- Mayo Clinic Careers
- Anesthesiology
- Dermatology
- Emergency Medicine
- Family Medicine
- Internal Medicine
- Lung Transplant
- Psychiatry & Psychology
- Nurse Practitioner & Physician Assistant
- Ambulance Service
- Clinical Labs
- Med Surg RN
- Radiology Imaging
- Clinical Research Coordinator
- Respiratory Care
- Senior Care
- Surgical Services
- Travel Surgical Tech
- Practice Operations
- Administrative Fellowship Program
- Administrative Internship Program
- Career Exploration
- Nurse Residency and Training Program
- Nursing Intern/Extern Programs
- Residencies & Fellowships (Allied Health)
- Residencies & Fellowships (Medical)
- SkillBridge Internship Program
- Training Programs & Internships
- Diversity, Equity & Inclusion
- Employees with Disabilities

Life-changing careers

Search life-changing careers.
Search by Role or Keyword
Enter Location
- United States Applicants
- United Kingdom Applicants
- Current Employees
To improve health care and offer new solutions and hope for patients, Mayo Clinic conducts basic, translational, clinical and epidemiological research at its campuses in Arizona, Florida and Minnesota and throughout Mayo Clinic Health System. Researchers investigate today’s medical mysteries, generating new knowledge and translating discoveries into therapies to advance patient care. You will become a vital member of a dynamic health care team, where you’ll experience the exceptional environment of one of the world’s cutting edge health care institutions.
You will discover a culture of teamwork, professionalism and mutual respect, with colleagues who inspire you to stretch and grow. Most of all, you will find a career that can change your life!
Research Jobs
- Paid Intern - Physiology and Biomedical Engineering 334326 Research Scottsdale, Arizona
- RTP-RESEARCH FELLOW-LS-Jaroszewski 334096 Research Phoenix, Arizona
- Graduate Research Employment Program - Rad Onc Research - Limited Tenure 334219 Research Rochester, Minnesota
- RTP-RESEARCH ASSOCIATE-LS 332996 Research Rochester, Minnesota
- Paid Education Student Intern - Urology 334116 Research Phoenix, Arizona
- Graduate Research Employment Program - Medina Lab (1 Year Limited Tenure) 333430 Research Rochester, Minnesota
- Graduate Research Employment Program - Immunology (1 Year Limited Tenure) 334238 Research Scottsdale, Arizona
- Research Fellow - Gastroenterology and Hepatology 334068 Post Doctoral Rochester, Minnesota
- RTP-Research Associate - Juna Musa 333297 Research Rochester, Minnesota
- Research Assistant - Orthopedics Res 333107 Research Rochester, Minnesota
Equal opportunity
All qualified applicants will receive consideration for employment without regard to race, color, religion, sex, gender identity, sexual orientation, national origin, protected veteran status, or disability status. Learn more about "EEO is the Law." Mayo Clinic participates in E-Verify and may provide the Social Security Administration and, if necessary, the Department of Homeland Security with information from each new employee's Form I-9 to confirm work authorization.
Reasonable accommodations
Mayo Clinic provides reasonable accommodations to individuals with disabilities to increase opportunities and eliminate barriers to employment. If you need a reasonable accommodation in the application process; to access job postings, to apply for a job, for a job interview, for pre-employment testing, or with the onboarding process, please contact HR Connect at 507-266-0440 or 888-266-0440.
Job offers are contingent upon successful completion of a post offer placement assessment including a urine drug screen, immunization review and tuberculin (TB) skin testing, if applicable.
Recruitment Fraud
Learn more about recruitment fraud and job scams
Advertising
Mayo Clinic is a not-for-profit organization and proceeds from Web advertising help support our mission. Mayo Clinic does not endorse any of the third party products and services advertised.
Advertising and sponsorship policy | Advertising and sponsorship opportunities
Reprint permissions
A single copy of these materials may be reprinted for noncommercial personal use only. "Mayo," "Mayo Clinic," "MayoClinic.org," "Mayo Clinic Healthy Living," and the triple-shield Mayo Clinic logo are trademarks of Mayo Foundation for Medical Education and Research.
Any use of this site constitutes your agreement to the Terms and Conditions and Privacy Policy linked below.
Terms and Conditions | Privacy Policy | Notice of Privacy Practices | Notice of Nondiscrimination
© 1998-2024 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved.
Join Our Talent Community
Sign up, stay connected and get opportunities that match your skills sent right to your inbox
Email Address
Phone Number
Upload Resume/CV (Must be under 1MB) Remove
Job Category* Select One Advanced Practice Providers Business Education Engineering Executive Facilities Support Global Security Housekeeping Information Technology Internship Laboratory Nursing Office Support Patient Care - Other Pharmacy Phlebotomy Physician Post Doctoral Radiology Imaging Research Scientist Surgical Services Therapy
Location Select Location Albert Lea, Minnesota Arcadia, Wisconsin Austin, Minnesota Barron, Wisconsin Bloomer, Wisconsin Caledonia, Minnesota Cannon Falls, Minnesota Chippewa Falls, Wisconsin Decorah, Iowa Duluth, Minnesota Eau Claire, Wisconsin Fairmont, Minnesota Faribault, Minnesota Holmen, Wisconsin Jacksonville, Florida La Crosse, Wisconsin Lake City, Minnesota London, England Mankato, Minnesota Menomonie, Wisconsin Minneapolis-St. Paul-Bloomington, Minnesota New Prague, Minnesota Onalaska, Wisconsin Osseo, Wisconsin Owatonna, Minnesota Phoenix, Arizona Prairie du Chien, Wisconsin Red Wing, Minnesota Rice Lake, Wisconsin Rochester, Minnesota Saint Cloud, Minnesota Saint James, Minnesota Scottsdale, Arizona Sparta, Wisconsin Tomah, Wisconsin Waseca, Minnesota Zumbrota, Minnesota
Area of Interest Select One Nursing Research Radiology Laboratory Medicine & Pathology Facilities Licensed Practical Nurse (LPN) Neurology Pharmacy Cardiovascular Medicine Surgery Physical Medicine & Rehabilitation General Services Psychiatry & Psychology Respiratory Therapy Finance Environmental Services Mayo Collaborative Services Ambulance Services Mayo Clinic Laboratories Surgical Technician Anesthesiology & Perioperative Medicine Emergency Medicine Social Work Gastroenterology & Hepatology Information Technology Family Medicine International Hospital Internal Medicine Medical Oncology Orthopedics Radiation Oncology Global Security Housekeeping Administration Education Hematology Patient Scheduling Pediatrics Senior Care Transplant Cardiovascular Surgery General Internal Medicine Hospice & Palliative Care Obstetrics & Gynecology Ophthalmology Critical Care Office Support Pulmonary/Sleep Medicine Engineering Dermatology Urology Artificial Intelligence & Informatics Desk Operations Oncology Physiology & Biomedical Engineering Sports Medicine Biochemistry & Molecular Biology Clinical Genomics Community Internal Medicine Health Care Delivery Research Linen & Central Services Nephrology & Hypertension Surgical Assistant Digital Endocrinology Immunology Infectious Diseases Neurosciences Otolaryngology (ENT) Quality Regenerative Biotherapeutics Rheumatology Business Development Cancer Center Epidemiology Molecular Medicine Molecular Pharmacology & Experimental Therapeutics Neurologic Surgery Primary Care Clinical Trials & Biostatistics Development/Philanthropy Healthcare Technology Management Information Security Legal Marketing Pain Medicine Women's Health Allergic Diseases Bariatric Medicine Cancer Biology Center for Individualized Medicine Clinical Nutrition Communications Comparative Medicine Dental Specialities Geriatric Medicine & Gerontology Informatics Mayo Clinic Platform Occupational/Preventative Medicine Spine Center Spiritual Care Travel Urgent Care Volunteer Services
Confirm Email
By submitting your information, you consent to receive email communication from Mayo Clinic.
Make Caring Your Career
Make Caring Your Career™
ExploreHealthCareers.org is a collaboration between today’s health professionals and leading health care associations designed to help people like you start down the road toward a career in health. Here you’ll find the latest health career information and tools to guide you as you prepare for a future in health care.
We'll help you find the answer.
We offer over 100 health care career profiles.
Submit to multiple programs with a single form.

- Anesthesiologist Assistant
- Blood Bank Technology Specialist
- Cardiopulmonary Rehabilitation Specialist
- Cardiovascular Technologist / Technician
- Medical Laboratory Scientist/Technician
- Community Health Worker
- Cytotechnologist
- Diagnostic Medical Sonographer
- Emergency Medical Technician
- Genetic Counselor
- Health Care Interpreter
- Health Information Manager
- Healthcare Documentation Specialist
- Home Care Assistant/Aide
- Medical Assistant
- Medical Coder
- Medical Dosimetrist
- Neurodiagnostic Technologist
- Nuclear Medicine Technologist
- Nurses Aide / Assistant
- Ophthalmic Laboratory Technician
- Ophthalmic Medical Technician
- Optician (Dispensing)
- Orientation & Mobility Specialist
- Pathologists’ Assistant
- Perfusionist
- Phlebotomist
- Radiologic Technologist
- Respiratory Therapist
- Surgical Technologist

- Art Therapist
- Medical Illustrator / Animator
- Medical Librarian

- Chiropractor

- Acupuncture/Oriental Medicine Practitioner
- Massage Therapist
- Allied Dental Educator
- Dental Assistant
- Dental Hygienist
- Dental Laboratory Technician

- Built Environment Specialist
- Environmental Health Advocate
- Environmental Health Practitioner
- Food Safety Specialist
- Occupational Health and Safety Expert

- Crime Scene Investigator
- Forensic Biologist
- Forensic Chemist
- Forensic Odontologist
- Forensic Pathologist
- Forensic Toxicologist

- Geriatric Pharmacist
- Geriatric Psychiatrist
- Geriatric Staff Nurse
- Geriatrician
- Health Administrator

- Dental Informaticist
- Nursing Informaticist

- Allopathic Physician (M.D.)
- Osteopathic Physician (D.O.)
- Physician Assistant
- Psychiatrist – DO/MD
- Psychologist
- Psychometrist
- Rehabilitation Counselor

- Naturopathic Physician

- Clinical Nurse Specialist
- Licensed Practical/Vocational Nurse
- Nurse Anesthetist
- Nurse Educator
- Nurse Midwife
- Nurse Practitioner
- Nurse Researcher
- Occupational Health Nurse
- Pediatric Nurse
- Public Health Nurse
- Registered Nurse (RN)

- Dietitian Nutritionist
- Nutrition and Dietetic Technician

- Occupational Therapist
- Occupational Therapy Aide
- Occupational Therapy Assistant

- Optometrist
- Orthotist and Prosthetist

- Pharmaceutical Scientist
- Medical Science Liaison
- Regulatory Affairs Specialist

- Pharmacy Technician

- Physical Therapist
- Physical Therapist Assistant

- Behavioral Science/Health Education
- Biomedical and Laboratory Practice
- Biostatistics
- Environmental Health Sciences
- Epidemiology
- Global Health
- Health Services Administration
- Maternal and Child Health
- Public Health Practice and Program Management
- Social Worker

- Audiologist (Doctor of Audiology)
- Speech-Language Pathologist

- Athletic Trainer
- Exercise Physiologist
- Kinesiotherapist
- Primary Care Sports Medicine Physician

- Animal Behaviorist
- Veterinarian
- Veterinary Technologist/Technician
- Student/Faculty Portal
- Learning Hub (Brightspace)
- Continuous Professional Development

What does a nurse do?
The fundamentals of nursing are to deliver direct patient care and act as an advocate and health educator for patients, families, and communities.
Nurses work to promote health, prevent disease, and help patients with illnesses. When treating a patient, they observe, assess, and record symptoms, reactions, and progress. Nurses work alongside doctors when it comes to treatment plans and exams, administering medications, and monitoring patient recovery.
Scope of practice
Nurses can work in any specialty area across many different areas of the hospital. Each area will have a different set of responsibilities, but a common set of duties includes:
- Patient intake and obtaining measurements, vitals, and health histories
- Monitoring patient vitals regularly
- Giving medication, recording doses, and timing
- Performing hands-on technical, and medical duties
- Communicating with patients about their care plan
- Charting and working with electronic health record software
- Relaying important information to the treating physician and other healthcare staff as needed
Unless you are a nurse practitioner, nurses do not prescribe medication or make diagnoses, but they do carry out physicians’ orders for administering medication and other items on a patient’s care plan.
Types of nurses
There are several different types of nurses. Nurses are needed in virtually every area of medicine. Depending on your level of education, interests, and experience level, you can excel in any area of medicine.
Different types of nursing degrees by level of education or certification
The field of nursing offers several levels of practice, each with different educational requirements.
Licensed practical nurse (L.P.N.)
Under the supervision of registered nurses and physicians, L.P.N.s may care for patients of all ages. Using learned technical skills, L.P.N.s assist patients in meeting their physical and psychosocial needs. They also administer medications and perform treatments.
Many employment opportunities are available to L.P.N.s in hospitals, clinics, nursing homes and home care. Graduates are awarded a diploma or certificate in practical nursing and are eligible to apply to take the National Council Licensure Examination for Practical Nurses (NCLEX-PN) .
Registered nurse (R.N.): Associate degree
The associate degree nursing program is designed to prepare graduates who administer safe, patient-centered nursing care in hospitals, home settings, nursing homes, clinics, and other healthcare facilities. Graduates are awarded an Associate of Science degree in nursing and are eligible to apply to take the National Council Licensure Examination for Registered Nurses (NCLEX-RN) .
Registered nurse (R.N.): Bachelor's degree with a major in nursing
The bachelor's degree in nursing is designed to provide opportunities for students to develop a sound theoretical and clinical foundation for the practice of professional (registered) nursing. Graduates are prepared for a variety of roles in hospitals, nursing homes, and community health settings. Graduates are awarded a Bachelor of Science degree in nursing and are eligible to take the National Council Licensure Examination (NCLEX-RN) .
Advanced clinical practice registered nurse (A.P.R.N.): Master's and doctoral degrees
Registered nurses with advanced training in education, research, administration, transcultural nursing, nursing leadership, and information technology — master's and doctoral degrees
Advanced clinical practice registered nurse and other advanced training: Master's degree and doctoral degree (Ph.D., D.N.P.)
Graduate study in nursing is designed to expand students' base of theoretical knowledge in nursing. Through scholarly inquiry, nurses in the master's program are prepared to manage and facilitate complex health care in many settings. The master's-prepared nurse may assume roles such as clinical nurse specialist, nurse educator, nurse practitioner , nurse-midwife , nurse anesthetist , or nurse administrator.
Doctoral programs prepare nurse scholars who generate, expand and disseminate nursing knowledge. They assume roles in practice, research, and education as advanced clinicians, administrators, educators, researchers, or policymakers.
Nursing is a profession in which your education, knowledge, skills, and experiences provide career flexibility and variety and can offer continued advancement and growth.
Different types of nurses by medical specialty field, department, or population
Nurses have the flexibility to work throughout the hospital or medical clinic in a variety of medical specialties. Working in a specific specialty or with a specific population of patients means you’ll typically work with patients experiencing common symptoms or being treated for similar conditions.
Another way to decide which type of nurse you want to become is by how the work unit is organized within the hospital. Working in a specific department still allows you to see and help treat a wide variety of patients with a variety of conditions and symptoms.
Common areas of specialization by medical specialty, department, or population include:
- Cardiac care nurse
- Emergency room nurse
- Family medicine nurse
- Geriatric nurse
- Intensive care unit (ICU) registered nurse
- Labor and delivery nurse
- Neonatal intensive care unit (NICU) nurse
- Neurology nurse
- Obstetrics (OB) nurse
- Oncology nurse
- Operating room (OR) nurse
- Pediatric nurse
- Surgical nurse
- Women’s health nurse
- Among many others
Work environment
On a given day, nurses may work with doctors, residents, nursing assistants, home health aides, speech therapists, occupational therapists, other nurses, and patients of all ages, from infants to the elderly.
Hospital work environment: In hospitals, nurses may be assigned to several patients from their unit and will check in on the patients throughout their shift, administering medications as needed, as well as writing down any symptoms or information on their condition.
Clinic work environment : In a clinic setting, nurses will often do patient intake, which involves taking vitals and entering basic health information for patients before they see the doctor, administering vaccinations, and delivering medications.
Laboratory work environment : Nurses in laboratory roles will mainly draw blood for a variety of tests and may monitor patients for urine tests or gather other fluid samples.
Positions can be anywhere from 10 to 40+ hours a week, and nurses often need to cover shifts on some holidays and weekends. Nurses are employed in hospitals, medical clinics, schools, nursing homes, and home health agencies.
Becoming a nurse
All paths to becoming a nurse require post-secondary education. Candidates for careers in nursing should be comfortable working closely with people from diverse backgrounds and should be motivated to help sick patients feel better.
In any nursing role, multitasking and time management are essential skills to being successful at managing patients in a fast-paced healthcare environment. Empathy and good communication are important factors in providing quality nursing care; developing positive relationships with your patients and their families helps patients feel better and more comfortable in a clinic or hospital.
Many nurses choose their profession based on a desire to work in health care and are determined to make a difference in the lives of others on a daily basis. Regardless of the setting — hospital, clinic, or laboratory — nurses may spend significantly more time with a patient than the treating physician, so there are daily opportunities to leave a lasting impression on people from your community.
Higher education requirements
The field of nursing offers several levels of practice, each with different educational requirements. To practice, some nurses earn a certificate while others complete a doctorate.
After completing high school and receiving a high school diploma (or equivalent), the career path of a nurse typically includes the following:
- A licensed practical nurse (L.P.N.) must earn a certificate, complete clinical training, and pass an exam to practice.
- A registered nurse (R.N.) must earn an associate degree or a bachelor’s degree, complete clinical training, and pass an exam to practice. Many R.N.s choose to get certified in a specialty area, which can increase earnings and career opportunities.
- An advanced practice registered nurse (A.P.R.N.) typically has several years of experience as an R.N. and then goes on to acquire further graduate-level training.
Career opportunities and outlook
The Bureau of Labor Statistics expects the employment of nurses to grow as fast as average, and jobs may increase by 9 percent by 2030. Opportunities should be excellent for nurses with advanced education and training. Some states report current and projected shortages of nurses, primarily due to an aging workforce and recent declines in nursing school enrollments.
With experience, L.P.N.s may advance to supervisory positions or complete an education program to become an R.N.
With experience and continuous education, R.N.s can move into supervisory or leadership roles such as assistant clinical nurse manager, charge nurse, head nurse, assistant director or director of nursing, vice president of nursing, or chief nursing officer.
Some R.N.s complete a graduate degree to become A.P.R.N.s, while some nurses move into the business side of health care or work as professors or researchers at colleges and universities.
Nursing programs at Mayo Clinic
Mayo Clinic School of Health Sciences provides exceptional clinical training experiences through many affiliated nursing education programs.
- Cardiology Nurse Practitioner Fellowship (Arizona)
- Heart Rhythm Device Nurse Fellowship (Arizona)
- Perioperative Nursing Fellowship (Arizona)
- Nurse Practitioner Clinical Education Collaboration (Minnesota)
- Nurse Practitioner Clinical Rotation (Arizona)
- Nurse Practitioner Clinical Rotation (Florida)
- Nurse Practitioner or Physician Assistant Abdominal Organ Transplant Fellowship (Arizona)
- Nurse Practitioner or Physician Assistant Critical Care Fellowship (Florida)
- Nurse Practitioner or Physician Assistant Critical Care Fellowship (Minnesota)
- Nurse Practitioner or Physician Assistant Emergency Medicine Fellowship (Minnesota)
- Nurse Practitioner or Physician Assistant Hematology Fellowship (Minnesota)
- Nurse Practitioner or Physician Assistant Hospice and Palliative Medicine Fellowship (Arizona)
- Nurse Practitioner or Physician Assistant Urology Fellowship (Minnesota)
- Nursing Clinical Education (Florida)
Browse similar careers

Hemodialysis technician

Nurse midwife

Nurse practitioner
Careers in healthcare: Let us help you find your fit
- U.S. Department of Health & Human Services

- Virtual Tour
- Staff Directory
- En Español

May Is Celiac Awareness Month
Following a gluten-free diet can relieve celiac disease symptoms and heal damage in the small intestine.
Learn more »

Join Us for Healthy Vision Month 2024!
NEI is shining a light on vision loss and mental health — and sharing steps people with a visual impairment can take to thrive in their daily lives.

RECOVER Initiative launches clinical trials evaluating treatments for exercise intolerance, post-exertional malaise, and sleep disturbances.

Celebrating at graduation this year?
Talk with your high school grads about celebrating safely.

STEM Teaching Resources
Innovative NIH-funded content to engage K-12 students in health science.
In the News

High-Risk Prostate Cancer
New urine test can identify aggressive cancers that need treatment

Parents Lost to Overdose
From 2011-21, more than 321,000 children lost a parent to a drug overdose.

Alzheimer’s Disease
People with two copies the APOE4 gene are at much higher risk.

Fentanyl Pill Seizures
Law enforcement sees massive jump in confiscated amount of the drug.
NIH at a Glance
Virtual-tour-screenshot-square.jpg.

Take the Virtual Tour
Explore the Bethesda campus and how NIH turns discovery into health.
monica-bertagnolli-thumbnail.jpg

The NIH Director
Monica M. Bertagnolli, M.D., is the NIH Director and provides leadership for the 27 Institutes and Centers that make up NIH.
nih-at-a-glance-funding.jpg

Funding for Research
NIH is the largest source of funding for medical research in the world, creating hundreds of thousands of high-quality jobs.
nih-at-a-glance-labs.jpg

Labs at NIH
Scientists conduct research on NIH campuses across the U.S., as part of our Intramural Research Program.
improving-health-collage.jpg

Impact of NIH Research
NIH-supported research has had a major positive impact on nearly all of our lives.
researcher-holding-petri-dish.jpg

Jobs at NIH
The central recruitment point of access to all NIH jobs and training opportunities
A public-private partnership to develop a coordinated research strategy to speed the most promising COVID-19 vaccines and treatments.
Rapid Acceleration of Diagnostics (RADx)
An initiative to speed innovation in the development, commercialization, and implementation of technologies for COVID-19 testing.
A new research initiative to understand, prevent, and treat the long-term effects of COVID-19.
COVID-19 Treatment Guidelines
Guidelines from NIH for the diagnosis, treatment, and control of COVID-19.
Research information from NIH
NIH supports research in COVID-19 testing, treatments, and vaccines. También disponible en español.
NIH COVID-19 Safety Plan
Guidance to NIH staff, including employees, contractors, trainees, and volunteers, related to COVID-19.
Featured Resources & Initiatives
A new science agency proposed by President Joseph Biden as part of NIH to drive biomedical breakthroughs and provide transformative solutions for all patients.
Anti-Sexual Harassment
NIH does not tolerate pervasive or severe harassment of any kind, including sexual harassment.
Ending Structural Racism
Learn more about NIH’s efforts to end structural racism in biomedical research through the UNITE initiative.
All of Us Research Program
A research effort to revolutionize how we improve health and treat disease.
NIH HEAL Initiative
Trans-agency effort to speed scientific solutions to stem the national opioid crisis.
Clinical Trials
Learn about participating in clinical trials and where to find them.
Accelerating Medicines Partnership
A bold venture to help identify new treatments and cures for diseases.
Medical Research Initiatives
Important initiatives aimed at improving medical research.
Training at NIH
NIH provides training opportunities internally, as well as at universities and other institutions across the U.S.
Connect with Us
- More Social Media from NIH
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Institute of Medicine (US) Committee on Health Research and the Privacy of Health Information: The HIPAA Privacy Rule; Nass SJ, Levit LA, Gostin LO, editors. Beyond the HIPAA Privacy Rule: Enhancing Privacy, Improving Health Through Research. Washington (DC): National Academies Press (US); 2009.

Beyond the HIPAA Privacy Rule: Enhancing Privacy, Improving Health Through Research.
- Hardcopy Version at National Academies Press
3 The Value, Importance, and Oversight of Health Research
The previous chapter reviewed the value of privacy, while this chapter examines the value and importance of health research. As noted in the introduction to Chapter 2 , the committee views privacy and health research as complementary values. Ideally, society should strive to facilitate both for the benefit of individuals as well as the public.
In addition to defining health research and delineating its value to individuals and society, this chapter provides an overview and historical perspective of federal research regulations that were in place long before the Privacy Rule was implemented. Because a great deal of medical research falls under the purview of multiple federal regulations, it is important to understand how the various rules overlap or diverge. The chapter also explains how the definition of research has become quite complex under the various federal regulations, which make a distinction between research and some closely related health practice activities that also use health data, such as quality improvement initiatives.
The chapter also reviews the available survey data regarding public perceptions of health research and describes the importance of effective communication about health research with patients and the public.
- CONCEPTS AND VALUE OF HEALTH RESEARCH
Definitions
Under both the Health Insurance Portability and Accountability Act (HIPAA) Privacy Rule and the Common Rule , “research” is defined as “a systematic investigation, including research development, testing and evaluation, designed to develop or contribute to generalizable knowledge.” This is a broad definition that may include biomedical research, epidemiological studies, 1 and health services research, 2 as well as studies of behavioral, social, and economic factors that affect health.
Perhaps the most familiar form of health research is the clinical trial, in which patients volunteer to participate in studies to test the efficacy and safety of new medical interventions. But an increasingly large portion of health research is now information based. A great deal of research entails the analysis of data and biological samples that were initially collected for diagnostic, treatment, or billing purposes, or that were collected as part of other research projects, and are now being used for new research purposes. This secondary 3 use of data is a common research approach in fields such as epidemiology, health services research, and public health research, and includes analysis of patterns of occurrences, determinants, and natural history of disease; evaluation of health care interventions and services; drug safety surveillance; and some genetic and social studies ( Lowrance, 2002 ; Lowrance and Collins, 2007 ).
The Importance of Health Research
Like privacy, health research has high value to society. It can provide important information about disease trends and risk factors, outcomes of treatment or public health interventions, functional abilities, patterns of care, and health care costs and use. The different approaches to research provide complementary insights. Clinical trials can provide important information about the efficacy and adverse effects of medical interventions by controlling the variables that could impact the results of the study, but feedback from real-world clinical experience is also crucial for comparing and improving the use of drugs, vaccines, medical devices, and diagnostics. For example, Food and Drug Administration (FDA) approval of a drug for a particular indication is based on a series of controlled clinical trials, often with a few hundred to a few thousand patients, but after approval it may be used by millions of people in many different contexts. Therefore, tracking clinical experience with the drug is important for identifying relatively rare adverse effects and for determining the effectiveness in different populations or in various circumstances. It is also vital to record and assess experience in clinical practice in order to develop guidelines for best practices and to ensure high-quality patient care.
Collectively, these forms of health research have led to significant discoveries, the development of new therapies, and a remarkable improvement in health care and public health. 4 Economists have found that medical research can have an enormous impact on human health and longevity, and that the resulting increased productivity of the population contributes greatly to the national economy ( Hatfield et al., 2001 ; Murphy and Topel, 1999 ) in addition to the individual benefits of improved health. If the research enterprise is impeded, or if it is less robust, important societal interests are affected.
The development of Herceptin as a treatment for breast cancer is a prime example of the benefits of research using biological samples and patient records ( Box 3-1 ) ( Slamon et al., 1987 ). Many other examples of findings from medical records research have changed the practice of medicine as well. Such research underlies the estimate that tens of thousands of Americans die each year from medical errors in the hospital, and research has provided valuable information for reducing these medical errors by implementing health information technology, such as e-prescribing ( Bates et al., 1998 ; IOM, 2000b ). This type of research also has documented that disparities in health care and lack of access to care in inner cities and rural areas result in poorer health outcomes ( Mick et al., 1994 ). Furthermore, medical records research has demonstrated that preventive services (e.g., mammography) substantially reduce mortality and morbidity at reasonable costs ( Mandelblatt et al., 2003 ), and has established a causal link between the nursing shortage and patient health outcomes by documenting that patients in hospitals with fewer registered nurses are hospitalized longer and are more likely to suffer complications, such as urinary tract infections and upper gastrointestinal bleeding ( Needleman et al., 2002 ). These findings have all informed and influenced policy decisions at the national level. As the use of electronic medical records increases, the pace of this form of research is accelerating, and the opportunities to generate new knowledge about what works in health care are expanding ( CHSR, 2008 ).
Examples of Important Findings from Medical Database Research. Herceptin and breast cancer: Data were collected from a cohort of more than 9,000 breast cancer patients whose tumor specimens were consecutively received at the University (more...)
Advances in health information technology are enabling a transformation in health research that could facilitate studies that were not feasible in the past, and thus lead to new insights regarding health and disease. As noted by the National Committee on Vital and Health Statistics, “Clinically rich information is now more readily available, in a more structured format, and able to be electronically exchanged throughout the health and health care continuum. As a result, the information can be better used for quality improvement, public health, and research, and can significantly contribute to improvements in health and health care for individuals and populations” ( NCVHS, 2007a ). The informatics grid recently developed with support from the National Cancer Institute (Cancer Biomedical Informatics Grid, or caBIG) is an example of a how information technologies can facilitate health research by enabling broader sharing of health data while still ensuring regulatory compliance and protecting patient privacy ( Box 3-2 ).
caBIG (Cancer Biomedical Informatics Grid). The National Cancer Institute’s caBIG Data Sharing and Intellectual Capital Workspace’s mission is to enable all constituencies in the cancer community—including researchers, physicians, (more...)
Science today is also changing rapidly and becoming more complex, so no single researcher or single site can bring all the expertise to develop and validate medical innovations or to ensure their safety. Thus, efficient sharing of information between institutions has become even more important than in previous eras, when there were fewer new therapies introduced. The expansion of treatment options, as well as the escalating expense of new therapies, mandates greater scrutiny of true effectiveness, 5 once efficacy has been demonstrated. This requires registries of patient characteristics, outcomes, and adverse events. Large populations are required to facilitate comparison of patient populations and to calculate risk/benefit estimates. For example, INTERMACS 6 (Interagency Registry for Mechanically Assisted Circulatory Support) is a national registry for patients who are receiving mechanical circulatory support device therapy to treat advanced heart failure. This registry was devised as a joint effort of the National Heart, Lung and Blood Institute, Centers for Medicare & Medicaid Services, FDA, clinicians, scientists and industry representatives. Analysis of the data collected is expected to facilitate improved patient evaluation and management while aiding in better device development. Registry results are also expected to influence future research and facilitate appropriate regulation and reimbursement of such devices. Similarly, the Extracorporeal Life Support Organization (ELSO), 7 an international consortium of health care professionals and scientists who focus on the development and evaluation of novel therapies for support of failing organ systems, maintains a registry of extracorporeal membrane oxygenation and other novel forms of organ system support. Registry data are used to support clinical practice and research, as well as regulatory agencies. Another example is the database developed by the United Network for Organ Sharing (UNOS) for the collection, storage, analysis and publication of data pertaining to the patient waiting list, organ matching, and transplants. 8 Launched in 1999, this secure Internet-based system contains data regarding every organ donation and transplant event occurring in the United States since 1986.
Information-based research, such as research using health information databases has many advantages (reviewed by Lowrance, 2002 ). It is often faster and less expensive than experimental studies; it can analyze very large sets of data and may detect unexpected phenomena or differences among subpopulations that might not be included in a controlled experimental study; it can often be undertaken when controlled trials are simply not possible for ethical, technical, or other reasons, and it can be used to study effectiveness of a specific test or intervention in clinical practice, rather than just the efficacy as determined by a controlled experimental study. It can also reexamine data accrued in other research studies, such as clinical trials, to answer new questions quickly and inexpensively. However, information-based research does have limitations. Often it has less statistical rigor than controlled clinical studies because it lacks scientific control over the original data collection, quality, and format that prospective experimental research can dictate from the start. In addition to these scientific limitations, because of its relational and often distant physical separation from the data subjects, and the sheer volume of the records involved, obtaining individual consent for the research can be difficult or impossible.
Advances in information-based medical research could also facilitate the movement toward personalized medicine, which will make health research more meaningful to individuals. The goal of personalized medicine is to tailor prevention strategies and treatments to each individual based on his/her genetic composition and health history. In spite of the strides made in improving health through new treatments, it is widely known that most drugs are effective in only a fraction of patients who have the condition for which the drug is indicated. Moreover, a small percentage of patients are likely to have adverse reactions to drugs that are found to be safe for the majority of the population at the recommended dose. Both of these phenomena are due to variability in the patient population. Revolutionary advances in the study of genetics and other markers of health and disease are now making it possible to identify and study these variations, and are leading to more personalized approaches to health care—that is, the ability to give “the appropriate drug, at the appropriate dose, to the appropriate patient, at the appropriate time.” Achieving the goals of personalized medicine will lead to improvements in both the effectiveness and the safety of medical therapies.
Public Perceptions of Health Research
A number of studies have been undertaken to gauge the public’s attitude toward research and the factors that influence individuals’ willingness to participate in research. The surveys reviewed in this chapter focus on interventional clinical trials. A review of survey questions to gauge the public willingness to allow their medical records to be used in research can be found in Chapter 2 .
The Public Values Health Research
A number of studies suggest that most Americans have a positive view of medical research and believe that research is beneficial to society. A recent Harris poll found that nearly 80 percent of respondents were interested in health research findings, consistent with previous survey results ( Westin, 2007 ). A study in 2005 compiled data from 70 state surveys and 18 national surveys and found that the majority of Americans believe maintaining world leadership in health-related research is important. Seventy-eight percent of respondents said that it is very important, and 17 percent said that it is somewhat important. Only 4 percent of Americans reported that maintaining world leadership in health-related research is not impor tant ( Woolley and Propst, 2005 ). Similar results were found in a 2007 survey—76 percent of respondents reported that science plays a very important role in our health, and 78 percent reported that science plays a very important role in our competitiveness ( Research!America, 2007 ).
The Virginia Commonwealth University 2004 Life Sciences Survey also found that most Americans have a positive view of research. In this study, 90 percent of respondents agreed that developments in science have made society better; 92 percent reported that “scientific research is essential for improving the quality of human lives”; and 84 percent agreed that “the benefits of scientific research outweigh the harmful results” ( NSF, 2006 ).
Overall Experience When Participating in Research
Little is known about the attitudes of individuals who have actually participated in medical research. However, the available evidence suggests that most research participants have positive experiences. A recent Harris Poll found that 13 percent of respondents had participated in some form of health research, and 87 percent of those felt comfortable about their experience ( Westin, 2007 ). In a study focused on cancer, 93 percent of respondents who participated in research reported it as a very positive experience; 76 percent said they would recommend participation in a clinical trial to someone with cancer. Most physicians surveyed in this study stated that they believe clinical trial participants receive the best possible care, and have outcomes at least as good as patients receiving standard cancer treatment ( Comis et al., 2000 ). Another study found that 55 percent of individuals who participated in a research study would be willing to participate again in a future research study ( Trauth et al., 2000 ).
Willingness to Participate in Research
Public opinion surveys indicate that a majority of Americans are willing to participate in clinical research studies. In 2001, a compilation of studies commissioned by Research !America found that 63 percent of Americans would be willing to participate in a clinical research study ( Woolley and Propst, 2005 ). This percentage has remained stable over time. A 2007 Research!America survey also found that 63 percent of Americans would be very likely to participate in a clinical research study if asked ( Research!America, 2007 ); 68 percent of respondents reported that their desire to improve their own health or the health of others was a major factor in deciding whether to participate in a clinical research project ( Research!America, 2007 ).
Other surveys also suggest that willingness to participate in research focused on specific diseases is quite high. In one survey, the percentage of respondents indicating a willingness to participate in a medical research study was 88 percent for cancer, 86 percent for heart disease, 83 percent for a noncurable fatal disease, 79 percent for addiction, 78 percent for depression, and 76 percent for schizophrenia ( Trauth et al., 2000 ). Respondents with greater knowledge of how research is conducted were more willing to participate ( Trauth et al., 2000 ). Another study found that 8 of 10 Americans would consider participating in a clinical trial if faced with cancer. More than two-thirds of respondents said they would be willing to participate in a clinical trial designed to prevent cancer ( Comis et al., 2000 ).
Americans also seem to be very supportive of medical research that relies on genetic data. A 2007 survey found that 93 percent of Americans supported the use of genetic testing if the information collected is used by researchers to find new ways to diagnose, prevent, or treat disease ( Genetics & Public Policy Center, 2007 ). Two separate surveys found that 66 percent of Americans would be willing to donate their genetic material for medical research ( Genetics & Public Policy Center, 2007 ; Research!America, 2007 ). However, despite this apparent positive view of genetic research, 92 percent of Americans reported they were concerned about their genetic information being used in a “harmful way” ( Genetics & Public Policy Center, 2007 ).
Many factors, in addition to concerns about privacy and confidentiality ( Genetics & Public Policy Center, 2007 ; Research!America, 2007 ), may influence an individual’s willingness to participate in a medical research study. The Trauth survey found that individuals with higher income levels, with a college or graduate degree, or with children were more likely to participate in research. Age affected willingness to participate: 57 percent of respondents ages 18–34 were willing to participate in research, but only 31 percent of respondents ages 65 or older were willing ( Trauth et al., 2000 ).
Other factors that potentially influence an individual’s willingness to participate in research are race and ethnicity. It is well documented that minorities participate in health research at a much lower percentage than white Americans. Many cultural, linguistic, and socioeconomic barriers could be responsible for this difference ( Giuliano et al., 2000 ), and study results have been variable on this issue. Several studies suggest that the low participation rates by racial and ethnic minority groups are due to their strong distrust of the medical research community compared to the general population ( Braunstein et al., 2008 ; Corbie-Smith et al., 1999 ; Farmer et al., 2007 ; Grady et al., 2006 ; Shavers et al., 2002 ).
However, other evidence suggests that the low percentage of minorities participating in research is related to minority groups’ lack of access to the research community ( Brown et al., 2000 ; Wendler et al., 2006 ; Williams and Corbie-Smith, 2006 ). Thus, it is likely that the low number of minority individuals participating in medical research is at least partly due to recruitment techniques that are ineffective for minority populations.
The survey that focused on cancer research suggests that one of the main reasons why individuals do not participate in research is lack of knowledge about the availability of clinical trials. In a survey of nearly 6,000 cancer patients, 85 percent said they were unaware of the opportunity to participate in a clinical trial. Respondents who did participate said they did so because of one of the following beliefs: (1) trials provide access to the best quality of care (76 percent), (2) their participation would benefit future cancer patients (72 percent), (3) they would receive newer and better treatment (63 percent), and (4) participation would get them more care and attention (40 percent) ( Comis et al., 2000 ).
A recommendation from a physician can also impact participation. In the United States, 48 percent of respondents to one survey reported that a physicians’ recommendation would be a major factor in deciding whether to take part in a research study. Nearly three-fourths of respondents also cited an institution’s reputation as a key factor to consider when deciding whether to participate in a study ( Research!America, 2007 ). Twenty percent of respondents in an Italian public survey indicated that the presence of a physician as a reference during a research study influenced their willingness to participate ( Mosconi et al., 2005 ).
In sum, surveys indicate that the vast majority of Americans have a positive view of medical research, believe that research is beneficial to society, and are interested in health research findings. Although little is known about the attitudes of individuals who have actually participated in medical research, the available evidence suggests that most research participants have positive experiences. Surveys also suggest that a majority of Americans are willing to participate in clinical research studies. Similar to the findings in Chapter 2 , surveys indicate that many factors, in addition to concerns about privacy and confidentiality, can potentially influence an individual’s willingness to participate in medical research, including the type of research and personal characteristics such as health status, age, education, and race. Notably, respondents with greater knowledge of how research is conducted were more willing to participate in research.
- OVERSIGHT OF HEALTH RESEARCH
Historical Development of Federal Protections of Health Information in Research
The development of international codes, federal legislation, and federal regulation of human subjects often occurred in response to past abuses in biomedical experiments (reviewed by Pritts, 2008 ) ( Box 3-3 ). The most well-known examples included (1) reported abuses of concentration camp prisoners in Nazi experiments during World War II, and (2) the Tuskegee syphilis study begun in 1932, in which researchers withheld effective treatment from affected African American men long after a cure for syphilis was found. Most of the current principles and standards for conducting human subjects research were developed primarily to protect against the physical and mental harms that can result from these types of biomedical experiments. Therefore, they focus on the principles of autonomy and consent. Although the standards apply to research that uses identifiable health information, research based solely on information is not their primary focus.
The Basis for Human Subjects Protections in Biomedical Research. Nuremberg Code The Nuremberg Code, created by the international community after the Nazi War Crimes Trials, is generally seen as the first codification (more...)
In the United States, perhaps the most influential inquiry into the protection of human subjects in research was the Belmont Report. The Belmont principles have been elaborated on in many settings, and served as the basis for formal regulation of human subjects research in the United States. In general, states do not directly regulate the activity of most researchers ( Burris et al., 2003 ). However, the Belmont Commission’s recommendations were reflected in the Department of Health and Human Services’ (HHS’s) Policy for Protection of Human Subjects Research , Subpart A of 45 C.F.R. 46 (“Subpart A”) in 1979. 9 These protections were considered a benchmark policy for federal agencies, and in December 1981, the President’s Commission for the Study of Ethical Problems in Medicine and Biomedical and Behavioral Research recommended 10 that all federal departments and agencies adopt the HHS regulations. 11
In 1982, the President’s Office of Science and Technology Policy appointed a Committee for the Protection of Human Research Subjects to respond to the recommendations of the President’s commission. The committee agreed that uniformity of federal regulations on human subjects protection is desirable to eliminate unnecessary regulations and to promote increased understanding by institutions that conduct federally supported or regulated research. As a result, in 1991, other federal departments and agencies joined HHS in adopting a uniform set of rules for the protection of human subjects of research, identical to Subpart A of 45 C.F.R. 46, which is now informally known as the “ Common Rule .” Eighteen federal agencies have now adopted the Common Rule as their own respective regulations.
Overview of the Common Rule
The Common Rule governs most federally funded research conducted on human beings and aims to ensure that the rights of human subjects are protected during the course of a research project. The Common Rule stresses the importance of individual autonomy and consent; requires independent review of research by an Institutional Review Board (IRB); and seeks to minimize physical and mental harm. Privacy and confidentiality protections, although not defined in a detailed and prescriptive manner, are included as important components of risk in research.
The framework for achieving the goal of protecting human subjects is based on two foundational requirements: the informed consent of the research participant and the review of proposed research by an IRB. This section describes some of the basic parameters of the Common Rule (reviewed by Pritts, 2008 ). Particular provisions that interact with the HIPAA Privacy Rule are described in more detail in Chapter 4 .
Scope of the Common Rule
In general, the Common Rule applies only to research on human subjects that is supported by the federal government. 12 As noted previously, research is defined as “a systematic investigation, including research development, testing, and evaluation, designed to develop or contribute to generalizable knowledge.” 13
Under the Common Rule , a “human subject” is defined as “a living individual about whom an investigator … conducting research obtains (1) Data through intervention or interaction with the individual, or (2) Identifiable private information.” Private information is considered to be personally identifiable if the identity of the subject is or may readily be ascertained by the investigator or associated with the information.
The Common Rule applies to most human subjects research conducted using federal funds, but its influence is broader because most institutions that accept federal funds sign an agreement (a Federalwide Assurance or FWA) with HHS to abide by the Common Rule requirements in all research, regardless of funding source. Nonetheless, some privately funded human subjects research is conducted outside the purview of federal regulation ( Goldman and Choy, 2001 ; Williams, 2005 ). Companies and other organizations may voluntarily choose to apply the Common Rule to their research projects, and many do. However, research projects in which compliance is voluntary are not subject to oversight or disciplinary action by HHS ( Goldman and Choy, 2001 ; Williams, 2005 ).
Informed Consent 14
The Common Rule requires that a researcher obtain informed consent (usually in writing) from a person before he/she can be admitted to a study ( Williams, 2005 ). Informed consent is sought through a process in which a person learns key facts about a research study, including the potential risks and benefits, so that he/she can then agree voluntarily to take part or decide against it.
The Common Rule informed consent regulations focus primarily on the elements and documentation of informed consent rather than on the process used to obtain it. As to the process, the regulations require that informed consent be sought only under circumstances that provide the prospective subject with adequate opportunity to consider whether to participate. The Common Rule requires that information pertaining to informed consent be given in language understandable to the subject, and that the consent does not imply that the subject is giving up his/her legal rights or that the investigator is released from liability for negligence during the conduct of the study. 15
The Common Rule also specifies a number of elements that must be provided when informed consent is sought. These elements include:
- an explanation of the purposes of the research,
- the expected duration of the subject’s participation,
- the potential risks and benefits of the research,
- how confidentiality will be maintained,
- the fact that participation is strictly voluntary, and
- who the subject can contact to answer questions about the study or about his/her rights as a research participant.
In certain limited circumstances, the Common Rule allows an informed consent to be for unspecified future research. For example, under the Common Rule an informed consent can be used to obtain a person’s permission to study personally identifiable information maintained in a repository for future, unspecified research purposes ( HHS, 2003 ).
For the most part, the required elements of an informed consent address all types of research, although some are more relevant to biomedical research (e.g., the consent must include a disclosure of appropriate alternative procedures or courses of treatment, if any, that might be advantageous to the subject). One required element of informed consent is particularly relevant to research involving personally identifiable health information. The Common Rule requires an informed consent to include a statement describing the extent, if any, to which confidentiality of records identifying the subject will be maintained. 16
Institutional Review Boards
Adopting the principles of the Belmont Report, the Common Rule requires that protocols for human subjects research be reviewed by an IRB ( Box 3-4 ) before research may begin. 17 The IRB must meet certain membership requirements, including having members with different expertise and at least one member who is not affiliated with the investigator’s institution. The Common Rule specifies which level of IRB review is needed for various types of research and provides criteria for the IRB to consider during the review. Although the Common Rule does not specify the procedures an IRB must follow in its review of protocols, it does require the IRB to have written procedures for how it will review protocols and document IRB decisions.
Institutional Review Boards. According to the Department of Health and Human Services (HHS) Institutional Review Board (IRB) guidebook, “the IRB is an administrative body established to protect the rights and welfare of human research subjects (more...)
The Common Rule requires that an IRB determine the following factors are satisfied to approve proposed research:
- Risks to subjects are minimized;
- Risks to subjects are reasonable in relation to anticipated benefits, if any, to subjects, and the importance of the knowledge that may reasonably be expected to result;
- The selection of subjects is equitable;
- Informed consent will be sought in accordance with the rules and will be documented;
- When appropriate, the research plan makes adequate provision for monitoring the data collected to ensure the safety of subjects; and
- When appropriate, adequate provisions are in place to protect the privacy of subjects and to maintain the confidentiality of data. 18
An IRB may waive the requirement to obtain informed consent or approve an alteration of the consent form for some minimal risk research. The IRB may also waive the requirement for signed consent in certain circumstances. 19
Anonymized Data
As noted above, the Common Rule considers use of “private identifiable information” to be human subjects research. Data are considered personally identifiable if the identity of the subject is or may be readily ascertained by the investigator or associated with the information accessed by the researcher. 20 However, the Common Rule exempts from its requirements research that involves:
[T]he collection or study of existing data, documents, records, pathological specimens, or diagnostic specimens, if these sources are publicly available or if the information is recorded by the investigator in such a manner that subjects cannot be identified, directly or through identifiers linked to the subjects. 21
Otherwise identifiable data may be deidentified or “anonymized” for purposes of the Common Rule if it is coded and certain other conditions are met ( HHS, 2004 ). Under Guidance issued by the Office for Human Research Protection, information is “coded” if identifying information (such as name or Social Security number) that would enable the investigator to readily ascertain the identity of the individual to whom the private information or specimens pertain has been replaced with a number, letter, symbol, or combination thereof (the code), and a key to decipher the code exists, enabling linkage of the identifying information to the private information or specimen.
Research involving only coded private information or specimens is not considered to involve human subjects under the Common Rule if the following conditions are met:
- The private information or specimens were not collected specifically for the currently proposed research project through an interaction or intervention with living individuals; and
- —The key to decipher the code is destroyed before the research begins;
- —The investigators and the holder of the key enter into an agreement prohibiting the release of the key to the investigators under any circumstances, until the individuals are deceased;
- —IRB-approved written policies and operating procedures for a repository or data management center prohibit the release of the key to investigators under any circumstances, until the individuals are deceased; or
- —Other legal requirements prohibit the release of the key to the investigators, until the individuals are deceased.
Under this standard, when a researcher accesses or receives data that have been coded and does not have access to the identifying key, the research is not considered human subjects research and is not subject to the Common Rule ’s requirements of informed consent or IRB review and approval of protocol.
Enforcement of the Common Rule
The Common Rule requirements for informed consent do not preempt any applicable federal, state, or local laws that require additional information to be disclosed to a subject in order for informed consent to be legally effective. 22
Federal funding can be suspended or withdrawn from an institution when it is found to be in material violation of the Common Rule . 23 There is no authority to impose penalties directly on individual researchers for violations. Neither does the Common Rule expressly provide a research participant with a private right of action. It should be noted, however, that recent cases indicate that courts may be willing to hold an institution liable under common law negligence theories where the approved informed consent form is determined to be less than adequate ( Shaul et al., 2005 ). 24
FDA Protection of Human Research Subjects
Some health research is also subject to FDA regulations. The FDA is charged by statute with ensuring the protection of the rights, safety, and welfare of human subjects who participate in clinical investigations 25 involving articles subject to the Federal Food, Drug, and Cosmetic Act 26 (the Act), as well as clinical investigations that support applications for research or marketing permits for products regulated by the FDA, including drugs, medical devices, and biological products for human use ( Box 3-5 ).
FDA Protection of Human Subjects Regulations. The Food and Drug Administration (FDA) Protection of Human Subjects Regulations aim to protect the rights of human subjects enrolled in research involving products that the FDA regulates (i.e., drugs, medical (more...)
In January 1981, the FDA adopted regulations governing informed consent of human subjects 27 and regulations establishing standards for the composition, operation, and responsibilities of IRBs that review clinical investigations involving human subjects. 28 At the same time, HHS adopted the Common Rule regulations on the protection of human research subjects. 29 The FDA’s regulations were harmonized with the Common Rule in 1991 to the extent permitted by statute. Key differences between FDA and HHS regulations include that the FDA does not allow for waiver or alteration of informed consent and requires that subjects be informed that the FDA may inspect their medical records. In addition, studies of efficacy based solely on medical records research are not permitted to support registration. Remaining differences in the rules are due to differences in the statutory scope or requirements ( Lee, 2000 ).
- DISTINGUISHING HEALTH RESEARCH FROM PRACTICE
The Common Rule and Privacy Rule make a somewhat artificial distinction between health research and some closely related health care practices, such as public health practice, quality improvement activities, program evaluations, 30 and utilization reviews, 31 all of which may involve collection and analysis of personally identifiable health information. However, determining which activities meet the definition of “research” is a major challenge for IRBs, Privacy Boards , 32 investigators, and health care practitioners because neither the regulations nor their interpretations by HHS provide clear guidance on how to distinguish research from activities that use similar techniques to analyze health information ( IOM, 2000a ).
It is important for IRBs and Privacy Boards to correctly distinguish among activities that are or are not subject to the various provisions of the Privacy Rule and the Common Rule . Only research requires formal IRB or Privacy Board review and informed consent. 33 Inappropriate classification of an activity as research can make it difficult or impossible for important health care activities, such as public health practice and quality improvement, to be undertaken. On the other hand, failure to correctly identify an activity as research could potentially allow improper disclosure of personally identifiable health information without sufficient oversight.
Thus, standard criteria are urgently needed for IRBs and Privacy Boards to use when making distinctions between health research and related activities, and the committee recommends that HHS consult with relevant stake holders to develop such standard criteria. HHS is aware of this need, and created a working document titled “What Is Research ?” However, the work on this project apparently has been delayed for unknown reasons ( NCURA, 2007 ). 34 As described below, a number of other models have already been proposed to help determine whether activities should be classified as research in the fields of public health and quality improvement, and these could be instructive for developing HHS guidance. Any criteria adopted by HHS should be regularly evaluated to ensure that they are helpful and producing the desired outcomes.
The following sections describe some ongoing efforts to develop such criteria in the fields of public health and quality improvement. The intent of the committee is not to endorse these particular models, but rather to illustrate the challenges associated with making these distinctions and establishing standard criteria.
Public Health Practice Versus Public Health Research
The Belmont Report defined health practice as “interventions designed solely to enhance the well-being of the person, patient or client, and which have reasonable expectation of success” ( CDC, 1999 ). To apply this definition to “public” health practice, the targeted beneficiary of the intervention must be expanded to include benefit to the community, rather than just a particular person. Neither the Common Rule nor the Privacy Rule provides a specific definition for public health research; rather public health research is included in the general definition of research. However, the Privacy Rule regulates public health practice differently from public health research (see Chapter 4 ).
An early model for distinguishing public health research from public health practice focused on the intent for which the activity was designed, noting that the intent of public health research is to “contribute to or generate generalizable knowledge,” while the intent of public health practice is to “conduct programs to prevent disease and injury and improve the health of communities” ( Snider and Stroup, 1997 ). The Centers for Disease Control and Prevention developed a similar method with an expanded assessment of intent. For example, the model posits that in public health research, the intended benefits of the project extend beyond the study participants, and the data collected exceed the requirements for the care of the study participants. But for public health practice, the intended benefits of the project are primarily for the participants in the activity, or for the participants’ community, and the only data collected are those needed to assess or improve a public health program or service, or the health of the participants and their community. The model also assumes that public health practice is based on well-established medical interventions and is nonexperimental ( CDC, 1999 ). However, these models both have been criticized as too subjective and too dependent on the opinion of the person conducting the activity ( Gostin, 2008 ; Hodge, 2005 ).
A new, more comprehensive model incorporating much of the previous two was recently proposed as a more objective checklist to be used by IRBs, Privacy Boards , and interested parties ( Hodge, 2005 ; Hodge and Gostin, 2004 ). The foundations for this model are specific definitions of public health research: “the collection and analysis of identifiable health data by a public health authority for the purpose of generating knowledge that will benefit those beyond the participating community who bear the risks of participation,” and public health practice: “the collection and analysis of identifiable health data by a public health authority for the purpose of protecting the health of a particular community, where the benefits and risks are primarily designed to accrue to the participating community.”
The model is based on two primary assumptions. First, the actor performing the activity in question is a governmental public health official, agent, agency, or entity at the federal, tribal, state, or local level. Second, the activity in question involves the acquisition, use, or disclosure of personally identifiable health data. The model is then divided into two stages. Stage 1 is applied to all activities, and can be used to distinguish practice from research in the easiest cases. Stage 2 is only applied to those cases that are hard to distinguish, and where Stage 1 failed to lead to a definitive IRB/ Privacy Board decision ( Box 3-6 ).
A Model for Distinguishing Public Health Practice from Research. Stage 1 Public health practice:
Quality Improvement Versus Health Research
Quality improvement has been defined as “systematic, data-guided activities designed to bring about immediate, positive change in the delivery of health care in a particular setting” ( Baily, 2008 ). Quality improvement activities do not require IRB or Privacy Board approval under the Common Rule or the Privacy Rule, which classify quality improvement as a component of health care operations. 35
However, in many cases, it is difficult for health care providers, IRBs, and Privacy Boards to determine whether a particular activity is purely for quality improvement, or whether it also entails research. One survey 36 exploring opinions in the health care community about the need for IRBs to review various quality-related activities found that physicians conducting quality improvement were less likely than IRB chairs to believe that IRB review was required for a given hypothetical activity, or that informed consent was necessary ( Lindenauer et al., 2002 ). Recently, a highly publicized case has again brought the issue to the forefront for all the stakeholders ( Box 3-7 ).
A Case Study of Quality Improvement and Research. Peter Pronovost of Johns Hopkins University (JHU) led a quality improvement effort at 103 intensive care units (ICUs) in Michigan hospitals to reduce the number of catheter-related bloodstream infections. (more...)
Some members of the health care community have proposed requiring that all prospective quality improvement activities go through external review ( Bellin and Dubler, 2001 ), while others have outlined specific criteria to differentiate quality improvement activities from research.
For example, Casarett and colleagues developed a two-part test to identify quality improvement activities. The first test is whether the majority of patients are expected to benefit directly from “the knowledge to be gained” from the initiative. This means that the patients must actually benefit from the knowledge learned during the evaluation, not just from being a recipient of the protocol itself. If the patients are generally expected to directly benefit from the knowledge gained during the activity, then the activity is quality improvement. If not, the activity is research. The second test is whether the participants would be subjected to additional risks or burdens, including the risk of privacy breach, beyond the usual clinical practice in order to make the results of the initiative generalizable. If yes, then the initiative should be reviewed as research ( Casarett et al., 2000 ).
More recently, the Hastings Center published a report exploring the similarities and differences between research and quality improvement. The report emphasized three fundamental characteristics of quality improvement and three fundamental characteristics of research. The authors argue that individuals have a responsibility to participate in the quality improvement activities because all patients have an interest in receiving high-quality medical care, and the success of a quality improvement activity depends on the cooperation of all patients. In addition, the report notes that quality improvement activities are a low risk to the patient, so there is little justification for not participating. The report also assumes that quality improvement activities are based on existing knowledge about human health and should lead to immediate local improvements in the provision of medical care.
In contrast, the report notes that participation in research should be voluntary, and decisions to participate should be based on researchers’ full disclosure of all the potential risks and benefits. In addition, the authors assert that research is designed to create new knowledge about human health, rather than relying solely on existing knowledge, and that most research does not result in any direct benefit to the institution where the research is being conducted.
The authors concluded that IRBs are not the appropriate body for the ethical oversight of quality improvement activities. They argue that IRBs unnecessarily impose high transaction costs on these activities because of the difference in the way they are conducted compared to research. For example, in research, any changes in methodology require further IRB approval. In contrast, quality improvement activities involve frequent adjustments in the intervention, measurement, and goals of the activity based on the experience of the investigators. Requiring the investigator to revisit an IRB every time a small adjustment is needed in such an activity significantly increases the amount of time and effort required to conduct the initiative and to produce meaningful data. Also, the investigators involved in quality improvement activities ordinarily are already involved in the clinical care of participants and bear responsibility for the quality and safety of an intervention. Thus, the authors argue that there is no need for the additional oversight by an IRB to protect participant safety.
Rather, the report recommended integrating the ethical oversight of quality improvement activities into the ongoing management of an institution’s health care delivery system, suggesting that oversight of quality improvement could be left with the managers of clinical care organizations, and that consent to receive treatment should include consent to participate in any quality improvement project that is minimal risk. However, the report stated that if a project has the characteristics of both quality improvement and research, the project should be reviewed as both human subjects research and quality improvement ( Baily et al., 2006 ; Lynn et al., 2007 ).
In response to the ongoing confusion over when quality improvement rises to the level of research and requires IRB review, the IOM jointly hosted a meeting with the American Board of Internal Medicine in May 2008 to discuss this issue. Key members of the quality improvement community attended, and short- and long-term solutions to this problem were proposed. However, no written report from this meeting was produced and no general consensus was reached.
- THE IMPORTANCE OF EFFECTIVE COMMUNICATION WITH THE PUBLIC
As noted previously in this chapter, surveys indicate that the vast majority of Americans believe that health research is important and are interested in the findings of research studies. The majority of patients also appear to be willing to participate in health research, either by volunteering for a study to test a medical intervention or by allowing access to their medical records or stored biospecimens, under certain conditions. Their willingness to participate depends on trust in researchers to safeguard the rights and well-being of patients, including assurance of privacy and confidentiality, and the belief that it is a worthwhile endeavor that warrants their involvement. Yet patients often lack information about how research is conducted, and are rarely informed about research results that may have a direct impact on their health. The committee’s recommendations in this section are intended to address both the public’s desire for more information about health research and to help fulfill two of the committees overarching goals of the report: (1) improving the privacy and security of health information, and (2) improving the effectiveness of health research.
Disseminating Health Research Results
Ethicists have long suggested greater community involvement in health research studies, including more communication about research results (reviewed by Shalowitz and Miller, 2008a , b ). In addition, the IOM committee identified transparency—the responsibility to disclose clearly how and why personally identifiable information is being collected—as an important component of comprehensive privacy protections. A previous IOM report also recommended improved communication with the public and research participants to ensure that the protection process is open and accessible to all interested parties ( IOM, 2002 ). Effective communication would build the public’s trust of the research community and is consistent with the principles of fair information practices.
When patients consent to the use of their medical records in a particular study, health researchers should make greater efforts at the conclusion of the study to inform study participants about the results, and the relevance and importance of those results. Learning about clinically relevant findings from a study in which a patient has participated could make patients feel more integrated into the process and could encourage more to participate in future studies. A recent United Kingdom report on the use of personal data in health research concluded that public involvement in research is necessary for the success of information-based research, and that a public informed about the value of research is likely to have greater enthusiasm and confidence in research and the research community ( AMS, 2006 ). Moreover, direct feedback with study participants could lead to improved health care for the individuals if the results indicate that an altered course of care is warranted.
Nonetheless, there are multiple impediments, beyond cost, to providing meaningful feedback to participants. A summary of the results alone, while necessary and reasonable, can be seen as a token, and also raises questions about issues such as how best to write summaries, the stage at which results should be disseminated, and how to present research with uninformative outcomes. For example, one recent study found that sharing results directly with study participants was met with overwhelmingly favorable reactions from patients, but the study also revealed some obstacles ( Partridge et al., 2008 ). In a survey of women who had participated in a randomized trial of breast cancer therapy and had received a summary of the study results by mail, 95 percent reported that they were glad they received the results. Most respondents interpreted the results correctly, although incorrect interpretation of the results was associated with increased anxiety, as was dissatisfaction with treatment.
Although some guidelines for providing and explaining study results to research participants have been proposed, they differ in details because limited data are available on this subject, and thus standards are lacking ( Partridge and Winer, 2002 ; Partridge et al., 2008 ; Shalowitz and Miller, 2008b ; Zarin and Tse, 2008 ). Because transparency is best achieved by providing graded levels of information and guidance to interested parties ( IOM, 2002 ), it will be important to develop effective and efficient ways to communicate with various sectors of the population. A commitment to the principles of “plain language” 37 will be important. Broader adoption of electronic medical records may also be helpful in accomplishing this goal.
Research Registries
One way to make information about research studies more broadly available to the public is through registration of trials and other studies in public databases. HHS should encourage such registration of trials and other studies, particularly when research is conducted with an IRB/ Privacy Board approved waiver of consent or authorization (see Chapter 4 ). Numerous clinical trial registries already exist, and registration has increased in recent years (reviewed by Zarin and Tse, 2008 ). In 2000, the National Library of Medicine established a clinical trials registry ( ClinicalTrials.gov ), which has expanded to include information from several other trial registries and to serve as the FDA-required site for submissions about clinical trials subject to the FDA databank requirement. The FDA Amendments Act of 2007 38 expanded the scope of required registrations at ClinicalTrials.gov and provided the first federally funded trials results database. It mandates registrations of controlled clinical investigations, except for Phase I trials, of drugs, biologics, and devices subject to FDA regulation.
A policy of the International Committee of Medical Journal Editors (ICMJE), adopted in fall 2005, also requires prospective trial registration as a precondition for publication ( DeAngelis et al., 2004 ). This policy led to a 73 percent increase in trial registrations of all intervention types from around the world ( Zarin et al., 2005 ). Nearly 45,000 trials had been registered by fall 2007.
However, although the development of such registries is an important first step toward providing high-quality clinical trial information to the public, no centralized system currently exists to disseminate information about clinical trials of drugs or other interventions, making it difficult for consumers and their health care providers to identify ongoing studies. The current statutory requirements for registration and data reporting in the United States are not as broad as the transnational policies of the ICMJE or the World Health Organization, which call for the registration of all interventional studies in human beings regardless of intervention type ( Laine et al., 2007 ; Sim et al., 2006 ). Moreover, noninterventional studies, such as observational studies that play an increasingly critical role in biomedical research, are not generally included in these databases. Because many noninterventional studies are conducted with an IRB/ Privacy Board approved waiver of consent or authorization, including those studies in a registry could be an important method for increasing public knowledge of such studies.
Informing the Public About the Methods and Value of Research
As noted previously, clinical trials are the most visible of the various types of health research, but a great deal of information-based health research entails analysis of thousands of patient records to better understand human diseases, to determine treatment effectiveness, and to identify adverse side effects of therapies. This form of research is likely to increase in frequency as the availability of electronic records continues to expand. As we move toward the goal of personalized medicine, research results will be even more likely to be directly relevant to patients, but more study subjects will be necessary to derive meaningful results.
However, many patients probably are not aware that their medical records are being used in information-based research. For example, the recent study that used focus groups to examine the views of veterans toward the use of medical records in research found that the majority of participants (75 percent) were not aware that “under some circumstances, [their] medical records could be used in some research studies without [their] permission,” despite the fact that a notice of privacy practices, which included a statement that such research could occur, had been mailed to all participants less than a year prior to the study ( Damschroder et al., 2007 ).
Moreover, surveys show that many patients desire not only notice, but also the opportunity to decide whether to consent to such research with medical records. Those surveys further indicate that patients who wish to be asked for consent for each study are most concerned about the potentially detrimental affects of inappropriate disclosure of their personally identifiable health information, including discrimination in obtaining health or life insurance or employment.
As noted in Chapter 2 , strengthening security protections of health data should reduce the risk of security breaches and their potential negative consequences, and thus should help to alleviate patient concerns in this regard. But educating patients about how health research is conducted, monitored, and reported on could also help to ease patient concerns about privacy and increase patients’ trust in the research community, which as noted above is important for the public’s continued participation in health research. For example, datasets are most often provided to researchers without direct identifiers such as name and Social Security number. Furthermore, identifiers are not included in publications about research results. Also, under both the Privacy Rule and the Common Rule , a waiver of consent and authorization is possible only under the supervision of an IRB or Privacy Board , and a waiver is granted only when the research entails minimal risk and when obtaining individual consent and authorization is impracticable (see the previous section and also Chapter 4 ). Finally, professional ethics dictate that researchers safeguard data and respect privacy.
Conveying the value of medical records research to patients will be important. Surveys show that people are more supportive of research that is relevant to them and their loved ones. At the same time, educational efforts should stress the negative impact of incomplete datasets on research findings. Representative samples are essential to ensure the validity and generalizability of health research ( Box 3-8 ), but datasets will not represent the entire population if some people withhold access to their health information.
Selection Bias in Health Research. When researchers are required to obtain consent or authorization to access each individual’s medical record for a research study, it is likely that individuals’ willingness to grant access will not be (more...)
In addition, an educated public could also decrease the potential for biased research samples. A universal requirement for consent or authorization in medical records research leads to incomplete datasets, and thus to biased results and inaccurate conclusions. Some large medical institutions with a strong research history and reputation (e.g., Mayo Clinic) can obtain authorization and consent rates as high as 80 percent, but the 20 percent who refuse have distinct demographic and health characteristics. In fact, even a refusal rate of less than 5 percent can create selection bias in the data ( Jacobsen et al., 1999 ; see Chapter 5 for more detail). Conveying to the public the importance of health care improvements derived from medical records research and stressing the negative impact of incomplete datasets on research findings may increase the public’s participation in research and their willingness to support information-based research that is conducted with IRB or Privacy Board oversight, under a waiver of patient consent or authorization.
Numerous examples of important research findings from medical records research would not have been possible if direct patient consent and authorization were always required ( Box 3-1 ). For example, analysis of medical records showed that infants exposed to diethylstilbesterol (DES) during the first trimester of pregnancy had an increased risk of breast, vaginal, and cervical cancer as well as reproductive anomalies as adults. Similarly, studies of medical records led to the discovery that folic acid supplementation during pregnancy can prevent neural tube defects.
Thus, HHS and the health research community should work to edu cate the public about how research is done and the value it provides. All stakeholders, including professional organizations, nonprofit funders, and patient organizations, have different interests and responsibilities to make sure that their constituencies are well informed. For example, the American Society of Clinical Oncology and the American Heart Association already have some online resources to help patients gather information about research that may be relevant to their conditions. But coordination and identification of best practices by HHS would be helpful, and research is needed to identify which segments of the population would be receptive to and benefit from various types of information about how research is done and its value in order to create and implement an effective plan.
Greater use of community-based participatory research, in which community-based organizations or groups bring community members into the research process as partners to help design studies and disseminate the knowledge gained, 39 could help achieve this goal. These groups help researchers to recruit research participants by using the knowledge of the community to understand health problems and to design activities that the community is likely to value. They also inform community members about how the research is done and what comes out of it, with the goal of providing immediate community benefits from the results when possible.
- CONCLUSIONS AND RECOMMENDATIONS
Based on its review of the information described in this chapter, the committee agreed on a second overarching principle to guide the formation of recommendations. The committee affirms the importance of maintaining and improving health research effectiveness. Research discoveries are central to achieving the goal of extending the quality of healthy lives. Research into causes of disease, methods for prevention, techniques for diagnosis, and new approaches to treatment has increased life expectancy, reduced infant mortality, limited the toll of infectious diseases, and improved outcomes for patients with heart disease, cancer, diabetes, and other chronic diseases. Patient-oriented clinical research that tests new ideas makes rapid medical progress possible. Today, the rate of discovery is accelerating, and we are at the precipice of a remarkable period of investigative promise made possible by new knowledge about the genetic underpinnings of disease. Genomic research is opening new possibilities for preventing illness and for developing safer, more effective medical care that may eventually be tailored for specific individuals. Further advances in relating genetic information to predispositions to disease and responses to treatments will require the use of large amounts of existing health-related information and stored tissue specimens. The increasing use of electronic medical records will further facilitate the generation of new knowledge through research and accelerate the pace of discovery. These efforts will require broad participation of patients in research and broad data sharing to ensure that the results are valid and applicable to different segments of the population. Collaborative partnerships among communities of patients, their physicians, and teams of researchers to gain new scientific knowledge will bring tangible benefits for people in this country and around the world.
Surveys indicate that the majority of Americans believe that health research is important, are interested in the findings of research studies, and are willing to participate in health research. But patients often lack information about how research is conducted and are rarely informed about research results that may have a direct impact on their health. Effective communication could build the public’s trust of the research community, which is important because trust is necessary for the public’s continued participation in research. Moreover, direct feedback could lead to improved health care for study participants if the results indicate that an altered course of care is warranted.
Thus, the committee recommends that when patients consent to the use of their medical records in a particular study, health researchers should make greater efforts when the study ends to inform study participants about the results, and the relevance and importance of those results. Broader adoption of electronic health records may be helpful in accomplishing this goal, but standards and guidelines for providing and explaining study results to research participants or various sectors of the public are needed.
HHS should also encourage registration of trials and other studies in public databases, particularly when research is conducted with an IRB/ Privacy Board approved waiver of consent or authorization, as a way to make information about research studies more broadly available to the public. Numerous clinical trial registries already exist, and registration has increased in recent years, but no centralized system currently exists for disseminating information about clinical trials of drugs or other interventions, making it difficult for consumers and their health care providers to identify ongoing studies. Moreover, noninterventional studies, such as observational studies that play an increasingly critical role in biomedical research, are not generally included in these databases. Because many noninterventional studies are conducted with an IRB/Privacy Board approved waiver of consent or authorization, including such studies in a registry could be an important method for increasing public knowledge of those studies.
Interventional clinical trials are the most visible of the various types of health research, but a great deal of information-based health research entails analysis of thousands of patient records to better understand human diseases, to determine treatment effectiveness, and to identify adverse side effects of therapies. This form of research is likely to increase in frequency as the availability of electronic health records continues to expand. As we move toward the goal of personalized medicine, research results will be even more likely to be directly relevant to patients, but more study participants will be necessary to derive meaningful results.
However, many patients are likely not aware that their medical records are being used in information-based research, and surveys show that many patients desire not only notice, but also the opportunity to decide about whether to consent to such research with medical records. As noted in Chapter 2 , strengthening security protections of health data should reduce the risk of security breaches and their potential negative consequences, and thus should help to alleviate patient concerns in this regard. But educating patients about how health research is conducted, monitored, and reported could also increase patients’ trust in the research community. Thus, HHS and the health research community should work to educate the public about how research is done.
It will also be important for HHS and researchers to convey the value of health care improvements derived from medical records research, and to stress the negative impact of incomplete datasets on research findings. Representative samples are essential to ensure the validity and generalizability of health research, but datasets will not be representative of the entire population if some people withhold access to their health information. A universal requirement for consent or authorization in information-based research may lead to incomplete datasets, and thus to biased results and inaccurate conclusions. Numerous examples of important research findings from medical records research would not have been possible if direct patient consent and authorization were always required.
To ensure that beneficial health research and related activities continue to be undertaken with appropriate oversight under federal regulations, it will be important for HHS to also provide more guidance on how to distinguish the various activities. The Privacy Rule makes a distinction between health research and some closely related endeavors, such as public health and quality improvement activities, which also may involve collection and analysis of personally identifiable health information. Under the Privacy Rule (as well as the Common Rule ), these activities, which aim to protect the public’s health and improve the quality of patient care, are considered health care “practice” rather than health research. Therefore, they can be undertaken without consent or authorization, or an IRB/ Privacy Board waiver of consent or authorization. However, it can be a challenge for IRBs and Privacy Boards to distinguish among activities that are or are not subject to the various provisions of the Privacy Rule and the Common Rule, and inappropriate decisions may prevent important activities from being undertaken or could potentially allow improper disclosure of personally identifiable health information.
To address these difficulties, a number of models have been proposed that outline the criteria IRBs and Privacy Boards should use to distinguish practice and research. For example, one recent model provides a detailed checklist for IRBs and Privacy Boards to use in determining whether an activity is public health research and required to comply with the research provisions of the Privacy Rule, or public health practice that does not need IRB/Privacy Board review. The committee believes that standardizing the criteria is essential to support the conduct of these important health care activities.
Thus, HHS should convene the relevant stakeholders to develop standard criteria for IRBs and Privacy Boards to use when making decisions about whether protocols entail research or practice. There should be flexibility in the regulation to allow important activities to go forward with appropriate levels of oversight. Also, it will be important to evaluate whether these criteria are effective in aiding IRB/Privacy Board reviews of proposed protocols, and whether they lead to appropriate IRB/Privacy Board decisions.
These changes suggested above could be accomplished without any changes to HIPAA by making them a condition of funding from HHS and other research sponsors and by providing some additional funds to cover the cost.
- AMS (Academy of Medical Sciences). Personal data for public good: Using health information in medical research. 2006. [accessed August 28, 2008]. http://www .acmedsci.ac .uk/images/project/Personal.pdf .
- Baily MA. Harming through protection? New England Journal of Medicine. 2008; 258 (8):768–769. [ PubMed : 18287599 ]
- Baily MA, Bottrell M, Lynn J, Jennings B. The ethics of using QI methods to improve health care quality and safety. A Hastings Center Special Report. 2006; 36 (4):S1–S40. [ PubMed : 16898359 ]
- Bates DW, Leape LL, Cullen DJ, Laird N, Petersen LA, Teich JM, Burdick E, Hickey M, Kleefield S, Shea B, Vander VM, Seger DL. Effect of computerized physician order entry and a team intervention on prevention of serious medication errors. JAMA. 1998; 280 (15):1311–1316. [ PubMed : 9794308 ]
- Bellin E, Dubler NN. The quality improvement-research divide and the need for external oversight. American Journal of Public Health. 2001; 91 (9):1512–1517. [ PMC free article : PMC1446813 ] [ PubMed : 11527790 ]
- Big Health. Big health consortium. 2008. [accessed October 29, 2008]. http://www .bighealthconsortium .org/about/
- Braunstein JB, Sherber NS, Schulman SP, Ding EL, Powe NR. Race, medical researcher distrust, perceived harm, and willingness to participate in cardiovascular prevention trials. Medicine. 2008; 87 (1):1–9. [ PubMed : 18204365 ]
- Brown DR, Fouad MN, Basen-Engquist K, Tortolero-Luna G. Recruitment and retention of minority women in cancer screening, prevention and treatment trials. Annals of Epidemiology. 2000; 10 :S13–S21. [ PubMed : 11189088 ]
- Burris S, Gable L, Stone L, Lazzarini Z. The role of state law in protecting human subjects of public health research and practice. Journal of Law, Medicine & Ethics. 2003; 31 :654. [ PubMed : 14968667 ]
- Casarett D, Karlawish J, Sugarman J. Determining when quality improvement initiatives should be considered research: Proposed criteria and potential implications. JAMA. 2000; 284 (7):2275–2280. [ PubMed : 10807388 ]
- Casarett D, Karlawish J, Andrews E, Caplan A. Bioethical issues in pharmacoepidemiological research. In: Strom BL, editor. Pharmacoepidemiology. West Sussex, England: John Wiley & Sons, Ltd.; 2005. pp. 417–432.
- CDC (Centers for Disease Control and Prevention). Guidelines for defining public health research and public health non-research. 1999. [accessed March 4, 2008]. http://www .cdc.gov/od /science/regs/hrpp/researchdefinition .htm .
- CHSR (Coalition for Health Services Research). Framework for health services research policy for 2008. 2008. [accessed August 21, 2008]. http://www .chsr.org/Policy_Priorities .pdf .
- Comis RL, Aldige CR, Stovall EL, Krebs LU, Risher PJ, Taylor HJ. A quantitative survey of public attitudes towards cancer clinical trials. Philadelphia, PA: Coalition of National Cancer Cooperative Groups, Cancer Research Foundation of America, Cancer Leadership Council, and Oncology Nursing Society; 2000.
- Corbie-Smith G, Thomas SB, Williams MV, Moody-Ayers S. Attitudes and beliefs of African Americans towards participation in medical research. Journal of General Internal Medicine. 1999; 14 :537–546. [ PMC free article : PMC1496744 ] [ PubMed : 10491242 ]
- Damschroder LJ, Pritts JL, Neblo MA, Kalarickal RJ, Creswell JW, Hayward RA. Patients, privacy and trust: Patients’ willingness to allow researchers to access their medical records. Social Science & Medicine. 2007; 64 (1):223–235. [ PubMed : 17045717 ]
- DeAngelis CD, Drazen JM, Frizelle FA, Haug C, Hoey J, Horton R, Kotzin S, Laine C, Marusic A, Overbeke AJPM, Schroeder TV, Sox HC, Van Der Weyden MB. Clinical trial registration: A statement from the International Committee of Medical Journal Editors. JAMA. 2004; 292 (11):1363–1364. [ PubMed : 15355936 ]
- Farmer D, Jackson SA, Camacho F, Hall MA. Attitudes of African American and low socioeconomic status white women toward medical research. Journal of Health Care for the Poor and Underserved. 2007; 18 :85–99. [ PubMed : 17337800 ]
- FDA (Food and Drug Administration). Certain estrogens for oral or parenteral use. Drugs for human use; drug efficacy study implementation. Federal Register. 1971; 36 (217):21537–21538.
- FDA. FDA public health advisory, deaths with antipsychotics in elderly patients with behavioral disturbances. 2005. [accessed August 18, 2008]. http://www .fda.gov/cder /drug/advisory/antipsychotics.htm .
- FDA. FDA alert [6/16/2008]: Information for healthcare professionals. Antipsychotics. 2008. [accessed August 18, 2008]. http://www .fda.gov/cder /drug/infosheets/hcp /antipsychotics_conventional.htm .
- Finkelstein EA, Fiebelkorn IC, Wang G. National medical spending attributable to overweight and obesity: How much, and who’s paying? Health Affairs Web Exclusive. 2003. [accessed August 21, 2008]. http://content .healthaffairs .org/cgi/content /abstract/hlthaff.w3.219v1 . [ PubMed : 14527256 ]
- Furrow BR, Greaney TL, Johnson SH, Jost TS, Schwartz RL. Bioethics: Health care law and ethics. St. Paul, MN: Thomson/West; 2004.
- GAO (Government Accountability Office). Scientific research: Continued vigilance critical to protecting human subjects. Washington, DC: GAO; 1996.
- Genetics & Public Policy Center. U.S. public opinion on uses of genetic information and genetic discrimination. 2007. [accessed August 21, 2008]. http://www .dnapolicy .org/resources/GINAPublic _Opinion_Genetic _Information_Discrimination.pdf .
- Gill S, Bronskill S, Normand S, Anderson G, Sykora K, Lam K, Bell C, Lee P, Fischer H, Herrmann N, Gurwitz J, Rochon P. Antipsychotic drug use and mortality in older adults with dementia. Annals of Internal Medicine. 2007; 146 :775–786. [ PubMed : 17548409 ]
- Giuliano AR, Mokuau N, Hughes C, Tortelero-Luna G, Risendal B, Ho RCS, Prewitt TE, McCaskill-Stevens WJ. Participation of minorities in cancer research: The influence of structural, cultural, and linguistic factors. Annals of Epidemiology. 2000; 10 :S22–S34. [ PubMed : 11189089 ]
- Goldman J, Choy A. Ethical and policy issues in research involving human participants. Bethesda, MD: National Bioethics Advisory Commission; 2001. Privacy and confidentiality in health research; pp. C1–C34.
- Gostin LO. Public health law: Power, duty, restraint. Berkeley, CA: University of California Press; 2008. Surveillance and public health research: Personal privacy and the “right to know.”
- Grady C, Hampson LA, Wallen GR, Rivera-Goba MV, Carrington KL, Mittleman BB. Exploring the ethics of clinical research in an urban community. American Journal of Public Health. 2006; 96 (11):1996–2001. [ PMC free article : PMC1751807 ] [ PubMed : 17018826 ]
- Hatfield M, Sonnenschein HF, Rosenberg LE. Exceptional returns: The economic value of America’s investment in medical research. 2001. [accessed August 21, 2008]. http://www .laskerfoundation .org/advocacy/pdf/exceptional.pdf .
- Herbst AL, Ulfelder H, Poskanzer DC. Adenocarcinoma of the vagina. Association of maternal stilbestrol therapy with tumor appearance in young women. New England Journal of Medicine. 1971; 284 (15):878–881. [ PubMed : 5549830 ]
- HEW (Department of Health, Education and Welfare). The Belmont Report: Ethical principles and guidelines for the protection of human subjects of research. 1979. [accessed August 21, 2008]. http://ohsr .od.nih.gov /guidelines/belmont.html . [ PubMed : 25951677 ]
- HHS (Department of Health and Human Services). Institutional review boards and the HIPAA Privacy Rule. 2003. [accessed August 21, 2008]. http: //privacyruleandresearch .nih.gov/pdf/IRB_Factsheet.pdf .
- HHS. Guidance on research involving coded private information or biological specimens. 2004. [accessed August 21, 2008]. http://www .hhs.gov/ohrp /humansubjects/guidance/cdebiol.pdf .
- Hodge JG Jr. An enhanced approach to distinguishing public health practice and human subjects research. Journal of Law, Medicine & Ethics. 2005; 33 (1):125–141. [ PubMed : 15934670 ]
- Hodge JG, Gostin LO. Public health practice vs. research: A report for public health practitioners including cases and guidance for making distinctions. Atlanta, GA: Council of State and Territorial Epidemiologists; 2004.
- IOM (Institute of Medicine). Health services research: Work force and educational issues. Washington, DC: National Academy Press; 1995.
- IOM. Protecting data privacy in health services research. Washington, DC: National Academy Press; 2000a. [ PubMed : 25057723 ]
- IOM. To err is human: Building a safer health system. Washington, DC: National Academy Press; 2000b. [ PubMed : 25077248 ]
- IOM. Responsible research: A systems approach to protecting research participants. Washington, DC: The National Academies Press; 2002. [ PubMed : 20669487 ]
- Jacobsen S, Xia Z, Campion M, Darby C, Plevak M, Seltman K, Melton L. Potential effect of authorization bias on medical record research. Mayo Clinic Proceedings. 1999; 74 :330–338. [ PubMed : 10221460 ]
- Laine C, Horton R, DeAngelis CD, Drazen JM, Frizelle FA, Godlee F, Haug C, Hébert PC, Kotzin S, Marusic A, Sahni P, Schroeder TV, Sox HC, Van Der Weyden MB, Verheugt FWA. Clinical trial registration—looking back and moving ahead. New England Journal of Medicine. 2007; 356 (26):2734–2736. [ PubMed : 17548427 ]
- Lee B. Comparison of FDA and HHS human subject protection regulations. 2000. [accessed August 21, 2008]. http://www .fda.gov/oc/gcp/comparison .html .
- Lindenauer PK, Benjamin EM, Naglieri-Prescod D, Fitzgerald J, Pekow P. The role of the institutional review board in quality improvement: A survey of quality officers, institutional review board chairs, and journal editors. The American Journal of Medicine. 2002; 113 :575–579. [ PubMed : 12459404 ]
- Lowrance WW. Learning from experience, privacy and the secondary use of data in health research. London: The Nuffield Trust; 2002.
- Lowrance WW, Collins FS. Identifiability in genomic research. Science. 2007; 317 :600–602. [ PubMed : 17673640 ]
- Lynn J, Baily MA, Bottrell M, Jennings B, Levine RJ, Davidoff F, Casarett D, Corrigan J, Fox E, Wynia MK, Agich GJ, Speroff T, Schyve P, Batalden P, Tunis S, Berlinger N, Cronenwett L, Fitzmaurice M, Dubler NN, James B. The ethics of using quality improvement methods in health care. Annals of Internal Medicine. 2007; 146 (6):666–674. [ PubMed : 17438310 ]
- Mandelblatt J, Saha S, Teutsch S, Hoerger T, Siu AL, Atkins D, Klein J, Helfand M. The cost-effectiveness of screening mammography beyond age 65: A systematic review for the U.S. Preventive Services Task Force. Annals of Internal Medicine. 2003; 139 :835–842. [ PubMed : 14623621 ]
- Mick S, Morlock LL, Salkever D, de Lissovoy G, Malitz F, Wise CG, Jones A. Strategic activity and financial performance of U.S. rural hospitals: A national study, 1983 to 1988. Journal of Rural Health. 1994; 10 (3):150–167. [ PubMed : 10138031 ]
- Mosconi P, Poli P, Giolo A, Apolone G. How Italian health consumers feel about clinical research: A questionnaire survey. European Journal of Public Health. 2005; 15 (4):372–379. [ PubMed : 16014662 ]
- Murphy K, Topel R. The economic value of medical research. Chicago, IL: University of Chicago Press; 1999.
- NCI (National Cancer Institute). Getting connected with caBIG: Data sharing and security framework. 2008. [accessed October 27, 2008]. https://cabig .nci.nih .gov/working_groups /DSIC_SLWG/data_sharing_policy/
- NCURA (National Council of University Research Administrators). Report on research compliance. 2007. [accessed March 4, 2008]. http://www .reportonresearchcompliance .com .
- NCVHS (National Committee on Vital and Health Statistics). Enhanced protections for uses of health data: A stewardship framework for “secondary uses” of electronically collected and transmitted health data. 2007a. [accessed December 19, 2007]. http://ncvhs .hhs.gov/071221lt.pdf .
- NCVHS, Ad Hoc Work Group on Secondary Uses of Health Data. Testimony of the cancer Biomedical Informatics Grid (caBIG) Data Sharing and Intellectual Capital (DSIC) workspace. 2007b August 1, 2007
- Needleman J, Buerhaus P, Mattke S, Stewart M, Zelevinsky K. Nurse-staffing levels and the quality of care in hospitals. New England Journal of Medicine. 2002; 346 (22):1715–1722. [ PubMed : 12037152 ]
- NSF (National Science Foundation). Science and Engineering Indicators 2006. Arlington, VA: National Science Foundation; 2006. Science and technology: Public attitudes and understanding. Chapter 7.
- OHRP (Office for Human Research Protections). IRB guidebook, part I.A. 2008a. [accessed August 21, 2008]. http://www .hhs.gov/ohrp /irb/irb_guidebook.htm .
- OHRP. OHRP concludes case regarding Johns Hopkins University research on hospital infections. 2008b. [accessed August 21, 2008]. http://www .hhs.gov/ohrp/news/recentnews .html#20080215 .
- Partridge A, Winer E. Informing clinical trial participants about study results. JAMA. 2002; 288 :363–365. [ PubMed : 12117402 ]
- Partridge AH, Wolff AC, Marcom PK, Kaufman PA, Zhang L, Gelman R, Moore C, Lake D, Fleming GF, Rugo HS, Atkins J, Sampson E, Collyar D, Winer EP. The impact of sharing results of a randomized breast cancer clinical trial with study participants. Breast Cancer Research and Treatment. 2008 June 10 [ PubMed : 18543100 ]
- Pitkin R. Folate and neural tube defects. American Journal of Clinical Nutrition. 2007; 85 (1):285S–288S. [ PubMed : 17209211 ]
- Pritts J. The importance and value of protecting the privacy of health information: Roles of HIPAA Privacy Rule and the Common Rule in health research. 2008. [accessed March 15, 2008]. http://www .iom.edu/CMS/3740/43729/53160 .aspx .
- Research!America. America speaks: Poll summary. Vol. 7. Alexandria, VA: United Health Foundation; 2007.
- Schneeweiss S, Setoguchi S, Brookhart A, Dormuth C, Wang P. Risk of death associated with the use of conventional versus atypical antipsychotic drugs among elderly patients. Canadian Medical Association Journal. 2007; 176 :672–632. [ PMC free article : PMC1800321 ] [ PubMed : 17325327 ]
- Shalowitz DI, Miller FG. Communicating the results of clinical research to participants: Attitudes, practices, and future directions. PLoS Medicine. 2008a May 13; 5 (5):e91. [ PMC free article : PMC2375946 ] [ PubMed : 18479180 ]
- Shalowitz DI, Miller FG. The search for clarity in communicating research results to study participants. Journal of Medical Ethics. 2008b September; 34 (9):e17. [ PubMed : 18757617 ]
- Shaul RZ, Birenbaum S, Evans M. Legal liability in research: Early lessons from North America. BMC Medical Ethics. 2005; 6 (4):1–4. [ PMC free article : PMC1182131 ] [ PubMed : 15953387 ]
- Shavers VL, Lynch CF, Burmeister LF. Racial differences in factors that influence the willingness to participate in medical research studies. Annals of Epidemiology. 2002; 12 :248–256. [ PubMed : 11988413 ]
- Sim I, Chan A-W, Gülmezoglu AM, Evans T, Pang T. Clinical trial registration: Transparency is the watchword. The Lancet. 2006; 367 (9523):1631–1633. [ PubMed : 16714166 ]
- Slamon D, Clark G, Wong S, Levin W, Ullrich A, McGuire W. Human breast cancer: Correlation of relapse and survival with amplification of the her-2/neu oncogene. Science. 1987; 235 (4785):177–182. [ PubMed : 3798106 ]
- Snider DE, Stroup DF. Defining research when it comes to public health. Public Health Reports. 1997; 112 :29–32. [ PMC free article : PMC1381834 ] [ PubMed : 9018284 ]
- Thorpe KE, Florence CS, Howard DH, Joski P. The impact of obesity in rising medical spending. Health Affairs Web Exclusive. 2004. [accessed August 21, 2008]. http://content .healthaffairs .org/cgi/content /abstract/hlthaff.w4.480v1 . [ PubMed : 15496437 ]
- Trauth JM, Musa D, Siminoff L, Jewell IK, Ricci E. Public attitudes regarding willingness to participate in medical research studies. Journal of Health & Social Policy. 2000; 12 (2):23–43. [ PubMed : 11184441 ]
- Veurink M, Koster M, Berg L. The history of DES, lessons to be learned. Pharmacy World & Science. 2005; 27 (3):139–143. [ PubMed : 16096877 ]
- Wendler D, Kington R, Madans J, Van Wye G, Christ-Schmidt H, Pratt LA, Brawley OW, Gross CP, Emanuel E. Are racial and ethnic minorities less willing to participate in health research? PLoS Medicine. 2006; 3 (2):201–210. [ PMC free article : PMC1298944 ] [ PubMed : 16318411 ]
- Westin A. How the public views privacy and health research. 2007. [accessed November 11, 2008]. http://www .iom.edu/Object .File/Master/48 /528/%20Westin%20IOM %20Srvy%20Rept%2011-1107.pdf .
- Williams ED. Federal protection for human research subjects: An analysis of the Common Rule and its interactions with FDA regulations and the HIPAA Privacy Rule, CRS report for Congress. Washington, DC: Congressional Research Service; 2005.
- Williams IC, Corbie-Smith G. Investigator beliefs and reported success in recruiting minority participants. Contemporary Clinical Trials. 2006; 27 :580–586. [ PubMed : 16839822 ]
- Winston FK, Durbin DR, Kallan MJ, Moll EK. The danger of premature graduation to seat belts for young children. Pediatrics. 2000; 105 (6):1179–1183. [ PubMed : 10835054 ]
- WMA (World Medical Association). Declaration of Helsinki: Ethical principles for medical research involving human subjects. 1964. [accessed August 21, 2008]. http://ohsr .od.nih.gov /guidelines/helsinki.html . [ PubMed : 16010903 ]
- Woolley M, Propst SM. Public attitudes and perceptions about health-related research. JAMA. 2005; 294 (11):1380–1384. [ PubMed : 16174697 ]
- Zarin DA, Tse T. Moving toward transparency of clinical trials. Science. 2008; 319 :1340–1342. [ PMC free article : PMC2396952 ] [ PubMed : 18323436 ]
- Zarin DA, Tse T, Ide NC. Trial registration at ClinicalTrials.gov between May and October 2005. New England Journal of Medicine. 2005; 353 (26):2779–2787. [ PMC free article : PMC1568386 ] [ PubMed : 16382064 ]
Epidemiology is the study of the occurrence, distribution, and control of diseases in populations.
Health services research has been defined as a multidisciplinary field of inquiry, both basic and applied, that examines the use, costs, quality, accessibility, delivery, organization, financing, and outcomes of health care services to increase knowledge and understanding of the structure, processes, and effects of health services for individuals and populations ( IOM, 1995 ).
The National Committee on Vital and Health Statistics has noted that “secondary uses” of health data is an ill-defined term, and urges abandoning it in favor of precise description of each use ( NCVHS, 2007a ). Thus, the committee chose to minimize use of the term in this report.
See Standards for Privacy of Individually Identifiable Health Information , 64 Fed. Reg. 59918, 59967 (preamble to rule proposed November 3, 1999) for a discussion on the benefits of health records research.
Effectiveness can be defined as the extent to which a specific test or intervention, when used under ordinary circumstances, does what it is intended to do. Efficacy refers to the extent to which a specific test or intervention produces a beneficial result under ideal conditions (e.g., in a clinical trial).
See http://www .intermacs.org .
See http://www .elso.med.umich.edu .
See http://www .unos.org/Data .
The Department of Health, Education and Welfare (now HHS) had previously issued policy and guidance on the protection of human subjects. See Williams (2005) .
In its report “First Biennial Report on the Adequacy and Uniformity of Federal Rules and Policies, and their Implementation, for the Protection of Human Subjects in Biomedical and Behavioral Research , Protecting Human Subjects.”
45 C.F.R. part 46 (2005).
See 45 C.F.R. § 46.101 (2005).
See 45 C.F.R. § 46.102(d) (2005).
This section on informed consent is based largely on a Congressional Research Service report ( Williams, 2005 ), as adapted by Pritts (2008) .
See 45 C.F.R. § 46.116 (2005).
See 45 C.F.R. § 46.116(b) (2005).
See 45 C.F.R. § 46.103 (2005).
See 45 C.F.R. § 46.111 (2005). There are additional factors if the study includes subjects who are likely to be vulnerable to coercion or undue influence.
See 45 C.F.R. § 46.116(d); 46.117(c) (2005).
See 45 C.F.R. § 46.102(f) (2005).
See 45 C.F.R. § 46.101(b)(4) (2005).
See 45 C.F.R. § 46.116(e) (2005).
See 45 C.F.R. § 46.123 (2005).
See also Grimes v. Kennedy Krieger Institute , 782 A. 2d 807 (Md. Ct. App. 2001); Gelsinger v. University of Pennsylvania (Philadelphia County Court of Common Pleas filed September 18, 2000), available at http://www .sskrplaw.com /links/healthcare2.html .
The FDA has defined “clinical investigation” to be synonymous with “research.”
The Food, Drug, and Cosmetic Act Section 505(i), 507(d), or 520(g) of 21 U.S.C. 355(i), 357(d), or 360j(g) (1972).
See 21 C.F.R. part 50 (2008); 46 Fed. Reg. 8942 (1981).
See 21 C.F.R. part 56 (2008); 46 Fed. Reg. 8958 (1981).
See 45 C.F.R. part 46 (2005); 46 Fed. Reg. 8366 (1981).
The Centers for Disease Control and Prevention defines program evaluation as the “systematic investigation of the merit, worth, or significance of organized public health action,” noting that such evaluations are “systematic ways to improve and account for public health actions by involving procedures that are useful, feasible, ethical, and accurate.” They can be based on goals, processes, outcomes, or value ( http://www .cdc.gov/mmwr /preview/mmwrhtml/rr4811a1.htm ).
The Utilization Review Accreditation Commission defines utilization review as “the evaluation of the medical necessity, appropriateness, and efficiency of the use of health care services, procedures, and facilities under the provisions of the applicable health benefits plans” ( http://www .urac.org/about/ ).
Another type of oversight board defined by the Privacy Rule. See Chapter 4 .
Under the Privacy Rule, consent is referred to as authorization. See Chapter 4 .
Personal communication, C. Heide, Office for Civil Rights, HHS, May 29, 2008.
The Privacy Rule defines the term “health care operations” by listing a number of specific activities that qualify as health care operations. These include “conducting quality assessment and improvement activities, population-based activities relating to improving or reducing health care costs, and case management and care coordination.” See 45 C.F.R. § 164.501 (2006).
A total of 444 surveys were mailed to the medical directors of quality improvement and IRB chairs at hospitals with 400 or more beds that belong to the Council of Teaching Hospitals of the Association of American Medical Colleges, and to the editors of all U.S.-based medical journals that publish original research and appear in the Abridged Index Medicus. 236 surveys were returned, for a 53 percent response rate. The survey consisted of six brief scenarios that asked respondents to determine whether the described project needed IRB review and informed consent.
See http: //plainlanguage.gov/index.cfm .
FDA, Public Law 110–85 § 801 (2007).
See http://www .ahrq.gov/research/cbprrole .htm .
- Cite this Page Institute of Medicine (US) Committee on Health Research and the Privacy of Health Information: The HIPAA Privacy Rule; Nass SJ, Levit LA, Gostin LO, editors. Beyond the HIPAA Privacy Rule: Enhancing Privacy, Improving Health Through Research. Washington (DC): National Academies Press (US); 2009. 3, The Value, Importance, and Oversight of Health Research.
- PDF version of this title (1.6M)
- Disable Glossary Links
In this Page
Other titles in this collection.
- The National Academies Collection: Reports funded by National Institutes of Health
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Recent Activity
- The Value, Importance, and Oversight of Health Research - Beyond the HIPAA Priva... The Value, Importance, and Oversight of Health Research - Beyond the HIPAA Privacy Rule
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
Official websites use .gov
A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
Microsoft Internet Explorer is not supported on this site. Please use a newer browser.
Careers at CDC

CDC scientists work 24/7 to protect the world from public health threats. Join us today!
Now accepting direct hire applications.
CDC is now accepting applications for a new fellowship !
Register for recruiting events and CDC webinars!
Read the CDC Director's message and review orientation information.
Learn about the opportunities at CDC.
Professionals in nearly all fields can find a career at CDC.
Learn about mission-critical occupations at CDC.
Among the best benefits offered in the private and public sectors.
NIOSH is accepting applications for Associate Director for Mining !
- New Employees
- New Hire Information
- Employee Benefits
Did you know CDC is on Linkedin? Connect with CDC on LinkedIn today!

Did you know that 8 out of 10 employees would recommend CDC as an employer of choice?

The Pathways Program for students and college graduates can be your ticket to a rewarding public health career with the CDC.
The Centers for Disease Control and Prevention works 24/7 to provide the American public with timely and accurate health information, responding to public health emergencies and natural disasters, and monitoring the spread of dangerous and life-threatening diseases.
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
10 high-paying public health jobs right now

Even before the pandemic hit, the field of public health had been experiencing explosive growth, with the number of public health degrees awarded swelling by more than 300% from 1992 to 2016 . Interest in medical professions surged even more after the appearance of COVID-19 on the global stage, with some master’s degree programs in public health (MPH) seeing the largest ever year-over-year increase in applications in their history. That interest hasn’t waned much.
“Students are still very interested across all the different areas of public health,” says Toy Draine, director of career services at George Washington University’s Milken Institute School of Public Health. “The program continues to grow, and our student population continues to grow.”

UNC's Online Master of Public Health Program
For those who are interested in pursuing public health jobs, here are 10 of the field’s top-paying roles.
10. Public health director
Top-paying companies: Bipartisan Policy Center, Amazon, City of Detroit
Description: Public health directors work for governments at the state or local level to manage public healthcare organizations and programs. This role creates and manages programs to improve the overall well being of a population. Public health directors tackle health challenges at the administrative level by consulting with other public health professionals, developing budgets, and reviewing data. They also hold hearings regarding public health issues, create emergency response plans, and report to public health boards of directors.
Salary: $93,124, according to Glassdoor .
Top-paying localities: Boston, Mass. ($121,742), Columbia, S.C. ($100,783), Minneapolis, Minn. ($100,076), according to Zippia .
9. Public health advisor
Top-paying companies: Centers for Disease Control and Prevention, NYC Health + Hospitals, New York City Department of Health and Mental Hygiene
Description: Public health advisors offer guidance and advice to government officials regarding community health. They work with medical and governmental personnel to create policies to address health issues. Often employed by federal agencies like the Centers for Disease Control, this role serves as the link between private medical personnel and the government.
Salary: $94,165, according to ZipRecruiter .
Top-paying localities: Berkeley, Calif. ($114,003), New York, N.Y. ($109,618), Renton, Wash. ($109,289), according to ZipRecruiter .
8. Environmental health and safety officer
Top-paying companies: Trane Technologies, Dunson and Associates, National Composites
Description: Environmental health and safety officers ensure that organizations comply with environmental laws and promote safe working practices. They monitor business operations to identify possible hazards and create procedures and policies to protect employees. This role may work for a single organization or contract to multiple organizations.
Salary : $100,120, according to Indeed
Top-paying localities: Marlborough, N.H. ($119,585), Springfield, Mo. ($109,758), Chicago, Ill. (106,263), according to Indeed .

7. Research scientist
Top-paying companies: NVIDIA, Citizens, Meta
Description: In the realm of public health, research scientists usually specialize in a certain aspect of tackling widespread health problems. By conducting experiments and investigations, they’re able to grapple with chronic diseases, poor nutrition, antibiotic resistance, and maternal mortality.
“They design and perform experiments, collect and analyze data, and publish findings to advance knowledge and inform public health practices,” Draine says.
Salary: $101,547, according to Indeed .
Top-paying localities: Menlo Park, Calif. ($168,417), Berkeley, Calif. ($123,453), San Diego, Calif. ($121,238), according to Indeed .
6. Medical and health services manager
Top-paying companies: AlliedMedix Resources, Advanced Medical and Professional Solutions, Physical Therapy & Sports Medicine Institute
Description: Medical and health services managers work behind the scenes to ensure that nursing homes, hospitals, and other group health facilities run smoothly. They plan, direct, and coordinate the actions of these facilities, and frequently liaise between administrators, doctors, and health insurance representatives. This role requires detail-oriented people with good analytical, communication, technical, and problem-solving skills.
Salary: $110,680, according to BLS .
Top-paying localities: Trenton, N.J. ($193,730), San Francisco, Calif. ($186,560), New York, N.Y. ($ 179,330), according to BLS .
5. Public health consultant
Top-paying companies: Triage Consulting Group, PwC, and Floyd Lee Locums
Description: Public health consultants work with businesses, communities, healthcare facilities, and government agencies to improve a population’s overall health. By providing information to these groups, public health consultants can directly impact the health of the public through improved policies and programs. This role also involves conducting research and, presenting findings to governmental agencies.
Public health consultants “have expertise in analyzing health data, development of public health strategies, evaluation of public health programs, and assisting with the development of policy with the goal of improvement of specific health challenges,” Draine says.
Salary: $112,000, according to Glassdoor .
Top-paying localities: Berkeley, Calif. ($92,733), Bailey’s Crossroads, Va. ($88,179), Daly City, Calif. ($87,761), according to ZipRecruiter .
4. Executive health director
Top-paying companies: Bristol Myers Squibb, Amgen, Alexion Pharmaceuticals
Description: Executive health directors oversee the delivery of healthcare services to communities on behalf of nongovernmental organizations and nonprofits. They make decisions about an organization’s budget and operations, and supervise its daily activities. They also manage program development, marketing, human resources, and fundraising.
“They are responsible for creating strategies and overseeing operations,” Draine says. “In this role they manage the budget of their organization and are the guiding force to [implement] public health programs and policies for improvement of community health.”
Salary: $121,754, according to Glassdoor .
Top-paying localities: San Buenaventura, Calif. ($169,832), Berkeley, Calif. ($117,542), New York, N.Y. ($113,721), according to ZipRecruiter .
3. Biostatistician
Top-paying companies: MWIDM Inc., Smith Hanley Associates LLC, Parexel
Description: Biostatisticians research public health topics using math and statistics. Through their high-level scientific research and analysis of information and data pulled from clinical research studies, biostatisticians can make data-driven decisions about the implementation of public health policies. In the context of public health, they figure out the best way to use resources to treat populations.
Salary: $125,350, according to Indeed .
Top-paying localities: Raleigh, N.C. ($159,790), Chicago, Ill. ($157,600), Redwood City, Calif. ($153,118), according to Indeed .
2. Natural sciences manager
Top-paying companies: Genentech, Chevron, Novartis
Description: Natural sciences managers are administrators who oversee teams of researchers, scientists, and technicians. Through the creation of research strategies, natural science managers lead these teams to achieve an organization’s goals. This role also communicates between researchers and management, determines staffing needs, oversees project resources, and evaluates the operations of an organization’s teams.
“A natural sciences manager within the public health space conducts research and development,” Draine says. “In addition, they manage data collection and analysis with the goal of making sure that scientific projects align with their organization’s public health objectives.”
Salary: $157,740, according to the U.S. Bureau of Labor Statistics .
Top-paying localities: Boston, Mass. ($222,080), New York, N.Y. ($199,990), Washington, D.C. ($166,780), according to BLS .
1. Medical director
Top-paying companies: VitalCore Health Strategies, Premise Health, Takeda Pharmaceuticals
Description: Medical directors manage a medical center or hospital’s daily operations. They guide and oversee the care that is provided at a facility and enact preventative measures to curb the transmission of disease. This leadership role provides a vision for quality improvement, organizes employee training, assesses the quality of healthcare services, and generally promotes the health and wellbeing of both patients and employees.
“A medical director in public health is usually a senior physician,” Draine says. “This role coordinates clinical aspects of public health programs and guides healthcare strategies and ensures compliance with health regulations.”
Salary: $199,661, according to Indeed .
Top-paying localities: Mishawaka, Ind. ($246,546), New Orleans, La. ($233,428), Bridgewater, N.J. ($219,879), according to Indeed .
The takeaway
With the U.S. Bureau of Labor Statistics projecting 1.8 million job openings per year in healthcare through 2032, public health remains an in-demand field that’s perfect for people who want to make a difference.
For those who wish to learn more about public health, Draine recommends checking out the websites of public health organizations like the World Health Organization, Centers for Disease Control, National Institutes of Health, and the Pan American Health Organization.
“It always feels like we’re building a public health army to get out there and help prevent disease, prevent chronic illnesses and try to impact policy,” Draine says. “If anyone is interested in doing that, public health is a good place to be.”

MPH@Simmons
Mba rankings.
- Best Online MBA Programs for 2024
- Best Online Master’s in Accounting Programs for 2024
- Best MBA Programs for 2024
- Best Executive MBA Programs for 2024
- Best Part-Time MBA Programs for 2024
- 25 Most Affordable Online MBAs for 2024
- Best Online Master’s in Business Analytics Programs for 2024
Information technology & data rankings
- Best Online Master’s in Data Science Programs for 2024
- Most Affordable Master’s in Data Science for 2024
- Best Master’s in Cybersecurity Degrees for 2024
- Best Online Master’s in Cybersecurity Degrees for 2024
- Best Online Master’s in Computer Science Degrees for 2024
- Best Master’s in Data Science Programs for 2024
- Most Affordable Online Master’s in Data Science Programs for 2024
- Most Affordable Online Master’s in Cybersecurity Degrees for 2024
Health rankings
- Best Online MSN Nurse Practitioner Programs for 2024
- Accredited Online Master’s of Social Work (MSW) Programs for 2024
- Best Online Master’s in Nursing (MSN) Programs for 2024
- Best Online Master’s in Public Health (MPH) Programs for 2024
- Most Affordable Online MSN Nurse Practitioner Programs for 2024
- Best Online Master’s in Psychology Programs for 2024
Leadership rankings
- Best Online Doctorate in Education (EdD) Programs for 2024
- Most Affordable Online Doctorate in Education (EdD) Programs for 2024
- Coding Bootcamps in New York for 2024
- Best Data Science and Analytics Bootcamps for 2024
- Best Cybersecurity Bootcamps for 2024
- Best UX/UI bootcamps for 2024
Boarding schools
- World’s Leading Boarding Schools for 2024
- Top Boarding School Advisors for 2024

MPH@GW: An Online MPH With Connections in Washington, D.C.
- Search all Locations
- Anchorage, AK
- Fairbanks, AK
- Wasilla, AK
- Glendale, AZ
- Little Rock, AR
- Foster City, CA
- Fullerton, CA
- La Jolla, CA
- Livermore, CA
- Los Angeles, CA
- Richmond, CA
- Sacramento, CA
- Salinas, CA
- San Diego, CA
- San Francisco, CA
- South San Francisco, CA
- Fort Collins, CO
- Farmington, CT
- Greenwich, CT
- New Haven, CT
- West Haven, CT
- Washington, DC
- Gainesville, FL
- Americus, GA
- Atlanta, GA
- Columbus, GA
- Savannah, GA
- Suwanee, GA
- Honolulu, HI
- Twin Falls, ID
- Chicago, IL
- Springfield, IL
- Bloomington, IN
- Indianapolis, IN
- Independence, IA
- Iowa City, IA
- Kansas City, KS
- Lawrence, KS
- Manhattan, KS
- Statewide, KS
- Wichita, KS
- Louisville, KY
- Coushatta, LA
- Marksville, LA
- Winnipeg, MB
- Annapolis, MD
- Baltimore, MD
- Beltsville, MD
- Bethesda, MD
- Hyattsville, MD
- Princess Anne, MD
- Rockville, MD
- Cambridge, MA
- North Grafton, MA
- Detroit, MI
- Minneapolis, MN
- Rochester, MN
- Maryville, MO
- Missoula, MT
- Lincoln, NE
- Las Vegas, NV
- Kenilworth, NJ
- Piscataway, NJ
- Princeton, NJ
- Trenton, NJ
- Albuquerque, NM
- Clayton, NM
- Las Cruces, NM
- Binghamton, NY
- Buffalo, NY
- New Suffolk, NY
- New York, NY
- Staten Island, NY
- Syracuse, NY
- Chapel Hill, NC
- Greenville, NC
- Raleigh, NC
- Grand Forks, ND
- Cincinnati, OH
- Findlay, OH
- Purcell, OK
- Stillwater, OK
- Hillsboro, OR
- Philadelphia, PA
- Pittsburgh, PA
- University Park, PA
- West Point, PA
- San Juan, PR
- Charleston, SC
- Clemson, SC
- Columbia, SC
- Darlington, SC
- Florence, SC
- Greenville, SC
- Richland, SC
- Brookings, SD
- Clarksville, TN
- Knoxville, TN
- Memphis, TN
- Morristown, TN
- Newport, TN
- Oak Ridge, TN
- Corpus Christi, TX
- El Paso, TX
- Fort Worth, TX
- Houston, TX
- Lubbock, TX
- Lake City, UT
- Burlington, VT
- Alexandria, VA
- Arlington, VA
- Blacksburg, VA
- Charlottesville, VA
- Norfolk, VA
- Painter, VA
- Quantico, VA
- Richmond, VA
- Roanoke, VA
- Pullman, WA
- Richland, WA
- Seattle, WA
- Spokane, WA
- Tumwater, WA
- Lewisburg, WV
- Morgantown, WV
- Eau Claire, WI
- Madison, WI
- Milwaukee, WI
- Cheyenne, WY
- Search All Categories
- Academic/Research Jobs
Academic/Research Jobs in Public Health
- next ››
Data and Integrity Branch Chief RESEARCH SCIENTIST SUPERVISOR II
Ection chief, adap evaluation and monitoring section research scientist supervisor i (epi/bio, lrn-c program supervisor | research scientist supervisor i (chemical sciences), pem chief | research scientist supervisor i, public notice for direct hire (data modernization) - operations research specialist, about academic/research jobs in public health.
- Assistant Professor – tenure-track faculty appointments as an Assistant Professor in various public health related departments.
- Research Scientist – provide expert statistical support for the coordination, analysis, and surveillance of various projects & research initiatives.
Connect with Local, State, and Territorial Health Departments
To find local governmental public health jurisdictions, see - www.naccho.org
Careers in research
Join a brilliant team of researchers working to solve technology’s most exciting challenges.
New roles at Microsoft Research
Microsoft Research provides a dynamic environment for research careers with a network of world-class research labs led by globally-recognized research scientists and engineers. Our researchers and engineers pursue innovation in a range of scientific and technical disciplines, to help solve complex challenges in diverse fields, including computing, healthcare, economics, and the environment.
Research Software Engineer II – Azure Research – Systems, Cloud Systems Power Efficiency
Location : Redmond, WA, US
Research Areas : Programming languages and software engineering, Systems and networking
Principal Applied Science Manager – Business Copilot Artificial Intelligence
Research Area : Artificial intelligence
Research Fellow – M365 Research group
Location : Bangalore, Karnataka, India
Research Areas : Artificial intelligence, Programming languages and software engineering, Systems and networking
Senior Applied Science Manager – Microsoft AI Development Acceleration Program
Research Areas : Artificial intelligence, Data platforms and analytics
Senior Researcher – Systems Innovation
Research Areas : Algorithms, Artificial intelligence, Systems and networking
Principal Data Science Manager – Teams Data Sciences
Research Area : Data platforms and analytics
About our roles
Research internships.
Research interns put inquiry and theory into practice. Alongside fellow doctoral candidates and some of the world’s best researchers, interns learn, collaborate, and network for life. Interns not only advance their careers but also contribute to exciting research and development strides. During the 12-week internship, students are paired with mentors and expected to collaborate with other interns and researchers, present findings, and contribute to the vibrant life of the community. Internships are available virtually, at our locations around the world, and in all areas of research. During the application process, we’ll work with you to find the opportunity that best aligns with your interests. Internships are offered year-round, though they typically begin in the summer. All internships are paid. We’ll also help with visa applications where needed.
Postdoctoral researcher positions
Microsoft Research provides a vibrant research environment, with an open publications policy and close links to top academic institutions across the world. Postdoctoral researcher positions provide an opportunity to develop your research career and to interact with some of the top minds in the research community, with the potential to have your research realized in products and services that will be used worldwide. Postdoc researchers are expected to demonstrate both independence in defining their own research strategy within a domain as well as an ability to drive forward an effective program of research. Postdoc researchers receive a competitive salary and benefits package and are eligible for relocation expenses. Our Postdoc positions are typically for a one-year or two-year fixed-term appointment.
Full-time academic research positions
Microsoft research teams are built with the world’s best researchers, engineers, program managers and designers who work together to seek innovative solutions to the world’s toughest challenges and improve the lives of people everywhere. We seek research candidates with PhDs and a proven track record of published papers and participation on program committees and editorial boards for our academic research positions. Microsoft Research has lab locations around the world and provides a collaborative, supportive and open academic environment.
Working at Microsoft Research
Our culture, your future.
Microsoft Research offers an exhilarating and supportive environment for both theoretical and empirical cutting-edge multidisciplinary research, with access to an extraordinary diversity of big and small data sources, an open publications policy, and close links to top academic institutions around the world.

We need your passion for science and your commitment to working on world-class research projects.
To help the researchers with their projects and unleash their full potential, we provide an open interdisciplinary research atmosphere with sufficient computational resources. Worldwide collaborations within Microsoft and with other institutes are encouraged and supported.
As a researcher, you have the opportunity to create and pursue a research agenda with our group’s diverse array of researchers and practitioners, as well as contribute to ongoing research projects.
Our researcher community
Here are just a few of the people doing research at Microsoft in a vast array of disciplines and roles. Learn more about the people who make it all possible.
We are committed to building an inclusive, diverse, and pluralistic research environment and strongly encourage applications from women, minorities, individuals with disabilities, veterans, as well as students with non-traditional backgrounds. We work collectively to make Microsoft Research a welcoming and productive space for all researchers.
Microsoft’s mission is to empower every person and every organization on the planet to achieve more. As employees, we come together with a growth mindset, innovate to empower others, and collaborate to realize our shared goals. Each day we build on our values of respect, integrity, and accountability to create a culture of inclusion where everyone can thrive at work and beyond.

Melissa Boone
Principal Xbox Research Manager

Victor Dibia
Principal Research Software Engineer

Asta Roseway
Principal Research Designer / Fusionist

Deepthi Sudharsan
Research Fellow

Vice President and Managing Director, Microsoft Research Redmond

Jaime Teevan
Chief Scientist & Technical Fellow
Research labs

“Over the coming decade, deep learning looks set to have a transformational impact on the natural sciences. The consequences are potentially far-reaching and could dramatically improve our ability to model and predict natural phenomena over widely varying scales of space and time. Our AI4Science team encompasses world experts in machine learning, quantum physics, computational chemistry, molecular biology, fluid dynamics, software engineering, and other disciplines, who are working together to tackle some of the most pressing challenges in this field.“ Professor Chris Bishop , Technical Fellow and Director, Microsoft Research AI4Science
AI Frontiers

At AI Frontiers, our mission is to revolutionize our understanding of intelligence by pushing the boundaries of AI. We strive to achieve this by continuously exploring and innovating current architectures and learning signals, unlocking new possibilities and shaping the future of AI.

Microsoft Research Asia (MSR Asia), based in Beijing and Shanghai, is Microsoft’s largest research institute outside the United States. Founded in 1998, MSR Asia has grown into a world-class research lab, with more than 300 scientists and engineers and conducts research in: natural user interface, artificial intelligence, cloud and edge computing, big data and knowledge mining, computer science fundamentals, intelligent multimedia, and computational science.
Cambridge Lab

“At Microsoft Research in Cambridge, our mission is to transform the world through deep research. We do this by working together in an interdisciplinary way, in close collaboration with the broader Microsoft business, to ensure that we are designing robust and trusted technologies to empower millions of people worldwide. To truly understand how we can empower others, we need to put the people at the centre of what we do. I am proud to be part of a team who is so enthusiastically committed to exploring and pushing the boundaries for the benefit of our society.” Abigail Sellen , Distinguished Scientist and Lab Director, Microsoft Research Cambridge
Health Futures

Microsoft Health Futures is focused on empowering every person on the planet to live a healthier future. To this end, we are responsible for research, incubations, and moonshots that drive cross-company strategy, partnerships, and real-world impact across healthcare and the life sciences. We are a global, inclusive, and diverse crew of researchers, scientists, engineers, biotechnologists, designers, social scientists, strategists, healthcare experts, and medical professionals.

Microsoft Research India brings together scientists, researchers, and engineers with backgrounds in algorithms, machine learning and AI, systems and socio-technical systems that empower marginalized populations. The lab also includes a Center for Societal impact through Cloud and Artificial Intelligence (SCAI) that focuses on creating, nurturing and deploying technologies that will have large scale impact on society through deep collaborations with academic groups, startups, NGOs and other organizations that share our passion for positively impacting society through technology.
Montréal Lab

The Microsoft Research Montréal lab strives to build machines that learn from and understand the world by bringing together researchers in the machine learning, reinforcement learning, and FATE (fairness accountability, transparency and ethics in AI) research areas. With a focus on advancing the state-of-the-art in deep learning, the lab’s researchers accelerate research breakthroughs across both existing and new models to advance state-of-the-art deep learning that has a positive impact on society.
New England Lab

Microsoft Research New England (MSR-NE) was founded in July 2008 in Cambridge, Massachusetts. The New England lab builds on Microsoft’s commitment to collaborate with the broader research community and pursues new, interdisciplinary areas of research that bring together core computer scientists and social scientists to understand, model, and enable computing and online experiences of the future.
New York City Lab

Researchers at this lab work together with others in Microsoft Research and in academia to advance the state of the art in social science, both computational and behavioral, computational economics and prediction markets, machine learning, as well as information retrieval. Along with helping to answer big data questions, their research will help us to understand economic and political predictions for understanding online human behavior. This research along with their study of social sciences will help to inform the technology of the future.
Redmond Lab

“Microsoft Research is doing foundational research, pursuing ambitious disruptions, and performing high-impact tech transfer. We want to create a better future for Microsoft and society through research.” Johannes Gehrke , Technical Fellow
- Follow on Twitter
- Like on Facebook
- Follow on LinkedIn
- Subscribe on Youtube
- Follow on Instagram
- Subscribe to our RSS feed
Share this page:
- Share on Twitter
- Share on Facebook
- Share on LinkedIn
- Share on Reddit
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- 15 May 2024
Neglecting sex and gender in research is a public-health risk
- Sue Haupt 0 ,
- Cheryl Carcel 1 &
- Robyn Norton 2
Sue Haupt is an honorary senior research fellow at Peter MacCallum Cancer Centre in Melbourne, Australia, and a research associate at The George Institute for Global Health, Women’s Health Program, Centre for Sex and Gender Equity in Health and Medicine, University of New South Wales (UNSW) Sydney, Australia.
You can also search for this author in PubMed Google Scholar
Cheryl Carcel is the head of the brain health programme at The George Institute for Global Health UNSW Sydney, Australia.
Robyn Norton is a founding director of The George Institute for Global Health, a professor of public health at UNSW Sydney and chair of global health at Imperial College London, UK.
Illustration: Sophi Gullbrants
You have full access to this article via your institution.
In 2022, clinical trials indicated that a drug called lecanemab could slow cognitive decline in people with Alzheimer’s disease; soon after the results were published, the global Alzheimer’s community heralded lecanemab as a momentous discovery. However, closer inspection of the data by independent investigators revealed that the drug might significantly help men, but not women 1 .
The finding is a reminder that, even though tremendous advances are being made in the clinical application of cutting-edge technologies, such as gene editing and artificial intelligence (AI), there is a remarkable lack of understanding about how many aspects of human health are affected by variables as seemingly basic as sex and gender.

Sex and gender in science
Over the past decade or so, funders and publishers have made extensive efforts to encourage researchers to address the effects of sex and, in human studies, gender where appropriate. Thanks in part to these efforts, more insights are beginning to emerge. For Alzheimer’s and many other diseases that are common causes of death, including cardiovascular diseases, cancer, chronic respiratory conditions and diabetes, a person’s sex and gender can influence their risk of developing the disease, how quickly and accurately they are diagnosed, what treatment they receive and how they fare.
But even for the most-studied conditions, many questions remain. Few investigators have begun to probe the interrelationships between sex and gender , for example. And in cases in which researchers are managing to unpick the multifaceted effects of sex, this knowledge is not being sufficiently incorporated into the design of clinical trials or adequately changing the practice of medicine.
The consideration of sex and, where appropriate, gender in biological research must become routine — especially as molecular genetics, biomedical engineering and AI open up possibilities for treatments that are better tailored to the needs of individuals. Likewise, the culture of medicine must be transformed so that approaches to treatment evolve in response to the data. This will require further engagement from funders and publishers, but action from many other players, too. Pharmaceutical companies and intergovernmental organizations, among others, must acknowledge three things: how sex and gender can have huge effects on health outcomes; how these effects are often disregarded in basic research and clinical trials; and that change can come only through increasing awareness among all stakeholders of the importance of shifting the dial.
Health outcomes affected
In most human clinical records so far, sex is reported by physicians or participants in studies ticking one of two boxes: ‘female’ or ‘male’. In those clinical studies in which data are collected on chromosomes, hormone levels, reproductive anatomy or other sex characteristics, these features will frequently reflect a person’s sex assigned at birth. But this is not always the case. Added to this, sex and gender have often been used interchangeably, but they are not the same and they do not always align. Current definitions of gender include the social, psychological, cultural and behavioural aspects of being a man or woman (whether cisgender or transgender), non-binary or identifying with one or more other evolving terms 2 .
In several countries, new recommendations about how researchers should obtain data on people’s sex and gender should mean that, in the future, investigators will be able to more-accurately probe the roles of both in human health. But in general, there has been incomplete capture of information for sex and gender so far, including for individuals whose sex characteristics and/or gender identities don’t fall into a binary categorization scheme.

Women are more likely to die after a severe heart attack than are men. Credit: Simon Dawson/Reuters
In this article, consistent with much of the published population-wide data, we refer to a woman as someone who identifies with that gender and was assigned female sex at birth (a cis woman), and a man as someone who identifies with that gender and was assigned male sex at birth (a cis man). But we recognize that participants in the studies we describe might not have been asked about both their gender and their sex.
For all sorts of non-communicable diseases, there are differences between men and women in the average age at which they are diagnosed, the average age at which they die and even in their rates of death.

We need more-nuanced approaches to exploring sex and gender in research
Such variations, from the earlier onset of cardiovascular diseases in men to the more frequent occurrence of Alzheimer’s disease in women, might stem from differences in biology, which can affect people’s likelihood of developing a disease and how they respond to treatment. Or these discrepancies might stem from variation in people’s exposure to the environmental factors that trigger the disease, how they manage their condition, how they are treated by carers and so on, all of which can be influenced by a person’s gender. Often, a combination of factors will be at work.
Take heart attacks. Studies conducted over the past decade have revealed extensive sex differences in the expression of certain genes in heart tissue, which in turn affect the type and function of the cells that make up the heart.
Such variation could help to explain why men are likely to have a heart attack for the first time around six years earlier than women — in the United States, at 65.6 years old in men compared with 72 years old in women 3 — and why (in Australia, at least) heart attacks are at least twice as common in men relative to women of comparable ages (see go.nature.com/3qbvrxq ). Likewise, although mechanisms are yet to be fully understood, it is plausible that differences in people’s biology help to explain why women are more likely to experience pain between their shoulder blades, nausea or vomiting and shortness of breath during a heart attack; why men are more likely to experience chest pain and increased sweating; and why women are nearly twice as likely as are men to die after a severe heart attack.
Yet, when it comes to the risk of dying, social and environmental factors — shaped by gender — also seem to be important.
Tobacco consumption increases a person’s risk of having a heart attack, and smoking is much more common among men globally. Worldwide, around 37% of men smoke compared with around 8% of women . Also, in part because health-care professionals and others are more familiar with the heart attack symptoms commonly seen in men, when women have a heart attack, they are more likely to delay seeking help, and carers are often slower to intervene 4 . In fact, in a study of more than 500,000 people who experienced a heart attack and were admitted to hospital in the United Kingdom between 2004 and 2013, women were 37% more likely to receive an incorrect initial diagnosis after a severe heart attack than were men 5 . Even when women tell their physicians that they have chest pain, they are two to three times less likely to be referred to a cardiologist than are men 6 .
A similarly complicated picture has been emerging in relation to strokes 7 — another cardiovascular disease — and, in the past few years, in relation to cancer.

Smoking is more common among men than women globally. Credit: Behrouz Mehri/AFP/Getty
Most cancers that occur in non-reproductive organs develop earlier in men than they do in women. In the United States, oesophageal cancer is 4.5 times more likely to occur and cause death in men than in women, for example, and lung cancers, the most common drivers of cancer-associated deaths worldwide, kill around 40% more men than women 8 .
Just as with heart disease and stroke, some of this variation seems to stem from behavioural differences. Tobacco consumption increases a person’s risk of developing several cancers 7 . For thyroid cancers, however, women are more likely to develop the disease than are men — three times more likely in some places — which suggests that other factors might drive the different rates of this particular cancer in women and men 9 . But tumours typically arise because of problems with cells’ genetic-repair systems, together with inadequate damage clearance, and genetic differences between men and women that affect cancers are beginning to emerge.

Male–female comparisons are powerful in biomedical research — don’t abandon them
Much more research is needed to understand how sex affects the rate at which genes mutate, cells’ capacities to repair and clear damaged DNA, and when genetic damage starts causing disease. Yet research led by one of us (S.H.) on lung adenocarcinoma, the most common type of lung cancer, suggests that women can survive for longer than men after they are diagnosed, in part thanks to cancer-defence genes in women driving more-robust immune responses 10 . X chromosomes encode many genes that are linked to immunity, and women with two X chromosomes might express these genes at higher levels than men with XY chromosomes.
Responses to cancer treatments also differ between men and women. Chemotherapies tend to work better in women than in men. This could be because it can take longer for women’s bodies to clear certain drugs, which could partly explain why women are also 34% more likely than men to experience harmful side effects 11 . Moreover, women with lung cancer typically have better outcomes after surgery, which they undergo more often than men 8 . This is probably due, at least in part, to women having less advanced disease when they are diagnosed than men do 12 . But the generally stronger immune responses in women might also help their recovery 8 .
Too often ignored
Despite these compelling indications that sex and gender matter, when it comes to many diseases that are leading causes of death, many researchers and health practitioners still fail to adequately take sex and gender into account. They might also be influenced by conscious or unconscious bias.
In the case of heart disease, the differences in gene expression and cellular make-up and activity found in men and women’s hearts highlight the need for sex-specific cardiac tissue models, sustained by sex-appropriate vasculature 13 . (Women on average have smaller hearts with narrower vessels compared with men.) Currently, researchers tend to construct heart models using either animal or human cells, but without necessarily ensuring that cells are sourced from individuals of only one sex per model. In fact, identifying sex disparities in basic heart biology is crucial to engineering relevant heart models with stem cells, for example, which investigators are now developing to aid the study of heart disease 13 .
For both heart disease and stroke, because of decades of under-representation of women in clinical trials, many of today’s standard treatments are based on studies of what happens in men who weigh around 70 kilograms. In clinical trials conducted for stroke and heart conditions between 2010 and 2017, women worldwide were under-enrolled relative to the prevalence of these diseases in the general population — by around 20% 14 . There is also significant underfunding of research for many conditions that are more prevalent in women compared with those that are more common in men (see ‘Disparities in health and disease’).
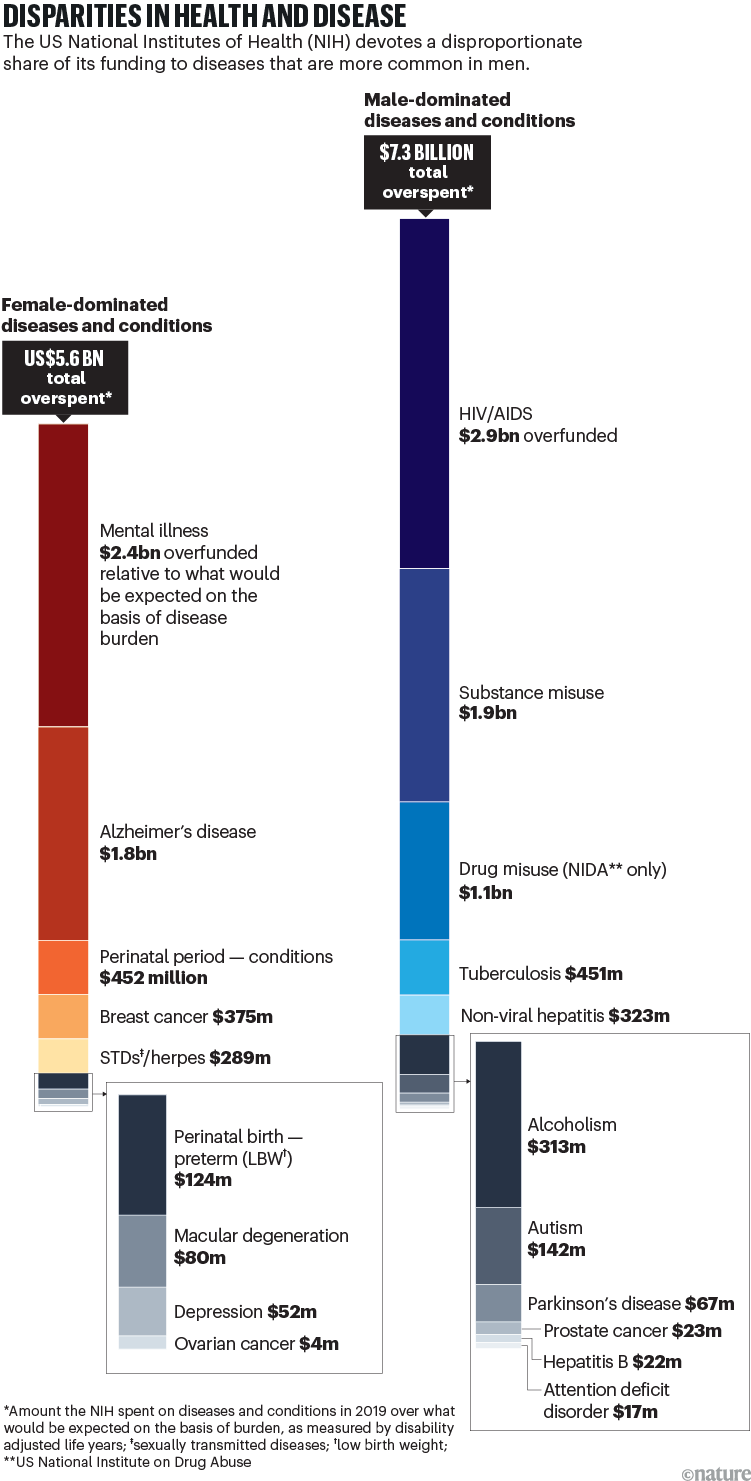
Source: A. A. Mirin J. Womens Health 30 , 956–963 (2021).
Basic research on cancer is similarly riddled with problems. Take the sex of the cell lines that are stored in commercial cell banks, which have been studied for decades and are the source of much of today’s textbook knowledge. For lung cancers, male lines outnumber female lines by two to one. For liver cancers, the ratio is seven to one. Until a few years ago, few researchers studying cancer in cultured cells in the lab even considered the sex of the cells they were studying. Also, the standard media in which cells are grown is frequently supplemented with fetal calf serum from a mixture of male and female calves, and so contains both male and female sex hormones. And phenol red, a dye commonly used to monitor the pH of tissue culture media mimics the hormone oestrogen 8 .
To add to the difficulties, research findings that emerge from the use of these cell lines are often tested in mice of only one sex. The results of these studies are then used to guide human trials that include both men and women participants. And in oncological clinical trials, just as with stroke and heart disease, women are still under-enrolled relative to the burden of disease they experience 7 .
Inclusivity in human trials will ensure the best possible outcomes for all participants, including cis and trans women and men, gender-diverse and intersex people (see ‘Inclusivity in practice’). Studies are showing, for example, that circadian rhythms — which can affect heart function and might impact how drugs are metabolized — differ between men and women 15 . So how might they compare in non-binary or transgender people? Likewise, knowledge about the immune responses of people with atypical numbers of sex chromosomes is likely to be crucial when it comes to the use of immune checkpoint inhibitors and other immune therapies for treating cancer. Those with Klinefelter syndrome, for example, who, similar to cis women, are at a higher risk of developing breast cancer than are cis men, have multiple X chromosomes that are rich in genes involved in the immune response.
Inclusivity in practice
How researchers include diverse groups of people in clinical trials with enough participants to be able to uncover between-group differences is a challenge.
Women represent nearly half of the population, but they are still under-represented in many clinical trials for numerous diseases, even in cases in which disease prevalence for women has been measured. For smaller population groups, such as transgender people, there are not enough data to even know what representative inclusion looks like. In fact, even if participation does reflect the prevalence of disease in the broader population in any one trial, teasing out effects might require combining the results of multiple studies in meta-analyses.
Advisory governing boards for pharmaceutical companies, such as the International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use, funders and regulatory agencies could help with this by ensuring that terminology is adequately and consistently defined, and that populations are properly profiled.
Heightened awareness
Routinely taking sex and gender into account in research and using that knowledge to change health care could benefit billions of people. So what’s needed to make this happen?
Policy changes — such as the US National Institutes of Health’s 2016 call for the inclusion of male and female sexes in studies involving cells, tissues and animals — are crucial. But for many researchers, such calls seem burdensome, especially because studying more than one sex can increase costs. ( Sample sizes might need to be increased to achieve sufficient statistical power when comparing groups.)
Alongside initiatives from funders and publishers, awareness must be built — among students, researchers, clinicians, medical ethics committees, research governance bodies and community groups — of the ramifications of failing to consider sex and gender, and how to correct the problem.

Accounting for sex and gender makes for better science
Efforts led by the Canadian Institutes of Health Research (CIHR) are encouraging. Even though the permeation of knowledge from research to health care has been glacial, between 2011 and 2019, the proportion of all research grant applications submitted to the CIHR that took sex into consideration increased from around 22% to 83%. Gender as a variable is now also included in many of the human studies funded by the CIHR .
Several initiatives have contributed to this. As an example, as well as asking grant applicants to include a section in their research proposals on whether they are considering sex and gender and how they will do so, or why this is not considered applicable, the CIHR has provided training for scientists and organized workshops involving researchers and specialists in sex and gender. Applicants are more likely to receive funding if they provide a satisfactory rationale for their choices.
Convincing people in leadership roles — in governments, laboratories, medical ethics boards, education and so on — of the importance of including sex and gender in research is especially crucial. More studies demonstrating the financial costs of not doing so could help. Between 1997 and 2000, for instance, eight prescription drugs were retracted from the US market because inadequate clinical testing in women had failed to identify that the drugs put women at greater risk of developing health problems than men. This error cost pharmaceutical companies and taxpayers an estimated US$1.6 billion per drug 16 .
The scale of transformation needed will also require more engagement from global players.
Even as far back as 2007, the 60th World Health Assembly — the decision-making body of the World Health Organization (WHO) — passed a resolution to urge researchers to split their data according to sex and to include gender analyses where appropriate. Steps to improve care for transgender people or those with diverse genders are also starting to be taken; in December last year, the WHO established a Guideline Development Group, to provide recommendations on how to address the health of transgender and gender-diverse people . But more extensive efforts, comparable to all United Nations member states committing to target 5.b of the 2015 Sustainable Development Goals by 2030, will be crucial. (This target is to “enhance the use of enabling technology, in particular information and communications technology, to promote the empowerment of women”.)
Lastly, under the guidance of regulatory bodies such as the European Medicines Agency and the scientific entrepreneur community, the pharmaceutical industry must do more to ensure that preclinical work is robust, and that products are tested on enough people of different sexes and genders. Many leading pharmaceutical companies acknowledge on their websites the importance of including diverse groups in clinical trials , but evidence of actions to address the issue is only just emerging.
Awareness of the problems around sex and gender is growing fast. And although many are concerned that medical applications of AI will perpetuate already existing biases 17 , promising developments are emerging in the use of machine learning to make diagnoses that are appropriate for people’s sex and gender.
For decades, for instance, physicians worldwide have been determining whether a person has had a heart attack by using the Global Registry of Acute Coronary Events (GRACE) score, which was derived from trials mainly involving men. In 2022, the application of machine learning to data that had been split for men and women refined the predictors for women. And these revised predictors did a better job of matching individuals to appropriate interventions 18 .
Greater awareness, the wealth of data now emerging and the possibilities presented by new tools, from AI to gene editing, could mean a new era for research and medicine.
Nature 629 , 527-530 (2024)
doi: https://doi.org/10.1038/d41586-024-01372-2
Buckley, R. F., Gong, J. & Woodward, M. JAMA Neurol . 80 , 769–770 (2023).
Article PubMed Google Scholar
Mauvais-Jarvis, F. et al. Lancet 396 , 565–582 (2020).
Benjamin, E. J. et al. Circulation 137 , e67–e492 (2018).
Stehli, J. et al. J. Am. Heart Assoc . 10 , e019938 (2021).
Wu, J. et al. Eur. Heart J. Acute Cardiovasc. Care 7 , 139–148 (2018).
Clerc Liaudat, C. et al. Womens Health https://doi.org/10.1177/1745506518805641 (2018).
Article Google Scholar
Carcel, C. et al. Nature Med. 30 , 51–60 (2024).
Haupt, S., Caramia, F., Klein, S. L., Rubin, J. B. & Haupt, Y. Nature Rev. Cancer 21 , 393–407 (2021).
Kim, J., Gosnell, J. E. & Roman, S. A. Nature Rev. Endocrinol. 16 , 17–29 (2020).
Freudenstein, D. et al. Cancers 12 , 1535 (2020).
Unger, J. M. et al. J. Clin. Oncol. 40 , 1474–1486 (2022).
Stabellini, N. et al. JTO Clin. Res. Rep. 3 , 100307 (2022).
PubMed Google Scholar
Lock, R. et al. Nature Rev. Mater. 7 , 295–313 (2022).
Jin, X. et al. Circulation 141 , 540–548 (2020).
Lévi, F. A., Okyar, A., Hadadi, E., Innominato, P. F. & Ballesta, A. Annu. Rev. Pharmacol. Toxicol. 64 , 89–114 (2024).
Wouters, O. J., McKee, M. & Luyten, J. JAMA 323 , 844–853 (2020).
Cirillo, D. et al. npj Digit. Med. 3 , 81 (2020).
Wenzl, F. A. et al. Lancet 400 , 744–756 (2022).
Download references
Reprints and permissions
Competing Interests
The authors declare no competing interests.
Related Articles

Podcast: Sex and gender discussions don't need to be toxic

Let’s talk about (biological) sex
- Public health
- Medical research

Can mathematicians help to solve social-justice problems?
Career Feature 22 MAY 24

Why role-playing games can spur climate action
World View 22 MAY 24
Internet use and teen mental health: it’s about more than just screen time
Correspondence 21 MAY 24

Ozempic keeps wowing: trial data show benefits for kidney disease
News 24 MAY 24
Trials that infected people with common colds can inform today’s COVID-19 challenge trials

A global pandemic treaty is in sight: don’t scupper it
Editorial 21 MAY 24

First ‘bilingual’ brain-reading device decodes Spanish and English words
News 21 MAY 24
Professor, Division Director, Translational and Clinical Pharmacology
Cincinnati Children’s seeks a director of the Division of Translational and Clinical Pharmacology.
Cincinnati, Ohio
Cincinnati Children's Hospital & Medical Center
Data Analyst for Gene Regulation as an Academic Functional Specialist
The Rheinische Friedrich-Wilhelms-Universität Bonn is an international research university with a broad spectrum of subjects. With 200 years of his...
53113, Bonn (DE)
Rheinische Friedrich-Wilhelms-Universität
Recruitment of Global Talent at the Institute of Zoology, Chinese Academy of Sciences (IOZ, CAS)
The Institute of Zoology (IOZ), Chinese Academy of Sciences (CAS), is seeking global talents around the world.
Beijing, China
Institute of Zoology, Chinese Academy of Sciences (IOZ, CAS)
Full Professorship (W3) in “Organic Environmental Geochemistry (f/m/d)
The Institute of Earth Sciences within the Faculty of Chemistry and Earth Sciences at Heidelberg University invites applications for a FULL PROFE...
Heidelberg, Brandenburg (DE)
Universität Heidelberg
Postdoc: deep learning for super-resolution microscopy
The Ries lab is looking for a PostDoc with background in machine learning.
Vienna, Austria
University of Vienna
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies

Transforming the understanding and treatment of mental illnesses.
Información en español
Celebrating 75 Years! Learn More >>
- Science News
- Meetings and Events
- Social Media
- Press Resources
- Email Updates
- Innovation Speaker Series
Basic Research Powers the First Medication for Postpartum Depression
May 14, 2024 • Feature Story • 75th Anniversary
At a Glance
- Postpartum depression (PPD) is a common mental disorder that many women experience after giving birth.
- Onset of PPD coincides with a dramatic drop in levels of a brain-derived steroid (neurosteroid) known as allopregnanolone.
- Decades of research supported by NIMH illuminated the role of neurosteroids like allopregnanolone in mental illnesses.
- In 2019, brexanolone—a medication that acts by mimicking allopregnanolone—became the first approved drug to treat PPD.
- Able to significantly and rapidly reduce PPD symptoms, brexanolone was a major leap forward in depression treatment.
Joshua A. Gordon, M.D., Ph.D., a practicing psychiatrist at the time, would never forget the call he received one night from a distraught mother.

“She was plagued with a deep, inescapable hopelessness—so depressed she was afraid she was going to hurt her month-old daughter. I helped her get to the hospital, where she spent the next 2 months in an in-patient program trying every available treatment to recover,” said Dr. Gordon, now the Director of the National Institute of Mental Health (NIMH).
Unfortunately, this experience is not uncommon among women and other postpartum people who may feel intense sadness, anxiety, and loss of interest after giving birth. These symptoms can be signs of a clinical disorder known as postpartum depression (PPD) . Unlike the "baby blues" or feelings of sadness many new mothers experience in the days after delivery, PPD is more intense and long-lasting, with damaging impacts on health and well-being.
More than the blues: Impacts of PPD on women's mental health
Depression is a common but serious mood disorder. According to the Centers for Disease Control and Prevention (CDC), rates of depression are high—and rising—among postpartum women. Using data from the 2018 Pregnancy Risk Assessment Monitoring System , the CDC found that about 1 in 8 postpartum women had symptoms of depression, while another CDC study showed rates of PPD that were seven times higher in 2015 compared to 2000.
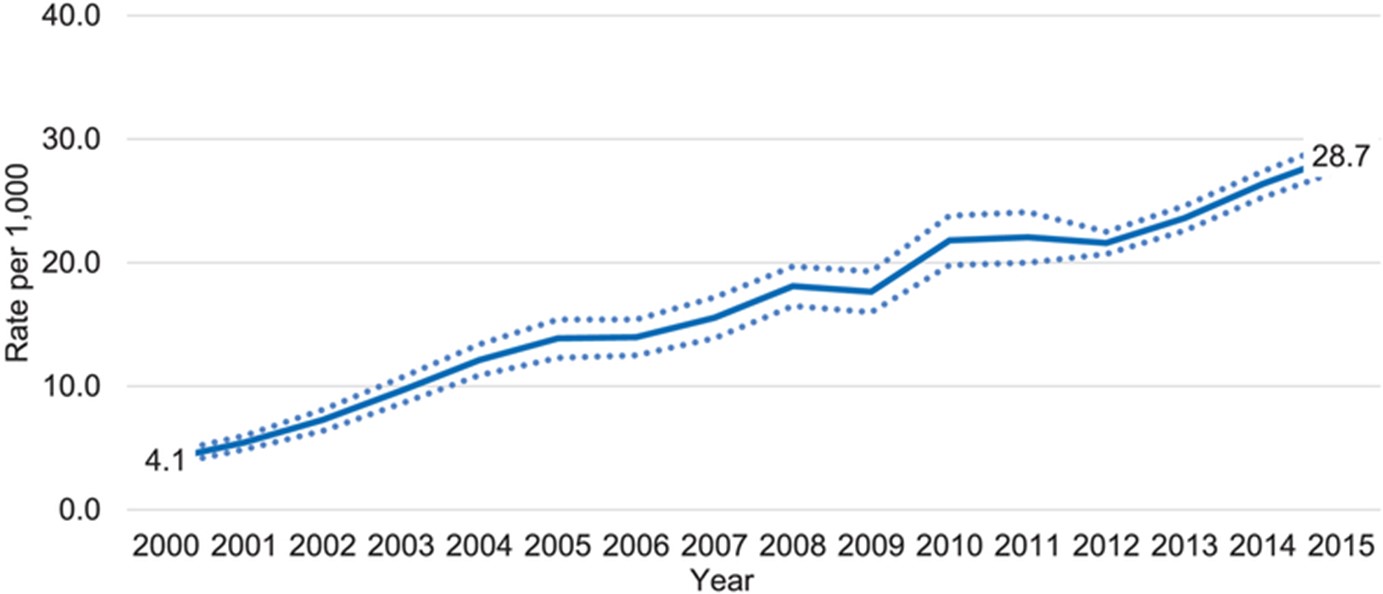
Depression can happen to anyone, and it's especially tough for new moms dealing with the physical challenges of childbirth and the stresses of caring for a young child. When women experience PPD, they often have strong feelings of sadness, anxiety, worthlessness, and guilt. Their sleep, eating, thoughts, and actions can all change noticeably. These mood and behavior changes can be highly distressing and even life-threatening, making it difficult for a woman to do everyday things and take care of herself or her child. In extreme cases, women with PPD may be at risk of hurting themselves or their child or attempting suicide.
Fast-acting, effective treatment for PPD can be life-changing and potentially lifesaving. However, for too long, such care was hard to reach, leaving many women to struggle with depression at a pivotal point in life. Despite some similarities, PPD is not the same as major depression at other times in life. Because of this, usual depression treatments are much less effective in managing the symptoms of PPD.

“PPD is very difficult to treat,” said Mi Hillefors, M.D., Ph.D., Deputy Director of the NIMH Division of Translational Research. “It is usually treated with medications originally approved for major depression—despite limited evidence that they are effective in treating PPD. Standard depression treatments, including antidepressants, psychotherapy, and brain stimulation therapy, can also take weeks or longer to work.”
PPD’s unique risk factors reflect the physical changes of pregnancy and the postpartum period, which include dramatic changes in levels of many hormones and other molecules.
These biological changes had long been seen as a possible source of postpartum mood disorders like depression. But could they also be a solution?
Unlocking the power of allopregnanolone through basic research
Some psychiatric medications owe their discovery to chance. Not so with brexanolone, the first-ever medication to specifically treat PPD. Brexanolone culminated a long series of research studies, much of it funded by NIMH as part of its commitment to understand and support women’s mental health .
Thanks to NIMH-supported basic research, brexanolone was developed by design—a design centered around a molecule called allopregnanolone .
Allopregnanolone is a steroid naturally produced in the brain and with important actions there, such as regulating neurotransmitter activity and protecting neurons from damage. Its impact extends to mental health, with higher levels linked to better mood, lower anxiety, and reduced depression .
Allopregnanolone is also important to pregnancy , during which its levels are extremely high. This happens because of the enhanced production of a hormone called progesterone, which prepares the body for pregnancy and childbirth.
In the last few months of pregnancy, the ovaries and placenta make more progesterone, causing a huge rise in allopregnanolone levels. These levels then drop rapidly after birth. Because allopregnanolone plays a crucial role in mood, these ups and downs can impact a woman’s mental health during and after pregnancy.
Researchers had been aware of brain-derived steroids like allopregnanolone as far back as the 1940s. But the journey to a new PPD treatment began within NIMH's Intramural Research Program (IRP) . At the helm was the NIMH Scientific Director at that time, Steven Paul, M.D., who collaborated with researchers in the NIMH Clinical Neuroscience Branch and at other NIH institutes, including the National Institute of Neurological Disorders and Stroke (NINDS). The researchers sought to understand how the steroids work, change over time, respond to stress, and ultimately relate to health and disease.
Early discoveries came in the 1980s. Paul, working with Maria Majewska, Ph.D., Jacqueline Crawley, Ph.D., A. Leslie Morrow, Ph.D., and other researchers showed that hormones such as progesterone and molecules derived from them have calming and anxiety-reducing effects . Extensive research by Paul’s lab showed that these anxiolytic effects come from enhancing the activity of GABA by binding to specific sites on its receptor. As the main inhibitory neurotransmitter (chemical messenger), GABA reduces the activity of neurons, making them less likely to fire. When molecules bind to its receptor, GABA becomes more potent at inhibiting electrical activity in the brain, with calming effects on behavior.
Paul and IRP colleague Robert Purdy, Ph.D., used the term “ neuroactive steroids ,” or neurosteroids, to describe these molecules able to bind to receptors in the brain to rapidly alter neuronal excitability. Their work in animals confirmed that allopregnanolone is synthesized in the brain . They also showed the effects of allopregnanolone on GABA receptors in humans. Moreover, they found that allopregnanolone affects the response to stress , with acute stress leading the neurosteroid to increase to levels that alter GABA activity. These findings suggested that neurosteroids play an important role in helping animals “reset” and adaptively respond to stressful life events.
Together, this IRP-conducted research established the importance of neurosteroids via their presence in the brain, ability to reduce neuronal activity, and release during stress. Although much of this work was conducted in animals, it would spotlight neurosteroids—and allopregnanolone in particular—as promising targets for treating mental disorders, eventually opening the door to their therapeutic use in humans.
Bridging the gap to advance clinical intervention
While NIMH intramural researchers were making remarkable strides, researchers at other institutions were also conducting work bolstered by funding from NIMH. Among them were Alessandro Guidotti, M.D., at the University of Illinois at Chicago; Istvan Mody, Ph.D., at the University of California, Los Angeles; and Charles Zorumski, M.D., at Washington University in St. Louis. Their NIMH-funded research propelled understanding of inhibitory neurosteroids and their importance in reducing the adverse effects of stress. This work would be the impetus for homing in on allopregnanolone as a treatment for PPD.

Guidotti and colleagues conducted several NIMH-funded studies. Their research in rodents confirmed that allopregnanolone is produced in the brain and helps regulate neuronal excitability by acting on GABA receptors. They also built on the knowledge that neurosteroids are affected by stress. However, unlike acute stress, a stressor lasting multiple weeks led to a decrease in allopregnanolone in brain areas involved in anxiety- and depression-like behaviors.
Importantly, their NIMH-funded work offered some of the earliest evidence that allopregnanolone contributes to depression by showing significantly lower levels in people with depression compared to people without the disorder, a rise in levels (but not that of other neurosteroids) after treatment with antidepressant medication , and a link between increased levels and reduced depression symptoms .
NIMH and NINDS funded multiple studies by Mody and colleagues on interactions of neurosteroids, stress, and GABA receptors. This research was integral to understanding a mechanism in the brains of mice that might explain why some people become depressed after childbirth. Their NIMH-supported research showed changes in GABA receptors in the brain, where neurosteroids are active, that impaired the body’s ability to adapt to hormonal fluctuations. Animals with an irregular GABA receptor component lacking sensitivity to neurosteroids showed depression-like behaviors and reduced maternal care; treating them with a drug that restored the receptor’s function reversed those changes.
Another study by Mody and colleagues revealed changes in GABA expression during pregnancy that led to greater neuronal activity in the brain—but could be brought down by allopregnanolone. This finding opened the door to future studies exploring whether a postpartum drop in the neurosteroid contributed to the risk for mood disorders after birth.
Zorumski led a team in extensively studying neurosteroids as well. Among their seminal findings was identifying the mechanisms by which inhibitory neurosteroids like allopregnanolone affect GABA receptor activity . Their NIMH-funded work dramatically augmented knowledge of how neurosteroids alter GABA receptors to contribute to the risk for mental disorders like PPD.
“The accumulated evidence from these studies established the necessary bridges to justify examining a potential therapeutic role for allopregnanolone in women with PPD,” said Peter Schmidt, M.D., Chief of the NIMH Behavioral Endocrinology Branch.
By the 2010s, researchers had a much better understanding of how allopregnanolone is linked to PPD. Studies showed decreased allopregnanolone in pregnant and postpartum women with symptoms of depression and higher allopregnanolone associated with a lower risk of PPD . The possibility that PPD might be caused by the downregulation of GABA receptors in response to low levels of allopregnanolone after birth inspired researchers to put that theory to the test in clinical studies with human participants.
Taking allopregnanolone from bench to bedside
Extensive research, supported by NIMH and other NIH institutes, found that neurosteroids play a key role in how people deal with stress. They also contribute to the development of mood disorders like anxiety and depression. For allopregnanolone, evidence that it sharply decreases after pregnancy and regulates GABA activity gave rise to the notion that it contributes to PPD—and inspired hope it could be used to treat the disorder.
The biopharmaceutical company Sage Therapeutics utilized this basic research to develop brexanolone. Administered intravenously by a health care professional in a doctor’s office or clinic, brexanolone mimics the effects of allopregnanolone, increasing the inhibitory actions of GABA receptors.
Stephen Kanes, M.D., Ph.D., at Sage Therapeutics and Samantha Meltzer-Brody, M.D., MPH, at the University of North Carolina led several randomized clinical trials to measure the effectiveness of the medication in treating PPD and evaluate its safety and tolerability. The studies, which recruited adult women with PPD from hospitals, research centers, and psychiatric clinics across the United States, measured the effects of brexanolone compared to a placebo over 4 weeks.
The trials were a success. Brexanolone significantly and meaningfully reduced PPD symptoms , and it had only mild side effects. Compared to usual depression treatments, brexanolone brought about a faster response and greater improvement . Whereas most antidepressants take weeks to work, brexanolone improved symptoms and functioning in women with PPD within a few hours to days. And the effects lasted up to a month after the treatment stopped. Not only was brexanolone more effective, but it also worked faster than other depression medications.
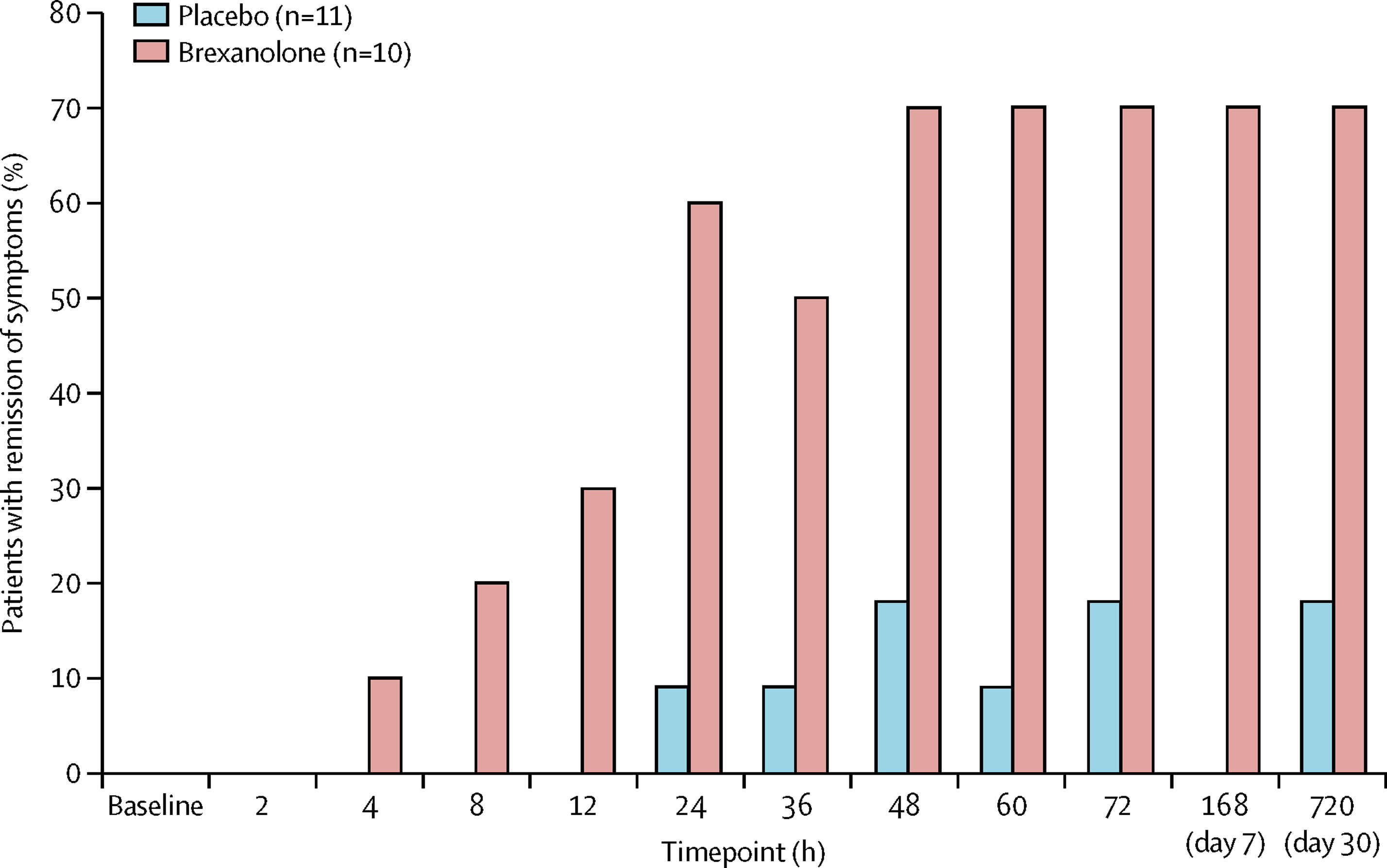
“The dramatic impact of basic research on real-world health outcomes has been inspiring. The fact that NIMH-supported studies contributed to successful drug development in a matter of decades is a remarkable feat and a powerful demonstration of the potential of this foundational research,” said Dr. Gordon.
Based on this promising evidence, the U.S. Food and Drug Administration (FDA) gave brexanolone priority review and breakthrough therapy designation in September 2016. Then, in March 2019, the FDA approved brexanolone , making it the first drug to treat PPD.
Brightening the future for women with PPD
For women with PPD, brexanolone was a long-awaited reason to celebrate. For NIMH, it was a testament to discoveries made through the decades of research it supported. Although some barriers to treatment persisted, women now had greater hope for treating depression symptoms after pregnancy.
“The approval of brexanolone was an important milestone. Finally, an effective, fast-acting medication specifically to treat PPD,” said Dr. Hillefors. “It was also a victory for psychiatric neuroscience because basic and translational research—by design, not chance—led to a truly novel and effective treatment for a psychiatric disorder.”
Without NIMH-supported studies providing the foundational knowledge of neurosteroids, researchers may have never made the connection between allopregnanolone and treating PPD. “That’s why the approval of brexanolone is such a cause for celebration for mental health research: It represents a true bench-to-bedside success,” said Dr. Gordon.
The success of brexanolone has continued to open the door to exciting advancements in mental health care. For instance, researchers and clinicians are investigating ways to make brexanolone work better for all postpartum people. Researchers are also testing how neurosteroids can be used to treat other forms of depression and other mental health conditions.
Just the beginning of treatment advances for PPD
Brexanolone is only the start of what will hopefully be a new future for PPD treatment. In August 2023, the FDA approved zuranolone as the first oral medication for PPD. Zuranolone acts via similar biological mechanisms as brexanolone. Its approval reflects the next step in NIMH-supported basic research being translated into clinical practice with real-world benefits.
The success of the drug, which is taken in pill form, was shown in two randomized multicenter clinical trials . Women with severe PPD who received zuranolone showed statistically significant and clinically meaningful improvements in depression symptoms compared to women who received a placebo. These effects were rapid, sustained through 45 days, and seen across a range of clinical measures. The benefits were mirrored in patients’ self-assessment of their depression symptoms.
According to Dr. Schmidt, “The approval of zuranolone to treat PPD provides women with a rapid and effective treatment that avoids some of the limitations of the original intravenous medication.”
And the journey is far from over. Researchers, clinicians, and industry are continuing to innovate new treatments for PPD to increase access and availability to ensure all people can receive help for their postpartum symptoms.
“While I will never forget that phone call from my patient, the development of these effective medications brings us hope for helping people with PPD and for the overall impact of basic research to truly make a difference in people’s lives,” concluded Dr. Gordon.
Publications
Burval, J., Kerns, R., & Reed, K. (2020). Treating postpartum depression with brexanolone. Nursing , 50 (5), 48−53. https://doi.org/10.1097/01.NURSE.0000657072.85990.5a
Cornett, E. M., Rando, L., Labbé, A. M., Perkins, W., Kaye, A. M., Kaye, A. D., Viswanath, O., & Urits, I. (2021). Brexanolone to treat postpartum depression in adult women. Psychopharmacology Bulletin , 51 (2), 115–130. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8146562/pdf/PB-51-2-115.pdf
Deligiannidis, K. M., Meltzer-Brody, S., Maximos, B., Peeper, E. Q., Freeman, M., Lasser, R., Bullock, A., Kotecha, M., Li, S., Forrestal, F., Rana, N., Garcia, M., Leclair, B., & Doherty, J. (2023). Zuranolone for the treatment of postpartum depression. American Journal of Psychiatry , 180 (9), 668−675. https://doi.org/10.1176/appi.ajp.20220785
Deligiannidis, K. M., Kroll-Desrosiers, A. R., Mo, S., Nguyen, H. P., Svenson, A., Jaitly, N., ... & Shaffer, S. A. (2016). Peripartum neuroactive steroid and γ-aminobutyric acid profiles in women at-risk for postpartum depression. Psychoneuroendocrinology , 70 , 98−107. https://doi.org/10.1016/j.psyneuen.2016.05.010
Edinoff, A. N., Odisho, A. S., Lewis, K., Kaskas, A., Hunt, G., Cornett, E. M., Kaye, A. D., Kaye, A., Morgan, J., Barrilleaux, P. S., Lewis, D., Viswanath, O., & Urits, I. (2021). Brexanolone, a GABAA modulator, in the treatment of postpartum depression in adults: A comprehensive review. Frontiers in Psychiatry , 12 , Article 699740. https://doi.org/10.3389/fpsyt.2021.699740
Epperson, C. N., Rubinow, D. R., Meltzer-Brody, S., Deligiannidis, K. M., Riesenberg, R., Krystal, A.D., Bankole, K., Huang, M. Y., Li, H., Brown, C., Kanes, S. J., & Lasser R. (2023). Effect of brexanolone on depressive symptoms, anxiety, and insomnia in women with postpartum depression: Pooled analyses from 3 double-blind, randomized, placebo-controlled clinical trials in the HUMMINGBIRD clinical program. Journal of Affective Disorders , 320 , 353−359. https://doi.org/10.1016/j.jad.2022.09.143
Gilbert Evans, S. E., Ross, L. E., Sellers, E. M., Purdy, R. H., & Romach, M. K. (2005). 3α-reduced neuroactive steroids and their precursors during pregnancy and the postpartum period. Gynecological Endocrinology , 21 (5), 268−279. https://doi.org/10.1080/09513590500361747
Guintivano, J., Manuck, T., & Meltzer-Brody, S. (2018). Predictors of postpartum depression: A comprehensive review of the last decade of evidence. Clinical Obstetrics and Gynecology , 61 (3), 591−603. https://doi.org/10.1097/GRF.0000000000000368
Gunduz-Bruce, H., Koji, K., & Huang, M.-Y. (2022). Development of neuroactive steroids for the treatment of postpartum depression. Journal of Neuroendocrinology , 34 (2), Article e13019. https://doi.org/10.1111/jne.13019
Haight, S. C., Byatt, N., Moore Simas, T. A., Robbins, C. L., & Ko, J. Y. (2019). Recorded diagnoses of depression during delivery hospitalizations in the United States, 2000-2015. Obstetrics and Gynecology , 133 (6), 1216−1223. https://doi.org/10.1097/AOG.0000000000003291
Hellgren, C., Åkerud, H., Skalkidou, A., Bäckström, T., & Sundström-Poromaa, I. (2014). Low serum allopregnanolone is associated with symptoms of depression in late pregnancy. Neuropsychobiology , 69 (3), 147–153. https://doi.org/10.1159/000358838
Hutcherson, T. C., Cieri-Hutcherson, N. E., & Gosciak, M. F. (2023). Brexanolone for postpartum depression. American Journal of Health-System Pharmacy , 77 (5), 336−345. https://doi.org/10.1093/ajhp/zxz333
Kanes, S., Colquhoun, H., Gunduz-Bruce, H., Raines, S., Arnold, R., Schacterle, A., Doherty, J., Epperson, C. N., Deligiannidis, K. M., Riesenberg, R., Hoffmann, E., Rubinow, D., Jonas, J., Paul, S., & Meltzer-Brody, S. (2017). Brexanolone (SAGE-547 injection) in post-partum depression: A randomised controlled trial. The Lancet , 390(10093), 480−489. https://doi.org/10.1016/S0140-6736(17)31264-3
Leader, L. D., O'Connell, M., & VandenBerg, A. (2019). Brexanolone for postpartum depression: Clinical evidence and practical considerations. Pharmacotherapy , 39 (11), 1105–1112. https://doi.org/10.1002/phar.2331
Maguire, J., & Mody, I. (2008). GABAAR plasticity during pregnancy: Relevance to postpartum depression. Neuron , 59 (2), P207–P213. https://doi.org/10.1016/j.neuron.2008.06.019
Maguire, J., & Mody, I. (2016). Behavioral deficits in juveniles mediated by maternal stress hormones in mice. Neural Plasticity , Article 2762518. https://doi.org/10.1155/2016/2762518
Majewska, M. D., Harrison, N. L., Schwartz, R. D., Barker, J. L., & Paul, S. M. (1986). Steroid hormone metabolites are barbiturate-like modulators of the GABA receptor. Science , 232 (4753), 1004−1007. https://doi.org/10.1126/science.2422758
McEvoy, K., & Osborne, L. M. (2019). Allopregnanolone and reproductive psychiatry: An overview. International Review of Psychiatry , 31 (3), 237–244. https://doi.org/10.1080/09540261.2018.1553775
Meltzer-Brody, S., Colquhoun, H., Riesenberg, R., Epperson, C. N., Deligiannidis, K. M., Rubinow, D. R., Li, H., Sankoh, A. J., Clemson, C., Schacterle, A., Jonas, J., & Kanes, S. (2018). Brexanolone injection in post-partum depression: Two multicentre, double-blind, randomised, placebo-controlled, phase 3 trials. The Lancet , 392 (10152), 1058−1070. https://doi.org/10.1016/S0140-6736(18)31551-4
Morrison, K. E., Cole, A. B., Thompson, S. M., & Bale, T. L. (2019). Brexanolone for the treatment of patients with postpartum depression. Drugs Today , 55 (9), 537–544. https://doi.org/10.1358/dot.2019.55.9.3040864
Purdy, R. H., Morrow, A. L., Moore, P. H., & Paul, S. M. (1991). Stress-induced elevations of gamma-aminobutyric acid type A receptor-active steroids in the rat brain. Proceedings of the National Academy of Sciences , 88 (10), 4553−4557. https://doi.org/10.1073/pnas.88.10.4553
Scarff, J. R. (2019). Use of brexanolone for postpartum depression. Innovations in Clinical Neuroscience , 16 (11−12), 32–35.
Schüle, C., Nothdurfter, C., & Rupprecht, R. (2014). The role of allopregnanolone in depression and anxiety. Progress in Neurobiology , 113 , 79−87. https://doi.org/10.1016/j.pneurobio.2013.09.003
Selye, H. (1941). Anesthetic effect of steroid hormones. Experimental Biology and Medicine , 46 (1), 116–121. https://doi.org/10.3181/00379727-46-11907
Shorey, S., Chee, C. Y. I., Ng, E. D., Chan, Y. H., Tam, W. W. S., & Chong, Y. S. (2018). Prevalence and incidence of postpartum depression among healthy mothers: A systematic review and meta-analysis. Journal of Psychiatric Research , 104 , 235–248. https://doi.org/10.1016/j.jpsychires.2018.08.001
Slomian, J., Honvo, G., Emonts, P., Reginster, J. Y., & Bruyère, O. (2019). Consequences of maternal postpartum depression: A systematic review of maternal and infant outcomes. Women's Health , 15 , 1−55. https://doi.org/10.1177/1745506519844044
- Perinatal Depression (NIMH brochure)
- Depression in Women: 4 Things You Should Know (NIMH health topic page)
- Depression (NIMH health topic page)
- Major Depression (NIMH statistics page)
- Women and Mental Health (NIMH health topic page)
- A Bench-to-Bedside Story: The Development of a Treatment for Postpartum Depression (NIMH Director’s Message)
- Bench-to-Bedside: NIMH Research Leading to Brexanolone, First-Ever Drug Specifically for Postpartum Depression (NIIMH press release)
- Population Study Finds Depression Is Different Before, During, and After Pregnancy (NIMH research highlight)
- FDA Approves First Treatment for Post-Partum Depression (FDA news release)
- FDA Approves First Oral Treatment for Postpartum Depression (FDA news release)
- Skip to main content
- Keyboard shortcuts for audio player
- Your Health
- Treatments & Tests
- Health Inc.
- Public Health
Reproductive rights in America
Despite state bans, abortions nationwide are up, driven by telehealth.

Elissa Nadworny

Abortion rights activists at the Supreme Court in Washington, D.C. on March 26, the day the case about the abortion drug mifepristone was heard. The number of abortions in the U.S. increased, a study says, surprising researchers. Drew Angerer/AFP via Getty Images hide caption
Abortion rights activists at the Supreme Court in Washington, D.C. on March 26, the day the case about the abortion drug mifepristone was heard. The number of abortions in the U.S. increased, a study says, surprising researchers.
In the 18 months following the Supreme Court's decision that ended federal protection for abortion, the number of abortions in the U.S. has continued to grow, according to The Society of Family Planning's WeCount project .
"We are seeing a slow and small steady increase in the number of abortions per month and this was completely surprising to us," says Ushma Upadhyay , a professor and public health scientist at the University of California, San Francisco who co-leads the research. According to the report, in 2023 there were, on average, 86,000 abortions per month compared to 2022, where there were about 82,000 abortions per month. "Not huge," says Upadhyay, "but we were expecting a decline."

Shots - Health News
What's at stake in the supreme court mifepristone case.
The slight increase comes despite the fact that 14 states had total abortion bans in place during the time of the research. According to the report, there were about 145,000 fewer abortions in person in those states since the Dobbs decision, which triggered many of the restrictive state laws.
"We know that there are people living in states with bans who are not getting their needed abortions," says Upadhyay. "The concern we have is that that might be overlooked by these increases."
Florida, California and Illinois saw the largest surges in abortions, which is especially interesting given Florida's recent 6-week ban that started on May 1.

Abortion rights opponents demonstrate in New York City, on March 23. Some states' abortion bans are known as "heartbeat bills," because they make abortion illegal after cardiac activity starts, usually around six weeks of pregnancy. Kena Betancur/AFP via Getty Images hide caption
Abortion rights opponents demonstrate in New York City, on March 23. Some states' abortion bans are known as "heartbeat bills," because they make abortion illegal after cardiac activity starts, usually around six weeks of pregnancy.
The latest report also captures for the first time the impact of providers offering telehealth abortions from states with protections for doctors and clinics known as shield laws – statutes that say they can't be prosecuted or held liable for providing abortion care to people from other states.
Between July and December 2023, more than 40,000 people in states with abortion bans and telehealth restrictions received medication abortion through providers in states protected by shield laws. Abortion pills can be prescribed via telehealth appointments and sent through the mail; the pills can safely end pregnancies in the first trimester.
The report includes abortions happening within the U.S. health care system, and does not include self-managed abortions, when people take pills at home without the oversight of a clinician. For that reason, researchers believe these numbers are still an undercount of abortions happening in the U.S.
Tessa Longbons Cox is a senior research associate at Charlotte Lozier Institute, a research organization that opposes abortion. She says the WeCount report, "highlights a concerning trend" that policies around mail-order abortion pills are boosting abortion rates. "By recklessly removing in-person medical visits and safeguards, abortion advocates have put women's health and safety last," Longbons Cox says in a statement.
Accounting for the increases
A major factor in the uptick in abortions nationwide is the rise of telehealth, made possible in part by regulations first loosened during the coronavirus pandemic.
According to the report, telehealth abortions now make up 19% of all abortions in the U.S. In comparison, the first WeCount report which spanned April 2022 through August 2022 showed telehealth abortions accounted for just 4% of all abortions. Research has shown that telehealth abortions are as safe and effective as in-clinic care.
"It's affordable, it's convenient, and it feels more private," says Jillian Barovick, a midwife in Brooklyn and one of the co-founders of Juniper Midwifery , which offers medication abortion via telehealth to patients in six states where abortion is legal. The organization saw its first patient in August 2022 and now treats about 300 patients a month.

A Supreme Court abortion pill case with potential consequences for every other drug
"Having an in-clinic abortion, even a medication abortion, you could potentially be in the clinic for hours, whereas with us you get to sort of bypass all of that," she says. Instead, patients can connect with a clinician using text messages or a secure messaging platform. In addition to charging $100 dollars for the consultation and medication – which is well below the average cost of an abortion – Barovick points to the cost savings of not having to take off work or arrange child care to spend multiple hours in a clinic.
She says her patients receive their medication within 1 to 4 business days, "often faster than you can get an appointment in a clinic."
A study published in JAMA Internal Medicine on Monday followed about 500 women who had medication abortions with the pills distributed via mail order pharmacy after an in-person visit with a doctor. More than 90% of the patients were satisfied with the experience; there were three serious adverse events that required hospitalization.
In addition to expansions in telehealth, there have been new clinics in states like Kansas, Illinois and New Mexico, and there's been an increase in funding for abortion care – fueled by private donors and abortion funds.
The impact of shield laws
During the period from October to December 2023, nearly 8,000 people per month in states with bans or severe restrictions accessed medication abortions from clinicians providing telehealth in the 5 states that had shield laws at the time. That's nearly half of all monthly telehealth abortions.
"It's telemedicine overall that is meeting the need of people who either want to or need to remain in their banned or restricted state for their care," says Angel Foster, who founded The MAP, a group practice operating a telehealth model under Massachusetts' shield laws. "If you want to have your abortion care in your state and you live in Texas or Mississippi or Missouri, right now, the shield law provision is by far the most dominant way that you'd be able to get that care."
Foster's group offers medication abortions for about 500 patients a month. About 90% of their patients are in banned or restrictive states; about a third are from Texas, their most common state of origin, followed by Florida.
"Patients are scared that we are a scam," she says, "they can't believe that we're legit."
Since the WeCount data was collected, additional states including Maine and California have passed shield laws protecting providers who offer care nationwide. The new shield laws circumvent traditional telemedicine laws, which often require out-of-state health providers to be licensed in the states where patients are located. States with abortion bans or restrictions and/or telehealth bans hold the provider at fault, not the patient.

The NPR Politics Podcast
One small pill — one big court case.
Existing lawsuits brought by abortion opponents, including the case awaiting a Supreme Court decision, have the potential to disrupt this telehealth surge by restricting the use of the drug mifepristone nationwide. If the Supreme Court upholds an appeals court ruling, providers would be essentially barred from mailing the drug and an in-person doctor visit would be required.
There is also an effort underway in Louisiana to classify abortion pills as a controlled substance.
- abortion bans
- Abortion rights
New Approach May Help People with Cancer Better Manage Depression, Pain, and Fatigue
May 14, 2024 , by Edward Winstead

In a clinical trial, people with cancer who received cognitive behavioral therapy via telehealth reported improvements in their quality of life.
Many people who are being treated for cancer experience symptoms of depression, pain, and fatigue. But scientists are still studying how best to manage these symptoms in people with cancer.
One approach is to integrate the assessment and treatment of symptoms as a part of routine cancer care. With this approach, people who need support are offered weekly cognitive behavioral therapy sessions from a trained counselor and/or medicine for their symptoms provided by their medical teams.
The strategy, called integrated screening and stepped collaborative care, has now shown promise in a large clinical trial involving people with different types and stages of cancer.
In the NCI-supported study, participants were randomly assigned to receive integrated screening and stepped collaborative care or standard care, which consisted of referring patients to health care providers for treatment.
The stepped collaborative care group had a greater improvement in health-related quality of life, including their emotional, physical, and functional well-being , during the first 6 months of treatment, according to results published March 12 in The Lancet .
The improvement was maintained for up to a year. In addition, participants who received stepped collaborative care also reported reductions in the three most common symptoms.
“Our results highlight the importance of integrating screening and treatment with routine cancer care and offering this at no cost to patients,” said the trial’s lead researcher, Jennifer Steel, Ph.D., a clinical health psychologist at the University of Pittsburgh Medical Center (UPMC).
“We need to revisit our current approach of screening patients for symptoms and referring them for treatment,” Dr. Steel said. “Our hope is that this research could lead to a shift in care that improves patient quality of life.”
Getting started with treatment for symptoms
The study occurred during the pandemic, and the stepped collaborative care intervention was delivered via telehealth. The trained counselors worked closely with the cancer care team to manage people’s symptoms.
With standard care, people being treated for cancer are screened for symptoms of depression, pain, and fatigue. Those who need treatment for these symptoms are referred to a specialist within or outside their health care facilities. Patients then follow up to arrange an appointment and may be responsible for some or all the treatment costs.
But this approach often fails to give people the full support they need, the researchers noted. Just getting started can be a challenge. By contrast, offering patients an integrated approach to screening for the symptoms and automated referral to receive stepped collaborative care increases the likelihood that they will begin treatment, Dr. Steel said.
In the trial, about 75% of the patients who were offered support began treatment with a trained counselor, compared with only about 4% of the patients in the standard treatment group.
Some of the participants in the stepped collaborative group said they were willing to try the therapy because it was free and part of their routine cancer care.
Being invited to participate in therapy was “helpful,” one participant said. The counselor “walks you through the process and knows your doctor,” the person added. “That makes you feel comfortable because you’re already scared to death.”
Another participant said, “Being reached out to absolutely influenced my decision” to receive treatment.
Reducing the use of health care resources
The trial included 459 people being treated for cancer who had certain levels of depression, pain, or fatigue (or all of these). They were treated at one of 29 cancer outpatient clinics affiliated with UPMC. The vast majority of participants were White and over age 60.
The researchers randomly assigned participants to receive stepped collaborative care or standard care, which included referring patients who showed evidence of depression, pain, or fatigue on screening to a health care professional.
In the stepped collaborative care group, participants were contacted to begin cognitive behavioral therapy for an hour once a week through telehealth. Patients received 8 to 12 sessions initially but could continue therapy for up to 6 months if needed. Medicine for depression, pain, and fatigue was also available if the patient preferred or did not respond to cognitive behavioral therapy.
After a median follow-up of 6 months, people in the stepped collaborative care group had clinically meaningful improvements in emotional, functional, and physical well-being, whereas those in the standard treatment group didn’t. The improvements lasted up to 1 year, which is how long the participants were followed.
In addition, people in the stepped collaborative care group had fewer emergency room visits, fewer hospital readmissions within 90 days, and shorter hospital stays than the standard care group.
Dr. Steel noted that reducing the use of health care resources might be important for patients. Fewer hospitalizations and emergency room visits “could lower cancer care costs to the patient, as well as stress associated with those visits for both the patient and the family,” she said.
“The trial highlights what can be achieved using telehealth,” said Paige A. Green, Ph.D., a health psychologist and behavioral medicine researcher in NCI’s Division of Cancer Control and Population Sciences who was not involved in the trial.
Dr. Green called the findings “promising” but noted that the trial had limitations, such as a study population that was more than 90% White.
“The lack of meaningful inclusion of patient populations that are often underrepresented in cancer research might limit the relevance of the study findings to those groups,” said Dr. Green.
How is cognitive behavior therapy used to manage symptoms?
The trial participants who underwent cognitive behavioral therapy were taught strategies to deal with their symptoms, including relaxation techniques and ways to alter core beliefs about themselves and their environment.
Participants who were experiencing pain and fatigue were taught strategies to positively affect their thinking, improve sleep hygiene, and increase physical activity.
With stepped care, health care providers continually monitor a person’s response to treatment until the symptoms are adequately addressed.
“If the person were not responding, the providers could ‘step up’ the care by increasing the frequency or the intensity of the treatment they were providing or by trying another treatment approach,” Dr. Steel explained.
Cost savings from stepped collaborative care
According to the researchers, if health care systems offered an integrated screening and treatment program at no cost to the patient, such systems would save about $16,000 per patient per year. Their estimate was based on the savings from shorter hospital stays, fewer emergency room visits, and fewer 90-day readmissions.
“This study is an important contribution” to the data on stepped collaborative care as part of cancer treatment, said Barbara L. Andersen, Ph.D., a clinical psychologist who studies biobehavioral aspects of cancer at The Ohio State University.
“The inclusion of cost data, I hope, will significantly strengthen the case for [providing] psychological care for patients in need,” added Dr. Andersen, who is also a member of an expert panel on the management of anxiety and depression in adult survivors of cancer .
For some participants in the trial, receiving mental health support at no cost played a role in their decisions to try cognitive behavioral therapy. One participant said cost was “a very big factor.”
“Seniors my age are on a budget,” the person explained. The cost of talking with a therapist on the phone “is the number one thing that anybody’s going to look at, especially if they’re 65 or older.”
Testing stepped collaborative care in up to 100 cancer clinics
For the study, Dr. Steel and her colleagues screened nearly 1,600 patients. Only 481 (30%) did not report any of the three symptoms targeted by the intervention.
Susanne Oksbjerg Dalton, Ph.D., and Christoffer Johansen, M.D., Ph.D., of Copenhagen University wrote in an accompanying editorial that the finding highlights the need to scale up collaborative care for nearly all people with cancer.
“Such a high symptom prevalence in patients treated for cancer seems overwhelming, but this underpins the negative effect of treatment on patient quality of life,” they wrote.
Dr. Steel and her colleagues are planning to develop a training institute to prepare mental health professionals to deliver the intervention. They are also planning a clinical trial to evaluate the new approach in nearly 100 clinics at UPMC Hillman Cancer Center.
Featured Posts
March 27, 2024, by Edward Winstead
March 21, 2024, by Elia Ben-Ari
March 5, 2024, by Carmen Phillips
- Biology of Cancer
- Cancer Risk
- Childhood Cancer
- Clinical Trial Results
- Disparities
- FDA Approvals
- Global Health
- Leadership & Expert Views
- Screening & Early Detection
- Survivorship & Supportive Care
- February (6)
- January (6)
- December (7)
- November (6)
- October (7)
- September (7)
- February (7)
- November (7)
- October (5)
- September (6)
- November (4)
- September (9)
- February (5)
- October (8)
- January (7)
- December (6)
- September (8)
- February (9)
- December (9)
- November (9)
- October (9)
- September (11)
- February (11)
- January (10)
A .gov website belongs to an official government organization in the United States.
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Preventing Chronic Diseases: What You Can Do Now
- Living with a Chronic Condition
- Chronic Disease Data
- Community Health Workers
- Workgroup on Translation Tools
- National Center for Chronic Disease Prevention and Health Promotion (NCCDPHP)
Fast Facts: Health and Economic Costs of Chronic Conditions
At a glance.
Chronic diseases account for most illness, disability, and deaths in the United States and are the leading drivers of health care costs.

The impact of chronic diseases in America
Ninety percent of the nation's $4.5 trillion in annual health care expenditures are for people with chronic and mental health conditions. 1 2 Interventions to prevent and manage these diseases have significant health and economic benefits .
Heart disease and stroke
Nothing kills more Americans than heart disease and stroke . More than 934,500 Americans die of heart disease or stroke every year—that's more than 1 in 4 deaths. 3 These diseases take an economic toll, as well, costing our health care system $251 billion per year and causing $156 billion in lost productivity on the job. Costs from cardiovascular diseases are projected to top $1 trillion by 2035. 3
See the health and economic benefits of high blood pressure interventions .
Each year in the United States, 1.7 million people are diagnosed with cancer , and more than 600,000 die from it, making it the second leading cause of death. The cost of cancer care continues to rise and is expected to reach more than $240 billion by 2030. 4
See the health and economic benefits of interventions for breast cancer , cervical cancer , colorectal cancer , and skin cancer .
More than 38 million Americans have diabetes , and another 98 million adults in the United States have prediabetes, which puts them at risk for type 2 diabetes. Diabetes can cause serious complications, including heart disease, kidney failure, and blindness. In 2022, the total estimated cost of diagnosed diabetes was $413 billion in medical costs and lost productivity. 5
See the health and economic benefits of diabetes interventions .
Obesity affects 20% of children and 42% of adults, putting them at risk of chronic diseases such as type 2 diabetes, heart disease, and some cancers. Over 25% of young people aged 17 to 24 are too heavy to join the U.S. military. Obesity costs the U.S. health care system nearly $173 billion a year. 6
Arthritis affects 53.2 million adults in the United States, which is about 1 in 5 adults. 7 It is a leading cause of work disability in the United States, one of the most common chronic conditions, and a leading cause of chronic pain. Arthritis costs appear to be increasing and were estimated at over $600 billion in 2019. 8 9
Alzheimer's disease
Alzheimer's disease , a type of dementia, is an irreversible, progressive brain disease that affects nearly 7 million Americans, including 1 in 9 adults aged 65 and older. Two-thirds of these older adults (4.1 million) are women. Deaths due to Alzheimer's disease more than doubled between 2000 and 2019, increasing 145%. The cost of caring for people with Alzheimer's and other dementias was an estimated $345 billion in 2023, with projected increases to nearly $1 trillion (in today's dollars) by 2050. 10
In the United States, about 3 million adults and about half a million children and teens younger than 18 have active epilepsy —meaning that they have been diagnosed by a doctor, had a recent seizure, or both. Adults with epilepsy report worse mental health, more cognitive impairment, and barriers in social participation compared to adults without epilepsy. In 2019, total health care costs (epilepsy-attributable and other health-related costs) for noninstitutionalized people with epilepsy was $13.4 billion, of which $5.4 billion were directly attributable to epilepsy. 11
Tooth decay
Cavities (also called tooth decay) are one of the most common chronic diseases in the United States. One in six children aged 6 to 11 years and 1 in 4 adults have untreated cavities. Untreated cavities can cause pain and infections that may lead to problems eating, speaking, and learning. On average, 34 million school hours are lost each year because of unplanned (emergency) dental care, and almost $46 billion is lost in productivity due to dental disease. 12 13
See the health and economic benefits of oral disease interventions .
Risk Factors
Cigarette smoking.
Cigarette smoking is the leading cause of preventable death and disease in the United States. More than 16 million Americans have at least one disease caused by smoking. This amounts to more than $240 billion in health care spending that could be reduced every year if we could prevent young people from starting to smoke and help every person who smokes quit. 14
See the health and economic benefits of tobacco use interventions .
Physical inactivity
Not getting enough physical activity comes with high health and financial costs. It can lead to heart disease, type 2 diabetes, some cancers, and obesity. 15 Physical inactivity also costs the nation $117 billion a year for related health care. 16
Excessive alcohol use
Excessive alcohol use is responsible for 140,000 deaths in the United States each year, including 1 in 5 deaths among adults aged 20 to 49 years. 17 18 Binge drinking is responsible for over 40% these deaths. 17 In 2010, excessive alcohol use cost the U.S. economy $249 billion, or $2.05 a drink, and $2 of every $5 of these costs were paid by the public. 19 Three-quarters of these costs were due to binge drinking.
- Buttorff C, Ruder T, Bauman M. Multiple Chronic Conditions in the United States . Rand Corp.; 2017.
- National health expenditure data: historical. Center for Medicare & Medicaid Services. Updated December 13, 2023. Accessed February 6, 2024. https://www.cms.gov/data-research/statistics-trends-and-reports/national-health-expenditure-data/historical
- Centers for Disease Control and Prevention, National Center for Health Statistics. Multiple Cause of Death 1999–2019 on CDC WONDER Online Database website. http://wonder.cdc.gov/mcd-icd10.html . Accessed February 1, 2023.
- Mariotto AB, Enewold L, Zhao J, Zeruto CA, Yabroff KR. Medical care costs associated with cancer survivorship in the United States. Cancer Epidemiol Biomarkers Prev. 2020;29:1304–1312.
- Parker ED, Lin J, Mahoney T, et al. Economic costs of diabetes in the U.S. in 2022. Diabetes Care. 2023. doi: 10.2337/dci23-0085
- Ward ZJ, Bleich SN, Long MW, Gortmaker SL. Association of body mass index with health care expenditures in the United States by age and sex. PLoS One . 2021;16(3):e0247307.
- Fallon EA, Boring MA, Foster AL, et al. Prevalence of diagnosed arthritis—United States, 2019–2021. MMWR Morb Mortal Wkly Rep . 2023;72:1101–1107.
- Murphy LB, Cisternas MG, Pasta DJ, Helmick CG, Yelin EH. Medical expenditures and earnings losses among US adults with arthritis in 2013. Arthritis Care Res (Hoboken) . 2018;70(6):869–876.
- Lo J, Chan L, Flynn S. A systematic review of the incidence, prevalence, costs, and activity and work limitations of amputation, osteoarthritis, rheumatoid arthritis, back pain, multiple sclerosis, spinal cord injury, stroke, and traumatic brain injury in the United States: a 2019 Update. Arch Phys Med Rehabil . 2021;102(1):115–131.
- Alzheimer's Association. 2023 Alzheimer's disease facts and figures. Alzheimers Dement . 2023;19(4).
- Moura LMVR, Karakis I, Zack MM, Tian N, Kobau R, Howard D. Drivers of US health care spending for persons with seizures and/or epilepsies, 2010-2018. Epilepsia . 2022;63(8):2144–2154.
- Righolt AJ, Jevdjevic M, Marcenes W Listl S. Global-, regional-, and country-level economic impacts of dental diseases. J Dent Res. 2018;97(5):501–507.
- Naavaal S, Kelekar U. Hours lost due to planned and unplanned dental visits among US adults. Health Behav Policy Rev. 2018;5(2):66–73.
- Xu X, Shrestha SS, Trivers KF, Neff L, Armour BS, King BA. U.S. healthcare spending attributable to cigarette smoking in 2014. Prev Med . 2021;150:106529.
- U.S. Department of Health and Human Services. Step It Up! The Surgeon General's Call to Action to Promote Walking and Walkable Communities . Office of the Surgeon General; 2015.
- Carlson SA, Fulton JE, Pratt M, Yang Z, Adams EK. Inadequate physical activity and health care expenditures in the United States . Prog Cardiovasc Dis . 2015;57:315–323.
- Centers for Disease Control and Prevention (CDC). Alcohol-Related Disease Impact (ARDI).
- Esser MB, Leung G, Sherk A, et al. Estimated deaths attributable to excessive alcohol use among US adults aged 20 to 64 years, 2015 to 2019. JAMA Netw Open . 2022;5(11):e2239485. doi: 10.1001/jamanetworkopen.2022.39485
- Sacks JJ, Gonzales KR, Bouchery EE, Tomedi LE, Brewer RD. 2010 national and state costs of excessive alcohol consumption. Am J Prev Med 2015;49(5):e73–e79.
Chronic Disease
Prevalence, costs, risks, prevention, and management of chronic diseases in the United States
For Everyone
Public health.

IMAGES
VIDEO
COMMENTS
10 careers in medical research Here are 10 careers you can pursue in the field of medical research: 1. Clinical laboratory scientist National average salary: $89,291 per year Primary duties: A clinical laboratory scientist is a scientist who specializes in using lab equipment to perform tests on biological specimens. This can involve extracting and testing bodily fluids to look for diseases or ...
Check out details about more than 40 jobs in healthcare and medicine, with trusted information from Mayo Clinic College of Medicine and Science. Career. Work type. Median salary. Higher education required. Athletic trainer. Patient care. $48,000. 4-6 years.
Research. To improve health care and offer new solutions and hope for patients, Mayo Clinic conducts basic, translational, clinical and epidemiological research at its campuses in Arizona, Florida and Minnesota and throughout Mayo Clinic Health System. Researchers investigate today's medical mysteries, generating new knowledge and translating ...
Health care in the United States has improved markedly over the past five decades, in large measure because of the advances in health research that have been supported by a myriad of federal agencies, industry, the private nonprofit sector, and research institutions. Diverse teams of scientists composed of basic scientists, physicians, nurses, dentists, pharmacists, and other health ...
Make Caring Your Career™. ExploreHealthCareers.org is a collaboration between today's health professionals and. leading health care associations designed to help people like you start down the road. toward a career in health. Here you'll find the latest health career information and tools to. guide you as you prepare for a future in ...
People entering the public health research field can expect rewarding work. The job outlook for these positions is promising. According to the U.S. Bureau of Labor Statistics (BLS), the number of public health research positions is projected to grow 8 percent by 2028. The median public health researcher salary was $88,790 in May 2019.
About our work at AHRQ. The Agency for Healthcare Research and Quality's (AHRQ) mission is to produce evidence to make health care safer, higher quality, more accessible, equitable, and affordable, and to work within the U.S. Department of Health and Human Services and with other partners to make sure that the evidence is understood and used.
There are so many other career opportunities in the health sciences. And here at Mayo Clinic, there's actually over 60 programs in the allied health sciences that exist, and allow students to pursue these opportunities and really be part of active patient care. Martha-Gracia Knuttinen, M.D., Ph.D. Associate Dean of Admissions, Diversity, Equity ...
Information on career opportunities at AHRQ and how to apply. Join the team that strives to improve healthcare for all Americans by: Investing in health systems research that generates evidence about how to deliver high-quality, safe, high-value healthcare.; Creating tools and strategies for health systems and frontline clinicians to support practice improvement.
Lewiston, ME 04240. $22 - $27 an hour. Full-time. 8 hour shift. Easily apply. We provide ongoing learning and training with up to date dental techniques and research. Full-Time 4 days/week - 9-hour shift (7:30am-5:30pm)*. Active 2 days ago. View similar jobs with this employer.
Behavioral Health Services Coding Research Specialist 14 - BPHASA - Hybrid. Departmental Analyst (Trainee) 9-12. Hybrid work in Lansing, MI. $5,219.20 - $7,784.00 a month. Full-time. Salary $2,609.60 - $3,892.00 Biweekly Location Lansing, MI Job Type Permanent Full Time Job Number 3901-24-BPHASA-SBHS-063-FILL Department Health and….
Working at CDC. Whether your background is in medicine, health care, research, or operations, you can help fight diseases and epidemics to make our nation, and the world, a better place for all to live and thrive. Saving lives and protecting people around the world—that's what CDC is all about. Learn More.
Health research entails systematic collection or analysis of data with the intent to develop generalizable knowledge to understand health challenges and mount an improved response to them. The full spectrum of health research spans five generic areas of activity: measuring the health problem; understanding its cause(s); elaborating solutions; translating the solutions or evidence into policy ...
Nurses are employed in hospitals, medical clinics, schools, nursing homes, and home health agencies. Becoming a nurse. All paths to becoming a nurse require post-secondary education. Candidates for careers in nursing should be comfortable working closely with people from diverse backgrounds and should be motivated to help sick patients feel better.
Official website of the National Institutes of Health (NIH). NIH is one of the world's foremost medical research centers. An agency of the U.S. Department of Health and Human Services, the NIH is the Federal focal point for health and medical research. The NIH website offers health information for the public, scientists, researchers, medical professionals, patients, educators,
Opportunities at NIMH. There are a wide range of opportunities available at NIMH. Extramural Research Program (ERP) careers are scientific research positions that support research grants and contracts across the country through the extramural research programs.. Intramural Research Program (IRP) careers are scientific research or clinical positions in the internal research division of NIMH ...
The Importance of Health Research. Like privacy, health research has high value to society. It can provide important information about disease trends and risk factors, outcomes of treatment or public health interventions, functional abilities, patterns of care, and health care costs and use.
The Centers for Disease Control and Prevention works 24/7 to provide the American public with timely and accurate health information, responding to public health emergencies and natural disasters, and monitoring the spread of dangerous and life-threatening diseases. Last Reviewed: May 21, 2024. Source: Centers for Disease Control and Prevention.
The U.S. Bureau of Labor Statistics projects 1.8 million job openings per year in healthcare through 2032. Even before the pandemic hit, the field of public health had been experiencing explosive ...
ABOUT ACADEMIC/RESEARCH JOBS IN PUBLIC HEALTH Apply Online for Academic/Research Jobs in Public Health and join us in our efforts to protect and promote the health and well-being of all patient communities across the US and its territories. When you choose a Public Health career in an Academic/Research job, you have the ability to truly impact ...
The University of Texas Health Science Center at San Antonio, also called UT Health San Antonio, is a leading academic health center with a mission to make lives better through excellence in advanced academics, life-saving research and comprehensive clinical care including health, dental and cancer services.
New roles at Microsoft Research. Microsoft Research provides a dynamic environment for research careers with a network of world-class research labs led by globally-recognized research scientists and engineers. Our researchers and engineers pursue innovation in a range of scientific and technical disciplines, to help solve complex challenges in ...
Neglecting sex and gender in research is a public-health risk. The data are clear: taking sex and gender into account in research and using that knowledge to change health care could benefit ...
Chemical engineer: $92,214 per year 42. Clinical psychologist: $109,754 per year 43. Data scientist: $123,493 per year 44. Data engineer: $126,425 per year. Explore 44 science and research jobs, read about the average salary information for each role and examine a brief job description for many of the positions.
About University of Utah Health. University of Utah Health is the state's only academic health care system, providing leading-edge and compassionate care for a referral area that encompasses 10% of the U.S., including Idaho, Wyoming, Montana and much of Nevada. A hub for health sciences research and education in the region, U of U Health has a $428 million research enterprise and trains the ...
Learn about NIMH priority areas for research and funding that have the potential to improve mental health care over the short, medium, and long term. Resources for Researchers Information about resources such as data, tissue, model organisms and imaging resources to support the NIMH research community.
The report includes abortions happening within the U.S. health care system, and does not include self-managed abortions, when people take pills at home without the oversight of a clinician ...
Stepped collaborative care is an approach for managing symptoms such as depression, pain, and fatigue in people with cancer. It includes psychotherapy and medication if the symptoms are not reduced by psychotherapy alone. A person's symptoms are assessed every 4 weeks. If the symptoms are not in the normal range, health care providers change ...
The independent source for health policy research, polling, and news. menu ... In 2024, Affordable Care Act (ACA) Marketplace enrollment hit a new record high, reaching over 21 million people ...
More than 934,500 Americans die of heart disease or stroke every year—that's more than 1 in 4 deaths. 3 These diseases take an economic toll, as well, costing our health care system $251 billion per year and causing $156 billion in lost productivity on the job. Costs from cardiovascular diseases are projected to top $1 trillion by 2035. 3.