nutritional strategies ( 19 ).
Malnutrition: Cause or Consequence of Poverty?
The question that now arises is whether malnutrition is a cause or consequence of poverty and vice versa? To elaborate upon this, it is important to highlight the relationship of human capital with nutrition and poverty.
Human capital is an integral asset of any country and the process of developing human capital begins from infancy and continues throughout the course of an individual's life ( 25 ). Nutritional status has a profound impact on human capital. The reasoning is simple, improved nutritional status is vital for escaping poverty, as good health is needed to increase productivity levels, contribute to economic growth, and improve a country's overall welfare ( 6 ). Without adequate nutrition, human capital starts to decline. This is because malnutrition negatively impacts physical and mental development, intellectual capacity, productivity, and the economic potential of an individual ( 25 ). As a consequence, economic stability is threatened, making a country more vulnerable to poverty. Poverty contributes to the problem of food insecurity which is referred to as a “resourced-constrained” or “poverty related” condition. Although the populations affected by poverty and food insecurity overlap; it is important to note that not all people living in poverty are food insecure and that this problem also exists in people living above the poverty line. Moreover, poverty also contributes in creating conditions of micro-nutrient deficiencies and hidden hunger. These factors exacerbate the issue of malnutrition and makes individuals more vulnerable to other health concerns. Irregular and unstable food supply along with low quality of food due to insufficient or inadequate nutrient intake can compromise immunity and make individuals more susceptible to infections. Additionally, if infected, matters tend to become worse because infections may further reduce nutritional and health status, thereby aggravating malnutrition and reinforcing its cycle with poverty ( 25 , 26 ).
A vicious cycle exists through which both poverty and malnutrition fuel and reinforce each other ( 25 ). Globally, the poorest countries are the countries bearing the highest burden of malnutrition. Nutritional imbalances reduce work capacity and human capital; and this makes countries more susceptible to poverty. Furthermore, malnutrition is also a consequence of poverty, as poverty increases food insecurity and hidden hunger; which contributes to the problem of malnutrition. This makes both these elements a cause and a consequence of each other. Establishing a linear relationship between the two would overlook the complexities and nuances that exist within the framework of this topic.
What Will be the Next Steps?
In order to progress socially and economically, there is an urgent need to recognize the burden of poverty and malnutrition and to take immediate steps to break the ongoing cycle. To achieve this target, it is important to understand what factors feed and reinforce it.
The cycle of poverty and malnutrition appears to be intergenerational. Evidence suggests that malnourished women are at a higher risk of having malnourished children and this creates an intergenerational effect ( 6 ). It is imperative to intervene early in life in order to maximize the effectiveness of interventions and break the cycle. The Lancet Nutrition Series ( 27 ) modeled the effect of 10 evidence based nutrition specific interventions on lives saved in the 34 countries that have 90% of the world's children with stunted growth. The series also examined the effect of various delivery platforms and delivery options using community health workers to engage poor populations and promote behavior change, access to and uptake of these interventions. Findings suggest that the current total of deaths in children younger than 5 years can be reduced by 15% if populations can access these 10 evidence-based nutrition interventions at 90% coverage. These nutrition specific interventions included salt iodization, multiple micronutrient supplementation in pregnancy (includes iron-folate), calcium supplementation in pregnancy, energy-protein supplementation in pregnancy, vitamin A supplementation in childhood, zinc supplementation in childhood, breastfeeding promotion, complementary feeding education, complementary food supplementation, and management of severe acute malnutrition in children. The findings also support the use of various community engagement and delivery strategies that can help reach poor segments of the population at greatest risk in order to make a difference ( 27 ). In other words, the interventions need to reach the poorest of the poor to break the cycle of malnutrition and poverty and should also incorporate disease and infection prevention as a part of their strategy ( 25 ).
Considering the inter-linkages described above between malnutrition and poverty, nutrition specific interventions need to be augmented with nutrition sensitive interventions in order to accelerate the progress of reducing malnutrition. Nutrition sensitive interventions are those that address intermediate and underlying causes of malnutrition and help to improve access to nutritious food, clean water and sanitation, education and employment, and health care etc. Large scale nutrition programs focusing on evidence based nutrition interventions should also target key underlying determinants of nutrition including poverty in order to enhance the coverage and effectiveness of nutrition-specific interventions. These include interventions in the sectors of agriculture, social safety nets, early child development, education, and women's empowerment. Women's empowerment is instrumental in not only improving malnutrition but general well-being ( 28 ). Hence, a parallel focus on nutrition sensitive and nutrition specific interventions has the potential to greatly accelerate progress in not only the areas of nutrition but also break the intergenerational cycle of malnutrition and poverty ( 29 ). More recently, bio-fortification and agricultural biodiversity are also considered to have the potential to cater to the issues of poverty and malnutrition in a parallel manner ( 30 ). In developing countries, bio-fortification could focus on improving quality of coarse cereals, as well as fodders along with community participatory approaches to enhance agricultural biodiversity. This approach not only could contribute to a reduction in malnutrition and poverty, but reduce food insecurity and improve sustainability ( 31 , 32 ), though further research is needed in the domain ( 30 , 31 ). Income disparity is also a factor that allows the malnutrition-poverty cycle to persist. In fact, a country may experience economic growth, but still have widespread poverty and high levels of malnutrition. This is because income inequality translates as health inequality; as the income gap grows, so does health disparity ( 7 , 13 , 25 ). Furthermore, gender inequities have also been associated with both poverty and malnutrition as a result of lower opportunities for women in the fields of education and employment. A recent analysis based on data from 49 low- and middle-income countries assessing the relationship between gender equity and malnutrition and health suggests that gender equity in education and employment decreases child malnutrition and is an important determinant in nutrition and access to health care ( 33 ). Therefore, any attempt to improve global nutritional status and to achieve the targets set by the “2030 Agenda for Sustainable Development” requires a focus on alleviating poverty and simultaneously focusing on agriculture, social safety nets, early child development, education, and strengthening women's position in society ( 34 – 37 ).
Nutritional interventions should be designed in an all-rounded, holistic manner. It would be fruitful to involve multiple stakeholders including health, education, agriculture, water, sanitation and hygiene, gender and economics. To ensure sustainability, nutritional interventions should be context-specific and should also be cost-effective since these issues concern low and middle income countries.
Ending poverty in all its forms is the first of the 17 Sustainable Development Goals and ending hunger, reducing food insecurity and improved nutrition and agriculture is the second goal. Furthermore, at least 12 of the 17 goals contain indicators that are highly relevant to nutrition. Poverty and malnutrition are deeply interrelated, with each fuelling the other and hence it is imperative to tackle both issues simultaneously rather than in parallel silos. A two-way link exists, with both elements being the cause and consequence of each other. This vicious cycle remains a prime public health concern and immediate strides need to be made against it. For a sustainable improvement in nutritional outcomes, the battle against poverty and malnutrition has to be fought on all fronts, to achieve a healthier and more equitable society.
Author Contributions
All authors contributed to the study and the write-up.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.

IMAGES
VIDEO
COMMENTS
Poverty, Racism, and the Public Health Crisis in America
Poverty and Health. Adriana Lleras-Muney, Hannes Schwandt & Laura Wherry. Working Paper 32866. DOI 10.3386/w32866. Issue Date August 2024. Poverty is strongly associated with worse health across countries and within countries across individuals. However, not all poor individuals suffer from poor health: the effects of poverty on health vary ...
Full article: Defining the characteristics of poverty and their ...
Introduction. Poverty and ill-health are inter-linked. The bilateral associations between poverty and ill-health result in a vicious cycle, especially in less developed countries with inadequate healthcare and welfare support systems [].The classic conceptual framework on poverty-health vicious cycle proposed by Wagstaff illustrated that ill-health affects individuals' financial status ...
Health and health system effects on poverty: A narrative ...
Poverty and mental health: policy, practice and research ...
Abstract. Why are people who live in poverty disproportionately affected by mental illness? We review the interdisciplinary evidence of the bidirectional causal relationship between poverty and common mental illnesses-depression and anxiety-and the underlying mechanisms. Research shows that mental illness reduces employment and therefore income ...
The health of individuals living in poverty poses greater challenges from policy, practice, and research standpoints. Public health professionals are poised uniquely to be advocates for the marginalized, be the resource persons for health education, implement health promotion programs, and conduct research to understand health effects of ...
866 August 2024JEL No. H50, I1, I14, I18, I30ABSTRACTPoverty is strongly associated with worse health a. ross countries and within countries across individuals. However, not all poor individuals suffer from poor health: the. ffects of poverty on health vary across place and time. In this review, we discuss the evidence documenti.
The Journal of Community & Applied Social Psychology publishes papers that cover the full spectrum of community and social psychology. ... mental health, and poverty research and advocacy work. 2.2 Inclusion criteria. Several inclusion criteria were applied. First, studies had to be primary research reported in peer-reviewed journals and ...
Public Health Challenges is a multidisciplinary journal addressing all areas of public health research, policy, and practice, and supporting the One Health agenda. ... The 15,143 journal papers on poverty were published in 36 languages; however, the top 10 languages were European and Chinese. The three most common languages of publication were ...
Poverty, depression, and anxiety: Causal evidence and ...
Since poverty is a global problem and poverty alleviation attracts worldwide attention, especially in developing countries, many scholars associate it with economic growth and diversification of poverty alleviation measures such as government spending and transfers, infrastructure development, and agricultural technology upgrading (Leng et al., 2021).
The health of individuals living in poverty poses greater challenges from policy, practice, and research standpoints. Public health professionals are poised uniquely to be advocates for the marginalized, be the resource persons for health education, implement health promotion programs, and conduct research to understand health effects of ...
This glossary addresses the complex nature of poverty and raises some conceptual and measurement issues related to poverty in the public health literature, with a focus on poor countries. ... Center for Research on Population and Health, American University of Beirut, Beirut 1107 2020, Lebanon; mk36aub.edu.lb;
The association between income and life expectancy, already well established, was detailed in a landmark 2016 JAMA study by Raj Chetty, PhD, of Stanford University, and colleagues. This study found a gap in life expectancy of about 15 years for men and 10 years for women when comparing the most affluent 1% of individuals with the poorest 1%.
The impact of food insecurity on health outcomes: empirical ...
This paper investigates how climate change and poverty affect child health inequality across 63 provinces in Vietnam from 2006 to 2023. By examining deaths and economic losses from storms and floods, we assess climate change's impact; while, infant mortality rate (IMR) and under-5 mortality rate (U5MR) serve as indicators of child health inequality. Findings reveal that climate change ...
To date, participatory research and peer involvement is widely underrepresented and should play a much more influential role in scientific studies and policies for mental health . On a neighborhood level, solidarity and mutual support appears to represent important mediators between neighborhood poverty and individual mental health.
Subsequent Effects of Children Growing Up Poor
Poverty and Health - The Family Medicine Perspective ...
Housing insecurity can be understood as experiencing or being at risk of multiple house moves that are not through choice and related to poverty. Many aspects of housing have all been shown to impact children/young people's health and wellbeing. However, the pathways linking housing and childhood health and wellbeing are complex and poorly understood.
Economic circumstances and related factors, including unemployment and poverty, can have substantial effects on suicide rates. This relationship applies in all countries, irrespective of their World Bank income status or level of development. Therefore, means of mitigating such influences are essential components of strategies to reduce suicides. In this Series paper, we consider examples of ...
This analysis presents the association between measures of poverty and health care activity, rather than attempting to isolate any causal relationship between poverty and health care activity. ... Research from The Health Foundation found that people with four or more conditions had an average of 8.9 outpatient visits and 24.6 GP visits over a ...
The Lancet Public Health series A Public Health Approach to Suicide Prevention is timely and represents the most comprehensive appraisal of a public health approach to suicide prevention yet published. A concerted focus on social factors and social determinants is urgently needed as the cost-of-living crisis, inflation, a weakened public sector, and housing problems are, sadly, all too common ...
The Social Consequences of Poverty: An Empirical Test on ...
In Brazil, menstrual health is poorly documented and period poverty remains a significant concern among low-income populations with less than half of elementary students disposing of the necessary materials to manage their periods. 20 Beyond period poverty, little is known about early adolescents' experiences of menstruation related to their ...
On a meso-level, on neighborhood-related poverty as a factor in individuals' mental illness. On a macro-level, on effects of income inequality on mental health. In several studies, it has been shown that on each level, poverty has a profound impact on mental health, though it must be noted that in some fields, research is still scarce.
Changing the Narrative on Suicide is the theme for World Suicide Prevention Day marked on September 10th with the call to action Start the Conversation. In line with this call a six-paper Series in this issue of The Lancet Public Health proposes a new narrative for suicide prevention. The Series describes a public health approach to suicide prevention that puts suicide prevention in the focus ...
The Intertwined Relationship Between Malnutrition and ...