- Undergraduate
- High School
- Architecture
- American History
- Asian History
- Antique Literature
- American Literature
- Asian Literature
- Classic English Literature
- World Literature
- Creative Writing
- Linguistics
- Criminal Justice
- Legal Issues
- Anthropology
- Archaeology
- Political Science
- World Affairs
- African-American Studies
- East European Studies
- Latin-American Studies
- Native-American Studies
- West European Studies
- Family and Consumer Science
- Social Issues
- Women and Gender Studies
- Social Work
- Natural Sciences
- Pharmacology
- Earth science
- Agriculture
- Agricultural Studies
- Computer Science
- IT Management
- Mathematics
- Investments
- Engineering and Technology
- Engineering
- Aeronautics
- Medicine and Health
- Alternative Medicine
- Communications and Media
- Advertising
- Communication Strategies
- Public Relations
- Educational Theories
- Teacher's Career
- Chicago/Turabian
- Company Analysis
- Education Theories
- Shakespeare
- Canadian Studies
- Food Safety
- Relation of Global Warming and Extreme Weather Condition
- Movie Review
- Admission Essay
- Annotated Bibliography
- Application Essay
Article Critique
- Article Review
- Article Writing
- Book Review
- Business Plan
- Business Proposal
- Capstone Project
- Cover Letter
- Creative Essay
- Dissertation
- Dissertation - Abstract
- Dissertation - Conclusion
- Dissertation - Discussion
- Dissertation - Hypothesis
- Dissertation - Introduction
- Dissertation - Literature
- Dissertation - Methodology
- Dissertation - Results
- GCSE Coursework
- Grant Proposal
- Marketing Plan
- Multiple Choice Quiz
- Personal Statement
- Power Point Presentation
- Power Point Presentation With Speaker Notes
- Questionnaire
- Reaction Paper
Research Paper
- Research Proposal
- SWOT analysis
- Thesis Paper
- Online Quiz
- Literature Review
- Movie Analysis
- Statistics problem
- Math Problem
- All papers examples
- How It Works
- Money Back Policy
- Terms of Use
- Privacy Policy
- We Are Hiring

Health Care in the United States, Essay Example
Pages: 4
Words: 1013
Hire a Writer for Custom Essay
Use 10% Off Discount: "custom10" in 1 Click 👇
You are free to use it as an inspiration or a source for your own work.
In the United States, there has long been discussion about the quality and nature of the delivery of healthcare. The debates have included who may receive such services, whether or not healthcare is a privilege or an entitlement, whether and how to make patient care affordable to all segments of the population, and the ways in which the government should, or should not, be involved in the provision of such services. Indeed, many people feel that the healthcare in this country is the best in the world; others believe tha (The Free Dictionary)t our health delivery system is broken. This paper shall examine different aspects of the healthcare system in our country, discussing whether it has been successful in providing essential services to American citizens.
The delivery of healthcare services is considered to be a system; according to the Free Diction- ary (Farlex, 2010), a system is defined as “a group of interacting, interrelated, or interdependent elements forming a complex whole.” This is an apt description of our healthcare structure, as it is compiled of patients, medical and mental health providers, hospitals, clinics, laboratories, insurance companies, and many other parties that are reliant on each other and that, when combined, make up the entity known as our healthcare system.
Those who believe that our healthcare system is the best in the world often point to the fact that leaders as well as private citizens from countries throughout the world frequently come to the United States to have surgeries and other treatments that they require for survival. A more cynical view of this phenomenon is that if people have the money, they are able to purchase quality care in the U.S., a “survival of the fittest” situation. Those who lack the resources to travel to the U.S. for medical treatment are simply out of luck, and often will die without the needed care.
In fact, reports by the World Health Organization and other groups consistently indicate that while the United States spends more than any other country on healthcare costs, Americans receive lower quality, less efficient and less fairness from the system. These conclusions come as a result of studying quality of care, access to care, equity and the ability to lead long, productive lives. (World Health Organization,2001.) What cannot be disputed is that the cost of healthcare is constantly rising, a fact which was the precipitant to the large movement to reform healthcare in our country in 2010. More than 10 years ago, the goal of managed care was to drive down the costs of healthcare, but those promises did not materialize (Garsten, 2010.) A large segment of the population is either uninsured or underinsured, and it is speculated that over the next decade, these problems will only increase while other difficulties will arise (Garson, 2010.)
When examining the healthcare system, there are three aspects of care that call for evaluation: the impact of delivering care on the patient, the benefits and harms of that treatment, and the functioning of the healthcare system, as described in an article by Adrian Levy. Levy argues that each of these outcomes should be assessed and should include both the successes and the limitations of each aspect. The idea is that there should be operational measurements of patients’ interactions with the healthcare system that would include patients’ experiences in hospitals, using measurements of their functional abilities and their qualities of life following discharge. The results of patients’ interactions with the healthcare system should be utilized to develop and improve the delivery of healthcare treatment, as well as to develop policy changes that would affect the entire field of healthcare in the United States.
One view of the state of American healthcare is that the system is fragmented; there have been many failed attempts by several presidents to introduce the idea of universal healthcare. Instead, American citizens are saddled with a system in which government pays either directly or indirectly for over 50% of the healthcare in our country, but the actual delivery of insurance and of care is undertaken by an assortment of private insurers, for-profit hospitals, and other parties who raise costs without increasing quality of service (Wells, Krugman, 2006.) If the United States were to switch to a single-payer system such as that provided in Canada, the government would directly provide insurance which would most likely be less expensive and provide better results than our current system.
It is clear that throwing money at a problem does not necessarily resolve it; the fact that the United States spends more than twice as much on healthcare provision as any other country in the world only makes it more ironic that when it comes to evaluating the service, Americans fall appallingly flat. In my opinion, if the new healthcare reform bill had included a public option which would have taken the profit margin out of the equation, the nation and its citizens would have been in a much better position to receive quality healthcare. The fact that people die every day from preventable illnesses and conditions simply because they do not have affordable insurance is a national disgrace. In addition, many of the people who have been the most adamantly against government “intrusion” into their healthcare are actually on Medicaid or Medicare, federally-funded programs. Their lack of understanding of what the debate actually involves is striking, and they are rallying against what is in their own best interests. These are people that equate Federal involvement in healthcare as socialism. Unless and until our healthcare system is able to provide what is needed to all of its citizens, all claims that we have the best healthcare system in the world are, sadly, utterly hollow.
Adrian R Levy (2005, December). Categorizing outcomes of Health Care delivery. Clinical and investigative medicine, pp. 347-351.
Arthur Garson (2000). The U.S. Healthcare System 2010: Problems Principles and Potential Solutions. Retrieved July 3, 2010, from Circulation: The Journal of the American Heart Association: http://circ.ahajournals.org/cgi/reprint/101/16/2015
The Free Dictionary. (n.d.). Farlex. Retrieved July 3, 2010. http://www.thefreedictionary.com/system
World Health Organization. (2003, July). WHO World Health Report 2000. Retrieved July 3, 2010, from State of World Health: http://faculty.washington.edu/ely/Report2000.htm
Stuck with your Essay?
Get in touch with one of our experts for instant help!
Using Learning Journals in Continuing and Higher Education, Article Critique Example
Prolonged Exposure Therapy, Research Paper Example
Time is precious
don’t waste it!
Plagiarism-free guarantee
Privacy guarantee
Secure checkout
Money back guarantee

Related Essay Samples & Examples
Voting as a civic responsibility, essay example.
Pages: 1
Words: 287
Utilitarianism and Its Applications, Essay Example
Words: 356
The Age-Related Changes of the Older Person, Essay Example
Pages: 2
Words: 448
The Problems ESOL Teachers Face, Essay Example
Pages: 8
Words: 2293
Should English Be the Primary Language? Essay Example
Words: 999
The Term “Social Construction of Reality”, Essay Example
Words: 371
Suggestions or feedback?
MIT News | Massachusetts Institute of Technology
- Machine learning
- Social justice
- Black holes
- Classes and programs
Departments
- Aeronautics and Astronautics
- Brain and Cognitive Sciences
- Architecture
- Political Science
- Mechanical Engineering
Centers, Labs, & Programs
- Abdul Latif Jameel Poverty Action Lab (J-PAL)
- Picower Institute for Learning and Memory
- Lincoln Laboratory
- School of Architecture + Planning
- School of Engineering
- School of Humanities, Arts, and Social Sciences
- Sloan School of Management
- School of Science
- MIT Schwarzman College of Computing
What has the pandemic revealed about the US health care system — and what needs to change?
Press contact :.

Previous image Next image
With vaccinations for Covid-19 now underway across the nation, MIT SHASS Communications asked seven MIT scholars engaged in health and health care research to share their views on what the pandemic has revealed about the U.S. health care system — and what needs to change. Representing the fields of medicine, anthropology, political science, health economics, science writing, and medical humanities, these researchers articulate a range of opportunities for U.S. health care to become more equitable, more effective and coherent, and more prepared for the next pandemic.
Dwaipayan Banerjee , associate professor of science, technology, and society
On the heels of Ebola, Covid-19 put to rest a persistent, false binary between diseases of the rich and diseases of the poor. For several decades, health care policymakers have labored under the impression of a great epidemiological transition. This theory holds that the developed world has reached a stage in its history that it no longer needs to worry about communicable diseases. These "diseases of the poor" are only supposed to exist in distant places with weak governments and struggling economies. Not here in the United States.
On the surface, Covid-19 made clear that diseases do not respect national boundaries. More subtly, it tested the hypothesis that the global north no longer need concern itself with communicable disease. And in so doing, it undermined our assumptions about global north health-care infrastructures as paradigmatically more evolved. Over the last decades, the United States has been focused on developing increasingly sophisticated drugs. While this effort has ushered in several technological breakthroughs, a preoccupation with magic-bullet cures has distracted from public health fundamentals. The spread of the virus revealed shortages in basic equipment and hospitals beds, the disproportionate effects of disease on the marginalized, the challenge of prevention rather than cure, the limits of insurance-based models to provide equitable care, and our unacknowledged dependence on the labor of underpaid health care workers.
To put it plainly, the pandemic did not create a crisis in U.S. health care. For many in the United States, crisis was already a precondition of care, delivered in emergency rooms and negotiated through denied insurance claims. As we begin to imagine a "new normal," we must ask questions about the old. The pandemic made clear that the "normal" had been a privilege only for a few well-insured citizens. In its wake, can we imagine a health-care system that properly compensates labor and recognizes health care as a right, rather than a privilege only available to the marginalized when an endemic crisis is magnified by a pandemic emergency?
Andrea Campbell , professor of political science
No doubt, the pandemic reveals the dire need to invest in public-health infrastructure to better monitor and address public-health threats in the future, and to expand insurance coverage and health care access. To my mind, however, the pandemic’s greatest significance is in revealing the racism woven into American social and economic policy.
Public policies helped create geographic and occupational segregation to begin with; inadequate racist and classist public policies do a poor job of mitigating their effects. Structural racism manifests at the individual level, with people of color suffering worse housing and exposure to toxins, less access to education and jobs, greater financial instability, poorer physical and mental health, and higher infant mortality and shorter lifespans than their white counterparts. Residential segregation means many white Americans do not see these harms.
Structural racism also materializes at the societal level, a colossal waste of human capital that undercuts the nation’s economic growth, as social and economic policy expert Heather McGhee shows in her illuminating book, "The Sum of Us." These society-wide costs are hidden as well; it is difficult to comprehend the counterfactual of what growth would look like if all Americans could prosper. My hope is that the pandemic renders this structural inequality visible. There is little point in improving medical or public-health systems if we fail to address the structural drivers of poor health. We must seize the opportunity to improve housing, nutrition, and schools; to enforce regulations on workplace safety, redlining, and environmental hazards; and to implement paid sick leave and paid family leave, among other changes. It has been too easy for healthy, financially stable, often white Americans to think the vulnerable are residual. The pandemic has revealed that they are in fact central. It’s time to invest for a more equitable future.
Jonathan Gruber , Ford Professor of Economics
The Covid-19 pandemic is the single most important health event of the past 100 years, and as such has enormous implications for our health care system. Most significantly, it highlights the importance of universal, non-discriminatory health insurance coverage in the United States. The primary source of health insurance for Americans is their job, and with unemployment reaching its highest level since the Great Depression, tens of millions of workers lost, at least temporarily, their insurance coverage.
Moreover, even once the economy recovers, millions of Americans will have a new preexisting condition, Covid-19. That’s why it is critical to build on the initial successes of the Affordable Care Act to continue to move toward a safety net that provides insurance options for all without discrimination.
The pandemic has also illustrated the power of remote health care. The vast majority of patients in the United States have had their first experience with telehealth during the pandemic and found it surprisingly satisfactory. More use of telehealth can lead to increased efficiency of health care delivery as well as allowing our system to reach underserved areas more effectively.
The pandemic also showed us the value of government sponsorship of innovation in the health sciences. The speed with which the vaccines were developed is breathtaking. But it would not have been possible without decades of National Institute of Health investments such as the Human Genome Project, nor without the large incentives put in place by Operation Warp Speed. Even in peacetime, the government has a critical role to play in promoting health care innovation
The single most important change that we need to make to be prepared for the next pandemic is to recognize that proper preparation is, by definition, overpreparation. Unless we are prepared for the next pandemic that doesn’t happen, we won’t possibly be ready for the next pandemic that does.
This means working now, while the memory is fresh, to set up permanent, mandatorily funded institutions to do global disease surveillance, extensive testing of any at-risk populations when new diseases are detected, and a permanent government effort to finance underdeveloped vaccines and therapeutics.
Jeffrey Harris , professor emeritus of economics and a practicing physician The pandemic has revealed the American health care system to be a non-system. In a genuine system, health care providers would coordinate their services. Yet when Elmhurst Hospital in Queens was overrun with patients, some 3,500 beds remained available in other New York hospitals. In a genuine system, everyone would have a stable source of care at a health maintenance organization (HMO). While our country has struggled to distribute the Covid-19 vaccine efficiently and equitably, Israel, which has just such an HMO-based system, has broken world records for vaccination.
Germany, which has all along had a robust public health care system, was accepting sick patients from Italy, Spain, and France. Meanwhile, U.S. hospitals were in financial shock and fee-for-service-based physician practices were devastated. We need to move toward a genuine health care system that can withstand shocks like the Covid-19 pandemic. There are already models out there to imitate. We need to strengthen our worldwide pandemic and global health crisis alert systems. Despite concerns about China’s early attempts to suppress the bad news about Covid-19, the world was lucky that Chinese investigators posted the full genome of SARS-CoV-2 in January 2020 — the singular event that triggered the search for a vaccine. With the recurrent threat of yet another pandemic — after H1N1, SARS, MERS, Ebola, and now SARS-Cov-2 — along with the anticipated health consequences of global climate change, we can’t simply cross our fingers and hope to get lucky again.
Erica Caple James , associate professor of medical anthropology and urban studies The coronavirus pandemic has revealed some of the limits of the American medical and health care system and demonstrated many of the social determinants of health. Neither the risks of infection nor the probability of suffering severe illness are equal across populations. Each depends on socioeconomic factors such as type of employment, mode of transportation, housing status, environmental vulnerability, and capacity to prevent spatial exposure, as well as “preexisting” health conditions like diabetes, obesity, and chronic respiratory illness.
Such conditions are often determined by race, ethnicity, gender, and “biology,” but also poverty, cultural and linguistic facility, health literacy, and legal status. In terms of mapping the prevalence of infection, it can be difficult to trace contacts among persons who are regular users of medical infrastructure. However, it can be extraordinarily difficult to do so among persons who lack or fear such visibility, especially when a lack of trust can color patient-clinician relationships.
One’s treatment within medical and health care systems may also reflect other health disparities — such as when clinicians discount patient symptom reports because of sociocultural, racial, or gender stereotypes, or when technologies are calibrated to the norm of one segment of the population and fail to account for the severity of disease in others.
The pandemic has also revealed the biopolitics and even the “necropolitics” of care — when policymakers who are aware that disease and death fall disproportionately in marginal populations make public-health decisions that deepen the risks of exposure of these more vulnerable groups. The question becomes, “Whose lives are deemed disposable?” Similarly, which populations — and which regions of the world — are prioritized for treatment and protective technologies like vaccines and to what degree are such decisions politicized or even racialized?
Although no single change will address all of these disparities in health status and access to treatment, municipal, state, and federal policies aimed at improving the American health infrastructure — and especially those that expand the availability and distribution of medical resources to underserved populations — could greatly improve health for all.
Seth Mnookin , professor of science writing
The Covid-19 pandemic adds yet another depressing data point to how the legacy and reality of racism and white supremacy in America is lethal to historically marginalized groups. A number of recent studies have shown that Black, Hispanic, Asian, and Native Americans have a significantly higher risk of infection, hospitalization, and death compared to white Americans.
The reasons are not hard to identify: Minority populations are less likely to have access to healthy food options, clean air and water, high-quality housing, and consistent health care. As a result, they’re more likely to have conditions that have been linked to worse outcomes in Covid patients, including diabetes, hypertension, and obesity.
Marginalized groups are also more likely to be socioeconomically disadvantaged — which means they’re more likely to work in service and manufacturing industries that put them in close contact with others, use public transportation, rely on overcrowded schools and day cares, and live in closer proximity to other households. Even now, more vaccines are going to wealthier people who have the time and technology required to navigate the time-consuming vaccine signup process and fewer to communities with the highest infection rates.
This illustrates why addressing inequalities in Americans’ health requires addressing inequalities that infect every part of society. Moving forward, our health care systems should take a much more active role in advocating for racial and socioeconomic justice — not only because it is the right thing to do, but because it is one of the most effective ways to improve health outcomes for the country as a whole.
On a global level, the pandemic has illustrated that preparedness and economic resources are no match for lies and misinformation. The United States, Brazil, and Mexico have, by almost any metric, handled the pandemic worse than virtually every other country in the world. The main commonality is that all three were led by presidents who actively downplayed the virus and fought against lifesaving public health measures. Without a global commitment to supporting accurate, scientifically based information, there is no amount of planning and preparation that can outflank the spread of lies.
Parag Pathak , Class of 1922 Professor of Economics The pandemic has revealed the strengths and weaknesses of America’s health care systems in an extreme way. The development and approval of three vaccines in roughly one year after the start of the pandemic is a phenomenal achievement. At the same time, there are many innovations for which there have been clear fumbles, including the deployment of rapid tests and contact tracing. The other aspect the pandemic has made apparent is the extreme inequality in America’s health systems. Disadvantaged communities have borne the brunt of Covid-19 both in terms of health outcomes and also economically. I’m hopeful that the pandemic will spur renewed focus on protecting the most vulnerable members of society. A pandemic is a textbook situation in economics of externalities, where an individual’s decision has external effects on others. In such situations, there can be major gains to coordination. In the United States, the initial response was poorly coordinated across states. I think the same criticism applies globally. We have not paid enough attention to population health on a global scale. One lesson I take from the relative success of the response of East Asian countries is that centralized and coordinated health systems are more equipped to manage population health, especially during a pandemic. We’re already seeing the need for international cooperation with vaccine supply and monitoring of new variants. It will be imperative that we continue to invest in developing the global infrastructure to facilitate greater cooperation for the next pandemic.
Prepared by MIT SHASS Communications Editor and designer: Emily Hiestand Consulting editor: Kathryn O'Neill
Share this news article on:
Related links.
- Program in Science, Technology and Society
- Graduate Program in Science Writing
- MIT Anthropology
- Department of Economics
- Department of Political Science
- Department of Urban Studies and Planning
Related Topics
- Anthropology
- Political science
- Program in STS
- Science writing
- Public health
- Health care
- Diversity and inclusion
- Science, Technology, and Society
- School of Humanities Arts and Social Sciences
Related Articles

Reflecting on a year of loss, grit, and pulling together
Building equity into vaccine distribution.

In online vigil, MIT community shares grief, anger, and hope
Previous item Next item
More MIT News

Scientists identify mechanism behind drug resistance in malaria parasite
Read full story →

Getting to systemic sustainability

New MIT-LUMA Lab created to address climate challenges in the Mediterranean region

MIT Press releases Direct to Open impact report

Modeling the threat of nuclear war
Modular, scalable hardware architecture for a quantum computer
- More news on MIT News homepage →
Massachusetts Institute of Technology 77 Massachusetts Avenue, Cambridge, MA, USA
- Map (opens in new window)
- Events (opens in new window)
- People (opens in new window)
- Careers (opens in new window)
- Accessibility
- Social Media Hub
- MIT on Facebook
- MIT on YouTube
- MIT on Instagram
- SUGGESTED TOPICS
- The Magazine
- Newsletters
- Managing Yourself
- Managing Teams
- Work-life Balance
- The Big Idea
- Data & Visuals
- Reading Lists
- Case Selections
- HBR Learning
- Topic Feeds
- Account Settings
- Email Preferences
5 Critical Priorities for the U.S. Health Care System
- Marc Harrison

A guide to making health care more accessible, affordable, and effective.
The pandemic has starkly revealed the many shortcomings of the U.S. health care system — as well as the changes that must be implemented to make care more affordable, improve access, and do a better job of keeping people healthy. In this article, the CEO of Intermountain Healthcare describes five priorities to fix the system. They include: focus on prevention, not just treating sickness; tackle racial disparities; expand telehealth and in-home services; build integrated systems; and adopt value-based care.
Since early 2020, the dominating presence of the Covid-19 pandemic has redefined the future of health care in America. It has revealed five crucial priorities that together can make U.S. health care accessible, more affordable, and focused on keeping people healthy rather than simply treating them when they are sick.
- Marc Harrison , MD, is president and CEO of Salt Lake City-based Intermountain Healthcare.
Partner Center
Understanding why health care costs in the U.S. are so high
The high cost of medical care in the U.S. is one of the greatest challenges the country faces and it affects everything from the economy to individual behavior, according to an essay in the May-June 2020 issue of Harvard Magazine written by David Cutler , professor in the Department of Global Health and Population at Harvard T.H. Chan School of Public Health.
Cutler explored three driving forces behind high health care costs—administrative expenses, corporate greed and price gouging, and higher utilization of costly medical technology—and possible solutions to them.
Read the Harvard Magazine article: The World’s Costliest Health Care
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
2021 National Healthcare Quality and Disparities Report [Internet]. Rockville (MD): Agency for Healthcare Research and Quality (US); 2021 Dec.
2021 National Healthcare Quality and Disparities Report [Internet].
Overview of u.s. healthcare system landscape.
The National Academy of Medicine defines healthcare quality as “the degree to which health care services for individuals and populations increase the likelihood of desired health outcomes and are consistent with current professional knowledge.” Many factors contribute to the quality of care in the United States, including access to timely care, affordability of care, and use of evidence-based guidelines to drive treatment.
This section of the report highlights utilization of healthcare services, healthcare workforce statistics, healthcare expenditures, and major contributors to morbidity and mortality. These factors help paint an overall picture of the U.S. healthcare system, particularly areas that need improvement. Quality measures show whether the healthcare system is adequately addressing risk factors, diseases, and conditions that place the greatest burden on the healthcare system and if change has occurred over time.
- Overview of the U.S. Healthcare System Infrastructure
The NHQDR tracks care delivered by providers in many types of healthcare settings. The goal is to provide high-quality healthcare that is culturally and linguistically sensitive, patient centered, timely, affordable, well coordinated, and safe. The receipt of appropriate high-quality services and counseling about healthy lifestyles can facilitate the maintenance of well-being and functioning. In addition, social determinants of health, such as education, income, and residence location can affect access to care and quality of care.
Improving care requires facility administrators and providers to work together to expand access, enhance quality, and reduce disparities. It also requires coordination between the healthcare sector and other sectors for social welfare, education, and economic development. For example, Healthy People 2030 includes 5 domains (shown in the diagram below) and 78 social determinants of health objectives for federal programs and interventions.
Healthy People 2030 social determinants of health domains.
The numbers of health service encounters and people working in health occupations illustrate the large scale and inherent complexity of the U.S. healthcare system. The tracking of healthcare quality measures in this report iii attempts to quantify progress made in improving quality and reducing disparities in the delivery of healthcare to the American people.
Number of healthcare service encounters, United States, 2018 and 2019.
- In 2018, there were 860 million physician office visits ( Figure 1 ).
- In 2019, patients spent 149 million days in hospice.
- In 2019, there were 100 million home health visits.
- Overview of Disease Burden in the United States
The National Institutes of Health defines disease burden as the impact of a health problem, as measured by prevalence, incidence, mortality, morbidity, extent of disability, financial cost, or other indicators.
This section of the report highlights two areas of disease burden that have major impact on the health system of the United States: years of potential life lost and leading causes of death. The NHQDR tracks measures of quality for most of these conditions. Variation in access to care and care delivery across communities contributes to disparities related to race, ethnicity, sex, and socioeconomic status.
The concept of years of potential life lost (YPLL) involves estimating the average time a person would have lived had he or she not died prematurely. This measure is used to help quantify social and economic loss from premature death, and it has been promoted to emphasize specific causes of death affecting younger age groups. YPLL inherently incorporates age at death, and its calculation mathematically weights the total deaths by applying values to death at each age. 1
According to the Centers for Disease Control and Prevention (CDC), unintentional injuries include opioid overdoses (unintentional poisoning), motor vehicle crashes, suffocation, drowning, falls, fire/burns, and sports and recreational injuries. Overdose deaths involving opioids, including prescription opioids , heroin , and synthetic opioids (e.g., fentanyl ), have been a major contributor to the increase in unintentional injuries. Opioid overdose has increased to more than six times its 1999 rate. 2
Age-adjusted years of potential life lost before age 65, by cause of death, 2010–2019. Key: YPLL = years of potential life lost. Note: The perinatal period occurs from 22 completed weeks (154 days) of gestation and ends 7 completed days after (more...)
- From 2010 to 2019, there were no changes in the ranking of the top 10 leading diseases and injuries contributing to YPLL. The top 5 were unintentional injury, cancer, heart disease, suicide, and complications during the perinatal period ( Figure 2 ). The remaining 5 were homicide, congenital anomalies, liver disease, diabetes, and cerebrovascular disease.
- Unintentional injury increased from 791.8 per 100,000 population in 2010 to 1,024.3 per 100,000 population in 2019.
- Cancer decreased from 635.2 per 100,000 population in 2010 to 533.3 per 100,000 population in 2019.
- Heart disease decreased from 474.3 per 100,000 population in 2010 to 453.2 per 100,000 population in 2019.
Age-adjusted years of potential life lost before age 65, by cause of death and race, 2019. Key: AI/AN = American Indian or Alaska Native; PI = Pacific Islander.
- In 2019, among American Indian and Alaska Native (AI/AN) people, the top five contributing factors for YPLL were unintentional injuries (1,284.6 per 100,000 population), suicide (457.7 per 100,000 population), liver disease (451.6 per 100,000 population), heart disease (399.8 per 100,000 population), and cancer (339.6 per 100,000 population) ( Figure 3 ).
- In 2019, among Asian and Pacific Islander people, the top five contributing factors for YPLL were cancer (375.7 per 100,000 population), unintentional injuries (299.4 per 100,000 population), complications in the perinatal period (203.4 per 100,000 population), suicide (198.5 per 100,000), and heart disease (197.7 per 100,000 population).
- In 2019 among Black people, the top five contributing factors for YPLL were unintentional injuries (1,085.8 per 100,000 population), heart disease (843.5 per 100,000 population), homicide (801.7 per 100,000 population), cancer (652.7 per 100,000 population), and complications in the perinatal period (560.4 per 100,000 population).
- In 2019, among White people, the top five contributing factors for YPLL were unintentional injuries (1,080.0 per 100,000 population), cancer (530.1 per 100,000 population), heart disease (406.6 per 100,000 population), suicide (387.6 per 100,000 population), and complications in the perinatal period (215.7 per 100,000 population).
Leading causes of death for the total population, United States, 2018 and 2019.
- In 2019, heart disease, cancer, unintentional injuries, chronic lower respiratory diseases, stroke, Alzheimer’s disease, and diabetes were among the leading causes of death for the overall U.S. population ( Figure 4 ).
- Overall, kidney disease moved from the 9 th leading cause of death in 2018 to the 8 th leading cause of death in 2019.
- Suicide remained the 10 th leading cause of death in 2018 and 2019.
The years of potential life lost, years with disability, and leading causes of death represent some aspects of the burden of disease experienced by the American people. Findings highlighted in this report attempt to quantify progress made in improving quality of care, reducing disparities in healthcare, and ultimately reducing disease burden.
- Overview of U.S. Community Hospital Intensive Care Beds
The United States has almost 1 million staffed hospital beds; nearly 800,000 are community hospital beds and 107,000 are intensive care beds. Figure 5 shows the numbers of different types of staffed intensive care hospital beds.
Medical-surgical intensive care provides patient care of a more intensive nature than the usual medical and surgical care delivered in hospitals, on the basis of physicians’ orders and approved nursing care plans. These units are staffed with specially trained nursing personnel and contain specialized equipment for monitoring and supporting patients who, because of shock, trauma, or other life-threatening conditions, require intensified comprehensive observation and care. These units include mixed intensive care units.
Pediatric intensive care provides care to pediatric patients that is more intensive in nature than that usually provided to pediatric patients. The unit is staffed with specially trained personnel and contains monitoring and specialized support equipment for treating pediatric patients who, because of shock, trauma, or other life-threatening conditions, require intensified, comprehensive observation and care.
Cardiac intensive care provides patient care of a more specialized nature than the usual medical and surgical care, on the basis of physicians’ orders and approved nursing care plans. The unit is staffed with specially trained nursing personnel and contains specialized equipment for monitoring, support, or treatment for patients who, because of severe cardiac disease such as myocardial infarction, open-heart surgery, or other life-threatening conditions, require intensified, comprehensive observation and care.
Neonatal intensive care units (NICUs) are distinct from the newborn nursery and provide intensive care to sick infants, including those with the very lowest birth weights (less than 1,500 grams). NICUs may provide mechanical ventilation, care before or after neonatal surgery, and special care for the sickest infants born in the hospital or transferred from another institution. Neonatologists typically serve as directors of NICUs.
Burn care provides care to severely burned patients. Severely burned patients are those with the following: (1) second-degree burns of more than 25% total body surface area for adults or 20% total body surface area for children; (2) third-degree burns of more than 10% total body surface area; (3) any severe burns of the hands, face, eyes, ears, or feet; or (4) all inhalation injuries, electrical burns, complicated burn injuries involving fractures and other major traumas, and all other poor risk factors.
Other intensive care unit beds are in specially staffed, specialty-equipped, separate sections of a hospital dedicated to the observation, care, and treatment of patients with life-threatening illnesses, injuries, or complications from which recovery is possible. This type of care includes special expertise and facilities for the support of vital functions and uses the skill of medical, nursing, and other staff experienced in the management of conditions that require this higher level of care.
U.S. community hospital intensive care staffed beds, by type of intensive care, 2019. Note: Community hospitals are defined as all nonfederal, short-term general, and other special hospitals. Other special hospitals include obstetrics and gynecology; (more...)
- In 2019, of the more than 900,000 staffed hospital beds in the United States, 86% were in community hospitals (data not shown).
- Most of the more than 107,000 intensive care beds in community hospitals were medical-surgical intensive care (51.9%) and neonatal intensive care beds (21.1%) ( Figure 5 ).
Critical access hospital (CAH) is a designation given to eligible rural hospitals by the Centers for Medicare & Medicaid Services (CMS). The CAH designation is designed to reduce the financial vulnerability of rural hospitals and improve access to healthcare by keeping essential services in rural communities. To accomplish this goal, CAHs receive certain benefits, such as cost-based reimbursement for Medicare services. As of July 16, 2021, 1,353 CAHs were located throughout the United States. 3 , iv
Distribution of critical access hospitals in the United States, 2021.
- According to CMS, CAHs must be located in a rural area or an area that is treated as rural, v so the number of CAHs varies by state ( Figure 6 ).
- In 2019, California had a population of 39.5 million and 36 CAHs compared with Iowa, which had a population of only 3.2 million but 82 CAHs.
- U.S. Healthcare Workforce
Healthcare access and quality can be affected by workforce shortages, particularly in rural areas. In addition, lack of racial, ethnic, and gender concordance between providers and patients can lead to miscommunication, stereotyping, and stigma, and, ultimately, suboptimal healthcare.
Healthcare Workforce Availability
Improving quality of care, increasing access to care, and controlling healthcare costs depend on the adequate availability of healthcare providers. 4 Physician shortages currently exist in many states across the nation, with relatively fewer primary care and specialty physicians available in nonmetropolitan counties compared with metropolitan counties. 5
The Health Resources and Services Administration (HRSA) further projects that the supply of key professions, including primary care providers, general dentists, adult psychiatrists, and addiction counselors, will fall short of demand by 2030. 6 These concerns have the potential to influence the delivery of healthcare and negatively affect patient outcomes.
Number of people working in health occupations, United States, 2019. Key: EMT = emergency medical technician. Note: Doctors of medicine also include doctors of osteopathic medicine. Active physicians include those working in direct patient care, administration, (more...)
- In 2019, there were 3.7 million registered nurses ( Figure 7 ).
- In 2019, there were 2.4 million healthcare aides, which includes nursing, psychiatric, home health, and occupational therapy aides and physical therapy assistants and aides.
- In 2019, there were 2.1 million health technologists.
- In 2019, 2.0 million other health practitioners provided care, including more than 145,000 physician assistants (PAs).
- In 2019, there were 972,000 active medical doctors in the United States, which include doctors of medicine and doctors of osteopathy.
- In 2019, there were 183,000 dentists.
In recent decades, promising approaches that address the supply-demand imbalance have emerged as alternatives to simply increasing the number of physicians. One strategy relies on telehealth technologies to improve physicians’ efficiency or to increase access to their services. For example, Project ECHO is a telehealth model in which specialists remotely support multiple rural primary care providers so that they can treat patients for conditions that might otherwise require traveling to distant specialty centers. 7
Another strategy relies on peer-led models, in which community-based laypeople receive the training and support needed to deliver care for a (typically) narrow range of conditions. Successful examples of this approach exist, including the deployment of community health workers to manage chronic diseases, 8 promotoras to provide maternal health services, 9 peer counselors for mental health and substance use disorders, 10 and dental health aides to deliver oral health services in remote locations. 11
The National Institutes of Health, HRSA, and the Agency for Healthcare Research and Quality (AHRQ) have sponsored formative research to examine key issues that must be addressed to further develop these models, but all show promise for expanding access to care and increasing overall diversity within the healthcare workforce.
Workforce Diversity
The number of full-time, year-round workers in healthcare occupations has almost doubled since 2000, increasing from 5 million to 9 million workers, according to the U.S. Census Bureau’s American Community Survey .
A racially and ethnically diverse health workforce has been shown to promote better access and healthcare for underserved populations and to better meet the health needs of an increasingly diverse population. People of color, however, remain underrepresented in several health professions, despite longstanding efforts to increase the diversity of the healthcare field. 12
Additional research has found that physicians from groups underrepresented in the health professions are more likely to serve minority and economically disadvantaged patients. It has also been found that Black and Hispanic physicians practice in areas with larger Black and Hispanic populations than other physicians do. 13
Gender diversity is also important. Women currently account for three-quarters of full-time, year-round healthcare workers. Although the number of men who are dentists or veterinarians has decreased over the past two decades, men still make up more than half of dentists, optometrists, and emergency medical technicians/paramedics, as well as physicians and surgeons earning over $100,000. 14
Women working as registered nurses, the most common healthcare occupation, earn on average $66,000. Women working as nursing, psychiatric, and home health aides, the second most common healthcare occupation, earn only $27,000. 14
The impact of unequal gender distribution in the healthcare workforce is observed in the persistence of gender inequality in heart attack mortality. Most physicians are male, and some may not recognize differences in symptoms in female patients. The fact that gender concordance correlates with whether a patient survives a heart attack has implications for theory and practice. Medical practitioners should be aware of the possible challenges male providers face when treating female heart attack patients. 15
Research has shown that some mental health workforce groups, such as psychiatrists, are more diverse than many other medical specialties, and this diversity has improved over time. However, this diversity has not translated as well to academic faculty or leadership positions for underrepresented minorities. It was found that there was more minority representation among psychiatry residents (16.2%) compared with faculty (8.7%) and practicing physicians (10.4%). This difference results in minority students and trainees having fewer minority mentors to guide them in the profession.
Racial and Ethnic Diversity Among Physicians
Diversification of the physician workforce has been a goal for several years and could improve access to primary care for underserved populations and address health disparities. Family physicians’ race/ethnicity has become more diverse over time but still does not reflect the national racial and ethnic composition. 16 , vi
Racial and ethnic distribution of all active physicians (left) and U.S. population racial and ethnic distribution (right), 2019. Note: White, Black, Asian, and >1 Race are non-Hispanic. Percentages of the U.S. population do not add to 100 due (more...)
- In 2019, White people were 60% of the U.S. population and approximately 64% of physicians ( Figure 8 ).
- Asian people were about 6% of the U.S. population and approximately 22% of physicians.
- Black people were 12% of the U.S. population but only 5% of physicians.
- Hispanic people were 18% of the U.S. population but only 7% of physicians.
- People of more than race made up about 3% of the U.S. population but less than 2% of physicians.
- AI/AN people and Native Hawaiian/Pacific Islander (NHPI) people accounted for 1% or less of the U.S. population and 1% or less of physicians (data not shown).
Preventive care, including screenings, is key to reducing death and disability and improving health. Evidence has shown that patients with providers of the same gender have higher rates of breast, cervical, and colorectal cancer screenings. 17
Physicians by race/ethnicity and sex, 2018. Key: AI/AN = American Indian or Alaska Native; NHPI = Native Hawaiian/Pacific Islander. Note: Physicians (federal and nonfederal) who are licensed by a state are considered active, provided they are working (more...)
- In 2018, among Black physicians, females (53.0%) constituted a larger percentage than males (47.0%) ( Figure 9 ).
- Among White physicians, 65.5% were male.
- Among Asian physicians, 55.7% were male.
- Among AI/AN physicians, 60.1% were male.
- Among Hispanic physicians, 59.5% were male.
White physicians by age and sex, 2018. Note : Physicians (federal and nonfederal) who are licensed by a state are considered active, provided they are working at least 20 hours per week. Physicians who are retired, semiretired, temporarily not in practice, (more...)
- In 2018, among White physicians, males were the vast majority of those age 65 years and over (79.3%) and of those ages 55–64 years (71.5%) ( Figure 10 ).
- A little more than half of White physicians age 34 and younger were females (50.6%).
- Among White physicians age 35 and over, males made up a larger percentage of the workforce than females. This percentage increased with age.
Black physicians by age and sex, 2018. Note: Physicians (federal and nonfederal) who are licensed by a state are considered active, provided they are working at least 20 hours per week. Physicians who are retired, semiretired, temporarily not in practice, (more...)
- In 2018, among Black physicians under age 55, females made up a larger percentage of the workforce than males. This percentage decreased with increasing age ( Figure 11 ).
- Females were 44.2% of Black physicians ages 55–64 and 34.9% of Black physicians age 65 and over.
Asian physicians by age and sex, 2018. Note: Physicians (federal and nonfederal) who are licensed by a state are considered active, provided they are working at least 20 hours per week. Physicians who are retired, semiretired, temporarily not in practice, (more...)
- In 2018, among Asian physicians, males were the vast majority of those age 65 years and over (72.7%) and of those ages 55–64 years (66.3%) ( Figure 12 ).
- Among Asian physicians age 34 and younger, there were more females (52.0%) than males (48.0%).
- Among Asian physicians age 35 and over, males made up a larger percentage of the workforce than females. This percentage increased with age.
American Indian or Alaska Native physicians by age and sex, 2018. Note: Physicians (federal and nonfederal) who are licensed by a state are considered active, provided they are working at least 20 hours per week. Physicians who are retired, semiretired, (more...)
- In 2018, among AI/AN physicians, males were the vast majority of those age 65 years and over (73.2%) and of those ages 55–64 years (62.6%) ( Figure 13 ).
- Among AI/AN physicians age 34 and younger, there were more females (57.9%) than males (42.1%).
- Among AI/AN physicians age 45 and over, males made up a larger percentage of the workforce than females. This percentage increased with age.
Hispanic physicians by age and sex, 2018. Note: Physicians (federal and nonfederal) who are licensed by a state are considered active, provided they are working at least 20 hours per week. Physicians who are retired, semiretired, temporarily not in practice, (more...)
- In 2018, most Hispanic physicians age 65 years and over (77.5%) and ages 55–64 years (67.5%) were males ( Figure 14 ).
- Among Hispanic physicians age 34 and younger, there were more females (55.3%) compared with males (44.7%).
- Among Hispanic physicians age 35 and over, males made up a larger percentage of the workforce than females. This percentage increased with age.
Racial and Ethnic Diversity Among Dentists
The racial and ethnic diversity of the oral healthcare workforce is insufficient to meet the needs of a diverse population and to address persistent health disparities. 18 However, among first-time, first-year enrollees in dental school, improved diversity has been observed. The number of African American enrollees nearly doubled and the number of Hispanic enrollees has increased threefold between 2000 and 2020. 19 Increased diversity among dentists may improve access and quality of care, particularly in the area of culturally and linguistically sensitive care.
Dentists by race (left) and U.S. population racial and ethnic distribution (right), 2019. Note: White, Black, Asian, and Other are non-Hispanic. If estimates for certain racial and ethnic groups meet data suppression criteria, they are recategorized into (more...)
- In 2019, the vast majority of dentists (70%) were non-Hispanic White ( Figure 15 ).
- Asian people, 18%,
- Hispanic people, 6%
- Black people, 5%, and
- Other (multiracial and AI/AN people), 1.0%.
Racial and Ethnic Diversity Among Registered Nurses
Ensuring workforce diversity and leadership development opportunities for racial and ethnic minority nurses must remain a high priority in order to eliminate health disparities and, ultimately, achieve health equity. 20
Registered nurses by race/ethnicity (left) and U.S. population racial and ethnic distribution (right), 2019. Note: White, Black, Asian, >1 Race, and Other are non-Hispanic. Percentages of the U.S. population do not add to 100 due to rounding and (more...)
- In 2019, the vast majority of RNs (69%) were non-Hispanic White ( Figure 16 ).
- Black people, 11%,
- Asian people, 9%,
- Hispanic people, 8%,
- Multiracial people, 2%, and
- Other (AI/AN and NHPI people), 1%.
Racial and Ethnic Diversity Among Pharmacists
Most healthcare diagnostic and treating occupations such as pharmacists, physicians, nurses, and dentists are primarily White while healthcare support roles such as dental assistants, medical assistants, and personal care aides are more diverse. To decrease disparities and enhance patient care, racial and ethnic diversity must be improved on all levels of the healthcare workforce, not just in support roles. 21
Progress has been made toward increased racial and ethnic diversity, but more work is needed. As Bush notes in an article on underrepresented minorities in pharmacy school, “If we are determined to reduce existing healthcare disparities among racial, ethnic, and socioeconomic groups, then we must be determined to diversify the healthcare workforce.” 22
Pharmacists by race (left) and U.S. population racial and ethnic distribution (right), 2019. Note: White, Black, Asian, and >1 Race are non-Hispanic. Percentages of the U.S. population do not add to 100 due to rounding and the exclusion of groups (more...)
- In 2019, the vast majority of pharmacists (65%) were non-Hispanic White ( Figure 17 ).
- Asian people, 20%,
- Black people, 7%,
- Hispanic people, 5%, and
- Multiracial people, 2%.
Racial and Ethnic Diversity Among Therapists
Occupational therapists, physical therapists, radiation therapists, recreational therapists, and respiratory therapists are classified as health diagnosing and treating practitioners. Hispanic people are significantly underrepresented in all of the occupations in the category of Health Diagnosing and Treating Practitioners. Among non-Hispanic people, Black people are underrepresented in most of these occupations.
Asian people are underrepresented among speech-language pathologists, and AI/AN people are underrepresented in nearly all occupations. To the extent they can be reliably reported, data also show that NHPI people are underrepresented in all occupations in the Health Diagnosing and Treating Practitioners group. 21
Therapists include occupational therapists, physical therapists, radiation therapists, recreational therapists, respiratory therapists, speech-language pathologists, exercise physiologists, and other therapists.
Therapists by race/ethnicity (left) and U.S. population racial and ethnic distribution (right), 2019. Note: White, Black, Asian, and >1 Race are non-Hispanic. Percentages of the U.S. population do not add to 100 due to rounding and the exclusion (more...)
- In 2019, the vast majority of therapists (74%) were non-Hispanic White ( Figure 18 ).
- Black people, 8%,
- Asian people, 8%,
- Hispanic people, 8%, and
Racial and Ethnic Diversity Among Advanced Practice Registered Nurses
The adequacy and distribution of the primary care workforce to meet the current and future needs of Americans continue to be cause for concern. Advanced practice registered nurses are increasingly being used to fill this gap but may include clinicians in areas beyond primary care, such as clinical nurse specialists, nurse-midwives, and nurse anesthetists.
Advanced practice registered nurses are registered nurses educated at the master’s or post-master’s level who serve in a specific role with a specific patient population. They include certified nurse practitioners, clinical nurse specialists, certified nurse anesthetists, and certified nurse-midwives.
While physicians continue to account for most of the primary care workforce (74%) in the United States, nurse practitioners represent nearly one-fifth (19%) of the primary care workforce, followed by physician assistants, accounting for 7%. 23
Nurse practitioners provide an extensive range of services that includes taking health histories and providing complete physical exams. They diagnose and treat acute and chronic illnesses, provide immunizations, prescribe and manage medications and other therapies, order and interpret lab tests and x rays, and provide health education and supportive counseling.
Nurse practitioners deliver primary care in practices of various sizes, types (e.g., private, public), and settings, such as clinics, schools, and workplaces. Nurse practitioners work independently and collaboratively. They often take the lead in providing care in innovative primary care arrangements, such as retail clinics. 24
Advanced practice registered nurses by race (left) and U.S. population racial and ethnic distribution (right), 2019. Note: White, Black, Asian, and >1 Race are non-Hispanic. Percentages of the U.S. population do not add to 100 due to rounding (more...)
- In 2019, the vast majority of advanced practice registered nurses (78 %) were non-Hispanic White ( Figure 19 ).
- Asian people, 6%,
- Hispanic people, 6%, and
Racial and Ethnic Diversity Among Emergency Professionals
Workforce diversity can reduce communication barriers and inequalities in healthcare delivery, especially in settings such as emergency departments, where time pressure and incomplete information may worsen the effects of implicit biases. The racial and ethnic makeup of the paramedic and emergency medical technician workforce indicates that concerted efforts are needed to encourage students of diverse backgrounds to pursue emergency service careers. 25
Emergency medical technicians and paramedics by race (left), and U.S. population racial and ethnic distribution (right), 2019. Note: White, Black, Asian, >1 Race, and Other are non-Hispanic. Percentages do not add to 100 due to rounding. In addition, (more...)
- In 2019, the vast majority of emergency medical technicians (EMTs) and paramedics (72%) were non-Hispanic White ( Figure 20 ).
- Hispanic people, 13%
- Asian people, 3%,
Racial and Ethnic Diversity Among Other Health Practitioners
Other health practitioners include physician assistants, medical assistants, dental assistants, chiropractors, dietitians and nutritionists, optometrists, podiatrists, and audiologists, as well as massage therapists, medical equipment preparers, medical transcriptionists, pharmacy aides, veterinary assistants and laboratory animal caretakers, phlebotomists, and healthcare support workers.
Other health practitioners by race/ethnicity (left) and U.S. population racial and ethnic distribution (right), 2019. Note: White, Black, Asian, >1 Race, and Other are non-Hispanic. Percentages of the U.S. population do not add to 100 due to rounding (more...)
- In 2019, the distribution of other health practitioners closely aligned with the racial and ethnic distribution of the U.S. population ( Figure 21 ).
- In 2019, 58% of other health practitioners were non-Hispanic White.
- In 2019, Hispanic people accounted for 20% of other health practitioners.
- Black people, 12%,
- Asian people, 7%,
Racial and Ethnic Diversity Among Physician Assistants
Physician assistants (PAs) are included in the Other Health Practitioners workforce group but are highlighted because they play a critical role in frontline primary care services in many settings, especially medically underserved and rural areas. With the demand for primary care services projected to grow and PAs’ roles in direct care, understanding this occupation’s racial and ethnic diversity is important.
Studies identify the value of advanced practice providers in patient care management, continuity of care, improved quality and safety metrics, and patient and staff satisfaction. These providers can also enhance the educational experience of residents and fellows. 26 However, a lack of workforce diversity has detrimental effects on patient outcomes, access to care, and patient trust, as well as on workplace experiences and employee retention. 27
Physician assistants by race/ethnicity (left) and U.S. population racial and ethnic distribution (right), 2019. Note: White, Black, Asian, >1 Race, and Other are non-Hispanic. Percentages of the U.S. population do not add to 100 due to rounding (more...)
- In 2019, the vast majority of physician assistants (73%) were non-Hispanic White ( Figure 22 ).
- Black people, 6%,
- Multiracial people, 3%, and
Racial and Ethnic Diversity Among Other Health Occupations
Other health occupations include veterinarians, acupuncturists, all other healthcare diagnosing or treating practitioners, dental hygienists, and licensed practical and licensed vocational nurses.
Other health occupations by race/ethnicity (left) and U.S. population racial and ethnic distribution (right), 2019. Note: White, Black, Asian, >1 Race, and Other are non-Hispanic. Percentages of the U.S. population do not add to 100 due to rounding (more...)
- In 2019, the vast majority of staff in other health occupations (61%) were non-Hispanic White ( Figure 23 ).
- Black people, 19%,
- Hispanic people, 11%
- Asian people, 6 %,
Racial and Ethnic Diversity Among Health Technologists
Health technologists include clinical laboratory technologists and technicians, cardiovascular technologists and technicians, diagnostic medical sonographers, radiologic technologists and technicians, magnetic resonance imaging technologists, nuclear medicine technologists and medical dosimetrists, pharmacy technicians, surgical technologists, veterinary technologists and technicians, dietetic technicians and ophthalmic medical technicians, medical records specialists, and opticians (dispensing), miscellaneous health technologists and technicians, and technical occupations.
Health technologists by race/ethnicity (left) and U.S. population racial and ethnic distribution (right), 2019. Note: White, Black, Asian, and >1 Race are non-Hispanic. Percentages of the U.S. population do not add to 100 due to rounding and the (more...)
- In 2019, the vast majority of health technologists (63%) were non-Hispanic White ( Figure 24 ).
- Black people, 14%,
- Hispanic people, 13%,
- Asian people, 8%, and
Racial and Ethnic Diversity Among Healthcare Aides
Healthcare aides include nursing, psychiatric, home health, occupational therapy, and physical therapy assistants and aides.
Healthcare aides by race/ethnicity (left) and U.S. population racial and ethnic distribution (right), 2019. Note: White, Black, Asian, >1 Race, and Other are non-Hispanic. Percentages of the U.S. population do not add to 100 due to rounding and (more...)
- In 2019, 41% of healthcare aides were non-Hispanic White ( Figure 25 ).
- Black people, 32%,
- Hispanic people, 18%,
Racial and Ethnic Diversity Among Psychologists
The United States has an inadequate workforce to meet the mental health needs of the population, 28 , 29 , 30 and it is estimated that in 2020, nearly 54% of the U.S. population age 18 and over with any mental illness did not receive needed treatment. 31 This unmet need is even greater for racial and ethnic minority populations. Nearly 80% of Asian and Pacific Islander people, vii 63% of African Americans, and 65% of Hispanic people with a mental illness do not receive mental health treatment. 29 , 32 , 33 , 34
These gaps in mental health care may be attributed to a number of reasons, including stigma, cultural attitudes and beliefs, lack of insurance, or lack of familiarity with the mental health system. 35 , 36 , 37 However, a significant contributor to this treatment gap is the composition of the workforce.
The current mental health workforce lacks racial and ethnic diversity. 34 , 38 Research has shown that racial and ethnic patient-provider concordance is correlated with patient engagement and retention in mental health treatment. 39 In addition, racial and ethnic minority providers are more likely to serve patients of color than White providers. 34 , 36
Among psychologists, a key practitioner group in the mental health workforce, 37 , 40 minorities are significantly underrepresented. Psychologists in the United States are predominantly non-Hispanic White, while all racial and ethnic minorities represented only about one-sixth of all psychologists from 2011 to 2015.
Reducing the serious gaps in mental health care for racial and ethnic minority populations will require a significant shift in the workforce. Workforce recruitment, training, and education of more racially, ethnically, and culturally diverse practitioners will be essential to reduce these disparities.
Psychologists by race/ethnicity (left) and U.S. population racial and ethnic distribution (right), 2019. Note: White, Black, Asian, and >1 Race are non-Hispanic. Psychologists include practitioners of general psychology, developmental and child (more...)
- In 2019, the vast majority of psychologists (79%) were non-Hispanic White ( Figure 26 ).
- Hispanic people,10%,
- Asian people, 4%, and
- Multiracial people, 2.0%.
Although the outpatient substance use treatment field has seen an increase in referrals of Black and Hispanic clients, there have been limited changes in the diversity of the workforce. This discordance may exacerbate treatment disparities experienced by these clients. 41
Substance abuse and behavioral disorder counselors by race/ethnicity (left) and U.S. population racial and ethnic distribution (right), 2019. Key: AI/AN = American Indian/Alaska Native. Note: White, Black, Asian, AI/AN, and >1 Race are non-Hispanic. (more...)
- In 2019, the majority of substance abuse and behavioral disorder counselors (58%) were non-Hispanic White ( Figure 27 ).
- Black people, 18%,
- Hispanic people, 16 %,
- Asian people, 4%,
- AI/AN people, 1%.
- Overview of Healthcare Expenditures in the United States
- Hospital care expenditures grew by 6.2% to $1.2 trillion in 2019, faster than the 4.2% growth in 2018.
- Physician and clinical services expenditures grew 4.6% to $772.1 billion in 2019, a faster growth than the 4.0% in 2018.
- Prescription drug spending increased by 5.7% to $369.7 billion in 2019, faster than the 3.8% growth in 2018.
- In 2019, the federal government (29%) and households (28%) each accounted for the largest shares of healthcare spending, followed by private businesses (19%), state and local governments (16%), and other private revenues (7%). Federal government spending on health accelerated in 2019, increasing 5.8% after 5.4% growth in 2018.
Personal Healthcare Expenditures
“Personal healthcare expenditures” measures the total amount spent to treat individuals with specific medical conditions. It comprises all of the medical goods and services used to treat or prevent a specific disease or condition in a specific person. These include hospital care; professional services; other health, residential, and personal care; home health care; nursing care facilities and continuing care retirement communities; and retail outlet sales of medical products. 43
Distribution of personal healthcare expenditures by type of expenditure, 2019. Key: CCRCs = continuing care retirement communities. Note: Percentages do not add to 100 due to rounding. Personal healthcare expenditures are outlays for goods and services (more...)
- In 2019, hospital care expenditures were $1.192 trillion, nearly 40% of personal healthcare expenditures ( Figure 28 ).
- Expenditures for physician and clinical services were $772.1 billion, almost one-fourth of personal healthcare expenditures.
- Prescription drug expenditures were $369.7 billion, 10% of personal healthcare expenditures.
- Expenditures for dental services were $143.2 billion, 5% of personal healthcare expenditures.
- Nursing care facility expenditures were $172.7 billion and home health care expenditures were $113.5 billion, 5% and 4% of personal healthcare expenditures, respectively.
Personal healthcare expenditures, by source of funds, 2019. Note: Data are available at https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/NationalHealthAccountsHistorical.html. Personal healthcare (more...)
- In 2019, private insurance accounted for 33% of personal healthcare expenditures, followed by Medicare (23%), Medicaid (17%), and out of pocket (13%) ( Figure 29 ).
- Private insurance accounted for 37% of hospital, 40% of physician, 15% of home health, 10% of nursing home, 43% of dental, and 45% of prescription drug expenditures.
- Medicare accounted for 27% of hospital, 25% of physician, 39% of home health, 22% of nursing home, 1.0% of dental, and 28% of prescription drug expenditures.
- Medicaid accounted for 17% of hospital, 11% of physician, 32% of home health, 29% of nursing home, 10% of dental, and 9% of prescription drug expenditures.
- Out-of-pocket payments accounted for 3% of hospital, 8% of physician, 11% of home health, 26% of nursing home, 42% of dental, and 15% of prescription drug expenditures.
Prescription drug expenditures, by source of funds, 2019. Note: Data are available at https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/NationalHealthAccountsHistorical.html. Percentages do (more...)
- Private health insurance companies accounted for 44.5% of retail drug expenses ($164.6 billion in 2019).
- Medicare accounted for 28.3% of retail drug expenses ($104.6 billion).
- Medicaid accounted for 8.5% of retail drug expenses ($31.4 billion).
- Other health insurance programs accounted for 3.0% of retail drug expenses ($11.0 billion).
Other third-party payers had the smallest percentage of costs (1.2%), which represented $4.3 billion in retail drug costs.
- Variation in Healthcare Quality
State-level analysis included 182 measures for which state data were available. Of these measures, 140 are core measures and 42 are supplemental measures from the National CAHPS Benchmarking Database (NCBD), which provides state data for core measures with MEPS national data only.
The state healthcare quality analysis included all 182 measures, and the state disparities analysis included 108 measures for which state-by-race or state-by-ethnicity data were available. State-level data are also available for 136 supplemental measures. These data are available from the Data Query tool on the NHQDR website but are not included in data analysis.
State-level data show that healthcare quality and disparities vary widely depending on state and region. Although a state may perform well in overall quality, the same state may face significant disparities in healthcare access or disparities within specific areas of quality.
Overall quality of care, by state, 2015–2020. Note: All state-level measures with data were used to compute an overall quality score for each state based on the number of quality measures above, at, or below the average across all states. States (more...)
- Some states in the Northeast (Maine, Massachusetts, New Hampshire, and Rhode Island), some in the Midwest (Iowa, Minnesota, North Dakota, and Wisconsin), two states in the West (Colorado and Utah), and North Carolina and Kentucky had the highest overall quality scores.
- Some Southern and Southwestern states (District of Columbia, viii Florida, Georgia, New Mexico, and Texas), two Western states (California and Nevada), some Northwestern states (Montana, Oregon, Washington, and Wyoming), and New York and Alaska had the lowest overall quality scores.
- More information about the measures and data sources included in the creation of this map can be found in Appendix C .
- More information about healthcare quality in each state can be found on the NHQDR website, https://datatools .ahrq.gov/nhqdr .
- Variation in Disparities in Healthcare
The disparities map ( Figure 32 ) shows average differences in quality of care for Black, Hispanic, Asian, NHPI, AI/AN, and multiracial people compared with the reference group, non-Hispanic White or White people. States with fewer than 50 data points are excluded.
Average differences in quality of care for Black, Hispanic, Asian, Native Hawaiian/Pacific Islander, American Indian or Alaska Native, and multiracial people compared with White people, by state, 2018–2019. Note: All measures in this report that (more...)
- Some Western and Midwestern states (Idaho, Iowa, Kansas, Montana, Nevada, New Mexico, Oregon, Utah, and Washington), several Southern states (Kentucky, Mississippi, Virginia, and West Virginia), and Maine had the fewest racial and ethnic disparities overall.
- Several Northeastern states (Massachusetts, New York, and Pennsylvania), two Midwestern states (Illinois and Ohio), two Southern States (Louisiana and Tennessee), and Texas had the most racial and ethnic disparities overall.
Major updates made to three data sources since 2018, specifically the Medical Expenditure Panel Survey, Healthcare Cost and Utilization Project, and National Health Interview Survey, have had an outsized impact on what the 2021 NHQDR can include. Trend data were provided in prior versions of the NHQDR but were not directly comparable for almost half of the core measures at the time this report was developed. Therefore, the 2021 NHQDR does not include a summary figure showing all trend measures or all changes in disparities. The report includes summary figures for trends and change in disparities for some populations and the results for individual measures.
More information on providers that may be eligible to become CAHs and the criteria a Medicare-participating hospital must meet to be designated by CMS as a CAH can be found at https://www .cms.gov/Medicare /Provider-Enrollment-and-Certification /CertificationandComplianc/CAHs .
All the criteria for a Medicare-participating hospital to be designated by CMS as a CAH can be found at https://www .cms.gov/Medicare /Provider-Enrollment-and-Certification /CertificationandComplianc/CAHs .
The most recent data year available is 2018 from the Association of American Medical Colleges, the current source for workforce data broken down by both race/ethnicity and sex.
The National Survey on Drug Use and Health at the Substance Abuse and Mental Health Services Administration combines data for Asian and Pacific Islander populations, which include Native Hawaiian populations.
For purposes of this report, the District of Columbia is treated as a state.
This document is in the public domain and may be used and reprinted without permission. Citation of the source is appreciated.
- Cite this Page 2021 National Healthcare Quality and Disparities Report [Internet]. Rockville (MD): Agency for Healthcare Research and Quality (US); 2021 Dec. OVERVIEW OF U.S. HEALTHCARE SYSTEM LANDSCAPE.
- PDF version of this title (8.0M)
In this Page
Other titles in this collection.
- National Healthcare Quality & Disparities Reports
Recent Activity
- OVERVIEW OF U.S. HEALTHCARE SYSTEM LANDSCAPE - 2021 National Healthcare Quality ... OVERVIEW OF U.S. HEALTHCARE SYSTEM LANDSCAPE - 2021 National Healthcare Quality and Disparities Report
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
How to build a better health system: 8 expert essays

We need to focus on keeping people healthy, not just treating them when they're sick Image: REUTERS/Rupak De Chowdhuri
.chakra .wef-1c7l3mo{-webkit-transition:all 0.15s ease-out;transition:all 0.15s ease-out;cursor:pointer;-webkit-text-decoration:none;text-decoration:none;outline:none;color:inherit;}.chakra .wef-1c7l3mo:hover,.chakra .wef-1c7l3mo[data-hover]{-webkit-text-decoration:underline;text-decoration:underline;}.chakra .wef-1c7l3mo:focus,.chakra .wef-1c7l3mo[data-focus]{box-shadow:0 0 0 3px rgba(168,203,251,0.5);} Global Future Council on Health and Healthcare
Introduction
By Francesca Colombo , Head, Health Division, Organisation for Economic Co-operation and Development (OECD) and Helen E. Clark , Prime Minister of New Zealand (1999-2008), The Helen Clark Foundation
Our healthy future cannot be achieved without putting the health and wellbeing of populations at the centre of public policy.
Ill health worsens an individual’s economic prospects throughout the lifecycle. For young infants and children, ill health affects their capacity to acumulate human capital; for adults, ill health lowers quality of life and labour market outcomes, and disadvantage compounds over the course of a lifetime.
And, yet, with all the robust evidence available that good health is beneficial to economies and societies, it is striking to see how health systems across the globe struggled to maximise the health of populations even before the COVID-19 pandemic – a crisis that has further exposed the stresses and weaknesses of our health systems. These must be addressed to make populations healthier and more resilient to future shocks.
Each one of us, at least once in our lives, is likely to have been frustrated with care that was inflexible, impersonal and bureaucratic. At the system level, these individual experiences add up to poor safety, poor care coordination and inefficiencies – costing millions of lives and enormous expense to societies.
This state of affairs contributes to slowing down the progress towards achieving the sustainable development goals to which all societies, regardless of their level of economic development, have committed.
Many of the conditions that can make change possible are in place. For example, ample evidence exists that investing in public health and primary prevention delivers significant health and economic dividends. Likewise, digital technology has made many services and products across different sectors safe, fast and seamless. There is no reason why, with the right policies, this should not happen in health systems as well. Think, for example, of the opportunities to bring high quality and specialised care to previously underserved populations. COVID-19 has accelerated the development and use of digital health technologies. There are opportunities to further nurture their use to improve public health and disease surveillance, clinical care, research and innovation.
To encourage reform towards health systems that are more resilient, better centred around what people need and sustainable over time, the Global Future Council on Health and Health Care has developed a series of stories illustrating why change must happen, and why this is eminently possible today. While the COVID-19 crisis is severally challenging health systems today, our healthy future is – with the right investments – within reach.
1. Five changes for sustainable health systems that put people first
The COVID-19 crisis has affected more than 188 countries and regions worldwide, causing large-scale loss of life and severe human suffering. The crisis poses a major threat to the global economy, with drops in activity, employment, and consumption worse than those seen during the 2008 financial crisis . COVID-19 has also exposed weaknesses in our health systems that must be addressed. How?
For a start, greater investment in population health would make people, particularly vulnerable population groups, more resilient to health risks. The health and socio-economic consequences of the virus are felt more acutely among disadvantaged populations, stretching a social fabric already challenged by high levels of inequalities. The crisis demonstrates the consequences of poor investment in addressing wider social determinants of health, including poverty, low education and unhealthy lifestyles. Despite much talk of the importance of health promotion, even across the richer OECD countries barely 3% of total health spending is devoted to prevention . Building resilience for populations also requires a greater focus on solidarity and redistribution in social protection systems to address underlying structural inequalities and poverty.
Beyond creating greater resilience in populations, health systems must be strengthened.
High-quality universal health coverage (UHC) is paramount. High levels of household out-of-pocket payments for health goods and services deter people from seeking early diagnosis and treatment at the very moment they need it most. Facing the COVID-19 crisis, many countries have strengthened access to health care, including coverage for diagnostic testing. Yet others do not have strong UHC arrangements. The pandemic reinforced the importance of commitments made in international fora, such as the 2019 High-Level Meeting on Universal Health Coverage , that well-functioning health systems require a deliberate focus on high-quality UHC. Such systems protect people from health threats, impoverishing health spending, and unexpected surges in demand for care.
Second, primary and elder care must be reinforced. COVID-19 presents a double threat for people with chronic conditions. Not only are they at greater risk of severe complications and death due to COVID-19; but also the crisis creates unintended health harm if they forgo usual care, whether because of disruption in services, fear of infections, or worries about burdening the health system. Strong primary health care maintains care continuity for these groups. With some 94% of deaths caused by COVID-19 among people aged over 60 in high-income countries, the elder care sector is also particularly vulnerable, calling for efforts to enhance control of infections, support and protect care workers and better coordinate medical and social care for frail elderly.
Third, the crisis demonstrates the importance of equipping health systems with both reserve capacity and agility. There is an historic underinvestment in the health workforce, with estimated global shortages of 18 million health professionals worldwide , mostly in low- and middle-income countries. Beyond sheer numbers, rigid health labour markets make it difficult to respond rapidly to demand and supply shocks. One way to address this is by creating a “reserve army” of health professionals that can be quickly mobilised. Some countries have allowed medical students in their last year of training to start working immediately, fast-tracked licenses and provided exceptional training. Others have mobilised pharmacists and care assistants. Storing a reserve capacity of supplies such as personal protection equipment, and maintaining care beds that can be quickly transformed into critical care beds, is similarly important.
Fourth, stronger health data systems are needed. The crisis has accelerated innovative digital solutions and uses of digital data, smartphone applications to monitor quarantine, robotic devices, and artificial intelligence to track the virus and predict where it may appear next. Access to telemedicine has been made easier. Yet more can be done to leverage standardised national electronic health records to extract routine data for real-time disease surveillance, clinical trials, and health system management. Barriers to full deployment of telemedicine, the lack of real-time data, of interoperable clinical record data, of data linkage capability and sharing within health and with other sectors remain to be addressed.
Fifth, an effective vaccine and successful vaccination of populations around the globe will provide the only real exit strategy. Success is not guaranteed and there are many policy issues yet to be resolved. International cooperation is vital. Multilateral commitments to pay for successful candidates would give manufacturers certainty so that they can scale production and have vaccine doses ready as quickly as possible following marketing authorisation, but could also help ensure that vaccines go first to where they are most effective in ending the pandemic. Whilst leaders face political pressure to put the health of their citizens first, it is more effective to allocate vaccines based on need. More support is needed for multilateral access mechanisms that contain licensing commitments and ensure that intellectual property is no barrier to access, commitments to technology transfer for local production, and allocation of scarce doses based on need.
The pandemic offers huge opportunities to learn lessons for health system preparedness and resilience. Greater focus on anticipating responses, solidarity within and across countries, agility in managing responses, and renewed efforts for collaborative actions will be a better normal for the future.
OECD Economic Outlook 2020 , Volume 2020 Issue 1, No. 107, OECD Publishing, Paris
OECD Employment Outlook 2020 : Worker Security and the COVID-19 Crisis, OECD Publishing, Paris
OECD Health at a Glance 2019, OECD Publishing, Paris
https://www.un.org/pga/73/wp-content/uploads/sites/53/2019/07/FINAL-draft-UHC-Political-Declaration.pdf
OECD (2020), Who Cares? Attracting and Retaining Care Workers for the Elderly, OECD Health Policy Studies, OECD Publishing, Paris
Working for Health and Growth: investing in the health workforce . Report of the High-Level Commission on Health Employment and Economic Growth, Geneva.
Colombo F., Oderkirk J., Slawomirski L. (2020) Health Information Systems, Electronic Medical Records, and Big Data in Global Healthcare: Progress and Challenges in OECD Countries . In: Haring R., Kickbusch I., Ganten D., Moeti M. (eds) Handbook of Global Health. Springer, Cham.
2. Improving population health and building healthy societies in times of COVID-19
By Helena Legido-Quigley , Associate Professor, London School of Hygiene and Tropical Medicine
The COVID-19 pandemic has been a stark reminder of the fragility of population health worldwide; at time of writing, more than 1 million people have died from the disease. The pandemic has already made evident that those suffering most from COVID-19 belong to disadvantaged populations and marginalised communities. Deep-rooted inequalities have contributed adversely to the health status of different populations within and between countries. Besides the direct and indirect health impacts of COVID-19 and the decimation of health systems, restrictions on population movement and lockdowns introduced to combat the pandemic are expected to have economic and social consequences on an unprecedented scale .
Population health – and addressing the consequences of COVID-19 – is about improving the physical and mental health outcomes and wellbeing of populations locally, regionally and nationally, while reducing health inequalities.¹ Moreover, there is an increasing recognition that societal and environmental factors, such as climate change and food insecurity, can also influence population health outcomes.
The experiences of Maria, David, and Ruben – as told by Spanish public broadcaster RTVE – exemplify the real challenges that people living in densely populated urban areas have faced when being exposed to COVID-19.¹
Maria is a Mexican migrant who has just returned from Connecticut to the Bronx. Her partner Jorge died in Connecticut from COVID-19. She now has no income and is looking for an apartment for herself and her three children. When Jorge became ill, she took him to the hospital, but they would not admit him and he was sent away to be cared for by Maria at home with their children. When an ambulance eventually took him to hospital, it was too late. He died that same night, alone in hospital. She thinks he had diabetes, but he was never diagnosed. They only had enough income to pay the basic bills. Maria is depressed, she is alone, but she knows she must carry on for her children. Her 10-year old child says that if he could help her, he would work. After three months, she finds an apartment.
David works as a hairdresser and takes an overcrowded train every day from Leganés to Chamberi in the centre of Madrid. He lives in a small flat in San Nicasio, one of the poorest working-class areas of Madrid with one of the largest ageing populations in Spain. The apartments are very small, making it difficult to be in confinement, and all of David’s neighbours know somebody who has been a victim of COVID-19. His father was also a hairdresser. David's father was not feeling well; he was taken to hospital by ambulance, and he died three days later. David was not able to say goodbye to his father. Unemployment has increased in that area; small local shops are losing their customers, and many more people are expecting to lose their jobs.
Ruben lives in Iztapalapa in Mexico City with three children, a daughter-in-law and five grandchildren. Their small apartment has few amenities, and no running water during the evening. At three o’clock every morning, he walks 45 minutes with his mobile stall to sell fruit juices near the hospital. His daily earnings keep the family. He goes to the central market to buy fruit, taking a packed dirty bus. He thinks the city's central market was contaminated at the beginning of the pandemic, but it could not be closed as it is the main source of food in the country. He has no health insurance, and he knows that as a diabetic he is at risk, but medication for his condition is too expensive. He has no alternative but to go to work every day: "We die of hunger or we die of COVID."
These real stories highlight the issues that must be addressed to reduce persistent health inequalities and achieve health outcomes focusing on population health. The examples of Maria, David and Ruben show the terrible outcomes COVID-19 has had for people living in poverty and social deprivation, older people, and those with co-morbidities and/or pre-existing health conditions. All three live in densely populated urban areas with poor housing, and have to travel long distances in overcrowded transport. Maria’s loss of income has had consequences for her housing security and access to healthcare and health insurance, which will most likely lead to worse health conditions for her and her children. Furthermore, all three experienced high levels of stress, which is magnified in the cases of Maria and David who were unable to be present when their loved ones died.
The COVID-19 pandemic has made it evident that to improve the health of the population and build healthy societies, there is a need to shift the focus from illness to health and wellness in order to address the social, political and commercial determinants of health; to promote healthy behaviours and lifestyles; and to foster universal health coverage.² Citizens all over the world are demanding that health systems be strengthened and for governments to protect the most vulnerable. A better future could be possible with leadership that is able to carefully consider the long-term health, economic and social policies that are needed.
In order to design and implement population health-friendly policies, there are three prerequisites. First, there is a need to improve understanding of the factors that influence health inequalities and the interconnections between the economic, social and health impacts. Second, broader policies should be considered not only within the health sector, but also in other sectors such as education, employment, transport and infrastructure, agriculture, water and sanitation. Third, the proposed policies need to be designed through involving the community, addressing the health of vulnerable groups, and fostering inter-sectoral action and partnerships.
Finally, within the UN's Agenda 2030 , Sustainable Development Goal (SDG) 3 sets out a forward-looking strategy for health whose main goal is to attain healthier lives and wellbeing. The 17 interdependent SDGs offer an opportunity to contribute to healthier, fairer and more equitable societies from which both communities and the environment can benefit.
The stories of Maria, David and Ruben are real stories featured in the Documentary: The impact of COVID19 in urban outskirts, Directed by Jose A Guardiola. Available here. Permission has been granted to narrate these stories.
Buck, D., Baylis, A., Dougall, D. and Robertson, R. (2018). A vision for population health: Towards a healthier future . [online] London: The King's Fund. [Accessed 20 Sept. 2020]
Wilton Park. (2020). Healthy societies, healthy populations (WP1734). Wiston House, Steyning. Retrieved from https://www.wiltonpark.org.uk/event/wp1734/ Cohen B. E. (2006). Population health as a framework for public health practice: a Canadian perspective. American journal of public health , 96 (9), 1574–1576.
3. Imagine a 'well-care' system that invests in keeping people healthy
By Maliha Hashmi , Executive Director, Health and Well-Being and Biotech, NEOM, and Jan Kimpen , Global Chief Medical Officer, Philips
Imagine a patient named Emily. Emily is aged 32 and I’m her doctor.
Emily was 65lb (29kg) above her ideal body weight, pre-diabetic and had high cholesterol. My initial visit with Emily was taken up with counselling on lifestyle changes, mainly diet and exercise; typical advice from one’s doctor in a time-pressured 15-minute visit. I had no other additional resources, incentives or systems to support me or Emily to help her turn her lifestyle around.
I saw Emily eight months later, not in my office, but in the hospital emergency room. Her husband accompanied her – she was vomiting, very weak and confused. She was admitted to the intensive care unit, connected to an insulin drip to lower her blood sugar, and diagnosed with type 2 diabetes. I talked to Emily then, emphasizing that the new medications for diabetes would only control the sugars, but she still had time to reverse things if she changed her lifestyle. She received further counselling from a nutritionist.
Over the years, Emily continued to gain weight, necessitating higher doses of her diabetes medication. More emergency room visits for high blood sugars ensued, she developed infections of her skin and feet, and ultimately, she developed kidney disease because of the uncontrolled diabetes. Ten years after I met Emily, she is 78lb (35kg) above her ideal body weight; she is blind and cannot feel her feet due to nerve damage from the high blood sugars; and she will soon need dialysis for her failing kidneys. Emily’s deteriorating health has carried a high financial cost both for herself and the healthcare system. We have prevented her from dying and extended her life with our interventions, but each interaction with the medical system has come at significant cost – and those costs will only rise. But we have also failed Emily by allowing her diabetes to progress. We know how to prevent this, but neither the right investments nor incentives are in place.
Emily could have been a real patient of mine. Her sad story will be familiar to all doctors caring for chronically ill patients. Unfortunately, patients like Emily are neglected by health systems across the world today. The burden of chronic disease is increasing at alarming rates. Across the OECD nearly 33% of those over 15 years live with one or more chronic condition, rising to 60% for over-65s. Approximately 50% of chronic disease deaths are attributed to cardiovascular disease (CVD). In the coming decades, obesity, will claim 92 million lives in the OECD while obesity-related diseases will cut life expectancy by three years by 2050.
These diseases can be largely prevented by primary prevention, an approach that emphasizes vaccinations, lifestyle behaviour modification and the regulation of unhealthy substances. Preventative interventions have been efficacious. For obesity, countries have effectively employed public awareness campaigns, health professionals training, and encouragement of dietary change (for example, limits on unhealthy foods, taxes and nutrition labelling).⁴,⁵ Other interventions, such as workplace health-promotion programmes, while showing some promise, still need to demonstrate their efficacy.

The COVID-19 crisis provides the ultimate incentive to double down on the prevention of chronic disease. Most people dying from COVID-19 have one or more chronic disease, including obesity, CVD, diabetes or respiratory problems – diseases that are preventable with a healthy lifestyle. COVID-19 has highlighted structural weaknesses in our health systems such as the neglect of prevention and primary care.
While the utility of primary prevention is understood and supported by a growing evidence base, its implementation has been thwarted by chronic underinvestment, indicating a lack of societal and governmental prioritization. On average, OECD countries only invest 2.8% of health spending on public health and prevention. The underlying drivers include decreased allocation to prevention research, lack of awareness in populations, the belief that long-run prevention may be more costly than treatment, and a lack of commitment by and incentives for healthcare professionals. Furthermore, public health is often viewed in a silo separate from the overall health system rather than a foundational component.
Health benefits aside, increasing investment in primary prevention presents a strong economic imperative. For example, obesity contributes to the treatment costs of many other diseases: 70% of diabetes costs, 23% for CVD and 9% for cancers. Economic losses further extend to absenteeism and decreased productivity.
Fee-for-service models that remunerate physicians based on the number of sick patients they see, regardless the quality and outcome, dominate healthcare systems worldwide. Primary prevention mandates a payment system that reimburses healthcare professionals and patients for preventive actions. Ministries of health and governmental leaders need to challenge skepticism around preventive interventions, realign incentives towards preventive actions and those that promote healthy choices by people. Primary prevention will eventually reduce the burden of chronic diseases on the healthcare system.
As I reflect back on Emily and her life, I wonder what our healthcare system could have done differently. What if our healthcare system was a well-care system instead of a sick-care system? Imagine a different scenario: Emily, a 32 year old pre-diabetic, had access to a nutritionist, an exercise coach or health coach and nurse who followed her closely at the time of her first visit with me. Imagine if Emily joined group exercise classes, learned where to find healthy foods and how to cook them, and had access to spaces in which to exercise and be active. Imagine Emily being better educated about her diabetes and empowered in her healthcare and staying healthy. In reality, it is much more complicated than this, but if our healthcare systems began to incentivize and invest in prevention and even rewarded Emily for weight loss and healthy behavioural changes, the outcome might have been different. Imagine Emily losing weight and continuing to be an active and contributing member of society. Imagine if we invested in keeping people healthy rather than waiting for people to get sick, and then treating them. Imagine a well-care system.
Anderson, G. (2011). Responding to the growing cost and prevalence of people with multiple chronic conditions . Retrieved from OECD.
Institute for Health Metrics and Evaluation. GBD Data Visualizations. Retrieved here.
OECD (2019), The Heavy Burden of Obesity: The Economics of Prevention, OECD Health Policy Studies, OECD Publishing, Paris.
OECD. (2017). Obesity Update . Retrieved here.
Malik, V. S., Willett, W. C., & Hu, F. B. (2013). Global obesity: trends, risk factors and policy implications. Nature Reviews Endocrinology , 9 (1), 13-27.
Lang, J., Cluff, L., Payne, J., Matson-Koffman, D., & Hampton, J. (2017). The centers for disease control and prevention: findings from the national healthy worksite program. Journal of occupational and environmental medicine , 59 (7), 631.
Gmeinder, M., Morgan, D., & Mueller, M. (2017). How much do OECD countries spend on prevention? Retrieved from OECD.
Jordan RE, Adab P, Cheng KK. Covid-19: risk factors for severe disease and death. BMJ. 2020;368:m1198.
Richardson, A. K. (2012). Investing in public health: barriers and possible solutions. Journal of Public Health , 34 (3), 322-327.
Yong, P. L., Saunders, R. S., & Olsen, L. (2010). Missed Prevention Opportunities The healthcare imperative: lowering costs and improving outcomes: workshop series summary (Vol. 852): National Academies Press Washington, DC.
OECD. (2019). The Heavy Burden of Obesity: The Economics of Prevention. Retrieved here .
McDaid, D., F. Sassi and S. Merkur (Eds.) (2015a), “Promoting Health, Preventing Disease: The Economic Case ”, Open University Press, New York.
OECD. (2019). The Heavy Burden of Obesity: The Economics of Prevention. Retrieved from OECD.
4. Why e arly detection and diagnosis is critical
By Paul Murray , Head of Life and Health Products, Swiss Re, and André Goy , Chairman and Executive Director & Chief of Lymphoma, John Theurer Cancer Center, Hackensack University Medical Center
Although healthcare systems around the world follow a common and simple principle and goal – that is, access to affordable high-quality healthcare – they vary significantly, and it is becoming increasingly costly to provide this access, due to ageing populations, the increasing burden of chronic diseases and the price of new innovations.
Governments are challenged by how best to provide care to their populations and make their systems sustainable. Neither universal health, single payer systems, hybrid systems, nor the variety of systems used throughout the US have yet provided a solution. However, systems that are ranked higher in numerous studies, such as a 2017 report by the Commonwealth Fund , typically include strong prevention care and early-detection programmes. This alone does not guarantee a good outcome as measured by either high or healthy life expectancy. But there should be no doubt that prevention and early detection can contribute to a more sustainable system by reducing the risk of serious diseases or disorders, and that investing in and operationalizing earlier detection and diagnosis of key conditions can lead to better patient outcomes and lower long-term costs.
To discuss early detection in a constructive manner it makes sense to describe its activities and scope. Early detection includes pre-symptomatic screening and treatment immediately or shortly after first symptoms are diagnosed. Programmes may include searching for a specific disease (for example, HIV/AIDS or breast cancer), or be more ubiquitous. Prevention, which is not the focus of this blog, can be interpreted as any activities undertaken to avoid diseases, such as information programmes, education, immunization or health monitoring.
Expenditures for prevention and early detection vary by country and typically range between 1-5% of total health expenditures.¹ During the 2008 global financial crisis, many countries reduced preventive spending. In the past few years, however, a number of countries have introduced reforms to strengthen and promote prevention and early detection. Possibly the most prominent example in recent years was the introduction of the Affordable Care Act in the US, which placed a special focus on providing a wide range of preventive and screening services. It lists 63 distinct services that must be covered without any copayment, co-insurance or having to pay a deductible.

Whilst logic dictates that investment in early detection should be encouraged, there are a few hurdles and challenges that need to be overcome and considered. We set out a few key criteria and requirements for an efficient early detection program:
1. Accessibility The healthcare system needs to provide access to a balanced distribution of physicians, both geographically (such as accessibility in rural areas), and by specialty. Patients should be able to access the system promptly without excessive waiting times for diagnoses or elective treatments. This helps mitigate conditions or diseases that are already quite advanced or have been incubating for months or even years before a clinical diagnosis. Access to physicians varies significantly across the globe from below one to more than 60 physicians per 10,000 people.² One important innovation for mitigating access deficiencies is telehealth. This should give individuals easier access to health-related services, not only in cases of sickness but also to supplement primary care.
2. Early symptoms and initial diagnosis Inaccurate or delayed initial diagnoses present a risk to the health of patients, can lead to inappropriate or unnecessary testing and treatment, and represents a significant share of total health expenditures. A medical second opinion service, especially for serious medical diagnoses, which can occur remotely, can help improve healthcare outcomes. Moreover, studies show that early and correct diagnosis opens up a greater range of curative treatment options and can reduce costs (e.g. for colon cancer, stage-four treatment costs are a multiple of stage-one treatment costs).³
3. New technology New early detection technologies can improve the ability to identify symptoms and diseases early: i. Advances in medical monitoring devices and wearable health technology, such as ECG and blood pressure monitors and biosensors, enable patients to take control of their own health and physical condition. This is an important trend that is expected to positively contribute to early detection, for example in atrial fibrillation and Alzheimers’ disease. ii. Diagnostic tools, using new biomarkers such as liquid biopsies or volatile organic compounds, together with the implementation of machine learning, can play an increasing role in areas such as oncology or infectious diseases.⁴
4. Regulation and Intervention Government regulation and intervention will be necessary to set ranges of normality, to prohibit or discourage overdiagnosis and to reduce incentives for providers to overtreat patients or to follow patients' inappropriate requests. In some countries, such as the US, there has been some success through capitation models and value-based care. Governments might also need to intervene to de-risk the innovation paradigm, such that private providers of capital feel able to invest more in the development of new detection technologies, in addition to proven business models in novel therapeutics.
OECD Health Working Papers No. 101 "How much do OECD countries spend on prevention" , 2017
World Health Organization; Global Health Observatory (GHO) data; https://www.who.int/gho/health_workforce/physicians_density/en/
Saving lives, averting costs; A report for Cancer Research UK, by Incisive Health, September 2014
Liquid Biopsy: Market Drivers And Obstacles; by Divyaa Ravishankar, Frost & Sullivan, January 21, 2019
Liquid Biopsies Become Cheap and Easy with New Microfluidic Device; February 26, 2019
How America’s 5 Top Hospitals are Using Machine Learning Today; by Kumba Sennaar, February 19, 2019
5. The business case for private investment in healthcare for all
Pascal Fröhlicher, Primary Care Innovation Scholar, Harvard Medical School, and Ian Wijaya, Managing Director in Lazard’s Global Healthcare Group
Faith, a mother of two, has just lost another customer. Some households where she is employed to clean, in a small town in South Africa, have little understanding of her medical needs. As a type 2 diabetes patient, this Zimbabwean woman visits the public clinic regularly, sometimes on short notice. At her last visit, after spending hours in a queue, she was finally told that the doctor could not see her. To avoid losing another day of work, she went to the local general practitioner to get her script, paying more than three daily wages for consultation and medication. Sadly, this fictional person reflects a reality for many people in middle-income countries.
Achieving universal health coverage by 2030, a key UN Sustainable Development Goal (SDG), is at risk. The World Bank has identified a $176 billion funding gap , increasing every year due to the growing needs of an ageing population, with the health burden shifting towards non-communicable diseases (NCDs), now the major cause of death in emerging markets . Traditional sources of healthcare funding struggle to increase budgets sufficiently to cover this gap and only about 4% of private health care investments focus on diseases that primarily affect low- and middle-income countries.
In middle-income countries, private investors often focus on extending established businesses, including developing private hospital capacity, targeting consumers already benefiting from quality healthcare. As a result, an insufficient amount of private capital is invested in strengthening healthcare systems for everyone.

Why is this the case? We discussed with senior health executives investing in Lower and Middle Income Countries (LMIC) and the following reasons emerged:
- Small market size . Scaling innovations in healthcare requires dealing with country-specific regulatory frameworks and competing interest groups, resulting in high market entry cost.
- Talent . Several LMICs are losing nurses and doctors but also business and finance professionals to European and North American markets due to the lack of local opportunities and a significant difference in salaries.
- Untested business models with relatively low gross margins. Providing healthcare requires innovative business models where consumers’ willingness to pay often needs to be demonstrated over a significant period of time. Additionally, relatively low gross margins drive the need for scale to leverage administrative costs, which increases risk.
- Government Relations. The main buyer of health-related products and services is government; yet the relationship between public and private sectors often lacks trust, creating barriers to successful collaboration. Add to that significant political risk, as contracts can be cancelled by incoming administrations after elections. Many countries also lack comprehensive technology strategies to successfully manage technological innovation.
- Complexity of donor funding. A significant portion of healthcare is funded by private donors, whose priorities might not always be congruent with the health priorities of the government.
Notwithstanding these barriers, healthcare, specifically in middle-income settings, could present an attractive value proposition for private investors:
- Economic growth rates . A growing middle class is expanding the potential market for healthcare products and services.
- Alignment of incentives . A high ratio of out-of-pocket payments for healthcare services is often associated with low quality. However, innovative business models can turn out of pocket payments into the basis for a customer-centric value proposition, as the provider is required to compete for a share of disposable income.
- Emergence of National Health Insurance Schemes . South Africa, Ghana, Nigeria and others are building national health insurance schemes, increasing a population’s ability to fund healthcare services and products .
- Increased prevalence of NCDs. Given the increasing incidence of chronic diseases and the potential of using technology to address these diseases, new business opportunities for private investment exist.
Based on the context above, several areas in healthcare delivery can present compelling opportunities for private companies.
- Aggregation of existing players.
- Leveraging primary care infrastructure. Retail companies can leverage their real estate, infrastructure and supply chains to deploy primary care services at greater scale than is currently the case.
- Telemedicine . Telecommunications providers can leverage their existing infrastructure and customer base to provide payment mechanisms and telehealth services at scale. As seen during the COVID-19 pandemic, investment in telemedicine can ensure that patients receive timely and continuous care in spite of restrictions and lockdowns.
- Cost effective diagnostics . Diagnostic tools operated by frontline workers and combined with the expertise of specialists can provide timely and efficient care.
To fully realize these opportunities, government must incentivise innovation, provide clear regulatory frameworks and, most importantly, ensure that health priorities are adequately addressed.
Venture capital and private equity firms as well as large international corporations can identify the most commercially viable solutions and scale them into new markets. The ubiquity of NCDs and the requirement to reduce costs globally provides innovators with the opportunity to scale their tested solutions from LMICs to higher income environments.
Successful investment exits in LMICs and other private sector success stories will attract more private capital. Governments that enable and support private investment in their healthcare systems would, with appropriate governance and guidance, generate benefits to their populations and economies. The economic value of healthy populations has been proven repeatedly , and in the face of COVID-19, private sector investment can promote innovation and the development of responsible, sustainable solutions.
Faith – the diabetic mother we introduced at the beginning of this article - could keep her client. As a stable patient, she could measure her glucose level at home and enter the results in an app on her phone, part of her monthly diabetes programme with the company that runs the health centre. She visits the nurse-led facility at the local taxi stand on her way to work when her app suggests it. The nurse in charge of the centre treats Faith efficiently, and, if necessary, communicates with a primary care physician or even a specialist through the telemedicine functionality of her electronic health system.
Improving LMIC health systems is not only a business opportunity, but a moral imperative for public and private leaders. With the appropriate technology and political will, this can become a reality.
6. How could COVID-19 change the way we pay for health services?
John E. Ataguba, Associate Professor and Director, University of Cape Town and Matthew Guilford, Co-Founder and Chief Executive Officer, Common Health
The emergence of the new severe acute respiratory syndrome coronavirus (SARS-Cov-2), causing the coronavirus disease 2019 (COVID-19), has challenged both developing and developed countries.
Countries have approached the management of infections differently. Many people are curious to understand their health system’s performance on COVID-19, both at the national level and compared to international peers. Alongside limited resources for health, many developing countries may have weak health systems that can make it challenging to respond adequately to the pandemic.
Even before COVID-19, high rates of out-of-pocket spending on health meant that every year, 800 million people faced catastrophic healthcare costs ,100 million families were pushed into poverty, and millions more simply avoided care for critical conditions because they could not afford to pay for it.
The pandemic and its economic fallout have caused household incomes to decline at the same time as healthcare risks are rising. In some countries with insurance schemes, and especially for private health insurance, the following questions have arisen: How large is the co-payment for a COVID-19 test? If my doctor’s office is closed, will the telemedicine consultation be covered by my insurance? Will my coronavirus care be paid for regardless of how I contracted the virus? These and other doubts can prevent people from seeking medical care in some countries.
In Nigeria, like many other countries in Africa, the government bears the costs associated with testing and treating COVID-19 irrespective of the individual’s insurance status. In the public health sector, where COVID-19 cases are treated, health workers are paid monthly salaries while budgets are allocated to health facilities for other services. Hospitals continue to receive budget allocations to finance all health services including the management and treatment of COVID-19. That implies that funds allocated to address other health needs are reduced and that in turn could affect the availability and quality of health services.
Although health workers providing care for COVID-19 patients in isolation and treatment centres in Nigeria are paid salaries that are augmented with a special incentive package, the degree of impact on the quality improvement of services remains unclear. The traditional and historical allocation of budgets does not always address the needs of the whole population and could result in poor health services and under-provision of health services for COVID-19 patients.
In some countries, the reliance on out-of-pocket funding is hardly better for private providers, who encounter brand risks, operational difficulties, and – in extreme cases – the risk of creating “debtor prisons” as they seek to collect payment from patients. Ironically, despite the huge demand for medical services to diagnose and treat COVID-19, large healthcare institutions and individual healthcare practitioners alike are facing financial distress.
Dependence on a steady stream of fee-for-service payments for outpatient consultations and elective procedures is leading to pay cuts for doctors in India , forfeited Eid bonuses for nurses in Indonesia , and hospital bankruptcies in the United States . In a recent McKinsey & Company survey, 77% of physicians reported that their business would suffer in 2020 , and 46% were concerned about their practice surviving the coronavirus pandemic.
COVID-19 is exposing how fee-for-service, historical budget allocation and out-of-pocket financing methods can hinder the performance of the health system. Some providers and health systems that deployed “value-based” models prior to the pandemic have reported that these approaches have improved financial resilience during COVID-19 and may support better results for patients. Nevertheless, these types of innovations do not represent the dominant payment model in any country.
How health service providers are paid has implications for whether service users can get needed health services in a timely fashion, and at an appropriate quality and an affordable cost. By shifting from fee-for-service reimbursements to fixed "capitation" and performance-based payments, these models incentivize providers to improve quality and coordination while also guaranteeing a baseline income level, even during times of disruption.
Health service providers could be paid either in the form of salaries, a fee for services they provide, by capitation (whether adjusted or straightforward), through global budgets, or by using a case-based payment system (for example, the diagnostics-related groups), among others. Because there are different incentives to consider when adopting any of the methods, they could be combined to achieve a specific goal. For example, in some countries, health workers are paid salaries , and some specific services are paid on a fee-for-service basis.
Ideally, health services could be purchased strategically , incorporating aspects of provider performance in transferring funds to providers and accounting for the health needs of the population they serve.
In this regard, strategic purchasing for health has been advocated and should be highlighted as crucial with the emergence of the COVID-19 pandemic. There is a need to ensure value in the way health providers are paid, inter alia to increase efficiency, ensure equity, and improve access to needed health services. Value-based payment methods, although not new in many countries, provide an avenue to encourage long-term value for money, better quality, and strategic purchasing for health, helping to build a healthier, more resilient world.
7. L essons in integrated care from the COVID-19 pandemic
Sarah Ziegler, Postdoctoral Researcher, Department of Epidemiology and Biostatistics, University of Zurich, and Ninie Wang, Founder & CEO, Pinetree Care Group.
Since the start of the COVID-19 pandemic, people suffering non-communicable diseases (NCDs) have been at higher risk of becoming severely ill or dying. In Italy, 96.2% of people who died of COVID-19 lived with two or more chronic conditions.
Beyond the pandemic, cardiovascular disease, cancer, respiratory disease and diabetes are the leading burden of disease, with 41 million annual deaths. People with multimorbidity - a number of different conditions - often experience difficulties in accessing timely and coordinated healthcare, made worse when health systems are busy fighting against the pandemic.
Here is what happened in China with Lee, aged 62, who has been living with Chronic Obstructive Pulmonary Disease (COPD) for the past five years.
Before the pandemic, Lee’s care manager coordinated a multi-disciplinary team of physicians, nurses, pulmonary rehabilitation therapists, psychologists and social workers to put together a personalized care plan for her. Following the care plan, Lee stopped smoking and paid special attention to her diet, sleep and physical exercises, as well as sticking to her medication and follow-up visits. She participated in a weekly community-based physical activity program to meet other COPD patients, including short walks and exchange experiences. A mobile care team supported her with weekly cleaning and grocery shopping.
Together with her family, Lee had follow-up visits to ensure her care plan reflected her recovery and to modify the plan if needed. These integrated care services brought pieces of care together, centered around Lee’s needs, and provided a continuum of care that helped keep Lee in the community with a good quality of life for as long as possible.
Since the COVID-19 outbreak, such NCD services have been disrupted by lockdowns, the cancellation of elective care and the fear of visiting care service . These factors particularly affected people living with NCDs like Lee. As such, Lee was not able to follow her care plan anymore. The mobile care team was unable to visit her weekly as they were deployed to provide COVID-19 relief. Lee couldn’t participate in her community-based program, follow up on her daily activities, or see her family or psychologists. This negatively affected Lee’s COPD management and led to poor management of her physical activity and healthy diet.
The pandemic highlights the need for a flexible and reliable integrated care system to enable healthcare delivery to all people no matter where they live, uzilizing approaches such as telemedicine and effective triaging to overcome care disruptions.
Lee’s care manager created short videos to assist her family through each step of her care and called daily to check in on the implementation of the plan and answer questions. Lee received tele-consultations, and was invited to the weekly webcast series that supported COPD patient communities. When her uncle passed away because of pneumonia complications from COVID-19 in early April, Lee’s care manager arranged a palliative care provider to support the family through the difficult time of bereavement and provided food and supplies during quarantine. Lee could even continue with her physical activity program with an online training coach. There were a total of 38 exercise videos for strengthening and stretching arms, legs and trunk, which she could complete at different levels of difficulty and with different numbers of repetitions.
Lee’s case demonstrates that early detection, prevention, and management of NCDs play a crucial role in a global pandemic response. It shows how we need to shift away from health systems designed around single diseases towards health systems designed for the multidimensional needs of individuals. As part of the pandemic responses, addressing and managing risks related to NCDs and prevention of their complications are critical to improve outcomes for vulnerable people like Lee.
How to design and deliver successful integrated care
The challenge for the successful transformation of healthcare is to tailor care system-wide to population needs. A 2016 WHO Framework on integrated people-centered health services developed a set of five general strategies for countries to progress towards people-centered and sustainable health systems, calling for a fundamental transformation not only in the way health services are delivered, but also in the way they are financed and managed . These strategies call for countries to:
- Engage and empower people / communities: an integrated care system must mobilize everyone to work together using all available resources, especially when continuity of essential health and community services for NCDs are at risk of being undermined.
- Strengthen governance and accountability, so that integration emphasizes rather than weakens leadership in every part of the system, and ensure that NCDs are included in national COVID-19 plans and future essential health services.
- Reorient the model of care to put the needs and perspectives of each person / family at the center of care planning and outcome measurement, rather than institutions.
- Coordinate services within and across sectors, for example, integrate inter-disciplinary medical care with social care, addressing wider socio-economic, environmental and behavioral determinants of health.
- Create an enabling environment, with clear objectives, supportive financing, regulations and insurance coverage for integrated care, including the development and use of systemic digital health care solutions.
Whether due to an unexpected pandemic or a gradual increase in the burden of NCDs, each person could face many health threats across the life-course.
Only systems that dynamically assess each person’s complex health needs and address them through a timely, well-coordinated and tailored mix of health and social care services will be able to deliver desired health outcomes over the longer term, ensuring an uninterrupted good quality of life for Lee and many others like her.
- Wang B, Li R, Lu Z, Huang Y. Does comorbidity increase the risk of patients with COVID-19: evidence from meta-analysis. Aging (Albany NY) 2020;12: 6049–57.
- WHO. Noncommunicable diseases in emergencies. Geneva: World Health Organization, 2016.
- WHO. COVID-19 significantly impacts health services for noncommunicable diseases. June 2020.
- Kluge HHP, Wickramasinghe K, Rippin HL, et al. Prevention and control of non-communicalbe diseases in the COVID-19 response. The Lancet. 2020. 395:1678-1680
- WHO. Framework on integrated people-centred health services. Geneva: World Health Organization, 2016.

8 . Why access to healthcare alone will not save lives
Donald Berwick, President Emeritus and Senior Fellow, Institute for Healthcare Improvement; Nicola Bedlington, Special Adviser, European Patient Forum; and David Duong, Director, Program in Global Primary Care and Social Change, Harvard Medical School.
Joyce lies next to 10 other women in bare single beds in the post-partum recovery room at a rural hospital in Uganda. Just an hour ago, Joyce gave birth to a healthy baby boy. She is now struggling with abdominal pain. A nurse walks by, and Joyce tries to call out, but the nurse was too busy to attend to her; she was the only nurse looking after 20 patients.
Another hour passes, and Joyce is shaking and sweating profusely. Joyce’s husband runs into the corridor to find a nurse to come and evaluate her. The nurse notices Joyce’s critical condition - a high fever and a low blood pressure - and she quickly calls the doctor. The medical team rushes Joyce to the intensive care unit. Joyce has a very severe blood stream infection. It takes another hour before antibiotics are started - too late. Joyce dies, leaving behind a newborn son and a husband. Joyce, like many before her, falls victim to a pervasive global threat: poor quality of care.
Adopted by United Nations (UN) in 2015, the Sustainable Development Goals (SDG) are a universal call to action to end poverty, protect the planet and ensure that all enjoy peace and prosperity by 2030. SDG 3 aims to ensure healthy lives and promote wellbeing for all. The 2019 UN General Assembly High Level Meeting on Universal Health Coverage (UHC) reaffirmed the need for the highest level of political commitment to health care for all.
However, progress towards UHC, often measured in terms of access, not outcomes, does not guarantee better health, as we can see from Joyce’s tragedy. This is also evident with the COVID-19 response. The rapidly evolving nature of the COVID-19 pandemic has highlighted long-term structural inefficiencies and inequities in health systems and societies trying to mitigate the contagion and loss of life.
Systems are straining under significant pressure to ensure standards of care for both COVID-19 patients and other patients that run the risk of not receiving timely and appropriate care. Although poor quality of care has been a long-standing issue, it is imperative now more than ever that systems implement high-quality services as part of their efforts toward UHC.
Poor quality healthcare remains a challenge for countries at all levels of economic development: 10% of hospitalized patients acquire an infection during their hospitalization in low-and-middle income countries (LMIC), whereas 7% do in high-income countries. Poor quality healthcare disproportionally affects the poor and those in LMICs. Of the approximately 8.6 million deaths per year in 137 LMICs, 3.6 million are people who did not access the health system, whereas 5 million are people who sought and had access to services but received poor-quality care.
Joyce’s story is all too familiar; poor quality of care results in deaths from treatable diseases and conditions. Although the causes of death are often multifactorial, deaths and increased morbidity from treatable conditions are often a reflection of defects in the quality of care.
The large number of deaths and avoidable complications are also accompanied by substantial economic costs. In 2015 alone, 130 LMICs faced US $6 trillion in economic losses. Although there is concern that implementing quality measures may be a costly endeavor, it is clear that the economic toll associated with a lack of quality of care is far more troublesome and further stunts the socio-economic development of LMICs, made apparent with the COVID-19 pandemic.
Poor-quality care not only leads to adverse outcomes in terms of high morbidity and mortality, but it also impacts patient experience and patient confidence in health systems. Less than one-quarter of people in LMICs and approximately half of people in high-income countries believe that their health systems work well.
A lack of application and availability of evidenced-based guidelines is one key driver of poor-quality care. The rapidly changing landscape of medical knowledge and guidelines requires healthcare workers to have immediate access to current clinical resources. Despite our "information age", health providers are not accessing clinical guidelines or do not have access to the latest practical, lifesaving information.
Getting information to health workers in the places where it is most needed is a delivery challenge. Indeed, adherence to clinical practice guidelines in eight LMICs was below 50%, and in OECD countries, despite being a part of national guidelines, 19-53% of women aged 50-69 years did not receive mammography screening.4 The evidence in LMICs and HICs suggest that application of evidence-based guidelines lead to reduction in mortality and improved health outcomes.
Equally, the failure to change and continually improve the processes in health systems that support the workforce takes a high toll on quality of care. During the initial wave of the COVID-19 pandemic, countries such as Taiwan, Hong Kong, Singapore and Vietnam, which adapted and improved their health systems after the SARS and H1N1 outbreaks, were able to rapidly mobilize a large-scale quarantine and contact tracing strategy, supported with effective and coordinated mass communication.
These countries not only mitigated the economic and mortality damage, but also prevented their health systems and workforce from enduring extreme burden and inability to maintain critical medical supplies. In all nations, investing in healthcare organizations to enable them to become true “learning health care systems,” aiming at continual quality improvement, would yield major population health and health system gains.
The COVID-19 pandemic underscores the importance for health systems to be learning systems. Once the dust settles, we need to focus, collectively, on learning from this experience and adapting our health systems to be more resilient for the next one. This implies a need for commitment to and investment in global health cooperation, improvement in health care leadership, and change management.
With strong political and financial commitment to UHC, and its demonstrable effect in addressing crises such as COVID-19, for the first time, the world has a viable chance of UHC becoming a reality. However, without an equally strong political, managerial, and financial commitment to continually improving, high-quality health services, UHC will remain an empty promise.
1. United Nations General Assembly. Political declaration of the high-level meeting on universal health coverage. New York, NY2019.
2. Marmot M, Allen J, Boyce T, Goldblatt P, Morrison J. Health equity in England: the Marmot review 10 years on. Institute of Health Equity;2020.
3. National Academies of Sciences, Engineering, and Medicine: Committee on Improving the Quality of Health Care Globally. Crossing the global quality chasm: Improving health care worldwide. Washington, DC: National Academies Press;2018.
4. World Health Organization, Organization for Economic Co-operation and Development, World Bank Group. Delivering quality health services: a global imperative for universal health coverage. World Health Organization; 2018.
5. Kruk ME, Gage AD, Arsenault C, et al. High-quality health systems in the Sustainable Development Goals era: time for a revolution. The Lancet Global Health. 2018;6(11):e1196-e1252.
6. Ricci-Cabello I, Violán C, Foguet-Boreu Q, Mounce LT, Valderas JM. Impact of multi-morbidity on quality of healthcare and its implications for health policy, research and clinical practice. A scoping review. European Journal of General Practice. 2015;21(3):192-202.
7. Valtis YK, Rosenberg J, Bhandari S, et al. Evidence-based medicine for all: what we can learn from a programme providing free access to an online clinical resource to health workers in resource-limited settings. BMJ global health. 2016;1(1).
8. Institute of Medicine. Best Care at Lower Cost: The Path to Continuously Learning Health Care in America . Washington, DC: National Academies Press 2012.
Select Your Interests
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
- Download PDF
- Share X Facebook Email LinkedIn
- Permissions
Confronting Challenges in the US Health Care System : Potential Opportunity in a Time of Crisis
- 1 Deputy Editor, JAMA Health Forum
- 2 Department of Health Policy, Vanderbilt University School of Medicine, Nashville, Tennessee
- Editorial The Near-Term Future of Health Care Reform Ezekiel J. Emanuel, MD, PhD JAMA
- Editorial Crucial Questions for US Health Policy in the Next Decade John Z. Ayanian, MD, MPP JAMA
The sheer number of challenges facing the Biden Administration and the 117th Congress in the health policy sphere is staggering, as is the range of potential solutions offered by the authors of the Viewpoints in the JAMA Health Policy series. 1 The most pressing challenges involve addressing the global COVID-19 pandemic. Yet policy makers would be remiss if they did not leverage this opportunity to also address the fundamental problems with the US health system laid bare by the nation’s response to the pandemic. These include major challenges related to health insurance coverage, the solvency of publicly funded programs, the stability of the health care safety net, market power and consolidation, inequities in health care access and outcomes, public health infrastructure, and the failure to effectively use technology to help counteract these problems.
Personal health crises, such as experiencing a myocardial infarction, can spur patients and their care teams to work to improve underlying health habits and conditions that contributed to the health event. Similarly, the havoc wrought by the COVID-19 pandemic is a clarion call to improve US health care coverage, financing, and organization. The status quo practices of the health system in the US—like poor health habits of a patient with heart disease—have left it susceptible to poor outcomes.
The high cost of the US health care system is its biggest weakness. In the US, national expenditures on health care goods and services were approximately $4 trillion in 2020, accounting for an estimated 18% of gross domestic product. 2 High prices for care explain a large part of the difference in spending between the US and other developed countries. Surprise billing is just one aspect of the pricing problem, but one that, as Colla 3 describes, illustrates many troubling trends in medicine. Consolidation of hospitals, insurers, and large and small practices has accelerated during the pandemic and as Dafny 4 explains, can be expected to lead to higher prices in the commercial market in the future. Chernew 5 elegantly discusses how market power and consolidation in the health care industry, exacerbated by the pandemic, could lead to still higher prices and a cycle of harms for individuals, governments, and society as a whole.
Those harms include incomplete insurance coverage, both in terms of numbers of people covered and the generosity of that coverage, due to high prices that lead to high insurance premiums. Higher premiums have meant that many people who are not eligible for subsidies on the health insurance exchanges find insurance unaffordable. The Biden campaign proposals to extend subsidies to higher income groups are designed to help solve this problem but will not address its root causes. High premiums have also contributed to wage stagnation for US workers with employment-based health insurance and to higher cost-sharing, which has been shown to reduce access to necessary care.
In addition, higher health care costs put pressure on state and federal budgets. As Gee et 6 al discuss, 12 states have not chosen to expand Medicaid to date, and a concern that even being responsible for 10% of the increased costs could be burdensome is one of the reasons cited for this choice. Frank and Neuman 7 emphasize that the looming deficits in the Medicare Part A Trust Fund will also put pressure on federal policy makers to find sources of new revenues or to cut benefits or payment rates. Perhaps even more important, as described by Venkataramani and colleagues, 8 high health care prices contribute to limited budgets for other social goods like education and housing that could improve health outcomes, possibly even more than direct spending on health care.
Similarly, it is now clear that the US has spent an increasing amount of resources on health care, but spending on public health has been inadequate. Investments in surveillance officers and systems and in stockpiles of equipment and medications are less appealing ways to spend public resources than covering new drugs or services. The pandemic has revealed the shortcomings of the US public health infrastructure and illustrates that neglecting to reinvest in public health after a pandemic will more severely compromise the ability to respond effectively to the next public health crisis. 9 Although none of the Viewpoints in this series focused on specific public health proposals, they should be part of every discussion of improving health and health care going forward. Public health policy must be central not only to health policy, but to economic policy and national security policy as well.
High health care prices might be less of a problem if the US health care system was uniformly delivering high-quality care and yielding high value. The US does prioritize health as a society and voters are reluctant to endorse solutions that limit access to the latest innovations in health care. However, a fundamental shortcoming in the US health care system is the tendency to create and perpetuate incentives to deliver higher-margin treatments and specialty care instead of primary care, preventive care, and public health. The central need to refine the focus on value was highlighted in many articles in the series.
Several Viewpoints in the Health Policy series provided worthy suggestions and policy recommendations the could help the US health care system recover from the current crises stronger. Berwick and Gilfillan 10 call for speeding the cycle time of demonstrations under the Center for Medicare and Medicaid Innovation, Dafny 4 suggests examining mergers and acquisitions more closely, and Chernew 5 proposes implementing “backstop” prices in commercial markets.
Another important step will be using data and technology strategically. During the pandemic, the health care system rapidly adopted telemedicine in clinical care. Millions of people accessed readily available data dashboards that illustrated the course of the pandemic and the extent of infections in specific areas, and many used the information to demand better and more equal care. As described by Adler-Milstein, 11 a digital transformation in the US health care system could make it possible to continuously monitor and use real-time data to inform preparedness and population-level care planning. Such data systems also could be used to help address and reduce disparities and inequities in care and to improve health system transparency, including around prices. Moreover, these systems could save money and reduce the reporting and patient tracking burdens on health care centers, physicians, and other clinicians participating in value-based care; administrative costs are estimated by Kocher et al 12 at $2500 per person per year.
Can commitments to improving health care coverage, financing, and organization be made in the midst of a pandemic and an affordability crisis? There are reasons to hope the answer is yes. The pandemic has substantially changed care patterns, shown the risks of fee-for-service payment and a reliance on highly reimbursed surgical procedures, and revealed the need for a stronger public health infrastructure and greater preparedness. Health systems will be increasingly held accountable for ensuring delivery of high-value care and for addressing health equity issues in ways that do not rely on outdated models of care. No one could have imagined or would wish the current economic, societal, or health care challenges of the COVID-19 pandemic on a new administration or Congress. But all have hope that leaders can confront these crises as potential opportunities for developing solutions to address the ongoing major challenges in the US health care system.
Correction: This article was updated on June 7, 2021, to correct the spelling of Dr Venkataramani’s name in the fifth paragraph.
Corresponding Author: Melinda B. Buntin, PhD, Department of Health Policy, Vanderbilt University School of Medicine, 2525 West End Ave, Ste 1200, Nashville, TN 37203 ( [email protected] ).
Conflict of Interest Disclosures: Dr Buntin reported being an unpaid board member of the Harvard Medical Faculty Practice in Boston, Massachusetts.
See More About
Buntin MB. Confronting Challenges in the US Health Care System : Potential Opportunity in a Time of Crisis . JAMA. 2021;325(14):1399–1400. doi:10.1001/jama.2021.1471
Manage citations:
© 2024
Artificial Intelligence Resource Center
Cardiology in JAMA : Read the Latest
Browse and subscribe to JAMA Network podcasts!
Others Also Liked
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts

Health Care Comes Home: The Human Factors (2011)
Chapter: 7 conclusions and recommendations.
7 Conclusions and Recommendations
Health care is moving into the home increasingly often and involving a mixture of people, a variety of tasks, and a broad diversity of devices and technologies; it is also occurring in a range of residential environments. The factors driving this migration include the rising costs of providing health care; the growing numbers of older adults; the increasing prevalence of chronic disease; improved survival rates of various diseases, injuries, and other conditions (including those of fragile newborns); large numbers of veterans returning from war with serious injuries; and a wide range of technological innovations. The health care that results varies considerably in its safety, effectiveness, and efficiency, as well as its quality and cost.
The committee was charged with examining this major trend in health care delivery and resulting challenges from only one of many perspectives: the study of human factors. From the outset it was clear that the dramatic and evolving change in health care practice and policies presents a broad array of opportunities and problems. Consequently the committee endeavored to maintain focus specifically on how using the human factors approach can provide solutions that support maximizing the safety and quality of health care delivered in the home while empowering both care recipients and caregivers in the effort.
The conclusions and recommendations presented below reflect the most critical steps that the committee thinks should be taken to improve the state of health care in the home, based on the literature reviewed in this report examined through a human factors lens. They are organized into four areas: (1) health care technologies, including medical devices and health information technologies involved in health care in the home; (2)
caregivers and care recipients; (3) residential environments for health care; and (4) knowledge gaps that require additional research and development. Although many issues related to home health care could not be addressed, applications of human factors principles, knowledge, and research methods in these areas could make home health care safer and more effective and also contribute to reducing costs. The committee chose not to prioritize the recommendations, as they focus on various aspects of health care in the home and are of comparable importance to the different constituencies affected.
HEALTH CARE TECHNOLOGIES
Health care technologies include medical devices that are used in the home as well as information technologies related to home-based health care. The four recommendations in this area concern (1) regulating technologies for health care consumers, (2) developing guidance on the structure and usability of health information technologies, (3) developing guidance and standards for medical device labeling, and (4) improving adverse event reporting systems for medical devices. The adoption of these recommendations would improve the usability and effectiveness of technology systems and devices, support users in understanding and learning to use them, and improve feedback to government and industry that could be used to further improve technology for home care.
Ensuring the safety of emerging technologies is a challenge, in part because it is not always clear which federal agency has regulatory authority and what regulations must be met. Currently, the U.S. Food and Drug Administration (FDA) has responsibility for devices, and the Office of the National Coordinator for Health Information Technology (ONC) has similar authority with respect to health information technology. However, the dividing line between medical devices and health information technology is blurring, and many new systems and applications are being developed that are a combination of the two, although regulatory oversight has remained divided. Because regulatory responsibility for them is unclear, these products may fall into the gap.
The committee did not find a preponderance of evidence that knowledge is lacking for the design of safe and effective devices and technologies for use in the home. Rather than discovering an inadequate evidence base, we were troubled by the insufficient attention directed at the development of devices that account, necessarily and properly, for users who are inadequately trained or not trained at all. Yet these new users often must
rely on equipment without ready knowledge about limitations, maintenance requirements, and problems with adaptation to their particular home settings.
The increased prominence of the use of technology in the health care arena poses predictable challenges for many lay users, especially people with low health literacy, cognitive impairment, or limited technology experience. For example, remote health care management may be more effective when it is supported by technology, and various electronic health care (“e-health”) applications have been developed for this purpose. With the spectrum of caregivers ranging from individuals caring for themselves or other family members to highly experienced professional caregivers, computer-based care management systems could offer varying levels of guidance, reminding, and alerting, depending on the sophistication of the operator and the criticality of the message. However, if these technologies or applications are difficult to understand or use, they may be ignored or misused, with potentially deleterious effects on care recipient health and safety. Applying existing accessibility and usability guidelines and employing user-centered design and validation methods in the development of health technology products designed for use in the home would help ensure that they are safe and effective for their targeted user populations. In this effort, it is important to recognize how the line between medical devices and health information technologies has become blurred while regulatory oversight has remained distinct, and it is not always clear into which domain a product falls.
Recommendation 1. The U.S. Food and Drug Administration and the Office of the National Coordinator for Health Information Technology should collaborate to regulate, certify, and monitor health care applications and systems that integrate medical devices and health information technologies. As part of the certification process, the agencies should require evidence that manufacturers have followed existing accessibility and usability guidelines and have applied user-centered design and validation methods during development of the product.
Guidance and Standards
Developers of information technologies related to home-based health care, as yet, have inadequate or incomplete guidance regarding product content, structure, accessibility, and usability to inform innovation or evolution of personal health records or of care recipient access to information in electronic health records.
The ONC, in the initial announcement of its health information technology certification program, stated that requirements would be forthcom-
ing with respect both to personal health records and to care recipient access to information in electronic health records (e.g., patient portals). Despite the importance of these requirements, there is still no guidance on the content of information that should be provided to patients or minimum standards for accessibility, functionality, and usability of that information in electronic or nonelectronic formats.
Consequently, some portals have been constructed based on the continuity of care record. However, recent research has shown that records and portals based on this model are neither understandable nor interpretable by laypersons, even by those with a college education. The lack of guidance in this area makes it difficult for developers of personal health records and patient portals to design systems that fully address the needs of consumers.
Recommendation 2. The Office of the National Coordinator for Health Information Technology, in collaboration with the National Institute of Standards and Technology and the Agency for Healthcare Research and Quality, should establish design guidelines and standards, based on existing accessibility and usability guidelines, for content, accessibility, functionality, and usability of consumer health information technologies related to home-based health care.
The committee found a serious lack of adequate standards and guidance for the labeling of medical devices. Furthermore, we found that the approval processes of the FDA for changing these materials are burdensome and inflexible.
Just as many medical devices currently in use by laypersons in the home were originally designed and approved for use only by professionals in formal health care facilities, the instructions for use and training materials were not designed for lay users, either. The committee recognizes that lack of instructional materials for lay users adds to the level of risk involved when devices are used by populations for whom they were not intended.
Ironically, the FDA’s current premarket review and approval processes inadvertently discourage manufacturers from selectively revising or developing supplemental instructional and training materials, when they become aware that instructional and training materials need to be developed or revised for lay users of devices already approved and marketed. Changing the instructions for use (which were approved with the device) requires manufacturers to submit the device along with revised instructions to the FDA for another 510(k) premarket notification review. Since manufacturers can find these reviews complicated, time-consuming, and expensive, this requirement serves as a disincentive to appropriate revisions of instructional or training materials.
Furthermore, little guidance is currently available on design of user
training methods and materials for medical devices. Even the recently released human factors standard on medical device design (Association for the Advancement of Medical Instrumentation, 2009), while reasonably comprehensive, does not cover the topic of training or training materials. Both FDA guidance and existing standards that do specifically address the design of labeling and ensuing instructions for use fail to account for up-to-date findings from research on instructional systems design. In addition, despite recognition that requirements for user training, training materials, and instructions for use are different for lay and professional users of medical equipment, these differences are not reflected in current standards.
Recommendation 3. The U.S. Food and Drug Administration (FDA) should promote development (by standards development organizations, such as the International Electrotechnical Commission, the International Organization for Standardization, the American National Standards Institute, and the Association for the Advancement of Medical Instrumentation) of new standards based on the most recent human factors research for the labeling of and ensuing instructional materials for medical devices designed for home use by lay users. The FDA should also tailor and streamline its approval processes to facilitate and encourage regular improvements of these materials by manufacturers.
Adverse Event Reporting Systems
The committee notes that the FDA’s adverse event reporting systems, used to report problems with medical devices, are not user-friendly, especially for lay users, who generally are not aware of the systems, unaware that they can use them to report problems, and uneducated about how to do so. In order to promote safe use of medical devices in the home and rectify design problems that put care recipients at risk, it is necessary that the FDA conduct more effective postmarket surveillance of medical devices to complement its premarket approval process. The most important elements of their primarily passive surveillance system are the current adverse event reporting mechanisms, including Maude and MedSun. Entry of incident data by health care providers and consumers is not straightforward, and the system does not elicit data that could be useful to designers as they develop updated versions of products or new ones that are similar to existing devices. The reporting systems and their importance need to be widely promoted to a broad range of users, especially lay users.
Recommendation 4. The U.S. Food and Drug Administration should improve its adverse event reporting systems to be easier to use, to collect data that are more useful for identifying the root causes of events
related to interactions with the device operator, and to develop and promote a more convenient way for lay users as well as professionals to report problems with medical devices.
CAREGIVERS IN THE HOME
Health care is provided in the home by formal caregivers (health care professionals), informal caregivers (family and friends), and individuals who self-administer care; each type of caregiver faces unique issues. Properly preparing individuals to provide care at home depends on targeting efforts appropriately to the background, experience, and knowledge of the caregivers. To date, however, home health care services suffer from being organized primarily around regulations and payments designed for inpatient or outpatient acute care settings. Little attention has been given to how different the roles are for formal caregivers when delivering services in the home or to the specific types of training necessary for appropriate, high-quality practice in this environment.
Health care administration in the home commonly involves interaction among formal caregivers and informal caregivers who share daily responsibility for a person receiving care. But few formal caregivers are given adequate training on how to work with informal caregivers and involve them effectively in health decision making, use of medical or adaptive technologies, or best practices to be used for evaluating and supporting the needs of caregivers.
It is also important to recognize that the majority of long-term care provided to older adults and individuals with disabilities relies on family members, friends, or the individual alone. Many informal caregivers take on these responsibilities without necessary education or support. These individuals may be poorly prepared and emotionally overwhelmed and, as a result, experience stress and burden that can lead to their own morbidity. The committee is aware that informational and training materials and tested programs already exist to assist informal caregivers in understanding the many details of providing health care in the home and to ease their burden and enhance the quality of life of both caregiver and care recipient. However, tested materials and education, support, and skill enhancement programs have not been adequately disseminated or integrated into standard care practices.
Recommendation 5. Relevant professional practice and advocacy groups should develop appropriate certification, credentialing, and/or training standards that will prepare formal caregivers to provide care in the home, develop appropriate informational and training materials
for informal caregivers, and provide guidance for all caregivers to work effectively with other people involved.
RESIDENTIAL ENVIRONMENTS FOR HEALTH CARE
Health care is administered in a variety of nonclinical environments, but the most common one, particularly for individuals who need the greatest level and intensity of health care services, is the home. The two recommendations in this area encourage (1) modifications to existing housing and (2) accessible and universal design of new housing. The implementation of these recommendations would be a good start on an effort to improve the safety and ease of practicing health care in the home. It could improve the health and safety of many care recipients and their caregivers and could facilitate adherence to good health maintenance and treatment practices. Ideally, improvements to housing design would take place in the context of communities that provide transportation, social networking and exercise opportunities, and access to health care and other services.
Safety and Modification of Existing Housing
The committee found poor appreciation of the importance of modifying homes to remove health hazards and barriers to self-management and health care practice and, furthermore, that financial support from federal assistance agencies for home modifications is very limited. The general connection between housing characteristics and health is well established. For example, improving housing conditions to enhance basic sanitation has long been part of a public health response to acute illness. But the characteristics of the home can present significant barriers to autonomy or self-care management and present risk factors for poor health, injury, compromised well-being, and greater dependence on others. Conversely, physical characteristics of homes can enhance resident safety and ability to participate in daily self-care and to utilize effectively health care technologies that are designed to enhance health and well-being.
Home modifications based on professional home assessments can increase functioning, contribute to reducing accidents such as falls, assist caregivers, and enable chronically ill persons and people with disabilities to stay in the community. Such changes are also associated with facilitating hospital discharges, decreasing readmissions, reducing hazards in the home, and improving care coordination. Familiar modifications include installation of such items as grab bars, handrails, stair lifts, increased lighting, and health monitoring equipment as well as reduction of such hazards as broken fixtures and others caused by insufficient home maintenance.
Deciding on which home modifications have highest priority in a given
setting depends on an appropriate assessment of circumstances and the environment. A number of home assessment instruments and programs have been validated and proven to be effective to meet this need. But even if needed modifications are properly identified and prioritized, inadequate funding, gaps in services, and lack of coordination between the health and housing service sectors have resulted in a poorly integrated system that is difficult to access. Even when accessed, progress in making home modifications available has been hampered by this lack of coordination and inadequate reimbursement or financial mechanisms, especially for those who cannot afford them.
Recommendation 6. Federal agencies, including the U.S. Department of Health and Human Services and the Centers for Medicare & Medicaid Services, along with the U.S. Department of Housing and Urban Development and the U.S. Department of Energy, should collaborate to facilitate adequate and appropriate access to health- and safety-related home modifications, especially for those who cannot afford them. The goal should be to enable persons whose homes contain obstacles, hazards, or features that pose a home safety concern, limit self-care management, or hinder the delivery of needed services to obtain home assessments, home modifications, and training in their use.
Accessibility and Universal Design of New Housing
Almost all existing housing in the United States presents problems for conducting health-related activities because physical features limit independent functioning, impede caregiving, and contribute to such accidents as falls. In spite of the fact that a large and growing number of persons, including children, adults, veterans, and older adults, have disabilities and chronic conditions, new housing continues to be built that does not account for their needs (current or future). Although existing homes can be modified to some extent to address some of the limitations, a proactive, preventive, and effective approach would be to plan to address potential problems in the design phase of new and renovated housing, before construction.
Some housing is already required to be built with basic accessibility features that facilitate practice of health care in the home as a result of the Fair Housing Act Amendments of 1998. And 17 states and 30 cities have passed what are called “visitability” codes, which currently apply to 30,000 homes. Some localities offer tax credits, such as Pittsburgh through an ordinance, to encourage installing visitability features in new and renovated housing. The policy in Pittsburgh was impetus for the Pennsylvania Residential VisitAbility Design Tax Credit Act signed into law on October 28, 2006, which offers property owners a tax credit for new construction
and rehabilitation. The Act paves the way for municipalities to provide tax credits to citizens by requiring that such governing bodies administer the tax credit (Self-Determination Housing Project of Pennsylvania, Inc., n.d.).
Visitability, rather than full accessibility, is characterized by such limited features as an accessible entry into the home, appropriately wide doorways and one accessible bathroom. Both the International Code Council, which focuses on building codes, and the American National Standards Institute, which establishes technical standards, including ones associated with accessibility, have endorsed voluntary accessibility standards. These standards facilitate more jurisdictions to pass such visitability codes and encourage legislative consistency throughout the country. To date, however, the federal government has not taken leadership to promote compliance with such standards in housing construction, even for housing for which it provides financial support.
Universal design, a broader and more comprehensive approach than visitability, is intended to suit the needs of persons of all ages, sizes, and abilities, including individuals with a wide range of health conditions and activity limitations. Steps toward universal design in renovation could include such features as anti-scald faucet valve devices, nonslip flooring, lever handles on doors, and a bedroom on the main floor. Such features can help persons and their caregivers carry out everyday tasks and reduce the incidence of serious and costly accidents (e.g., falls, burns). In the long run, implementing universal design in more homes will result in housing that suits the long-term needs of more residents, provides more housing choices for persons with chronic conditions and disabilities, and causes less forced relocation of residents to more costly settings, such as nursing homes.
Issues related to housing accessibility have been acknowledged at the federal level. For example, visitability and universal design are in accord with the objectives of the Safety of Seniors Act (Public Law No. 110-202, passed in 2008). In addition, implementation of the Olmstead decision (in which the U.S. Supreme Court ruled that the Americans with Disabilities Act may require states to provide community-based services rather than institutional placements for individuals with disabilities) requires affordable and accessible housing in the community.
Visitability, accessibility, and universal design of housing all are important to support the practice of health care in the home, but they are not broadly implemented and incentives for doing so are few.
Recommendation 7. Federal agencies, such as the U.S. Department of Housing and Urban Development, the U.S. Department of Veterans Affairs, and the Federal Housing Administration, should take a lead role, along with states and local municipalities, to develop strategies that promote and facilitate increased housing visitability, accessibil-
ity, and universal design in all segments of the market. This might include tax and other financial incentives, local zoning ordinances, model building codes, new products and designs, and related policies that are developed as appropriate with standards-setting organizations (e.g., the International Code Council, the International Electrotechnical Commission, the International Organization for Standardization, and the American National Standards Institute).
RESEARCH AND DEVELOPMENT
In our review of the research literature, the committee learned that there is ample foundational knowledge to apply a human factors lens to home health care, particularly as improvements are considered to make health care safe and effective in the home. However, much of what is known is not being translated effectively into practice, neither in design of equipment and information technology or in the effective targeting and provision of services to all those in need. Consequently, the four recommendations that follow support research and development to address knowledge and communication gaps and facilitate provision of high-quality health care in the home. Specifically, the committee recommends (1) research to enhance coordination among all the people who play a role in health care practice in the home, (2) development of a database of medical devices in order to facilitate device prescription, (3) improved surveys of the people involved in health care in the home and their residential environments, and (4) development of tools for assessing the tasks associated with home-based health care.
Health Care Teamwork and Coordination
Frail elders, adults with disabilities, disabled veterans, and children with special health care needs all require coordination of the care services that they receive in the home. Home-based health care often involves a large number of elements, including multiple care providers, support services, agencies, and complex and dynamic benefit regulations, which are rarely coordinated. However, coordinating those elements has a positive effect on care recipient outcomes and costs of care. When successful, care coordination connects caregivers, improves communication among caregivers and care recipients and ensures that receivers of care obtain appropriate services and resources.
To ensure safe, effective, and efficient care, everyone involved must collaborate as a team with shared objectives. Well-trained primary health care teams that execute customized plans of care are a key element of coordinated care; teamwork and communication among all actors are also
essential to successful care coordination and the delivery of high-quality care. Key factors that influence the smooth functioning of a team include a shared understanding of goals, common information (such as a shared medication list), knowledge of available resources, and allocation and coordination of tasks conducted by each team member.
Barriers to coordination include insufficient resources available to (a) help people who need health care at home to identify and establish connections to appropriate sources of care, (b) facilitate communication and coordination among caregivers involved in home-based health care, and (c) facilitate communication among the people receiving and the people providing health care in the home.
The application of systems analysis techniques, such as task analysis, can help identify problems in care coordination systems and identify potential intervention strategies. Human factors research in the areas of communication, cognitive aiding and decision support, high-fidelity simulation training techniques, and the integration of telehealth technologies could also inform improvements in care coordination.
Recommendation 8 . The Agency for Healthcare Research and Quality should support human factors–based research on the identified barriers to coordination of health care services delivered in the home and support user-centered development and evaluation of programs that may overcome these barriers.
Medical Device Database
It is the responsibility of physicians to prescribe medical devices, but in many cases little information is readily available to guide them in determining the best match between the devices available and a particular care recipient. No resource exists for medical devices, in contrast to the analogous situation in the area of assistive and rehabilitation technologies, for which annotated databases (such as AbleData) are available to assist the provider in determining the most appropriate one of several candidate devices for a given care recipient. Although specialists are apt to receive information about devices specific to the area of their practice, this is much less likely in the case of family and general practitioners, who often are responsible for selecting, recommending, or prescribing the most appropriate device for use at home.
Recommendation 9. The U.S. Food and Drug Administration, in collaboration with device manufacturers, should establish a medical device database for physicians and other providers, including pharmacists, to use when selecting appropriate devices to prescribe or recommend
for people receiving or self-administering health care in the home. Using task analysis and other human factors approaches to populate the medical device database will ensure that it contains information on characteristics of the devices and implications for appropriate care recipient and device operator populations.
Characterizing Caregivers, Care Recipients, and Home Environments
As delivery of health care in the home becomes more common, more coherent strategies and effective policies are needed to support the workforce of individuals who provide this care. Developing these will require a comprehensive understanding of the number and attributes of individuals engaged in health care in the home as well as the context in which care is delivered. Data and data analysis are lacking to accomplish this objective.
National data regarding the numbers of individuals engaged in health care delivery in the home—that is, both formal and informal caregivers—are sparse, and the estimates that do exist vary widely. Although the Bureau of Labor Statistics publishes estimates of the number of workers employed in the home setting for some health care classifications, they do not include all relevant health care workers. For example, data on workers employed directly by care recipients and their families are notably absent. Likewise, national estimates of the number of informal caregivers are obtained from surveys that use different methodological approaches and return significantly different results.
Although numerous national surveys have been designed to answer a broad range of questions regarding health care delivery in the home, with rare exceptions such surveys reflect the relatively limited perspective of the sponsoring agency. For example,
- The Medicare Current Beneficiary Survey (administered by the Centers for Medicare & Medicaid Services) and the Health and Retirement Survey (administered by the National Institute on Aging) are primarily geared toward understanding the health, health services use, and/or economic well-being of older adults and provide no information regarding working-age adults or children or information about home or neighborhood environments.
- The Behavioral Risk Factors Surveillance Survey (administered by the Centers for Disease Control and Prevention, CDC), the National Health Interview Survey (administered by the CDC), and the National Children’s Study (administered by the U.S. Department of Health and Human Services and the U.S. Environmental Protection Agency) all collect information on health characteristics, with limited or no information about the housing context.
- The American Housing Survey (administered by the U.S. Department of Housing and Urban Development) collects detailed information regarding housing, but it does not include questions regarding the health status of residents and does not collect adequate information about home modifications and features on an ongoing basis.
Consequently, although multiple federal agencies collect data on the sociodemographic and health characteristics of populations and on the nation’s housing stock, none of these surveys collects data necessary to link the home, its residents, and the presence of any caregivers, thus limiting understanding of health care delivered in the home. Furthermore, information is altogether lacking about health and functioning of populations linked to the physical, social, and cultural environments in which they live. Finally, in regard to individuals providing care, information is lacking regarding their education, training, competencies, and credentialing, as well as appropriate knowledge about their working conditions in the home.
Better coordination across government agencies that sponsor such surveys and more attention to information about health care that occurs in the home could greatly improve the utility of survey findings for understanding the prevalence and nature of health care delivery in the home.
Recommendation 10. Federal health agencies should coordinate data collection efforts to capture comprehensive information on elements relevant to health care in the home, either in a single survey or through effective use of common elements across surveys. The surveys should collect data on the sociodemographic and health characteristics of individuals receiving care in the home, the sociodemographic attributes of formal and informal caregivers and the nature of the caregiving they provide, and the attributes of the residential settings in which the care recipients live.
Tools for Assessing Home Health Care Tasks and Operators
Persons caring for themselves or others at home as well as formal caregivers vary considerably in their skills, abilities, attitudes, experience, and other characteristics, such as age, culture/ethnicity, and health literacy. In turn, designers of health-related devices and technology systems used in the home are often naïve about the diversity of the user population. They need high-quality information and guidance to better understand user capabilities relative to the task demands of the health-related device or technology that they are developing.
In this environment, valid and reliable tools are needed to match users with tasks and technologies. At this time, health care providers lack the
tools needed to assess whether particular individuals would be able to perform specific health care tasks at home, and medical device and system designers lack information on the demands associated with health-related tasks performed at home and the human capabilities needed to perform them successfully.
Whether used to assess the characteristics of formal or informal caregivers or persons engaged in self-care, task analysis can be used to develop point-of-care tools for use by consumers and caregivers alike in locations where such tasks are encouraged or prescribed. The tools could facilitate identification of potential mismatches between the characteristics, abilities, experiences, and attitudes that an individual brings to a task and the demands associated with the task. Used in ambulatory care settings, at hospital discharge or other transitions of care, and in the home by caregivers or individuals and family members themselves, these tools could enable assessment of prospective task performer’s capabilities in relation to the demands of the task. The tools might range in complexity from brief screening checklists for clinicians to comprehensive assessment batteries that permit nuanced study and tracking of home-based health care tasks by administrators and researchers. The results are likely to help identify types of needed interventions and support aids that would enhance the abilities of individuals to perform health care tasks in home settings safely, effectively, and efficiently.
Recommendation 11. The Agency for Healthcare Research and Quality should collaborate, as necessary, with the National Institute for Disability and Rehabilitation Research, the National Institutes of Health, the U.S. Department of Veterans Affairs, the National Science Foundation, the U.S. Department of Defense, and the Centers for Medicare & Medicaid Services to support development of assessment tools customized for home-based health care, designed to analyze the demands of tasks associated with home-based health care, the operator capabilities required to carry them out, and the relevant capabilities of specific individuals.
Association for the Advancement of Medical Instrumentation. (2009). ANSI/AAMI HE75:2009: Human factors engineering: Design of medical devices. Available: http://www.aami.org/publications/standards/HE75_Ch16_Access_Board.pdf [April 2011].
Self-Determination Housing Project of Pennsylvania, Inc. (n.d.) Promoting visitability in Pennsylvania. Available: http://www.sdhp.org/promoting_visitability_in_pennsy.htm [March 30, 2011].
In the United States, health care devices, technologies, and practices are rapidly moving into the home. The factors driving this migration include the costs of health care, the growing numbers of older adults, the increasing prevalence of chronic conditions and diseases and improved survival rates for people with those conditions and diseases, and a wide range of technological innovations. The health care that results varies considerably in its safety, effectiveness, and efficiency, as well as in its quality and cost.
Health Care Comes Home reviews the state of current knowledge and practice about many aspects of health care in residential settings and explores the short- and long-term effects of emerging trends and technologies. By evaluating existing systems, the book identifies design problems and imbalances between technological system demands and the capabilities of users. Health Care Comes Home recommends critical steps to improve health care in the home. The book's recommendations cover the regulation of health care technologies, proper training and preparation for people who provide in-home care, and how existing housing can be modified and new accessible housing can be better designed for residential health care. The book also identifies knowledge gaps in the field and how these can be addressed through research and development initiatives.
Health Care Comes Home lays the foundation for the integration of human health factors with the design and implementation of home health care devices, technologies, and practices. The book describes ways in which the Agency for Healthcare Research and Quality (AHRQ), the U.S. Food and Drug Administration (FDA), and federal housing agencies can collaborate to improve the quality of health care at home. It is also a valuable resource for residential health care providers and caregivers.
READ FREE ONLINE
Welcome to OpenBook!
You're looking at OpenBook, NAP.edu's online reading room since 1999. Based on feedback from you, our users, we've made some improvements that make it easier than ever to read thousands of publications on our website.
Do you want to take a quick tour of the OpenBook's features?
Show this book's table of contents , where you can jump to any chapter by name.
...or use these buttons to go back to the previous chapter or skip to the next one.
Jump up to the previous page or down to the next one. Also, you can type in a page number and press Enter to go directly to that page in the book.
Switch between the Original Pages , where you can read the report as it appeared in print, and Text Pages for the web version, where you can highlight and search the text.
To search the entire text of this book, type in your search term here and press Enter .
Share a link to this book page on your preferred social network or via email.
View our suggested citation for this chapter.
Ready to take your reading offline? Click here to buy this book in print or download it as a free PDF, if available.
Get Email Updates
Do you enjoy reading reports from the Academies online for free ? Sign up for email notifications and we'll let you know about new publications in your areas of interest when they're released.
Access to Healthcare in the United States Essay
One of humanity’s biggest challenges is preventing harm to human beings by providing accessible health to everyone in the world. Thus, many governments struggle with that task. The recent COVID-19 pandemic further strained many countries’ healthcare systems and revealed many issues. However, these challenges also suggest solutions, exposing the problem areas. The US specifically struggles with the inequality and lack of consistent quality in healthcare across the nation. According to Randy Oostra, five numbers that determine the life and death of a person are zip codes. In other words, the location and socioeconomic status connected to this location predict the health outcomes of the whole community because of the nature of the government’s financing and spending. Thus, the most important solution is to redistribute the funding of the healthcare system to ensure equality of access and better quality of care.
The social aspect is a more significant determinant of health than the physical under the US healthcare system. Randy Oostra describes the lives of the average US citizen from birth to death. Along this journey, the zip code and socioeconomic position of the family and community is the major factor in their health, from infant physical conditions to adult obesity to senior care. In other words, the US is divided into zones along the lines of prosperity, which determines one’s weight, health conditions, and even longevity. The overall physical health correlates with the income levels in the community, including the most striking example, obesity. Randy Oostra emphasizes that the US government spends six trillion, yet thirty million people are uninsured. The lack of health insurance in the US means a lack of accessible healthcare. Therefore, the gap in health outcomes arises under these conditions. As the access to healthcare remains a basic human right, the US needs to redistribute its enormous government spending budget to favor more socially equal healthcare outcomes and better quality.
- Differences of Entire Us Demography as Compared That One of Zip Code 60614
- Zip Auto Parts Company's International Expansion
- Benefits of Zip Lock Bags to Keep Fresh Cereals
- The Efficacy of Maryland’s “All-Payer” Model
- US Centers for Disease Control and Prevention
- Health and Medicine: National Health Service
- Montefiore Medical Center's Patient Engagement Activities
- Change Leadership: Telehealth Technology at Orlando Health
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2023, July 2). Access to Healthcare in the United States. https://ivypanda.com/essays/access-to-healthcare-in-the-united-states/
"Access to Healthcare in the United States." IvyPanda , 2 July 2023, ivypanda.com/essays/access-to-healthcare-in-the-united-states/.
IvyPanda . (2023) 'Access to Healthcare in the United States'. 2 July.
IvyPanda . 2023. "Access to Healthcare in the United States." July 2, 2023. https://ivypanda.com/essays/access-to-healthcare-in-the-united-states/.
1. IvyPanda . "Access to Healthcare in the United States." July 2, 2023. https://ivypanda.com/essays/access-to-healthcare-in-the-united-states/.
Bibliography
IvyPanda . "Access to Healthcare in the United States." July 2, 2023. https://ivypanda.com/essays/access-to-healthcare-in-the-united-states/.
A .gov website belongs to an official government organization in the United States.
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- About Health Effects of Cigarette Smoking
- Secondhand Smoke
- E-cigarettes (Vapes)
- Menthol Tobacco Products
- Morbidity and Mortality Weekly Reports (MMWR)
- About Surveys
- Other Tobacco Products
- Smoking and Tobacco Use Features
- Patient Care Settings and Smoking Cessation
- Patient Care
- Funding Opportunity Announcements
- State and Community Work
- National and State Tobacco Control Program
- Multimedia and Tools
- Tobacco - Health Equity
- Tobacco - Surgeon General's Reports
- State Tobacco Activities Tracking and Evaluation (STATE) System
- Global Tobacco Control
Health Effects of Vaping
At a glance.
Learn more about the health effects of vaping.
- No tobacco products, including e-cigarettes, are safe.
- Most e-cigarettes contain nicotine, which is highly addictive and is a health danger for pregnant people, developing fetuses, and youth. 1
- Aerosol from e-cigarettes can also contain harmful and potentially harmful substances. These include cancer-causing chemicals and tiny particles that can be inhaled deep into lungs. 1
- E-cigarettes should not be used by youth, young adults, or people who are pregnant. E-cigarettes may have the potential to benefit adults who smoke and are not pregnant if used as a complete substitute for all smoked tobacco products. 2 3 4
- Scientists still have a lot to learn about the short- and long-term health effects of using e-cigarettes.
Most e-cigarettes, or vapes, contain nicotine, which has known adverse health effects. 1
- Nicotine is highly addictive. 1
- Nicotine is toxic to developing fetuses and is a health danger for pregnant people. 1
- Acute nicotine exposure can be toxic. Children and adults have been poisoned by swallowing, breathing, or absorbing vaping liquid through their skin or eyes. More than 80% of calls to U.S. poison control centers for e-cigarettes are for children less than 5 years old. 5
Nicotine poses unique dangers to youth because their brains are still developing.
- Nicotine can harm brain development which continues until about age 25. 1
- Youth can start showing signs of nicotine addiction quickly, sometimes before the start of regular or daily use. 1
- Using nicotine during adolescence can harm the parts of the brain that control attention, learning, mood, and impulse control. 1
- Adolescents who use nicotine may be at increased risk for future addiction to other drugs. 1 6
- Youth who vape may also be more likely to smoke cigarettes in the future. 7 8 9 10 11 12
Other potential harms of e-cigarettes
E-cigarette aerosol can contain substances that can be harmful or potentially harmful to the body. These include: 1
- Nicotine, a highly addictive chemical that can harm adolescent brain development
- Cancer-causing chemicals
- Heavy metals such as nickel, tin, and lead
- Tiny particles that can be inhaled deep into the lungs
- Volatile organic compounds
- Flavorings such as diacetyl, a chemical linked to a serious lung disease. Some flavorings used in e-cigarettes may be safe to eat but not to inhale because the lungs process substances differently than the gut.
E-cigarette aerosol generally contains fewer harmful chemicals than the deadly mix of 7,000 chemicals in smoke from cigarettes. 7 13 14 However, this does not make e-cigarettes safe. Scientists are still learning about the immediate and long-term health effects of using e-cigarettes.
Dual use refers to the use of both e-cigarettes and regular cigarettes. Dual use is not an effective way to safeguard health. It may result in greater exposure to toxins and worse respiratory health outcomes than using either product alone. 2 3 4 15
Some people who use e-cigarettes have experienced seizures. Most reports to the Food and Drug Administration (FDA ) have involved youth or young adults. 16 17
E-cigarettes can cause unintended injuries. Defective e-cigarette batteries have caused fires and explosions, some of which have resulted in serious injuries. Most explosions happened when the batteries were being charged.
Anyone can report health or safety issues with tobacco products, including e-cigarettes, through the FDA Safety Reporting Portal .
Health effects of vaping for pregnant people
The use of any tobacco product, including e-cigarettes, is not safe during pregnancy. 1 14 Scientists are still learning about the health effects of vaping on pregnancy and pregnancy outcomes. Here's what we know now:
- Most e-cigarettes, or vapes, contain nicotine—the addictive substance in cigarettes, cigars, and other tobacco products. 18
- Nicotine is a health danger for pregnant people and is toxic to developing fetuses. 1 14
- Nicotine can damage a fetus's developing brain and lungs. 13
- E-cigarette use during pregnancy has been associated with low birth weight and pre-term birth. 19 20
Nicotine addiction and withdrawal
Nicotine is the main addictive substance in tobacco products, including e-cigarettes. With repeated use, a person's brain gets used to having nicotine. This can make them think they need nicotine just to feel okay. This is part of nicotine addiction.
Signs of nicotine addiction include craving nicotine, being unable to stop using it, and developing a tolerance (needing to use more to feel the same). Nicotine addiction can also affect relationships with family and friends and performance in school, at work, or other activities.
When someone addicted to nicotine stops using it, their body and brain have to adjust. This can result in temporary symptoms of nicotine withdrawal which may include:
- Feeling irritable, jumpy, restless, or anxious
- Feeling sad or down
- Having trouble sleeping
- Having a hard time concentrating
- Feeling hungry
- Craving nicotine
Withdrawal symptoms fade over time as the brain gets used to not having nicotine.
Nicotine addiction and mental health
Nicotine addiction can harm mental health and be a source of stress. 21 22 23 24 More research is needed to understand the connection between vaping and mental health, but studies show people who quit smoking cigarettes experience: 25
- Lower levels of anxiety, depression, and stress
- Improved positive mood and quality of life
Mental health is a growing concern among youth. 26 27 Youth vaping and cigarette use are associated with mental health symptoms such as depression. 22 28
The most common reason middle and high school students give for currently using e-cigarettes is, "I am feeling anxious, stressed, or depressed." 29 Nicotine addiction or withdrawal can contribute to these feelings or make them worse. Youth may use tobacco products to relieve their symptoms, which can lead to a cycle of nicotine addiction.
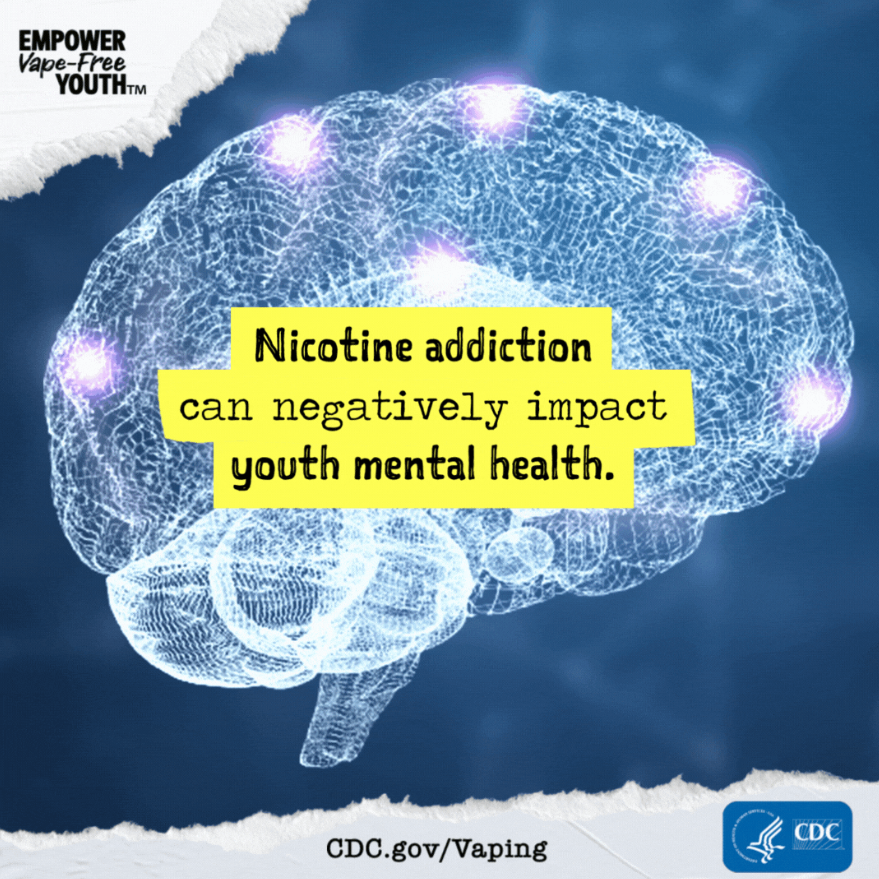
- U.S. Department of Health and Human Services. E-Cigarette Use Among Youth and Young Adults: A Report of the Surgeon General . Centers for Disease Control and Prevention; 2016. Accessed Feb 14, 2024.
- Goniewicz ML, Smith DM, Edwards KC, et al. Comparison of nicotine and toxicant exposure in users of electronic cigarettes and combustible cigarettes . JAMA Netw Open. 2018;1(8):e185937.
- Reddy KP, Schwamm E, Kalkhoran S, et al. Respiratory symptom incidence among people using electronic cigarettes, combustible tobacco, or both . Am J Respir Crit Care Med. 2021;204(2):231–234.
- Smith DM, Christensen C, van Bemmel D, et al. Exposure to nicotine and toxicants among dual users of tobacco cigarettes and e-cigarettes: Population Assessment of Tobacco and Health (PATH) Study, 2013-2014 . Nicotine Tob Res. 2021;23(5):790–797.
- Tashakkori NA, Rostron BL, Christensen CH, Cullen KA. Notes from the field: e-cigarette–associated cases reported to poison centers — United States, April 1, 2022–March 31, 2023 . MMWR Morb Mortal Wkly Rep. 2023;72:694–695.
- Yuan M, Cross SJ, Loughlin SE, Leslie FM. Nicotine and the adolescent brain . J Physiol. 2015;593(16):3397–3412.
- National Academies of Sciences, Engineering, and Medicine. Public Health Consequences of E-Cigarettes . The National Academies Press; 2018.
- Barrington-Trimis JL, Kong G, Leventhal AM, et al. E-cigarette use and subsequent smoking frequency among adolescents . Pediatrics. 2018;142(6):e20180486.
- Barrington-Trimis JL, Urman R, Berhane K, et al. E-cigarettes and future cigarette use . Pediatrics. 2016;138(1):e20160379.
- Bunnell RE, Agaku IT, Arrazola RA, et al. Intentions to smoke cigarettes among never-smoking US middle and high school electronic cigarette users: National Youth Tobacco Survey, 2011-2013 . Nicotine Tob Res. 2015;17(2):228–235.
- Soneji S, Barrington-Trimis JL, Wills TA, et al. Association between initial use of e-cigarettes and subsequent cigarette smoking among adolescents and young adults: a systematic review and meta-analysis . JAMA Pediatr. 2017;171(8):788–797.
- Sun R, Méndez D, Warner KE. Association of electronic cigarette use by U.S. adolescents with subsequent persistent cigarette smoking . JAMA Netw Open. 2023;6(3):e234885.
- U.S. Department of Health and Human Services. How Tobacco Smoke Causes Disease: The Biology and Behavioral Basis for Smoking-Attributable Disease . Centers for Disease Control and Prevention; 2010. Accessed Feb 13, 2024.
- U.S. Department of Health and Human Services. The Health Consequences of Smoking: 50 Years of Progress. A Report of the Surgeon General . Centers for Disease Control and Prevention; 2014. Accessed Feb 12, 2024.
- Mukerjee R, Hirschtick JL, LZ Arciniega, et al. ENDS, cigarettes, and respiratory illness: longitudinal associations among U.S. youth . AJPM. Published online Dec 2023.
- Faulcon LM, Rudy S, Limpert J, Wang B, Murphy I. Adverse experience reports of seizures in youth and young adult electronic nicotine delivery systems users . J Adolesc Health . 2020;66(1):15–17.
- U.S. Food and Drug Administration. E-cigarette: Safety Communication - Related to Seizures Reported Following E-cigarette Use, Particularly in Youth and Young Adults . U.S. Department of Health and Human Services; 2019. Accessed Feb 14, 2024.
- Marynak KL, Gammon DG, Rogers T, et al. Sales of nicotine-containing electronic cigarette products: United States, 2015 . Am J Public Health . 2017;107(5):702-705.
- Regan AK, Bombard JM, O'Hegarty MM, Smith RA, Tong VT. Adverse birth outcomes associated with prepregnancy and prenatal electronic cigarette use . Obstet Gynecol. 2021;138(1):85–94.
- Regan AK, Pereira G. Patterns of combustible and electronic cigarette use during pregnancy and associated pregnancy outcomes . Sci Rep. 2021;11(1):13508.
- Kutlu MG, Parikh V, Gould TJ. Nicotine addiction and psychiatric disorders . Int Rev Neurobiol. 2015;124:171–208.
- Obisesan OH, Mirbolouk M, Osei AD, et al. Association between e-cigarette use and depression in the Behavioral Risk Factor Surveillance System, 2016-2017 . JAMA Netw Open. 2019;2(12):e1916800.
- Prochaska JJ, Das S, Young-Wolff KC. Smoking, mental illness, and public health . Annu Rev Public Health. 2017;38:165–185.
- Wootton RE, Richmond RC, Stuijfzand BG, et al. Evidence for causal effects of lifetime smoking on risk for depression and schizophrenia: a Mendelian randomisation study . Psychol Med. 2020;50(14):2435–2443.
- Taylor G, McNeill A, Girling A, Farley A, Lindson-Hawley N, Aveyard P. Change in mental health after smoking cessation: systematic review and meta-analysis . BMJ. 2014;348:g1151.
- Centers for Disease Control and Prevention. Youth Risk Behavior Survey Data Summary & Trends Report: 2011–2021 . U.S. Department of Health and Human Services; 2023. Accessed Dec 15, 2023.
- U.S. Department of Health and Human Services. Protecting Youth Mental Health: The U.S. Surgeon General's Advisory . Office of the Surgeon General; 2021. Accessed Jan 5, 2024.
- Lechner WV, Janssen T, Kahler CW, Audrain-McGovern J, Leventhal AM. Bi-directional associations of electronic and combustible cigarette use onset patterns with depressive symptoms in adolescents . Prev Med. 2017;96:73–78.
- Gentzke AS, Wang TW, Cornelius M, et al. Tobacco product use and associated factors among middle and high school students—National Youth Tobacco Survey, United States, 2021 . MMWR Surveill Summ. 2022;71(No. SS-5):1–29.
Smoking and Tobacco Use
Commercial tobacco use is the leading cause of preventable disease, disability, and death in the United States.
For Everyone
Health care providers, public health.
- Open access
- Published: 24 May 2024
For the rural curious: mixed methods evaluation of a rural pharmacy practice elective
- Timothy P. Stratton 1
BMC Medical Education volume 24 , Article number: 573 ( 2024 ) Cite this article
88 Accesses
Metrics details
As of 2020, 20% of people residing in the United States of America (U.S.) lived in rural communities. Despite rural residents tending to be older, poorer, and having greater disease burden than their urban counterparts, the number of rural primary care providers continues to decline. Nearly 66% of U.S. Primary Care Health Professional Shortage Areas are designated as rural. Pharmacists can help address this shortage of rural primary care providers, often serving as providers of first-contact care; however, only 12% of U.S. pharmacists practice in rural communities. To help address this gap, in 2022 an elective Rural Pharmacy course was created at the University of Minnesota College of Pharmacy by a faculty member who has rural practice experience.
The course combines formal lectures, guest presentations by rural pharmacists and student interviews with additional rural pharmacists. For the 42 students enrolled in the course in 2022 and 2023, non-parametric statistics were used to compare the percentage of students who were raised in rural communities or who otherwise had extensive exposure to rural, and compare student interest ratings (1 to 7) about practicing/living rural at the beginning and end of the course. Students also wrote end-of-course reflection papers, commenting on the course and their interviews with rural pharmacists.
Across both years, 45% of the enrolled students had previous experience in rural communities. The net change in Rural Interest scores among students completing both questionnaires was + 5 in 2022 and + 2 in 2023, both non-significant differences. The largest shifts in student interest were from “Not Sure” at the start of the course to “Interested” or “Not Interested” at the end of the course, and from “Interested” to “Very Interested.” In their reflection papers nearly 60% of students reported being most impressed by their interviews with rural pharmacists.
Conclusions
A course addressing the benefits and challenges of practicing pharmacy in rural communities was well-received by pharmacy students. Even students who have little interest in living in a rural community can benefit from being introduced to rural culture, enabling them to provide more culturally-responsive care for patients from rural communities.
Peer Review reports
Introduction
The Unites States (U.S.) Census Bureau redefined “rural” for the 2020 census as communities with populations of fewer than 5,000 people (fewer than 2,000 housing units) and located more than 1.5 miles (2.4 km) from a high-density urban area. Based on this revised definition, 20% of the U.S. population in 2020 lived in rural communities [ 1 ]. The percentage of rural residents varied greatly by region, with only 11% of people in the West Region residing in rural areas, followed by 16% in the Northeast Region, 24% in the South Region and 26% in the Midwest Region [ 2 ]. At the extremes, fewer than 6% of people in California lived in rural areas, while nearly 65% of Vermont residents lived in rural areas [ 1 ]. In contrast, as of 2021 the U.S. Bureau of Labor Statistics reported that only 12% of the nation’s pharmacists practiced in nonmetro (rural) communities [ 3 ].
On average, rural residents tend to be older [ 4 ], poorer [ 5 ], experience greater disease burden [ 6 ] and lack health insurance or be underinsured [ 7 ] than residents of urban communities. The average age and disease burden among rural residents is increasing due to outmigration of young adults from rural to urban communities and the in-migration of older adults to rural communities following retirement [ 4 ]. Yet as the proportion of older residents in rural communities continues to increase, the availability of primary care providers in rural communities continues to decrease. Nearly 66% of Primary Care Health Professional Shortage Areas in 2023 are designated as rural [ 8 ]. Pharmacists can be part of the solution to address the existing and anticipated shortage of primary care providers in rural communities [ 9 ]. Rural pharmacists often serve as “providers of first-contact care” for patients who are seeking to self-treat a health condition [ 10 ]. Where self-treatment is inappropriate, the pharmacist is in a position to refer the patient to appropriate professional care.
This paper describes a new course taught in the Doctor of Pharmacy (PharmD) program in the University of Minnesota College of Pharmacy that introduces students to the unique benefits and challenges of practicing pharmacy in rural communities.
One college, two campuses
The University of Minnesota (UMN) is a public, research-intensive (Carnegie R1) institution. The UMN College of Pharmacy opened on the Minneapolis campus in 1892 [ 11 ]. Prior to 2003, the College of Pharmacy included four departments: Experimental & Clinical Pharmacology, Medicinal Chemistry, Pharmaceutics, and Pharmacy Care & Health Systems. However, to address a shortage of pharmacists in Greater Minnesota – counties outside of the seven-county Minneapolis-St. Paul Twin Cities Metro Area [ 12 ] – in 2003 the College of Pharmacy expanded its program 150 miles (241 km) north to Duluth on the University of Minnesota Duluth campus, adding a fifth department to the College, Pharmacy Practice and Pharmaceutical Sciences (PPPS).
The specific multi-campus model used by the UMN College of Pharmacy is somewhat unique among multi-campus pharmacy programs in the U.S. The PPPS department includes faculty representing Biochemistry and each of the major Pharmacy disciplines (Clinical Pharmacy, Medicinal Chemistry, Pharmaceutics, Pharmacology, Pharmacy Practice, and Social & Administrative Pharmacy). Didactic courses within the College are taught using videoconferencing technology, with classroom presentations/lectures originating from either Minneapolis or Duluth and being broadcast to the other campus.
The mission of the PPPS department includes preparing pharmacists to provide patient care in rural and Indigenous communities [ 13 ]. PPPS faculty embody this mission in all four areas of an academic health professions program, highlighting the unique health needs of rural residents in their teaching, addressing these needs through community-based participatory research [ 14 ], conducting service activities in rural communities, and providing clinical services. Until 2022, however, no single course in the College of Pharmacy’s curriculum was devoted specifically to rural health.
Rural pharmacy elective-course description and structure
To help address this gap in the College of Pharmacy curriculum, the author – a pharmacist who has practiced hospital, community and long-term care pharmacy in frontier/Indigenous communities in Alaska [ 10 ], Eastern Montana and Minnesota – created a two-credit elective course (two hours per week for 15 weeks) in Rural Pharmacy to introduce students to the benefits and challenges of living and practicing in rural communities. Development of the course was guided by the author’s teaching philosophy; to paraphrase Confucian philosopher Xun Kuang [ 15 ]: “Tell me and I will forget. Show me and I will remember. Involve me and I will understand.”
The Rural Pharmacy course was designed as a HyFlex course [ 16 ] that allows the learner to choose by which content delivery method they would like to learn. Learners in a Hyflex course may elect to attend a live class session in person in a classroom, may attend a live class session remotely via videoconference, or may learn online anytime. Each live class session is recorded to accommodate students who prefer to learn online during a given week, or throughout the entire course.
The Rural Pharmacy elective is a “modified” HyFlex design in that no in-person option is available. University of Minnesota College of Pharmacy faculty and students are accustomed to videoconferencing as a course delivery method, the college having used videoconference technology since 2003 to conduct live, in-person sessions for learners on campuses located 2.5 h apart from one other. Required and elective didactic courses delivered by videoconference are always recorded, enabling learners to view the recording at a more convenient time if they are unable to attend the live class session. Another reason that an in-person option for the Rural Pharmacy elective is not offered is that live course sessions are conducted in the evening to accommodate students from different years in the pharmacy program (P2 and P3) whose other courses are all on different schedules, and Minnesota’s frequent snowy and icy winter conditions are not always conducive to safe travel to and from campus, especially at night.
At the time of this writing, during the first three pre-clinical years University of Minnesota College of Pharmacy students are required to complete 15 credits of elective courses above and beyond their required courses. The Rural Pharmacy elective is open to students in the final two pre-clinical years of the PharmD program (P2 and P3), but enrollment is capped by the instructor at 25 students per offering. Live class sessions are conducted once weekly for two hours in the early evening by videoconference for all students, whether based in Duluth or in the Minneapolis-St. Paul Twin Cities area. The early evening hours avoid conflicts with students’ other courses, which are on different schedules between 8:00 am and 5:30 pm for both of the two years. Students are encouraged to attend as many live videoconference sessions as possible, especially when a guest presenter is scheduled; however, as noted above all class sessions are recorded for viewing or reviewing at a more convenient time. The recordings accommodate students who may be working in a pharmacy as a Pharmacy Intern or Pharmacy Technician at the time class is scheduled, or students who desire to review one or more recorded class sessions prior to the written midterm examination.
A University of Minnesota Post-Graduate Year 1 (PGY1) Rural Pharmacy Resident [ 17 ] serves as the Teaching Assistant for the course each year, participating in the live class sessions via videoconference. The Pharmacy Resident is based out of a rural community in central Minnesota, traveling to two other rural communities and providing comprehensive medication management services [ 18 ] to residents of all three communities. While maintaining patient confidentiality, the Resident shares with students their experiences caring for patients in rural communities, some stories being only a few hours old. In addition to regularly participating in live class sessions, the TA prepares and leads a class session on their own, and conducts the live session interviews with guest rural pharmacists as described below.
About half of the class sessions feature guest pharmacists who currently practice in rural communities, guests joining the live class sessions via videoconference. When a guest pharmacist is invited to participate in the course, the instructor provides the pharmacist with a list of potential interview questions that they would be asked to address during the class session. On rare occasions the visits with pharmacist(s) are pre-recorded either to better accommodate the pharmacist’s work schedule or because of time zone differences between Minnesota and the states where the pharmacists live/work. Pre-recorded interviews are played during the live class session, and students submit questions they would have asked the pharmacist had the pharmacist been able to join the class session in real time. Those questions are then summarized by the instructor and forwarded to the guest pharmacist to respond to as the pharmacist’s time allows. Pharmacists living and practicing in rural and Indigenous communities from throughout Minnesota and from as far away as Alaska have participated in the live sessions, either pre-recorded or in real time. In addition to rural pharmacists, guest presenters have included Advance Practice Nurses [ 19 ] from rural communities, and a Biologist who works with an Indigenous community on the impacts of climate change on the health of the community.
A variety of assessments are utilized in the course including reflection papers, an online multiple-choice/true–false/short answer midterm exam, written participation in online discussions, in-class student presentations and written summaries of interviews with pharmacists practicing in rural communities. The course is graded on a A,B,C,D,F letter grade scale. A total of 300 points are available across nine activities in the course, ranging in value from 5–50 points. The grading scale used in the course is the professional scale used in all of the college’s courses, an A grade being attained by students who earn at least 93% of the available points while students earning fewer than 60% of available points do not receive a passing grade. The possible number of points available on individual assignments are assigned by the instructor based on the amount of time and effort students are expected to expend on the assignment as well as the quality of each assignment’s deliverable.
At the start of the course students complete a brief 7-point Likert-type questionnaire regarding their familiarity with rural communities and interest in possibly practicing in a rural community. The questionnaires are confidential rather than anonymous as students complete the same questionnaire again at the end of the course. The course director uses student names to match start-of-course and end-of-course questionnaires to measure changes in student attitudes. Students also write a brief paper describing their experiences with rural communities and the reason for their interest in learning (or learning more) about living and practicing in rural communities. The instructor uses this information to tailor presentations in the course for the entire class based on the students’ familiarity with rural communities. This information also familiarizes the instructor with students’ backgrounds, enabling the instructor to invite specific students to share their rural experiences as relevant opportunities arise during live class sessions. The initial questionnaire and interest paper collectively constitute 8.37% of the course grade.
The online midterm examination is based on material provided in the textbook [ 20 ] or during instructor or Resident presentations. Students are tested on their knowledge about what constitutes “rural” as defined by several different U.S. government agencies, rural culture, challenges in rural public health, and opportunities and challenges related to practicing pharmacy in rural communities. The midterm exam score constitutes 16.7% of the course grade.
As mentioned previously, the HyFlex nature of the course accommodates students who are unable to attend the live videoconference sessions. All students, however, participate in weekly written online discussions based on the live videoconference session from that week. Live sessions are recorded so that any student may view and listen to the session at their leisure. In the online discussion, students are asked to respond to an instructor-generated question based on that week’s live class session. Students are asked to post their response first, then comment on the response of at least one other classmate. The Canvas learning management system [ 21 ] facilitates this learning approach, providing the instructor the option to require a student to post their response before reading the responses of classmates. Students who post their responses by the weekly deadline receive full participation credit for the week, rather than being graded on the length of their response or on the number of responses they make to classmates’ postings. As a HyFlex course, students are not awarded extra points for attending the live videoconference session, nor are they penalized for not participating in the live videoconference session. Participation constitutes 16.7% of the course grade.
Indigenous people began living in what today is referred to as Minnesota some 13,000 years ago. Among the earliest identifiable tribes in Minnesota were the Dakota (Sioux) circa 1000 CE and the Anishinaabe (Chippewa, Ojibwe) who arrived in the mid-1700s [ 22 ]. Today, Minnesota is home to four Dakota and seven Anishibaabe reservations [ 23 ], most of these communities being located in rural or frontier Minnesota counties. In contrast to these early inhabitants whose ancestors have lived in Minnesota for hundreds of years, today foreign immigrants are arriving in Minnesota in increasing numbers [ 24 ]. Many of these new arrivals settle in communities outside of the Twin Cities Metro Area [ 25 ]. This spectrum of diversity underlies the importance for healthcare providers to learn to provide culturally-responsive care [ 26 ]; therefore, students in the course learn about Indigenous people or foreign-born immigrants they might encounter if practicing in rural Minnesota. Each student is assigned a particular culture (not their own), and through readings about and/or interviews with members from that culture prepares a brief presentation they share with the class during a live videoconference session. Again, because this is a HyFlex course a student who knows in advance that they will be unable to attend class when they are scheduled to present are able to pre-record their presentation. Pre-recorded student presentations are played during the live course session. This exercise constitutes 16.7% of the course grade.
As students in this course are training to become pharmacists, they interview pharmacists who currently practice in rural communities (or who have practiced in a rural community in the recent past). These interviews supplement the rural pharmacy practice stories provided by the instructor, the Resident, and the pharmacists who present during class videoconference sessions. Most, but not all, of the pharmacists who participate in the course are the instructor’s former students from the UMN College of Pharmacy, Duluth. In addition to pharmacists with practice experience in rural Minnesota, pharmacists in the instructor’s circle of contacts from rural Alaska, Wisconsin and Michigan have participated in the course, as have pharmacists from four different rural Indian Health Service [ 27 ] /Tribal Health Clinics. Potential pharmacist participants are contacted by the course instructor before the course begins to gauge their interest and willingness to participate in a live class session or be interviewed by the students, and are provided with the list of interview questions that will be asked. Characteristics and practice settings of the pharmacists who participated during the first two offerings of the course are presented in Table 1 .
The instructor assigns the students to interview teams of two to three students who conduct structured interviews with the rural pharmacists who practice in community, critical access hospital [ 28 ], health system hospital or Indian Health Service/Tribal Health settings. Each student is assigned to one team to interview a community pharmacist, and then to a different team to interview the health system pharmacist. Where possible, teams are structured to reflect gender diversity and include students from different years in the pharmacy program. Each student team contacts their assigned pharmacist and schedules a telephone or videoconference interview. Interviews are intended to last no more than 30 min, but oftentimes go longer as the conversations between the students and the pharmacist range far beyond the structured questions provided by the instructor.
Each student submits written summaries of their two interviews. Each interview team provides informal presentations about their interviews to the class during a live videoconference class session. Each interview assignment constitutes 16.7% of the course grade.
At the end of the course, students once again complete the 7-point Likert-type questionnaire regarding their interest in possibly practicing in a rural community. The numerical results from this questionnaire are compared to the numerical results of the interest questionnaire that the student completed at the start of the course. Each student also writes a brief reflection paper regarding what they learned in the course about practicing pharmacy in a rural community, and what aspect of the course they found most interesting/helpful in their learning. As with the similar assignments at the beginning of the course, the final questionnaire and final reflection paper constitutes 8.37% of the course grade.
Rural pharmacy elective-topics
Topics presented in the course are listed in Table 2 . Topics for didactic sessions early in the course are based on selected chapters from the textbook required for the course, Foundations of Rural Public Health in America (2022), by Joseph N. Inungu and Mark J. Minelli [ 20 ]. The course also features interdisciplinary and interprofessional components. As noted earlier, one guest presenter is a PhD Biologist employed by one of Minnesota’s American Indian tribes. That individual addresses Climate Justice, explaining the impact of climate change on rural Indigenous communities. Also as noted earlier, a group of rural Advanced Practice Nurses in different subspecialties present a panel session addressing the challenges faced by the communities they serve, and describe how they interact with rural pharmacists in their communities.
Assessing course outcomes
The percentages of students enrolled in the course on each campus who reported growing up in a rural community or having spent considerable time visiting relatives who lived in rural communities were compared using Fisher’s exact test [ 29 ]. For students completing rural interest questionnaires both at the beginning and the end of the course, rating scores from both years and both campuses were combined and paired. Given the ordinal nature of the data, beginning/end of course ratings were evaluated using the Wilcoxon signed-rank test [ 30 ]. A two-tailed alpha value of 0.05 was selected as the criterion to indicate significance in all numerical comparisons.
For the first offering of the course in Spring, 2022 a total of 25 students completed the course. Spring 2023 had 17 students in the course. The demographics of the students in these two cohorts are summarized in Table 3 .
Between the first two offerings of this course, 25 students on the Minneapolis campus enrolled in the course. Of these 25, 10 (40%) reported growing up in a rural community or having spent considerable time visiting relatives who lived in rural communities. Among the 17 Duluth students enrolled in the course between the two years, nine (53%) reported having grown up or otherwise spent considerable time in rural areas. This difference was not statistically significant.
At the beginning and end of the course, students rated their interest in living/practicing in rural community using a 7-point Likert-type scale ranging from “1-No interest” to “7-When can I start?!” The results from the 36 students who completed both the pre and post questionnaires are presented in Fig. 1 .
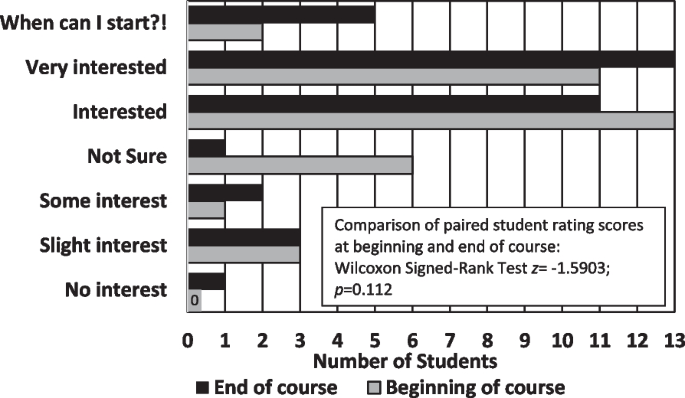
Interest in Practicing Pharmacy in Rural Communities ( n = 36)
The total net change in Rural Interest scores across all students completing both questionnaires was + 5 in 2022 and + 2 in 2023, some student scores increasing, others decreasing, and still others remaining the same. Results of the Wilcoxon Signed-Ranks Test were non-significant ( z = -1.5903; p = 0.112).
The largest change in scores occurred in the “Not sure” category (middle choice), with only one student remaining unsure of their interest in practicing in a rural community at the end of the course compared to six students at the beginning of the course. Four students who selected “Not sure” at the start of the course expressed lower interest in practicing in a rural community at the end of the course, one of these students moving down three levels from “Not sure” to “No interest.” One student who had selected “Interested” at the beginning of the course also dropped three levels at the end of the course to “Slight interest.” In contrast, several students who had selected “Interested” at the start of the course moved up to “Very Interested” or “When can I start?!”.
At the end of the course, students were asked to reflect on the impact of the course on their interest in practicing pharmacy in a rural community. Among the 42 students enrolled in the course during the first two years, 25 students in their reflection papers explicitly expressed appreciation for being able to interview pharmacists currently practicing in rural communities, while 20 explicitly expressed appreciation for having rural pharmacists and other professionals as guest speakers during class sessions. Two word clouds were generated from students’ reflection papers, one based on student perceptions of the benefits of living/practicing in a rural community (Fig. 2 ), and the other based on student perceptions of the challenges of living/practicing in a rural community (Fig. 3 ).
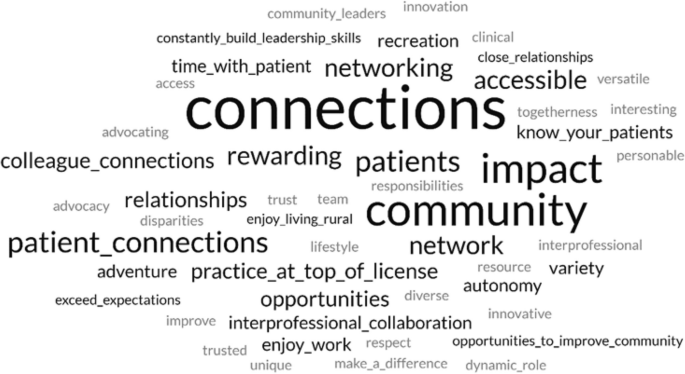
Word cloud featuring perceived benefits of living and practicing pharmacy mentioned in Rural Pharmacy students’ end-of-course reflection papers. “Courtesy of FreeWordCloudGenerator.com”
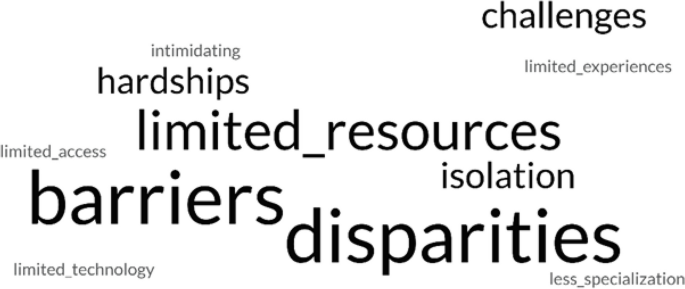
Word cloud featuring perceived challenges of living and practicing pharmacy mentioned in Rural Pharmacy students’ end-of-course reflection papers. “Courtesy of FreeWordCloudGenerator.com”
Representative student comments excerpted from their reflection papers regarding what they had heard from rural pharmacists who participated in the course are provided below. Each student’s comment is followed by that student’s final rating of their interest in practicing pharmacy in a rural community (1 = No interest, 7 = When can I start?!):
Before this course I had no interest in practicing rural before but now I’d at least entertain the idea after speaking and interviewing pharmacists that did or currently practice there. (Student selected ratings of 1 and 2) Hearing so many amazing stories, pharmacists are truly more than just “pill counting” because a single pharmacy can connect them with other rural health professionals, expanding the capabilities of rural pharmacists…. (2) If you can dream it you can do it in rural pharmacy. (5) It was great to have [the pharmacist I interviewed] in my network, as [they] said I can contact [them] anytime with questions outside… [of] my interview. I learned that having many contacts in your network, especially in rural areas, is so important…. (6) This class stimulated a future career interest that I already had, but was not sure exactly how to get started and who to ask if I had any questions. I feel like I now have many resources to reach out to when it comes to my future career, which makes me incredibly happy and comfortable. (7)
Students also expressed appreciation for other aspects of the course, whether the students were interested in practicing in a rural community at the end of the course or not. Again, each student’s comment is followed by that student’s final rating of their interest in practicing pharmacy in a rural community (1 = No interest, 7 = When can I start?!):
Even if I do not practice as a rural pharmacist, I will value the exposure and learning that has come from the topics covered in this course. (3) To be frank, I never even entertained the idea of practicing as a rural pharmacist. I’ve always wanted to work in an urban ambulatory care setting…. I did not expect the class to be as eye opening as it truly was…. I’m much more open to serving in a rural community and may consider it strongly . (3) It would be a huge adjustment to move to a rural area since I have grown up in [an urban community] my whole life. I want to work in a rural community since it is rewarding, but it is difficult to leave family behind and essentially start a new life with new people. (4) This is a rural pharmacy class, but it did not feel biased towards only working rural…. I came into this class knowing that I had an interest in rural pharmacy, but I did not expect to come out of this class even more interested in what rural areas have to offer. (6) Before starting this course, I knew that I wanted to practice pharmacy in a rural community…. Many times during this course we stated, “When you’ve seen one rural community, you’ve seen one rural community.” I did not know how true this statement was before this course…. Despite their vast differences, one common underlying theme is the health disparities seen in rural areas. (7)
It is important that health professions students be introduced to rural culture, even if they are “never” going to live/practice in a rural community themselves. With 5–64% of states’ populations living in rural communities [ 1 ], the odds are good that at some point in their careers, health professionals living in large urban centers are going to care for patients who have come from rural communities to receive more specialized care than is available locally [ 31 ]. Being introduced to rural culture can help students provide more culturally responsive care [ 32 ] to patients from rural communities during their careers.
The purpose of this course was to introduce pharmacy students to the advantages and challenges of practicing and living in rural communities. The course was not intended to “change hearts and minds” of students regarding their possible interest in practicing in a rural setting, and as can be seen from the results, students’ “interest in rural” ratings collectively neither significantly increased nor decreased between the beginning and the end of the course. Regardless, from comments in their reflection papers students generally appreciated the course, finding the interviews with rural pharmacists to be particularly valuable. This finding was heartening to the instructor who was initially concerned about the amount of out-of-class work being asked of the students.
Likewise, guest presenters who participated in the live class sessions and pharmacists interviewed by the students informally expressed their satisfaction with participating in the course, and expressed gratitude that this course was being offered. One pharmacist who previously practiced in a remote Alaska community but had recently moved to a major urban center in the “Lower 48” (Alaskan reference to states in the contiguous United States south of the 49th Parallel) expressed how much they enjoyed sharing their stories with the Rural Pharmacy students. The students with which this pharmacist currently works all desire to practice in large urban centers and are not particularly interested in hearing about the pharmacist’s experiences practicing in small, isolated communities. Another pharmacist noted that they really appreciated joining the students virtually in the live classroom, and was going to recommend this approach to other pharmacy schools with which they work as a way to generate interest in rural pharmacy in general, as well as interest in their particular pharmacy as a clinical rotation site.
A few changes were made in the roster of pharmacists participating in the course from year to year; however, most of the guest speakers and pharmacists who were interviewed by the students participated in the course both years. Another change being considered for the next offering of the course is to add a live videoconference session with a Minnesota Department of Agriculture “Farm Counselor” (a Licensed Professional Counselor) who makes in-person “farm calls” to address farm families’ mental health needs within the unique context of farm culture [ 33 ] (MN Dept of Ag, 2023).
A course specifically addressing the benefits and challenges of practicing pharmacy in rural communities was well-received by pharmacy students enrolled in the course, and by the rural guest presenters and rural pharmacists who were interviewed by the students. Even students who have little interest in living or practicing in a rural community can benefit from being introduced to rural culture, helping all students provide more culturally-responsive care for patients from rural communities.
Availability of data and materials
The data analyzed during the current study are not publicly available due to stipulations in the U.S. Family Educational Rights and Privacy Act (FERPA), but are available in de-identified form from the corresponding author on reasonable request.
Abbreviations
Students enrolled in years 1, 2 or 3 of the Doctor of Pharmacy (PharmD) program
Post-Graduate Year 1
Doctor of Pharmacy
Doctor of Philosophy
Pharmacy Practice and Pharmaceutical Sciences
Teaching Assistant
University of Minnesota
United States of America
United States Census Bureau. Nation’s urban and rural populations shift following 2020 Census. Press Release Number CB22-CN.25. Suitland (MD): U.S. Census Bureau; 2022. Available from: https://www.census.gov/newsroom/press-releases/2022/urban-rural-populations.html . Cited 2023 Aug 29.
United States National Center for Health Statistics. Health, United States, 2020-2021. Hyattsville (MD): U.S. Centers for Disease Control and Prevention; 2023. Available from: https://www.cdc.gov/nchs/hus/sources-definitions/geographic-region.htm . Cited 2024 Jan 22.
RHIhub. Rural Pharmacy and Prescription Drugs. [Internet]. Rural Health Information Hub. Available from: https://www.ruralhealthinfo.org/topics/pharmacy-and-prescription-drugs . Updated 2023 Jan 26; cited 2023 Aug 29.
Davis JC, Rupasingha A, Cromartie J, Sanders A. Rural America at a glance. Washington, DC: U.S: Department of Agriculture, Economic Research Service; 2022. Available from: Rural America at a Glance: 2022 Edition (usda.gov) . Cited 2023 Aug 29.
Google Scholar
United States Department of Agriculture Economic Research Service. Rural poverty & well-being. Washington, DC: U.S. Department of Agriculture; [updated 2022 Nov 29. Available from: USDA ERS - Rural Poverty & Well-Being . Cited 2023 Aug 29.
United States Centers for Disease Control and Prevention. About rural health. [Internet]. Atlanta (GA): Centers for Disease Control and Prevention. Available from: About Rural Health | CSELS | Rural Health | CDC . Updated 2023 May 09; cited 2023 Aug 29.
Turrini G, Branham DK, Chen L, Conmy AB, Chappel AR, De Lew N, Sommers BD. Access to Affordable Care in Rural America: Current Trends and Key Challenges. Washington, DC: United State Department of Health & Human Services, Assistant Secretary for Planning and Evaluation. Available from: https://aspe.hhs.gov/sites/default/files/2021-07/rural-health-rr.pdf . 2021 July 09; Cited 23 Aug 29.
United States. Department of Health & Human Services, Health Resources and Services Administration, Bureau of Health Workforce. Designated health professional shortage areas statistics. Washington, DC: U.S. Department of Health & Human Services. Available from: BCD_HPSA_SCR50_Qtr_Smry.pdf . Updated, 2023 Mar 31; cited 2023 Aug 29. https://data.hrsa.gov/Default/GenerateHPSAQuarterlyReport .
Council on Graduate Medical Education. Rural health policy brief 1. Special needs in rural America: Implications for healthcare workforce education, training and practice. Washington, DC: Health Resources & Services Administration. Available from: COGME Rural Health Policy Brief 1 (hrsa.gov) . Updated 2020 July 17; cited 2023 Aug 29.
Stratton TP. The economic realities of rural pharmacy practice. J Rural Health. 2001;17(2):77–81. https://doi.org/10.1111/j.1748-0361.2001.tb00261.x .
Article Google Scholar
Speedie MK, Ruhrold LN. A history of the University of Minnesota College of Pharmacy, 1892–2017. Research Triangle (NC): Lulu Press, Inc.; 2021. p. 285.
Nagel P, Yuan F. High-resolution land cover and impervious surface classifications in the twin cities metropolitan area with NAIP imagery. Photogrammet Eng Remote Sensing. 2016;82(1):63–71. Available from: https://www.researchgate.net/publication/288684001_High-resolution_Land_Cover_and_Impervious_Surface_Classifications_in_the_Twin_Cities_Metropolitan_Area_with_NAIP_Imagery .
University of Minnesota, College of Pharmacy, Department of Pharmacy Practice and Pharmaceutical Sciences. Minneapolis (MN): University of Minnesota College of Pharmacy; c2023. Available from: https://www.pharmacy.umn.edu/pharmacy-practice-pharmaceutical-sciences . Cited 2023 Aug 29.
United States Department of Health & Human Services, National Institute on Minority Health and Health Disparities. Community-Based Participatory Research Program (CBPR). NIH Guide No. RFA-MD-15-010. [Internet]. Bethesda (MD): National Institutes of Health. Available from: https://www.nimhd.nih.gov/programs/extramural/community-based-participatory.html . Updated 2018 Oct 02; cited 2023 Aug 29.
O’Toole, G. Quote Investigator. Xun Kuang. 2023. Available from: https://www.goodreads.com/quotes/7565817-tell-me-and-i-forget-teach-me-and-i-may . Cited 2023 Aug 29.
Beatty BJ. Hybrid-flexible course design: Implementing student-directed hybrid classes. 2019. Available from: https://edtechbooks.org/hyflex . Cited 2023 Aug 29.
University of Minnesota College of Pharmacy. Residency Sites & Emphasis Areas. Minneapolis (MN): University of Minnesota College of Pharmacy; c2023. Available from: https://www.pharmacy.umn.edu/degrees-programs/postgraduate-pharmacy-residency-program/residency-sites-emphasis-areas-2 . Cited 2023 Aug 29.
GTMRx Institute. c2019. Available from: https://gtmr.org/what-is-the-comprehensive-medication-management-process/ . Cited 2023 Aug 29.
American Nurses Association. Advanced practice registered nurse (APRN). [Internet]. Silver Spring (MD): American Nurses Association. Available from: https://www.nursingworld.org/practice-policy/workforce/what-is-nursing/aprn/ .
Ingunu JN, Minelli MJ. Foundations of rural public health in America. Burlington: Jones & Bartlett Learning; 2022. p. 491.
Canvas LMS. Salt Lake City (UT): Instructure. c2008-2023. Available from: https://www.instructure.com/canvas . Cited 2023 Aug 29.
Furst R. Which Indigenous tribes first called Minnesota home? Star Tribune [Internet] (Minneapolis, Minnesota). 2021. Available from: https://www.startribune.com/native-american-dakota-ojibwe-history/600097050/#:~:text=The%20earliest%20identifiable%20tribe%20in,Ojibwe%20in%20the%20mid%2D1700s . Cited 2023 Aug 29.
State of Minnesota. Minnesota Indian Tribes. St. Paul (MN): State of Minnesota. Available from: https://mn.gov/portal/government/tribal/mn-indian-tribes/#:~:text=In%20Minnesota%2C%20there%20are%20seven,links%20to%20other%20valuable%20resources.&text=What%20does%20the%20term%20Federally%20Recognized%20mean%3F . Cited 2023 Aug 29.
American Immigration Council. Immigrants in Minnesota. Washington, DC: American Immigration Council. c2023. Available from: https://map.americanimmigrationcouncil.org/locations/minnesota/?_gl=1*5ervbb*_ga*MTYyMDYyNjcyNy4xNjkyMjExNzI4*_ga_W0MSMD2GPV*MTY5MjIxMTcyOC4xLjEuMTY5MjIxMTk3Mi4wLjAuMA . Cited 2023 Aug 29.
Minnesota Chamber of Commerce. Economic contributions by region. St. Paul (MN): Minnesota Chamber of Commerce. 2021 Mar 23. Available from: https://www.mnchamber.com/blog/economic-contributions-region . Cited 2023 Aug 29.
Prasad SJ, Nari P, Gadhvi, K, Barai I, Danish H, Philip AB. Cultural humility: treating the patient, not the illness. Med Educ Online. 2016 Feb 3;216;21: 10.3402/meo.v21.30908. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4742464/ . Cited 2023 Aug 29.
U.S. Department of Health and Human Services, Indian Health Service. Rockville (MD): U.S. Department of Health & Human Services. Available from: https://www.ihs.gov/ .
Centers for Medicare and Medicaid Services. Critical Access Hospitals. Woodlawn (MD): Centers for Medicare and Medicaid Services; [updated 2021 Dec 12. Available from: https://www.cms.gov/medicare/provider-enrollment-and-certification/certificationandcomplianc/cahs . Cited 2023 Aug 29.
Siegel S. Fisher’s exact test. Nonparametric statistics for the behavioral sciences. New York: McGraw-Hill. 1956. pp 96–104.
Siegel S. Wilcoxon signed-rank test. Nonparametric statistics for the behavioral sciences. New York: McGraw-Hill; 1956. pp. 75–83.
Casey M, McCullough J, Kreiger R. Which Medicare patients are transferred from rural emergency departments? [Internet]. Minneapolis (MN): University of Minnesota Rural Health Research Center. 2014. p. 19. Available from: https://rhrc.umn.edu/wp-content/uploads/2017/11/whichmedicarepatientsaretransferred.pdf . Cited 2023 Aug 29.
Minnesota Department of Health. Culturally responsive care. St. Paul (MN): Minnesota Department of Health. 2019 May 01. Available from: https://www.health.state.mn.us/docs/communities/titlev/cultresponsive.pdf . Cited 2023 Aug 29.
Minnesota Department of Agriculture. Stress&Crisis: Get Help Now. St. Paul (MN): Minnesota Department of Agriculture. c2023. Available from: https://www.mda.state.mn.us/about/mnfarmerstress/copingstress . Cited 2023 Aug 29.
Download references
Acknowledgements
Not applicable.
No funding was received for this project.
Author information
Authors and affiliations.
University of Minnesota College of Pharmacy, Duluth, MN, USA
Timothy P. Stratton
You can also search for this author in PubMed Google Scholar
Contributions
T.P.S. solely conceived and undertook all aspects of this project and preparation of this manuscript.
Author’s information
TPS is Professor of Pharmacy Practice in the University of Minnesota College of Pharmacy, Duluth. He has practiced community, hospital and long-term care pharmacy in frontier communities in Southeast Alaska, and at Indian Health Service/Tribal Health clinics in frontier Alaska and eastern Montana, and in rural Minnesota. He is a member of the Rural Pharmacy Consortium , a Past Chair of the Small and Rural Hospital Section Advisory Group for the American Society of Health-System Pharmacists, and a Past President of the Minnesota Rural Health Association.
Corresponding author
Correspondence to Timothy P. Stratton .
Ethics declarations
Ethics approval and consent to participate.
Approval - The Institutional Review Board (IRB) of the University of Minnesota determined that this project constituted Exempt Research.
Informed consent - The Institutional Review Board (IRB) of the University of Minnesota waived the need for informed consent in this project.
Consent for publication
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Stratton, T.P. For the rural curious: mixed methods evaluation of a rural pharmacy practice elective. BMC Med Educ 24 , 573 (2024). https://doi.org/10.1186/s12909-024-05539-3
Download citation
Received : 18 September 2023
Accepted : 08 May 2024
Published : 24 May 2024
DOI : https://doi.org/10.1186/s12909-024-05539-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Rural pharmacy
- Pharmacists
- Rural health
- Pharmacy education
BMC Medical Education
ISSN: 1472-6920
- Submission enquiries: [email protected]
- General enquiries: [email protected]
It’s Time to Put Americans’ Health Care Decisions Back in Our Own Hands
Photograph by Nathaniel St. Clair
We all deserve the right to make informed decisions about our own health. That right has been in danger for years — and since the Supreme Court overturned Roe v. Wade , it’s under siege.
I grew up in the South with an abstinence-only education — if you can call that an “education.”
This approach, which teaches nothing about sex except not to have it, is an utter failure . It’s been proven to have no effect on reducing adolescent pregnancies. And couples who’ve received abstinence-only messaging use less birth control and STD protection than couples who’ve been taught about them.
When I went to college and became aware of the harmful effects of abstinence-only “education,” I joined a peer-based sex ed group on campus. We were health- and sex-positive. But abortion was still only discussed in the shadows, in hushed tones, if at all.
But now, like sex ed, these discussions need to be out in the open.
When my birth control failed, I became pregnant. My now-husband and I were in a long-distance relationship while he finished a paramedic program. We were considering marriage, but we weren’t there yet and didn’t have enough money to raise a child. We made what was, for us, the responsible decision.
The truth is, all kinds of people get abortions. More than half are already parents . People who identify as “pro-life” get abortions, and people who are married get abortions. And the vast majority of Americans support the right to choose an abortion.
After my legal abortion, I began volunteering at an abortion clinic in Florida. Years later, I was offered a job at the Yellowhammer Fund , which provides support to pregnant people seeking reproductive care and family planning in Alabama and across the South.
Reproductive health care wasn’t easy even before the Supreme Court reversed Roe, especially in the South.
For instance, in Alabama, we had only three health care providers willing to provide abortion care. The state imposed stricter than national average gestational limits, a two-visit prerequisite, and a 48-hour waiting period. If the situation was an emergency, the documentation for a medical exception was extremely difficult to obtain.
Now it’s even worse. Not only can we not provide care, we can’t help patients cross state lines to get it elsewhere. We can’t even help patients understand where and how they can receive the abortion care they need. Our speech has been criminalized.
In states like mine where care has now been prohibited, it’s not the pregnant person, their family, and doctors who determine their care. It’s ideologically extreme lawmakers with no medical background or knowledge of individual circumstances who dictate those deeply personal decisions.
We’re doing what we can. For now, we can direct people seeking abortion care to published articles where they can find information. We can still help families with legal challenges and provide safe sex kits.
Importantly, we’re also training community members across the rural South to be advocates and provide supportive resources for those seeking reproductive justice. And the Yellowhammer Fund has launched a lawsuit to restore our right to help clients find abortion care, and there is some hopeful movement.
But we also need lawmakers to know that every decision they make restricting reproductive care is life-ruining. They aren’t “pro-life.” They aren’t saving lives. All too often, when women can’t get miscarriage treatments or other emergency care, they’re ending lives.
Midwives and birthing centers need to be free to care for their patients in ways that maximize that patient’s health and family, free of state control and threats of prison. This is a message that the majority of Americans support. We need to make sure lawmakers listen.
Kelsea McLain was born and raised in the South. She’s the Deputy Director of the Yellowhammer Fund in Alabama and a member of the Southern Reproductive and Sexual Health Advocates table convened by the National Health Law Program .
CounterPunch+
- Capitalism Attacks Argentine Workers and You May be Next
- Blaming Soros for Campus Protests is Anti-Semitic — Just Ask Israel
- Three Strikes
- Fallen Angel
- The Great Resignation
Australian Government Department of Health and Aged Care
Budget 2024–25
Fact sheets and other health, aged care and sport information from the 2024–25 Budget.

Scroll down to access downloads and media.
Ministers' media releases
Budget 2024–25: Cheaper medicines, new Medicare Urgent Care Clinics and more free mental health services in a stronger Medicare
Budget 2024–25: Investing in quality aged care
Portfolio Budget Statements
Budget 2024–25: Health and Aged Care Portfolio Budget Statements
Stakeholder pack
Budget 2024–25: Stakeholder pack
Budget 2024–25: Budget overview
Budget 2024–25: Ensuring all Australians get the health care they need
Fact sheets
Budget 2024–25: Strengthening Medicare
Budget 2024–25: Cheaper medicines
Budget 2024–25: Quality aged care
Budget 2024–25: A fit and healthy Australia
We aim to provide documents in an accessible format. If you're having problems using a document with your accessibility tools, please contact us for help .
- About the department
Is there anything wrong with this page?
Help us improve health.gov.au
If you would like a response please use the enquiries form instead.
- Share full article

When Prison and Mental Illness Amount to a Death Sentence
The downward spiral of one inmate, Markus Johnson, shows the larger failures of the nation’s prisons to care for the mentally ill.
Supported by
By Glenn Thrush
Photographs by Carlos Javier Ortiz
Glenn Thrush spent more than a year reporting this article, interviewing close to 50 people and reviewing court-obtained body-camera footage and more than 1,500 pages of documents.
- Published May 5, 2024 Updated May 7, 2024
Markus Johnson slumped naked against the wall of his cell, skin flecked with pepper spray, his face a mask of puzzlement, exhaustion and resignation. Four men in black tactical gear pinned him, his face to the concrete, to cuff his hands behind his back.
He did not resist. He couldn’t. He was so gravely dehydrated he would be dead by their next shift change.
Listen to this article with reporter commentary
“I didn’t do anything,” Mr. Johnson moaned as they pressed a shield between his shoulders.
It was 1:19 p.m. on Sept. 6, 2019, in the Danville Correctional Center, a medium-security prison a few hours south of Chicago. Mr. Johnson, 21 and serving a short sentence for gun possession, was in the throes of a mental collapse that had gone largely untreated, but hardly unwatched.
He had entered in good health, with hopes of using the time to gain work skills. But for the previous three weeks, Mr. Johnson, who suffered from bipolar disorder and schizophrenia, had refused to eat or take his medication. Most dangerous of all, he had stealthily stopped drinking water, hastening the physical collapse that often accompanies full-scale mental crises.
Mr. Johnson’s horrific downward spiral, which has not been previously reported, represents the larger failures of the nation’s prisons to care for the mentally ill. Many seriously ill people receive no treatment . For those who do, the outcome is often determined by the vigilance and commitment of individual supervisors and frontline staff, which vary greatly from system to system, prison to prison, and even shift to shift.
The country’s jails and prisons have become its largest provider of inpatient mental health treatment, with 10 times as many seriously mentally ill people now held behind bars as in hospitals. Estimating the population of incarcerated people with major psychological problems is difficult, but the number is likely 200,000 to 300,000, experts say.
Many of these institutions remain ill-equipped to handle such a task, and the burden often falls on prison staff and health care personnel who struggle with the dual roles of jailer and caregiver in a high-stress, dangerous, often dehumanizing environment.
In 2021, Joshua McLemore , a 29-year-old with schizophrenia held for weeks in an isolation cell in Jackson County, Ind., died of organ failure resulting from a “refusal to eat or drink,” according to an autopsy. In April, New York City agreed to pay $28 million to settle a lawsuit filed by the family of Nicholas Feliciano, a young man with a history of mental illness who suffered severe brain damage after attempting to hang himself on Rikers Island — as correctional officers stood by.
Mr. Johnson’s mother has filed a wrongful-death suit against the state and Wexford Health Sources, a for-profit health care contractor in Illinois prisons. The New York Times reviewed more than 1,500 pages of reports, along with depositions taken from those involved. Together, they reveal a cascade of missteps, missed opportunities, potential breaches of protocol and, at times, lapses in common sense.

Prison officials and Wexford staff took few steps to intervene even after it became clear that Mr. Johnson, who had been hospitalized repeatedly for similar episodes and recovered, had refused to take medication. Most notably, they did not transfer him to a state prison facility that provides more intensive mental health treatment than is available at regular prisons, records show.
The quality of medical care was also questionable, said Mr. Johnson’s lawyers, Sarah Grady and Howard Kaplan, a married legal team in Chicago. Mr. Johnson lost 50 to 60 pounds during three weeks in solitary confinement, but officials did not initiate interventions like intravenous feedings or transfer him to a non-prison hospital.
And they did not take the most basic step — dialing 911 — until it was too late.
There have been many attempts to improve the quality of mental health treatment in jails and prisons by putting care on par with punishment — including a major effort in Chicago . But improvements have proved difficult to enact and harder to sustain, hampered by funding and staffing shortages.
Lawyers representing the state corrections department, Wexford and staff members who worked at Danville declined to comment on Mr. Johnson’s death, citing the unresolved litigation. In their interviews with state police investigators, and in depositions, employees defended their professionalism and adherence to procedure, while citing problems with high staff turnover, difficult work conditions, limited resources and shortcomings of co-workers.
But some expressed a sense of resignation about the fate of Mr. Johnson and others like him.
Prisoners have “much better chances in a hospital, but that’s not their situation,” said a senior member of Wexford’s health care team in a deposition.
“I didn’t put them in prison,” he added. “They are in there for a reason.”
Markus Mison Johnson was born on March 1, 1998, to a mother who believed she was not capable of caring for him.
Days after his birth, he was taken in by Lisa Barker Johnson, a foster mother in her 30s who lived in Zion, Ill., a working-class city halfway between Chicago and Milwaukee. Markus eventually became one of four children she adopted from different families.
The Johnson house is a lively split level, with nieces, nephews, grandchildren and neighbors’ children, family keepsakes, video screens and juice boxes. Ms. Johnson sits at its center on a kitchen chair, chin resting on her hand as children wander over to share their thoughts, or to tug on her T-shirt to ask her to be their bathroom buddy.
From the start, her bond with Markus was particularly powerful, in part because the two looked so much alike, with distinctive dimpled smiles. Many neighbors assumed he was her biological son. The middle name she chose for him was intended to convey that message.
“Mison is short for ‘my son,’” she said standing over his modest footstone grave last summer.
He was happy at home. School was different. His grades were good, but he was intensely shy and was diagnosed with attention deficit hyperactivity disorder in elementary school.
That was around the time the bullying began. His sisters were fierce defenders, but they could only do so much. He did the best he could, developing a quick, taunting tongue.
These experiences filled him with a powerful yearning to fit in.
It was not to be.
When he was around 15, he called 911 in a panic, telling the dispatcher he saw two men standing near the small park next to his house threatening to abduct children playing there. The officers who responded found nothing out of the ordinary, and rang the Johnsons’ doorbell.
He later told his mother he had heard a voice telling him to “protect the kids.”
He was hospitalized for the first time at 16, and given medications that stabilized him for stretches of time. But the crises would strike every six months or so, often triggered by his decision to stop taking his medication.
His family became adept at reading signs he was “getting sick.” He would put on his tan Timberlands and a heavy winter coat, no matter the season, and perch on the edge of his bed as if bracing for battle. Sometimes, he would cook his own food, paranoid that someone might poison him.
He graduated six months early, on the dean’s list, but was rudderless, and hanging out with younger boys, often paying their way.
His mother pointed out the perils of buying friendship.
“I don’t care,” he said. “At least I’ll be popular for a minute.”
Zion’s inviting green grid of Bible-named streets belies the reality that it is a rough, unforgiving place to grow up. Family members say Markus wanted desperately to prove he was tough, and emulated his younger, reckless group of friends.
Like many of them, he obtained a pistol. He used it to hold up a convenience store clerk for $425 in January 2017, according to police records. He cut a plea deal for two years of probation, and never explained to his family what had made him do it.
But he kept getting into violent confrontations. In late July 2018, he was arrested in a neighbor’s garage with a handgun he later admitted was his. He was still on probation for the robbery, and his public defender negotiated a plea deal that would send him to state prison until January 2020.
An inpatient mental health system
Around 40 percent of the about 1.8 million people in local, state and federal jails and prison suffer from at least one mental illness, and many of these people have concurrent issues with substance abuse, according to recent Justice Department estimates.
Psychological problems, often exacerbated by drug use, often lead to significant medical problems resulting from a lack of hygiene or access to good health care.
“When you suffer depression in the outside world, it’s hard to concentrate, you have reduced energy, your sleep is disrupted, you have a very gloomy outlook, so you stop taking care of yourself,” said Robert L. Trestman , a Virginia Tech medical school professor who has worked on state prison mental health reforms.
The paradox is that prison is often the only place where sick people have access to even minimal care.
But the harsh work environment, remote location of many prisons, and low pay have led to severe shortages of corrections staff and the unwillingness of doctors, nurses and counselors to work with the incarcerated mentally ill.
In the early 2000s, prisoners’ rights lawyers filed a class-action lawsuit against Illinois claiming “deliberate indifference” to the plight of about 5,000 mentally ill prisoners locked in segregated units and denied treatment and medication.
In 2014, the parties reached a settlement that included minimum staffing mandates, revamped screening protocols, restrictions on the use of solitary confinement and the allocation of about $100 million to double capacity in the system’s specialized mental health units.
Yet within six months of the deal, Pablo Stewart, an independent monitor chosen to oversee its enforcement, declared the system to be in a state of emergency.
Over the years, some significant improvements have been made. But Dr. Stewart’s final report , drafted in 2022, gave the system failing marks for its medication and staffing policies and reliance on solitary confinement “crisis watch” cells.
Ms. Grady, one of Mr. Johnson’s lawyers, cited an additional problem: a lack of coordination between corrections staff and Wexford’s professionals, beyond dutifully filling out dozens of mandated status reports.
“Markus Johnson was basically documented to death,” she said.
‘I’m just trying to keep my head up’
Mr. Johnson was not exactly looking forward to prison. But he saw it as an opportunity to learn a trade so he could start a family when he got out.
On Dec. 18, 2018, he arrived at a processing center in Joliet, where he sat for an intake interview. He was coherent and cooperative, well-groomed and maintained eye contact. He was taking his medication, not suicidal and had a hearty appetite. He was listed as 5 feet 6 inches tall and 256 pounds.
Mr. Johnson described his mood as “go with the flow.”
A few days later, after arriving in Danville, he offered a less settled assessment during a telehealth visit with a Wexford psychiatrist, Dr. Nitin Thapar. Mr. Johnson admitted to being plagued by feelings of worthlessness, hopelessness and “constant uncontrollable worrying” that affected his sleep.
He told Dr. Thapar he had heard voices in the past — but not now — telling him he was a failure, and warning that people were out to get him.
At the time he was incarcerated, the basic options for mentally ill people in Illinois prisons included placement in the general population or transfer to a special residential treatment program at the Dixon Correctional Center, west of Chicago. Mr. Johnson seemed out of immediate danger, so he was assigned to a standard two-man cell in the prison’s general population, with regular mental health counseling and medication.
Things started off well enough. “I’m just trying to keep my head up,” he wrote to his mother. “Every day I learn to be stronger & stronger.”
But his daily phone calls back home hinted at friction with other inmates. And there was not much for him to do after being turned down for a janitorial training program.
Then, in the spring of 2019, his grandmother died, sending him into a deep hole.
Dr. Thapar prescribed a new drug used to treat major depressive disorders. Its most common side effect is weight gain. Mr. Johnson stopped taking it.
On July 4, he told Dr. Thapar matter-of-factly during a telehealth check-in that he was no longer taking any of his medications. “I’ve been feeling normal, I guess,” he said. “I feel like I don’t need the medication anymore.”
Dr. Thapar said he thought that was a mistake, but accepted the decision and removed Mr. Johnson from his regular mental health caseload — instructing him to “reach out” if he needed help, records show.
The pace of calls back home slackened. Mr. Johnson spent more time in bed, and became more surly. At a group-therapy session, he sat stone silent, after showing up late.
By early August, he was telling guards he had stopped eating.
At some point, no one knows when, he had intermittently stopped drinking fluids.
‘I’m having a breakdown’
Then came the crash.
On Aug. 12, Mr. Johnson got into a fight with his older cellmate.
He was taken to a one-man disciplinary cell. A few hours later, Wexford’s on-site mental health counselor, Melanie Easton, was shocked by his disoriented condition. Mr. Johnson stared blankly, then burst into tears when asked if he had “suffered a loss in the previous six months.”
He was so unresponsive to her questions she could not finish the evaluation.
Ms. Easton ordered that he be moved to a 9-foot by 8-foot crisis cell — solitary confinement with enhanced monitoring. At this moment, a supervisor could have ticked the box for “residential treatment” on a form to transfer him to Dixon. That did not happen, according to records and depositions.
Around this time, he asked to be placed back on his medication but nothing seems to have come of it, records show.
By mid-August, he said he was visualizing “people that were not there,” according to case notes. At first, he was acting more aggressively, once flicking water at a guard through a hole in his cell door. But his energy ebbed, and he gradually migrated downward — from standing to bunk to floor.
“I’m having a breakdown,” he confided to a Wexford employee.
At the time, inmates in Illinois were required to declare an official hunger strike before prison officials would initiate protocols, including blood testing or forced feedings. But when a guard asked Mr. Johnson why he would not eat, he said he was “fasting,” as opposed to starving himself, and no action seems to have been taken.
‘Tell me this is OK!’
Lt. Matthew Morrison, one of the few people at Danville to take a personal interest in Mr. Johnson, reported seeing a white rind around his mouth in early September. He told other staff members the cell gave off “a death smell,” according to a deposition.
On Sept. 5, they moved Mr. Johnson to one of six cells adjacent to the prison’s small, bare-bones infirmary. Prison officials finally placed him on the official hunger strike protocol without his consent.
Mr. Morrison, in his deposition, said he was troubled by the inaction of the Wexford staff, and the lack of urgency exhibited by the medical director, Dr. Justin Young.
On Sept. 5, Mr. Morrison approached Dr. Young to express his concerns, and the doctor agreed to order blood and urine tests. But Dr. Young lived in Chicago, and was on site at the prison about four times a week, according to Mr. Kaplan. Friday, Sept. 6, 2019, was not one of those days.
Mr. Morrison arrived at work that morning, expecting to find Mr. Johnson’s testing underway. A Wexford nurse told him Dr. Young believed the tests could wait.
Mr. Morrison, stunned, asked her to call Dr. Young.
“He’s good till Monday,” Dr. Young responded, according to Mr. Morrison.
“Come on, come on, look at this guy! You tell me this is OK!” the officer responded.
Eventually, Justin Duprey, a licensed nurse practitioner and the most senior Wexford employee on duty that day, authorized the test himself.
Mr. Morrison, thinking he had averted a disaster, entered the cell and implored Mr. Johnson into taking the tests. He refused.
So prison officials obtained approval to remove him forcibly from his cell.
‘Oh, my God’
What happened next is documented in video taken from cameras held by officers on the extraction team and obtained by The Times through a court order.
Mr. Johnson is scarcely recognizable as the neatly groomed 21-year-old captured in a cellphone picture a few months earlier. His skin is ashen, eyes fixed on the middle distance. He might be 40. Or 60.
At first, he places his hands forward through the hole in his cell door to be cuffed. This is against procedure, the officers shout. His hands must be in back.
He will not, or cannot, comply. He wanders to the rear of his cell and falls hard. Two blasts of pepper spray barely elicit a reaction. The leader of the tactical team later said he found it unusual and unnerving.
The next video is in the medical unit. A shield is pressed to his chest. He is in agony, begging for them to stop, as two nurses attempt to insert a catheter.
Then they move him, half-conscious and limp, onto a wheelchair for the blood draw.
For the next 20 minutes, the Wexford nurse performing the procedure, Angelica Wachtor, jabs hands and arms to find a vessel that will hold shape. She winces with each puncture, tries to comfort him, and grows increasingly rattled.
“Oh, my God,” she mutters, and asks why help is not on the way.
She did not request assistance or discuss calling 911, records indicate.
“Can you please stop — it’s burning real bad,” Mr. Johnson said.
Soon after, a member of the tactical team reminds Ms. Wachtor to take Mr. Johnson’s vitals before taking him back to his cell. She would later tell Dr. Young she had been unable to able to obtain his blood pressure.
“You good?” one of the team members asks as they are preparing to leave.
“Yeah, I’ll have to be,” she replies in the recording.
Officers lifted him back onto his bunk, leaving him unconscious and naked except for a covering draped over his groin. His expressionless face is visible through the window on the cell door as it closes.
‘Cardiac arrest.’
Mr. Duprey, the nurse practitioner, had been sitting inside his office after corrections staff ordered him to shelter for his own protection, he said. When he emerged, he found Ms. Wachtor sobbing, and after a delay, he was let into the cell. Finding no pulse, Mr. Duprey asked a prison employee to call 911 so Mr. Johnson could be taken to a local emergency room.
The Wexford staff initiated CPR. It did not work.
At 3:38 p.m., the paramedics declared Markus Mison Johnson dead.
Afterward, a senior official at Danville called the Johnson family to say he had died of “cardiac arrest.”
Lisa Johnson pressed for more information, but none was initially forthcoming. She would soon receive a box hastily crammed with his possessions: uneaten snacks, notebooks, an inspirational memoir by a man who had served 20 years at Leavenworth.
Later, Shiping Bao, the coroner who examined his body, determined Mr. Johnson had died of severe dehydration. He told the state police it “was one of the driest bodies he had ever seen.”
For a long time, Ms. Johnson blamed herself. She says that her biggest mistake was assuming that the state, with all its resources, would provide a level of care comparable to what she had been able to provide her son.
She had stopped accepting foster care children while she was raising Markus and his siblings. But as the months dragged on, she decided her once-boisterous house had become oppressively still, and let local agencies know she was available again.
“It is good to have children around,” she said. “It was too quiet around here.”
Read by Glenn Thrush
Audio produced by Jack D’Isidoro .
Glenn Thrush covers the Department of Justice. He joined The Times in 2017 after working for Politico, Newsday, Bloomberg News, The New York Daily News, The Birmingham Post-Herald and City Limits. More about Glenn Thrush
Advertisement

COMMENTS
The delivery of healthcare services is considered to be a system; according to the Free Diction- ary (Farlex, 2010), a system is defined as "a group of interacting, interrelated, or interdependent elements forming a complex whole.". This is an apt description of our healthcare structure, as it is compiled of patients, medical and mental ...
An expensive health care system translates to an increasing proportion of the population being unable to access the much needed medical care. The New York Times reports that according to census survey carried out in the year 2007, an estimated 45.6 million people in the USA were uninsured and hence unlikely to receive comprehensive medical care from hospitals (1).
2. Argument against Universal Healthcare. Though the majority of post-industrial Westernized nations employ a universal healthcare model, few—if any—of these nations are as geographically large, populous, or ethnically/racially diverse as the U.S. Different regions in the U.S. are defined by distinct cultural identities, citizens have unique religious and political values, and the populace ...
The US Healthcare System Essay Essay. The delivery system of medical care in America today is an extensive institution, with numerous types of institutions such as clinics, hospitals and boarding houses. The US health care system does not provide uniform coverage for citizens at the federal level. In this regard, there are several basic types ...
Germany, which has all along had a robust public health care system, was accepting sick patients from Italy, Spain, and France. Meanwhile, U.S. hospitals were in financial shock and fee-for-service-based physician practices were devastated. We need to move toward a genuine health care system that can withstand shocks like the Covid-19 pandemic.
They include: focus on prevention, not just treating sickness; tackle racial disparities; expand telehealth and in-home services; build integrated systems; and adopt value-based care. Since early ...
Universal health care is the provision of healthcare services by a government to all its citizens (insurancespecialists.com). This means each citizen can access medical services of standard quality. In the United States, about 25% of its citizens are provided with healthcare funded by the government. These citizens mainly comprise the elderly ...
The high cost of medical care in the U.S. is one of the greatest challenges the country faces and it affects everything from the economy to individual behavior, according to an essay in the May-June 2020 issue of Harvard Magazine written by David Cutler, professor in the Department of Global Health and Population at Harvard T.H. Chan School of Public Health.
A Crisis in Public Health. The United States has 4% of the world's population but, as of July 16, approximately 26% of its Covid-19 cases and 24% of its Covid-19 deaths. 17 These startling ...
Introduction. In the previous edition of U.S. Health Care from a Global Perspective, we reported that people in the United States experience the worst health outcomes overall of any high-income nation. 1 Americans are more likely to die younger, and from avoidable causes, than residents of peer countries.. Between January 2020 and December 2021, life expectancy dropped in the U.S. and other ...
The National Academy of Medicine defines healthcare quality as "the degree to which health care services for individuals and populations increase the likelihood of desired health outcomes and are consistent with current professional knowledge." Many factors contribute to the quality of care in the United States, including access to timely care, affordability of care, and use of evidence ...
Health benefits aside, increasing investment in primary prevention presents a strong economic imperative. For example, obesity contributes to the treatment costs of many other diseases: 70% of diabetes costs, 23% for CVD and 9% for cancers. Economic losses further extend to absenteeism and decreased productivity.
The high cost of the US health care system is its biggest weakness. In the US, national expenditures on health care goods and services were approximately $4 trillion in 2020, accounting for an estimated 18% of gross domestic product. 2 High prices for care explain a large part of the difference in spending between the US and other developed ...
Health Care Professionals Healthcare Professionals the Paper. The paper is based on the healthcare professionals. It starts by analyzing the reasons why there may be physician shortage rather than a surplus in the United States. The paper as well analyses the factors that contribute to the nursing shortage in the U.S.
Health reform: How to improve U.S. health care in 2020 and beyond. Health care remains a major theme in our national conversation. And as we approach the November 2020 election, we will hear a lot of debate about the right path forward to fix what ails our current system. It is encouraging to hear so many people—candidates, policymakers ...
In the United States, health care devices, technologies, and practices are rapidly moving into the home. The factors driving this migration include the costs of health care, the growing numbers of older adults, the increasing prevalence of chronic conditions and diseases and improved survival rates for people with those conditions and diseases ...
The public spending on total health in the United States is below 50 percent compared to the OCED countries with an average of 73 percent. In the adjusted for price levels United States spends $8,713 per head in 2013, whereas the average of OCED countries spends $3,453. This essay was reviewed by.
For more comparative health system data from the OECD, click here. A 2015 Commonwealth Fund brief showed that — before the major provisions of the Affordable Care Act were introduced — the United States had worse outcomes and spent more on health care, largely because of greater use of medical technology and higher prices, compared to other high-income countries. 1 By benchmarking the ...
This is an essay on health care issues in the United States, which highlights the challenges faced by Americans due to the high cost of medical care. Currently, around 44 million people in the US do not have any health insurance, and an additional 38 million have inadequate coverage. This issue is exacerbated by the exorbitant prices of drugs ...
Access to Healthcare in the United States Essay. One of humanity's biggest challenges is preventing harm to human beings by providing accessible health to everyone in the world. Thus, many governments struggle with that task. The recent COVID-19 pandemic further strained many countries' healthcare systems and revealed many issues.
The annual spending of health care increased from 75 billion in 1970 to 2.0 trillion in 2005 and is estimated to reach 4.0 trillion in 2015 (Kaiser Foundation, 2013). U.S. citizens spent 5,267 per capita for health care in 2002- 53 percent more than any other country" (2005). "America spent 5267 per capita and in Switzerland they spent 3074 ...
The US is very different from other nations in that we have one of the highest health care expenditures, making up 17.1% of our GDP, which is 50% more than any other developed nation. Even with these statistics, it is shocking to discover that population does not have a higher quality of life or better health compared to that of other developed ...
Scientists are still learning about the immediate and long-term health effects of using e-cigarettes. Dual use refers to the use of both e-cigarettes and regular cigarettes. Dual use is not an effective way to safeguard health. It may result in greater exposure to toxins and worse respiratory health outcomes than using either product alone. 2 3 ...
The first step providers often take in tailoring care to a patient's needs is screening, whether through a standardized instrument or informal conversations initiated by clinicians, social workers, or care coordinators. 7 Primary care providers, who serve as the "front door" to health care for most people, may be well positioned to screen ...
Background As of 2020, 20% of people residing in the United States of America (U.S.) lived in rural communities. Despite rural residents tending to be older, poorer, and having greater disease burden than their urban counterparts, the number of rural primary care providers continues to decline. Nearly 66% of U.S. Primary Care Health Professional Shortage Areas are designated as rural ...
Midwives and birthing centers need to be free to care for their patients in ways that maximize that patient's health and family, free of state control and threats of prison. This is a message ...
Fact sheets and other health, aged care and sport information from the 2024-25 Budget. Fact sheets and other health, aged care and sport information from the 2024-25 Budget. ... Help us improve health.gov.au. If you would like a response please use the enquiries form instead. What you were doing? (mandatory) What went wrong?
Americans, especially Medicare beneficiaries, are getting more medical care these days. Demand from aging Baby Boomers is keeping people in doctor's offices, and health care providers are ...
Glenn Thrush spent more than a year reporting this article, interviewing close to 50 people and reviewing court-obtained body-camera footage and more than 1,500 pages of documents.
Over 150 million Americans get their health care coverage from their employer through employer-sponsored insurance. These plans provide employees with access to high-quality, low-cost health care.