
- < Previous
Home > History Community Special Collections > Remembering COVID-19 Community Archive > Community Reflections > 21


Community Reflections
My life experience during the covid-19 pandemic.
Melissa Blanco Follow
Document Type
Class Assignment
Publication Date
Affiliation with sacred heart university.
Undergraduate, Class of 2024
My content explains what my life was like during the last seven months of the Covid-19 pandemic and how it affected my life both positively and negatively. It also explains what it was like when I graduated from High School and how I want the future generations to remember the Class of 2020.
Class assignment, Western Civilization (Dr. Marino).
Recommended Citation
Blanco, Melissa, "My Life Experience During the Covid-19 Pandemic" (2020). Community Reflections . 21. https://digitalcommons.sacredheart.edu/covid19-reflections/21
Creative Commons License

Since September 23, 2020
Included in
Higher Education Commons , Virus Diseases Commons
To view the content in your browser, please download Adobe Reader or, alternately, you may Download the file to your hard drive.
NOTE: The latest versions of Adobe Reader do not support viewing PDF files within Firefox on Mac OS and if you are using a modern (Intel) Mac, there is no official plugin for viewing PDF files within the browser window.
Advanced Search
- Notify me via email or RSS
- Expert Gallery
- Collections
- Disciplines
Author Corner
- SelectedWorks Faculty Guidelines
- DigitalCommons@SHU: Nuts & Bolts, Policies & Procedures
- Sacred Heart University Library
Home | About | FAQ | My Account | Accessibility Statement
Privacy Copyright
I Thought We’d Learned Nothing From the Pandemic. I Wasn’t Seeing the Full Picture

M y first home had a back door that opened to a concrete patio with a giant crack down the middle. When my sister and I played, I made sure to stay on the same side of the divide as her, just in case. The 1988 film The Land Before Time was one of the first movies I ever saw, and the image of the earth splintering into pieces planted its roots in my brain. I believed that, even in my own backyard, I could easily become the tiny Triceratops separated from her family, on the other side of the chasm, as everything crumbled into chaos.
Some 30 years later, I marvel at the eerie, unexpected ways that cartoonish nightmare came to life – not just for me and my family, but for all of us. The landscape was already covered in fissures well before COVID-19 made its way across the planet, but the pandemic applied pressure, and the cracks broke wide open, separating us from each other physically and ideologically. Under the weight of the crisis, we scattered and landed on such different patches of earth we could barely see each other’s faces, even when we squinted. We disagreed viciously with each other, about how to respond, but also about what was true.
Recently, someone asked me if we’ve learned anything from the pandemic, and my first thought was a flat no. Nothing. There was a time when I thought it would be the very thing to draw us together and catapult us – as a capital “S” Society – into a kinder future. It’s surreal to remember those early days when people rallied together, sewing masks for health care workers during critical shortages and gathering on balconies in cities from Dallas to New York City to clap and sing songs like “Yellow Submarine.” It felt like a giant lightning bolt shot across the sky, and for one breath, we all saw something that had been hidden in the dark – the inherent vulnerability in being human or maybe our inescapable connectedness .
More from TIME
Read More: The Family Time the Pandemic Stole
But it turns out, it was just a flash. The goodwill vanished as quickly as it appeared. A couple of years later, people feel lied to, abandoned, and all on their own. I’ve felt my own curiosity shrinking, my willingness to reach out waning , my ability to keep my hands open dwindling. I look out across the landscape and see selfishness and rage, burnt earth and so many dead bodies. Game over. We lost. And if we’ve already lost, why try?
Still, the question kept nagging me. I wondered, am I seeing the full picture? What happens when we focus not on the collective society but at one face, one story at a time? I’m not asking for a bow to minimize the suffering – a pretty flourish to put on top and make the whole thing “worth it.” Yuck. That’s not what we need. But I wondered about deep, quiet growth. The kind we feel in our bodies, relationships, homes, places of work, neighborhoods.
Like a walkie-talkie message sent to my allies on the ground, I posted a call on my Instagram. What do you see? What do you hear? What feels possible? Is there life out here? Sprouting up among the rubble? I heard human voices calling back – reports of life, personal and specific. I heard one story at a time – stories of grief and distrust, fury and disappointment. Also gratitude. Discovery. Determination.
Among the most prevalent were the stories of self-revelation. Almost as if machines were given the chance to live as humans, people described blossoming into fuller selves. They listened to their bodies’ cues, recognized their desires and comforts, tuned into their gut instincts, and honored the intuition they hadn’t realized belonged to them. Alex, a writer and fellow disabled parent, found the freedom to explore a fuller version of herself in the privacy the pandemic provided. “The way I dress, the way I love, and the way I carry myself have both shrunk and expanded,” she shared. “I don’t love myself very well with an audience.” Without the daily ritual of trying to pass as “normal” in public, Tamar, a queer mom in the Netherlands, realized she’s autistic. “I think the pandemic helped me to recognize the mask,” she wrote. “Not that unmasking is easy now. But at least I know it’s there.” In a time of widespread suffering that none of us could solve on our own, many tended to our internal wounds and misalignments, large and small, and found clarity.
Read More: A Tool for Staying Grounded in This Era of Constant Uncertainty
I wonder if this flourishing of self-awareness is at least partially responsible for the life alterations people pursued. The pandemic broke open our personal notions of work and pushed us to reevaluate things like time and money. Lucy, a disabled writer in the U.K., made the hard decision to leave her job as a journalist covering Westminster to write freelance about her beloved disability community. “This work feels important in a way nothing else has ever felt,” she wrote. “I don’t think I’d have realized this was what I should be doing without the pandemic.” And she wasn’t alone – many people changed jobs , moved, learned new skills and hobbies, became politically engaged.
Perhaps more than any other shifts, people described a significant reassessment of their relationships. They set boundaries, said no, had challenging conversations. They also reconnected, fell in love, and learned to trust. Jeanne, a quilter in Indiana, got to know relatives she wouldn’t have connected with if lockdowns hadn’t prompted weekly family Zooms. “We are all over the map as regards to our belief systems,” she emphasized, “but it is possible to love people you don’t see eye to eye with on every issue.” Anna, an anti-violence advocate in Maine, learned she could trust her new marriage: “Life was not a honeymoon. But we still chose to turn to each other with kindness and curiosity.” So many bonds forged and broken, strengthened and strained.
Instead of relying on default relationships or institutional structures, widespread recalibrations allowed for going off script and fortifying smaller communities. Mara from Idyllwild, Calif., described the tangible plan for care enacted in her town. “We started a mutual-aid group at the beginning of the pandemic,” she wrote, “and it grew so quickly before we knew it we were feeding 400 of the 4000 residents.” She didn’t pretend the conditions were ideal. In fact, she expressed immense frustration with our collective response to the pandemic. Even so, the local group rallied and continues to offer assistance to their community with help from donations and volunteers (many of whom were originally on the receiving end of support). “I’ve learned that people thrive when they feel their connection to others,” she wrote. Clare, a teacher from the U.K., voiced similar conviction as she described a giant scarf she’s woven out of ribbons, each representing a single person. The scarf is “a collection of stories, moments and wisdom we are sharing with each other,” she wrote. It now stretches well over 1,000 feet.
A few hours into reading the comments, I lay back on my bed, phone held against my chest. The room was quiet, but my internal world was lighting up with firefly flickers. What felt different? Surely part of it was receiving personal accounts of deep-rooted growth. And also, there was something to the mere act of asking and listening. Maybe it connected me to humans before battle cries. Maybe it was the chance to be in conversation with others who were also trying to understand – what is happening to us? Underneath it all, an undeniable thread remained; I saw people peering into the mess and narrating their findings onto the shared frequency. Every comment was like a flare into the sky. I’m here! And if the sky is full of flares, we aren’t alone.
I recognized my own pandemic discoveries – some minor, others massive. Like washing off thick eyeliner and mascara every night is more effort than it’s worth; I can transform the mundane into the magical with a bedsheet, a movie projector, and twinkle lights; my paralyzed body can mother an infant in ways I’d never seen modeled for me. I remembered disappointing, bewildering conversations within my own family of origin and our imperfect attempts to remain close while also seeing things so differently. I realized that every time I get the weekly invite to my virtual “Find the Mumsies” call, with a tiny group of moms living hundreds of miles apart, I’m being welcomed into a pocket of unexpected community. Even though we’ve never been in one room all together, I’ve felt an uncommon kind of solace in their now-familiar faces.
Hope is a slippery thing. I desperately want to hold onto it, but everywhere I look there are real, weighty reasons to despair. The pandemic marks a stretch on the timeline that tangles with a teetering democracy, a deteriorating planet , the loss of human rights that once felt unshakable . When the world is falling apart Land Before Time style, it can feel trite, sniffing out the beauty – useless, firing off flares to anyone looking for signs of life. But, while I’m under no delusions that if we just keep trudging forward we’ll find our own oasis of waterfalls and grassy meadows glistening in the sunshine beneath a heavenly chorus, I wonder if trivializing small acts of beauty, connection, and hope actually cuts us off from resources essential to our survival. The group of abandoned dinosaurs were keeping each other alive and making each other laugh well before they made it to their fantasy ending.
Read More: How Ice Cream Became My Own Personal Act of Resistance
After the monarch butterfly went on the endangered-species list, my friend and fellow writer Hannah Soyer sent me wildflower seeds to plant in my yard. A simple act of big hope – that I will actually plant them, that they will grow, that a monarch butterfly will receive nourishment from whatever blossoms are able to push their way through the dirt. There are so many ways that could fail. But maybe the outcome wasn’t exactly the point. Maybe hope is the dogged insistence – the stubborn defiance – to continue cultivating moments of beauty regardless. There is value in the planting apart from the harvest.
I can’t point out a single collective lesson from the pandemic. It’s hard to see any great “we.” Still, I see the faces in my moms’ group, making pancakes for their kids and popping on between strings of meetings while we try to figure out how to raise these small people in this chaotic world. I think of my friends on Instagram tending to the selves they discovered when no one was watching and the scarf of ribbons stretching the length of more than three football fields. I remember my family of three, holding hands on the way up the ramp to the library. These bits of growth and rings of support might not be loud or right on the surface, but that’s not the same thing as nothing. If we only cared about the bottom-line defeats or sweeping successes of the big picture, we’d never plant flowers at all.
More Must-Reads from TIME
- How Joe Biden Leads
- TIME100 Most Influential Companies 2024
- Javier Milei’s Radical Plan to Transform Argentina
- How Private Donors Shape Birth-Control Choices
- What Sealed Trump’s Fate : Column
- Are Walking Pads Worth It?
- 15 LGBTQ+ Books to Read for Pride
- Want Weekly Recs on What to Watch, Read, and More? Sign Up for Worth Your Time
Contact us at [email protected]
COVID-19: A year in reflections

As we mark a full year since the global pandemic upended all of our lives, we asked members of the UC community to share their reflections on how these past months have changed them, and what will stay with them about this unprecedented time in the years to come.
The picture that emerges is one of hardship, courage, gratitude and resilience. For many of us, the last 12 months have meant long hours and rising to meet new challenges with our teammates, families, communities and bubbles. We helped support others in their grief and were helped by others when grief came home to us. We found new strengths in loneliness and formed new practices and bonds to ward off despair.
Now, as we begin to see a little light at the end of the tunnel, here in their own voices, members of UC’s community look back on a year like no other.
On never falling off the treadmill

In the early days of 2020, two doctors, Daniel Uslan and Annabelle de St. Maurice , had already begun preparations with their colleagues in the command center at UCLA Health for the looming pandemic. As clinical chief of infectious diseases and co-chief infection prevention officer at UCLA Health, Dr. Uslan was working alongside Dr. de St. Maurice, pediatric infection control lead and co-chief infection prevention officer, nearly every waking moment. Their work spanned planning for patients, emergency preparedness, communications, and more.
“By the time California shut down non-essential businesses, I had already been working on COVID-19 for several weeks and my day-to-day life had already been thrown into chaos. In the early days I hoped, perhaps naively, that we would all hunker down for a few months and then the crisis would pass us by.”
As more information became available, that hope dimmed.

Dr. Tisha Wang put her entire life on hold when the pandemic hit — as the person overseeing pulmonary and critical care faculty and trainees for UCLA Health, she had no other option. It was clear, early on, that protecting health care workers from infection would be absolutely vital for saving the lives of the critically ill patients showing up at the hospital.
She describes those last three weeks of March 2020 as the worst three weeks of her career. Protecting the workforce, so they could protect the critically ill, was a heavy burden to carry. And as we know, that burden was carried for far longer than those three weeks (Dr. Wang speaks about the difficult experiences of saying goodbye to patients during the COVID-19 pandemic, here ). Dr. Wang:
“We wondered if it was ever going to end — the deaths, the grieving, the suffering, the stress and anxiety compounded by the social isolation. In our minds, how could this possibly go on for months to years? I felt like I was constantly running on a treadmill and close to running out of steam. To my disbelief, after 9 months of running, the speed of the treadmill was turned up by 50 percent when Los Angeles became the epicenter of the pandemic. I had no choice but to keep running, but was I going to fall off?
“What have I learned? This is actually a team-based marathon. I was never going to fall off of that treadmill. Someone was going to come along and tag me out and let me breathe and rest for a moment. And as soon as I got some water and air, I was going to jump back on and do the same for them.”
Now there is time, and hope, we can address this situation better in the future. Dr. de St. Maurice has begun to reflect:
“The pandemic has taught us many lessons about preparedness and health equity, among other things. What can we do better in the future to prevent pandemics like this from occurring? What modifications have we made in our lives as a result of the pandemic that are positive and how can we continue these in the future? What health care inequities have intensified as a result of the pandemic and how can we work to improve those inequities?
“In the past many physicians and health care workers would work when they weren’t feeling well and I think that will change going forward.”
On living in a bubble year
Steven Pease has been working part-time at home in his capacity in IT asset management, in a bubble with his wife, their children and her parents, one of whom, her father, passed just before turning 100 in October. Planning the funeral and sharing mourning in the pandemic was challenging, an experience shared by many. Still, Pease felt gratitude for his connection to his family.
“To be certain, some of this will go down in our collective memories as the worst of times. That said, to have been locked up in our little ‘bubble’ together; forced to navigate together uncertain and new waters, but to get to do so with someone I love was in some ways very, very special. I believe that someday I'll look back on this time and see it as some of the best.”

Valerie Simmermaker has been working remotely for the UCPath Center near Riverside and finding silver linings in the pandemic as a single mom.
“I would say for us the stay at home order — working and schooling from home has ultimately been really good for us. I have always been a single parent and my children were used to coming home from school alone, and helping with chores and cooking, sometimes even doing grocery shopping while I worked. This has allowed us to really bond, I am finally able to help them with school work and we eat dinner before 7 p.m., we have really gotten close during this time together.”

Darlene Alvarez at the UC Retirement Administration Service Center (RASC) has had similar experiences with her children, trying to juggle work and keep her children motivated and focused on their school work. One thing that has helped is carving out 30 minutes a day to read for pleasure or dance along to music videos (current favorite is “Levitating” by Dua Lipa featuring DaBaby)!
“Another way we cope with challenges is through creative expression. For instance, we’ve made parols (Filipino Christmas ornamental lanterns) and foam mosaic art. We’re also making more homemade dishes, like arepas (Venezuelan cornmeal cakes).”

Helping to guide our kids through the pandemic hasn’t been easy. Jennifer Mushinskie , a senior communications officer/interim operations liaison at the UCPath Center in Riverside and her son grappled with the loss of high school experiences you can’t get back, while still dealing with the social anxieties that are rampant in the teen years.
“It's heartbreaking to see a screen with 30 kids and only the teacher is on video. The kids aren't required to be on camera, per the district, so the teachers are frustrated, and the kids won't go on camera. I have tried to get him on video but he won’t – saying “Mom, that’s embarrassing if I go on and no one else does.
“Waiting has been exhausting on the kids mentally and physically. It's been a rough road. Our kids witnessed area businesses and mall parking lots filled with cars and shoppers, but they weren’t allowed to play in a high school football game or another type of school sport. We watched the Superbowl, with fans in the stadium, but our children in California weren’t in school or on the field. My son was so frustrated with this and it broke my heart. I’m grateful things are starting to get better.”
For Annette Dwyer , an accounts receivable associate at UCPath in Riverside, the pandemic brought her husband to her, then took him away, before returning him again.

“I married my Welsh boyfriend in July 2019, and had barely started the immigration process for my husband in January 2020, which was expected to take 12-18 months. We planned to pass the time with short visits. He was scheduled to visit in March 2020 to spend time with us during spring break, and for us to have a mini-honeymoon of sorts. That all changed when the executive order was issued on international travel to the U.S. (He barely made it on the plane and through customs thanks to a photocopy of my passport.) He was locked down with us in March, ‘getting stuck’ here for almost four months. We were devastated when my husband was called back to work and had to return to the U.K. in July. We did not know when we would get to see him again and hoped his immigration interview would be soon. (At that point, we were waiting to hear from the embassy.) He ended up receiving his interview in August and his immigrant visa was approved within an unheard of seven-month timeline. He immigrated here at the very end of August.”
On finding strength in community/new families
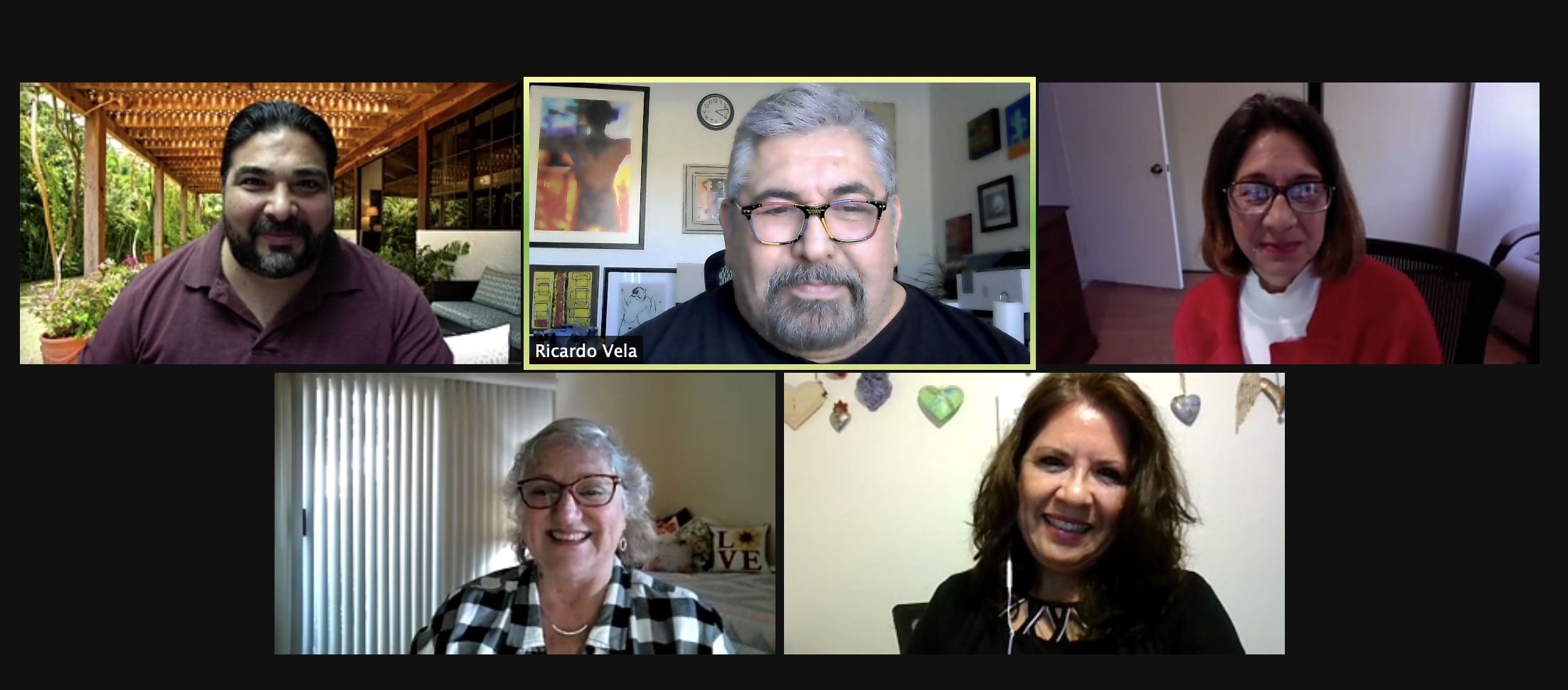
Ricardo Vela , who leads Spanish language news and outreach for UC’s Agriculture and Natural Resources division, has seen the pandemic turn his co-workers into family, the result of the intense bonds developed as they helped each other through the crisis. Several of his family members fell seriously ill with COVID-19, but recovered. Some of his colleagues were not so fortunate, and he and his team struggled through those moments together.
“As a team, during the pandemic, we have grown closer together. Even when we have not been in the same place for over a year, we pushed each other to think outside the box to accomplish our work's goals. We did better than ever before.
“But despite our success we fell at times into depression and anxiety, for days. When one of my staffers lost her father, we fell into despair, wondering "who is next?" We saw how personal the pandemic could get. It stopped being another headline and became real and painful.
“We shared tears of despair, impotence, and at times of joy! As a team, we pulled it together, we stopped being co-workers, and we became a family.
“A year after, I can say we are stronger, resilient. We learned that distance is only a click away, that we can express that love in many ways. We are ready to face the ‘new normal.’”

Azure Otani , a second-year business administration major at UC Riverside, felt “scared, lonely and claustrophobic” when the pandemic began. To cope, she pushed herself to become more (virtually) involved on campus — and in doing so, found a new sense of community. Today she holds officer positions in several student groups and has even mentored freshmen via text message.
“When the virus basically shut down the world at the snap of a finger, I thought I wasn’t going to be able to accomplish anything. Instead, I’ve been able to teach and learn from other people, and help bring meaning to their lives, just like they’ve brought to mine. I’ve never met any of them in person, but I know that many of them would have my back. I feel a true sense of community and am grateful for what I’ve learned in the process — what I value, how I like to work and the importance of taking time to reflect.
“I will forever be more conscious of the people around me — whether that is recognizing that I don’t know what others are going through or keeping my mask on when I’m sick. Life is extremely short and we don’t know when we’re going to lose everything we have. I know how important it is to spend my time with loved ones and reach out to give back as much as I can.”
On embracing change — and science

Heather Buschman , Ph.D., is assistant director of Communications and Media Relations at UC San Diego Health and an instructor at UC San Diego Extension. Since the start of the pandemic, her team has shared scientists’ stories and fact-based public information. She also volunteered at a vaccination site. From her unique perspective, Buschman has seen the magnitude of the pandemic, and the remarkable strides we’ve made.
“I was in my office when I heard that schools were closing. I ran to tell a coworker and choked with emotion over the gravity of the situation. For more than a month, I’d been serving shifts as a public information officer in our incident command center, which activated to manage coronavirus patient care and protect health care workers. But until then the pandemic hadn’t really affected my family.
“Until they arrived at UC San Diego Health, I never believed we’d have COVID-19 vaccines by early 2021 — and yet here we are, administering multiple, highly effective vaccines since late 2020. I’m blown away by what the scientific community has accomplished with so many people working together, focused on a single problem, with appropriate funding. I’m proud to tell scientists’ stories and play a small part in distributing vaccines to our community. It’s truly historic.”
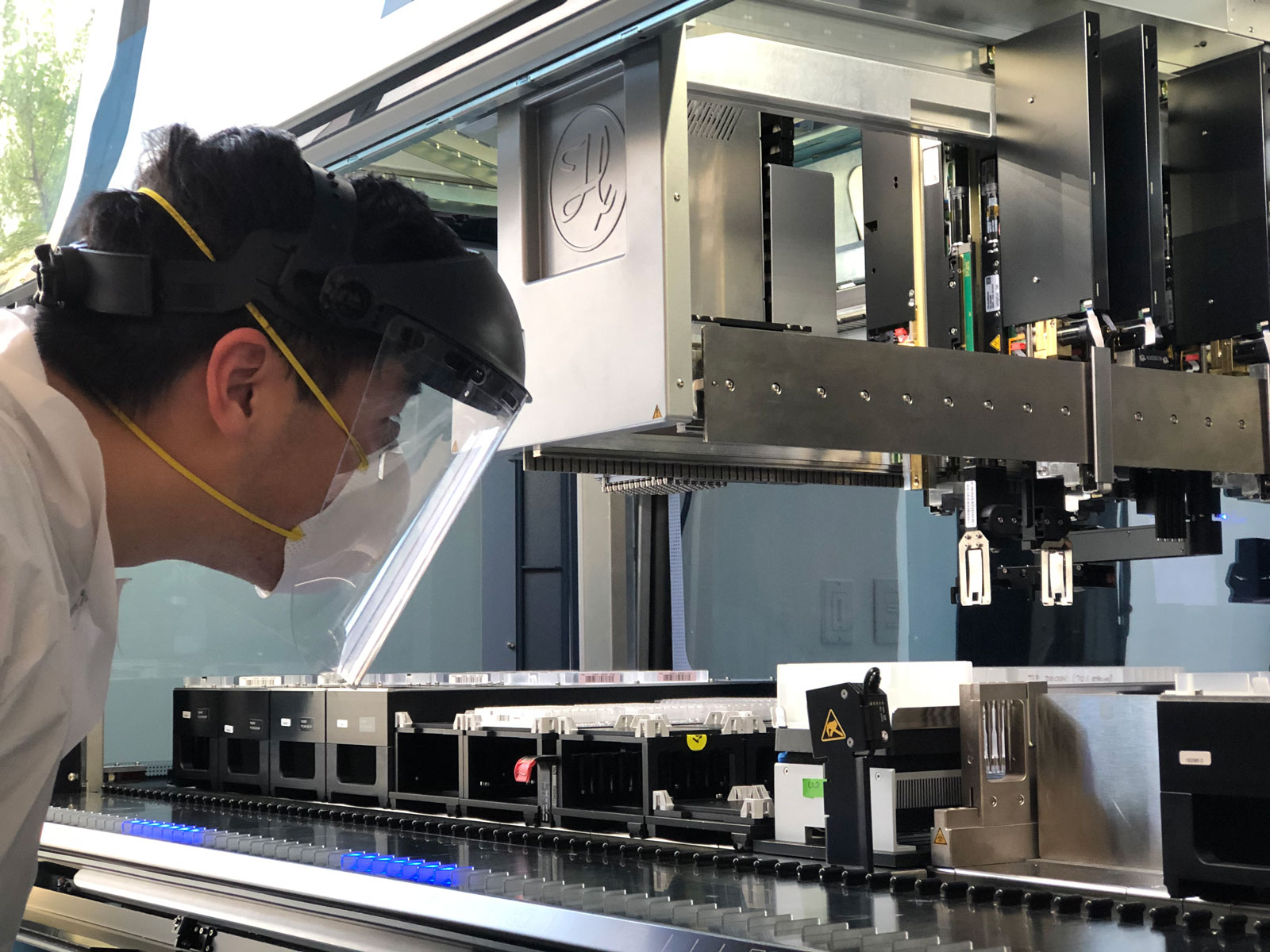
Connor Tsuchida is a graduate student in Jennifer Doudna’s lab at UC Berkeley, working on research related to the gene-editing technology known as CRISPR. When the pandemic hit, he and his colleagues at the Innovative Genomics Institute put aside their regular research to stand up a COVID rapid-results testing lab to meet the urgent need for COVID diagnoses. The transition from one new frontier of science to another wasn’t easy.
“For a [disease] testing lab, the concepts are not the same as genetic engineering, but the skills and technology you use is similar. We knew some of the techniques and protocols of diagnostic testing, and we were familiar with the equipment. That gave us a leg up so we weren’t starting from zero.
“One of the best things has been the opportunity to work with professionals from other fields: volunteer physicians from UC Berkeley’s student health center, people from public health — it’s a multi-disciplinary, team endeavor.
“For me, it’s also been a lesson in setting something up and then being okay with transitioning it to other people. There’s a controlling nature with research that if you are going to do it right, you need to do it yourself. It’s a good experience to hand off what you helped establish and see it take on a life of its own.”
Another bright spot: Tsuchida’s work in biomedical research now seems more vital than ever — and not only to those in the field.
There was so much work done in science and research before the pandemic that we absolutely were able to build upon when developing therapies and vaccines for COVID-19. I hope this will bring home the importance of that research and encourage everyone to support putting money into science.
Teresa Andrews, M.S., is an education and outreach specialist at the Western Center for Agricultural Health and Safety at UC Davis, focusing on the workplace health and safety of farmworkers. Before the pandemic, Andrews and her team hosted in-person trainings for farmworkers and employers across California. COVID-19 forced them to reinvent their approach while maintaining connections with agricultural communities.
“We adapted our interactive activities to a virtual platform and started learning all we could about what farmworkers needed to know about COVID-19 and how employers could reduce workplace infections. Our goal was to be a resource, alleviate fears and empower workers and employers with the knowledge they needed to operate within this new reality.
“Since then, we’ve mastered the use of technology to fill the gap and stay connected. We offer more presentations and workshops than ever before and are reaching more people throughout our region, connecting with workers wherever they are. It brings me satisfaction to counter fears with science; to help explain concepts that can seem abstract to people — what a virus is, how your body responds, and what you can do to reduce the risk of infection — in language that’s easy to understand.”

Paul Kasemsap , an international student from Thailand, stayed close to campus partially to care for the plants he studies. But he also found himself drawn to the local Davis community, volunteering with the food bank to bring groceries to those most at-risk for COVID-19, so they didn’t have to risk trips to the store.
“After this is over, I hope we continue to take care of and check in with each other. I had indeed been taking in-person interactions and small talk for granted. But the pandemic showed me how powerful a role social support plays in our life. I hope we continue to tell our loved ones how much we love them and appreciate their support. Don't wait until the next pandemic!”
Aaron Zachmeier , UCSC Online Education instructional designer, helped hundreds of faculty put their classes online virtually overnight.
“Before the pandemic, the unit I'm in, Online Education, worked with a relatively small number of faculty on online and hybrid courses. We were kind of a boutique unit. When the shut-down happened, we started working with people all over campus.
“My colleagues and I created all sorts of resources to help with the transition to remote teaching and learning and remote working: workshops, self-paced courses, videos, text tutorials, checklists, infographics.
“We had a chat/discussion space that we opened up to all staff and faculty for the pandemic, and it has now become a lively place that spans departments and administrative units. People ask questions and have conversations about technology, teaching, and policy. Those conversations will continue.
“All of those people who started working together to facilitate the transition to remote are still talking regularly. They'll keep talking. That's a wonderful change.”
On improvising

Frida Hernandez is a Class of 2020 UC Berkeley grad. As the first in her family to graduate from college, she was looking forward to celebrating her big day with her family. While a virtual graduation wasn’t what she had hoped for, she was still able to share her accomplishments alongside her family at home in San Diego.
“Graduating in the middle of a pandemic as a first-gen student was tough because I felt the pressure to have my next steps all figured out to make my family proud. I have two younger siblings who are currently in high school, so I wanted to set a good example for them. Luckily, I was able to find a job in my field and I am so grateful I did. Landing my first full-time job in the middle of a pandemic gave me a new perspective on life because I was thankful to find some stability amidst all the chaos. I’ve really enjoyed spending time with my family (in my household) during this time. I moved back in with them after graduation and I’m grateful we have each other during these difficult times.
“As we begin to resume ‘normal’ life, I will live my life with more intention and gratitude. I hope to make up for all the celebrations I missed out on during this past year, such as my college graduation and numerous birthdays.”
In normal times, UC Santa Barbara’s Saameh Solaimani works as an early education specialist at the campus child care center. When the pandemic forced it to close, Solaimani quickly found new ways to help UC families by starting a website, www.ourchildrenscenter.org , that provided a high-quality resource for early child educators and those with young children.
“To see the pivot that so many teachers have made to ensure the healthy development of their students and learning communities, from pre-school all the way through higher-ed, has been incredible. These circumstances have reaffirmed what I knew to be true: That we, in the field of education, got into this work with hope for a better future and we are relentless with that hope, which is what keeps us going.”

Glenn Beltz is a mechanical engineering professor and associate dean at UC Santa Barbara. When the pandemic first hit, he saw first hand that family circumstances made online learning difficult for many students — there were no simple solutions. He and his academic advising team rose to the challenge by providing individual guidance to help as many students navigate the situation as possible. The Academic Senate’s decision at UC Santa Barbara to allow flexibility with pass/no pass grading was a huge help for students, allowing courses to count toward their degree requirements.
His own family faced different, but equally challenging circumstance with online learning.
“I am a parent so the kid aspect strikes a nerve. It has been rough. My wife and I have 2 kids, a daughter in 10th grade and a son in 4th grade. It has been particularly difficult with my son, who is autistic. Every autistic kid is different, but there is no way you could get my son to sit in front of a Zoom session for hours on end. No way at all. I fear that much of this past year will be a lost year in terms of his education. Fortunately, in January ’21, his elementary school worked out a protocol to be able to take him and a few other special-needs kids back. That has been a godsend.”
But he expects to take some positives forward.
“There are many aspects of teaching that I hope will remain in the long term. I think it’s awesome that students can pull a set of notes online from whatever I taught on a given day or even pull a recording of the lecture. Sure, that kind of stuff occurred in former times, but it was not widespread. I don’t think I will ever give a paper-based, sit-down exam again. I like being able to administer and grade exams online via various tools that are available.”
Top photo: One of Frida Hernandez’s journals from the pandemic.
Keep reading
3D-printed ‘living material’ could clean up contaminated…
Combined with a seaweed polymer, a bacteria associated with algae blooms can actually make water cleaner — then eliminate itself when it is done.

More than half of UC transfer students pay no tuition: 8…
The cost of transferring to UC shouldn’t keep you up at night. Here are 8 encouraging facts about affordability at UC.
- Skip to main content
- Keyboard shortcuts for audio player

- LISTEN & FOLLOW
- Apple Podcasts
- Google Podcasts
- Amazon Music
- Amazon Alexa
Your support helps make our show possible and unlocks access to our sponsor-free feed.
Reflections On Coronavirus A Year In
Madeline K. Sofia

Rebecca Ramirez

Emily Kwong

An elderly couple wearing face masks walks in Madrid on April 30, 2020 during a national lockdown to prevent the spread of the COVID-19 disease. Gabriel Bouys/AFP via Getty Images hide caption
An elderly couple wearing face masks walks in Madrid on April 30, 2020 during a national lockdown to prevent the spread of the COVID-19 disease.
It's been about a year since the World Health Organization declared the coronavirus a pandemic. The world has learned a lot in that time — about how the virus spreads, who is at heightened risk and how the disease progresses. Today, Maddie walks us through some of these big lessons.
Follow NPR's continued coverage of the coronavirus pandemic.
Helpful links from the episode:
- How To Protect Yourself From Aerosol Transmission
- Risk for COVID-19 Infection, Hospitalization, and Death By Race/Ethnicity
- The Key To Coronavirus Testing Is Community
Reach the show by emailing [email protected] .
This episode was produced by Rebecca Ramirez, edited by Gisele Grayson, and fact-checked by Rasha Aridi. Stacey Abbott was the audio engineer. Special thanks to Ariela Zebede and Leah Donella.
A year later: Reflections on learning, adapting, and scaling education interventions during COVID-19
Subscribe to the center for universal education bulletin, tendekai mukoyi , tendekai mukoyi education program coordinator - youth impact molly curtiss wyss , and molly curtiss wyss senior project manager and senior research analyst - global economy and development , center for universal education jenny perlman robinson jenny perlman robinson nonresident senior fellow - global economy and development , center for universal education @jennyperlman.
April 2, 2021
Already more than a full year into the COVID-19 pandemic, it is sobering to reflect on the ongoing responses to the global pandemic, as well as future disruptions to children’s learning. The past year has really put to the test scaling principles and elucidated important lessons about catalyzing and sustaining transformative change in rapidly evolving contexts. Many of these principles—such as adaptive learning and systems thinking—are being unpacked and explored in Real-time Scaling Labs (RTSL), a collaboration with the Center for Universal Education at Brookings and local institutions and governments around the world to learn from, document, and support education initiatives in the process of scaling.
In Botswana, Young 1ove and CUE have been partnering on an RTSL convened by the Ministry of Basic Education (MoBE) focused on scaling Teaching at the Right Level (TaRL). The experience of the Botswana scaling lab over the past year offers several important insights and reflections that may be useful more broadly for those working to affect large-scale improvements in children’s learning, particularly in low-resource environments.
Insight 1 : National scale can be pursued from the top down and bottom up
Expanding and deepening the impact of an education intervention requires nurturing partnerships from grassroots to national levels, with the understanding that buy-in and ownership for scale needs to involve players at all levels. Young 1ove has been collaborating closely with the MoBE at the central offices to support progress toward the ultimate goal of infusing TaRL into daily teaching practices in all primary school classrooms in Botswana. However, the past year has revealed significant potential for scaling via regional pathways, as many stakeholders at the highest levels of government have been consumed by national responses to COVID-19-related school closures and health crises.
For example, MoBE partners in the North East region took the lead in reinstating TaRL as schools reopened by mobilizing teachers and school-based youth volunteers to restart the program even amid shorter shift-system school days (where students attend classes in shift for half the day rather than for the full day). North East regional leaders also adapted TaRL delivery in response to COVID-19, including creating safety protocols that adhere to COVID-19 health protocols and taking full ownership of TaRL data collection and submission by utilizing existing school-based tablets. Student learning results from the region show a 79 percent decline in innumeracy, a near doubling of students who could perform all mathematical operations, and 57 percent of students learning a new operation, further evidencing how strong regional leadership can catalyze change that directly impacts children’s learning.
The success in North East illustrates how scale-up efforts can be made more powerful and sustainable when led by regional directors in the MoBE. The partnership between Young 1ove and the MoBE jointly supporting TaRL implementation prior to COVID-19 likely facilitated this approach, as regional stakeholders already had the tools and knowledge in place to take TaRL implementation and run with it.
Insight 2: Local champions leading the charge on the ground can be particularly important, even in a virtual world
Key to a regional scaling approach has been the role of a supportive and enthusiastic MOBE regional director. Young 1ove already knew that changemakers in bureaucracy are central to the scaling process, but this has proven especially true at the regional level, where an engaged director who champions TaRL can make significant progress in advancing and prioritizing TaRL within the region.
Further, Young 1ove has found that embedding a staff member in the regional government has been a particularly powerful scaling asset. Even as the world has shifted to virtual meetings and phone calls, having someone from Young 1ove physically present has helped the organization remain actively involved in and aware of conversations and schooling decisions. Moreover, the integration of this staff member in the regional government supports the shift to seeing TaRL as a sustainable government program led by strong regional champions. In regions where they do not have a staff member embedded, Young 1ove has found lapsed communication over the past year and faced more challenges “restarting” TaRL after COVID-19 school closures.
Insight 3 : Short-term shocks can lead to long-term learnings
The COVID-19 pandemic has demonstrated the absolute need to be flexible, adaptive, and responsive to changes in the education landscape in real-time. This experience has also underscored the importance of evidence and learning alongside adaptation and rapid response.
The TaRL implementation cycle in Botswana is typically designed to last 30 days. However, as a result of COVID-19, the implementation period was cut by over half during the first term of the 2020 school year with an average implementation period of eight days across schools. To understand the impact of this significant shift, Young 1ove collected data on student learning outcomes and discovered that despite the reduced intervention time, students demonstrated strong learning gains—almost equal to previous 30-day cycles as shown in Figure 1.

This finding not only suggests that even relatively short periods of high-quality implementation can improve student learning, but also underscores the importance of tracking results—even during unexpected adaptations. In this case, tight feedback loops provided evidence of possibilities for refining the TaRL model beyond this pandemic in ways that maximize effectiveness and scalability.
Learnings for beyond the pandemic
The RTSL experience adapting and scaling TaRL in Botswana in the midst of a global pandemic offers key insights that are applicable well beyond this immediate pandemic:
- An orientation toward rapid learning and evidence generation is key to maintain alongside innovation and adaptation, especially in a crisis like COVID-19. Balancing the need for adjustments and iteration with the collection and use of timely data and learning can help respond to disruptions of scaling efforts.
- Focusing on regional/grassroots partnerships for scaling can be particularly effective as those closest to the problems are most often best placed—and have the most incentive—to respond. Even where the ultimate goal is national scaling or ownership of the initiative by the central government, a more decentralized approach to scaling can be an effective way to make progress toward this goal, especially when national-level actors are consumed by crisis-response.
- And, finally, even in a more virtual world, regional and local champions present on the ground are important for maintaining scaling momentum and expanding impact.
Photo credit: Thimonyo Karunga, Northeast Sub-Regional Coordinator at Young 1ove
Related Content
Gabby Arenge, Jenny Perlman Robinson
October 31, 2019
Rebecca Winthrop, Mahsa Ershadi, Noam Angrist, Efua Bortsie, Moitshepi Matsheng
November 2, 2020
Jenny Perlman Robinson, Molly Curtiss Wyss, Patrick Hannahan
June 24, 2020
Global Education
Global Economy and Development
Center for Universal Education
Millions Learning
Emily Markovich Morris, Laura Nóra, Richaa Hoysala, Max Lieblich, Sophie Partington, Rebecca Winthrop
May 31, 2024
Online only
9:30 am - 11:00 am EDT
The Brookings Institution, Washington DC
8:30 am - 4:30 pm EDT
Caring for the self and others: a reflection on everyday commoning amid the COVID-19 pandemic
- Reflective Essay
- Published: 24 August 2020
- Volume 2 , pages 243–251, ( 2020 )
Cite this article

- Chun Zheng 1
43k Accesses
6 Citations
11 Altmetric
Explore all metrics
In this essay, I share my experiences and reflection on fighting the COVID-19 pandemic from the perspective of a Chinese student residing in Pittsburgh, USA. Three examples of “commoning”—acts of managing shared resources by a group of people—reveal the importance of care and collaboration in the time of uncertainty. First, when COVID-19 posed a threat to the food supply chain, community gardens and home gardening ensured food security and enhanced mutual support. Second, the emergence of online activities of teaching, learning, and collaborating presented an opportunity of having more collective, equitable, and diverse formats of virtual communities. Lastly, volunteering in the distribution of “Healthy Packs,” I witnessed the nurture of a sense of belonging and a connection with home in the student community. These examples suggest that facing the crisis, care-driven commoning activities at the individual, everyday level lay the foundation for large-scale collaborative systems.
Similar content being viewed by others

How phenomenology can help us learn from the experiences of others

The Person-Centred Nursing Framework
Conducting qualitative research online: challenges and solutions.
Avoid common mistakes on your manuscript.
1 Commoning in a crisis
The COVID-19 pandemic is sweeping the planet. We, as individuals in the extended human family, are living through a crisis together. Within the vast and daunting global crisis are changes to every person’s daily life. These changes reveal the normally hidden human needs of care and collaboration and force us to re-invest in ourselves and our communities. In this essay, I share my personal experiences since the beginning of the pandemic and my observations of care-based everyday commoning activities over this period from the perspective of a Chinese student residing in Pittsburgh, USA (Fig. 1 ). Commoning, as defined by Gibson-Graham et al. ( 2013 ), takes place when a group of people is motivated by an ethic of care for a flourishing and sustainable common future and decides to manage shared resources in a collective manner. After discussing three examples of everyday commoning: gardening as commoning, online sharing as commoning, and volunteering as commoning, I reflect on the potential of expanding the sentiment of care for ourselves and others into larger-scale collaborative networks.
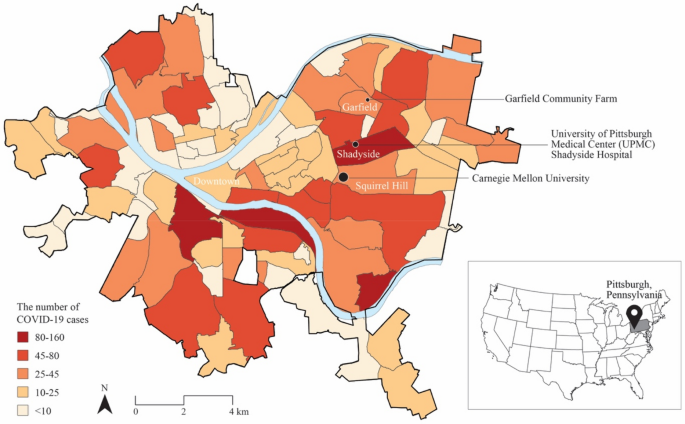
Spatial pattern of COVID-19 cases in Pittsburgh neighborhoods. Locations mentioned in this paper are highlighted. The map was created by the author based on the open data accessed on July 28 from Allegheny County Public Health Department ( https://www.alleghenycounty.us/Health-Department/Resources/COVID-19/COVID-19.aspx ) and Esri ArcGIS Database ( https://www.esri.com/en-us/arcgis/products/arcgis-online/resources )
2 From one epicenter to another
January 23rd, the day before the Chinese Lunar New Year’s Eve, the news that Wuhan and three other surrounding cities were going into lockdown Footnote 1 struck all TV channels in China. While words of the spread of a new type of pneumonia had been circulating for days (Wee and Wang 2020 ), Wuhan’s lockdown marked the start of an unprecedented national struggle and later, a global crisis.
Although physically stranded overseas, I could hear the worry in my family and friends’ voices over the phone. The anticipated joy of the annual family reunion was completely overwhelmed. In the following month, tracking the number of confirmed cases and the death toll became my daily routine. Watching more and more cities turn into darker colors Footnote 2 on the color-coded live COVID-19 tracking map put me into fear and homesickness.
Subsequently, I observed, in Pittsburgh, USA, personal protective equipment (PPE) in nearby pharmacies were almost sold out by February (Fig. 2 ). I collected 80 masks from over 10 shops in our region, most of which were the last bundles left for sale, to mail to a police friend working at the frontline in China. By the time I was ready to mail out the package, all flights to and from China had been banned (Corkery and Karni 2020 ). The travel ban not only meant the package would not have guaranteed delivery in the foreseeable future, but also put me into the mentality of being cut off from my homeland. Throughout February, via WeChat, Footnote 3 family and friends shared stay-home updates, cheered up each other, and even guided me to prepare for a potential COVID-19 outbreak in Pittsburgh. Geographical separations and time differences didn’t prevent us from caring for and supporting each other.

Last of N95 masks left in a Home Depot, 13 miles away from central Pittsburgh (February 2, 2020. Photography provided by the author)
On March 16, when most students were in the spring break, Pittsburgh officially reported its first two cases, Footnote 4 which meant educational entities had to make different decisions. Pittsburgh heavily relies on its education industry. The student population takes up 27% of the total population of the city. Footnote 5 Therefore, schools, preceding other public and private sectors in the city, responded to the outbreak first by switching to online classes, which lowered the risk of infection and spreading of the virus in the city that might be caused by students’ domestic and international travel. Still, I believe more earlier actions could have been implemented citywide and nationwide, including social distancing, encouragement to wear masks, and cancellations of large gatherings, to name a few. Nonetheless, what seemed so obvious to me, or to any Chinese citizen living in the USA, turned out to be invisible to most Americans, especially politicians and decision makers. The US government was overly optimistic about the epidemic and focused its resources on political rivalries, thus missing early opportunities to contain the outbreak. Compared with the constant and rolling media coverage of self-help prevention measures in China, the American people were given confusing and sometimes contradictory information, which blurred the severity of the pandemic. The rest of the story is well known. The malfunction of the government, the partisan differences, the sacrifices of healthcare workers, the hoarding of living essentials and weapons, etc., have become new abnormal norms in the USA. In these selfish, divisive and confusing situations, it is inevitable for many to find alternatives to self-help.
The duality of my experiences in two epicenters—the USA and China—has inspired me to recognize and cherish the spirit of mutual support and sentiment of care from others, as well as rethink where we can individually begin to act upon and contribute to forming a more collaborative and interconnected world. It took a long time for the majority of the world to realize that “the well-being of the group is endangered by indifferent individuals, and that community means originally simply a pooling of duties” (Jones 2020 , para 9). As individuals, we are incapable of changing the irreversible crisis; our duties lie simply in small everyday commoning actions.
3 Care and commoning
Commoning is the act of managing and sharing material and non-material resources, of creating things together, and of cooperating to meet shared goals among a group of people (Bollier and Helfrich 2015 , p. 17; Džokić and Neelen 2015 , p. 15; Bollier 2014 , p. 15). The participants in commoning processes are people who prioritize care for one another. Volunteering, altruism, selflessness, peer-assistance, mutual support, and so on can all be considered synonyms of commoning (Bollier 2020 , para 10). Prior to the pandemic, the logic of commoning can be found in cooperatively managed forests, social currencies, open-source software, citizen-managed urban spaces, community gardens, cooperative housings, and more. Commoning has been and is prevalent around the world as an essential survival strategy, especially in challenging times (Troncoso 2020 ; Baibarac and Petrescu 2017 , p. 229). We can, moreover, note that when governmental or market systems fail in the crisis, more people are finding their ways to support others through commoning—for instance, in the USA, crowdsourcing masks and ventilators, and mobilizing food bank resources for the elderly living alone amid the COVID-19 pandemic. A critical emotional motivation behind these commoning activities is care.
Our perception of care often draws on the traditional imaginaries of the parents’ domestic responsibility of taking care of children and the housework, or the healthcare workers’ job of providing service in the medical sphere. On the one hand, the ongoing pandemic has brought these traditional imaginaries of care into the spotlight. Healthcare workers who haven’t been paid enough appreciation are now deemed essential and thus regarded with greater value than before (Fig. 3 ). Households are forced to devote increasing time in domestic caregiving during physical distancing. On the other hand, the current crisis also triggers our rethink of alternative ways of caring beyond these formats (Morrow and Parker 2020 ; Thackara 2015 ; Petrescu and Trogal 2017 ). Here, I argue that care, manifesting in ways of verbal encouragement, physical gestures like waving and hugging, a sense of responsibility, commoning activities, etc., is a more inclusive concept than the traditional perception of care. It is a deep-rooted ability of human beings to resonate and connect with others. As Sennett claims, “Buried in all of us is the infantile experience of relating and connecting to the others who took care of us” (Sennett 2012 , p. 9). The pandemic is a catalyst for awakening people’s innate ability to care. We can all find ways to care for the self and others. The following examples aim at sharing my encounters of care-driven everyday commoning activities during the COVID-19 pandemic. They manifest that commoning is one of the most efficient ways of caregiving and is essential for not only our current survival but also a collective caring future.

“Heroes at work” slogans were displayed in the garden and on the building façade of the University of Pittsburgh Medical Center (UPMC) Shadyside Hospital in Pittsburgh, USA (May 5, 2020. Photography provided by the author)
4 Gardening as commoning
The top priority for individuals in quarantine is food. The food supply chain, including food production, processing, distribution, consumption, and disposal, needs to be operational for all of us to survive. However, the current food supply chain is severely compromised by COVID-19. According to the Washington Post (Telford and Kindy 2020 ), over 30 meat plants across the country owned by major American meat processing companies reported coronavirus outbreaks in their factories. The plants were forced to shut down because of growing numbers of confirmed cases and lack of PPE. Meanwhile, the transportation and distribution links on the supply chain also face unprecedented challenges. High demands for food delivery services put drivers and distributors at risk, as the virus can stay viable on cardboard boxes or plastic bags for a few days. Footnote 6 Both the processing and distribution links on the food supply chain are weakened, which has turned tons of milk, vegetables, and meat into waste.
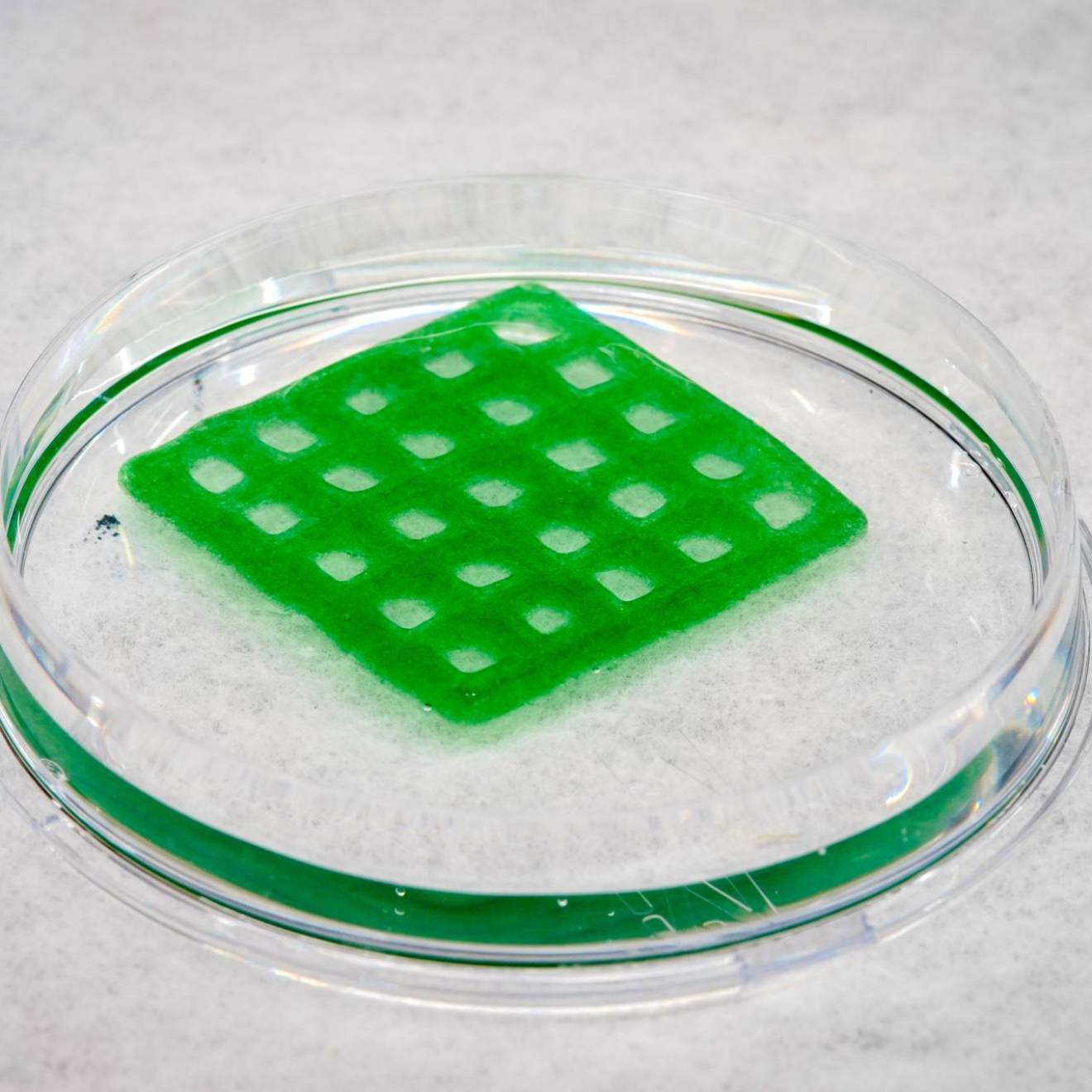
Recognizing the vulnerability of a long food supply chain, many individuals and nonprofit organizations, such as community gardens, community farms, and home gardeners, have made contributions to shorten the food supply chain. By securing their own and local food supplies, they reduce the reliance on processing and transportation links on the chain (Fig. 4 ). In the Pittsburgh neighborhood of Garfield, the Garfield Community Farm, despite suffering from a large loss of financial income and voluntary labor during COVID-19, decided to donate all their sales to restaurants to the poor and healthcare workers in the neighborhood (Fig. 5 ). On the other side of the globe, the Knowledge and Innovation Community (KIC) Garden in Shanghai initiated a SEEDING campaign to facilitate community trust-building amid the pandemic (Jian 2020 ). The campaign encouraged people to develop a self-sufficient lifestyle at home and to share their home-grown produce and seeds with neighbors in non-contact ways. Many creative participants designed, modeled, and built small exchange stations in their local communities. Conversations among neighbors were triggered upon the implementation of these stations. Several weeks ago, I joined the SEEDING group and started to share the progress of my own home seeding project. Quick growing herbs, like basil and oregano, are optimal for apartment dwellers like me. My project is still gradually expanding with handmade hydroponics of onions, green onions, and garlic (Fig. 6 ).
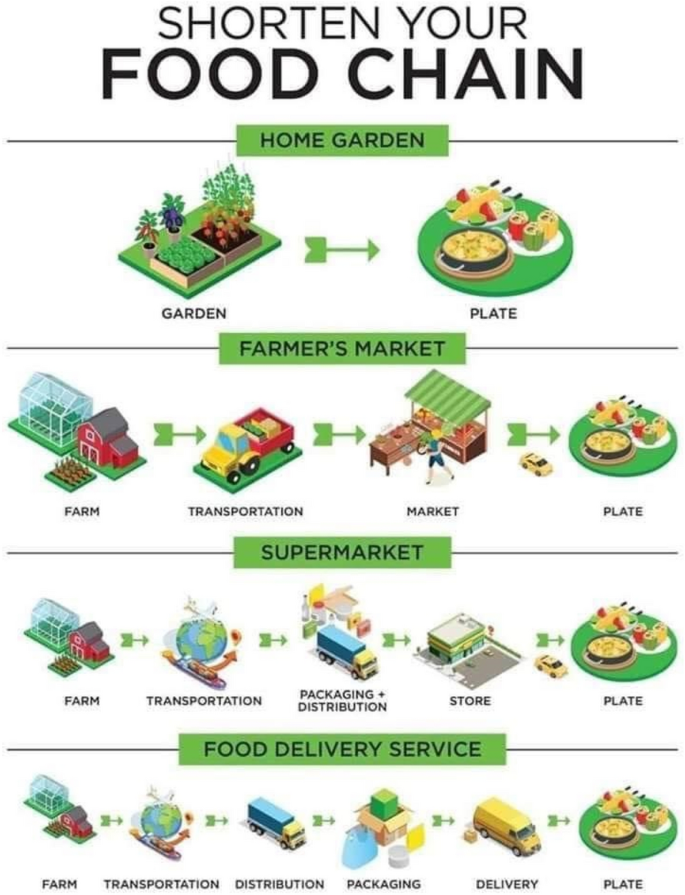
Food supply chain infographic (Source: Sandia Seed Company. https://www.sandiaseed.com/blogs/news/shorten-your-food-chain-infographic . Accessed by the author on May 5, 2020)

On March 25, the first donation was made by Garfield Farm since the stay-at-home order was placed in Pittsburgh (Source: Garfield Community Farm Facebook page. https://www.facebook.com/GarfieldCommunityFarm . Accessed by the author on April 25, 2020)

The author’s home planting project on the windowsill (June 26, 2020. Photography provided by the author)
Gardening as a commoning practice has both ecological and social benefits. Growing and eating locally reduces the energy consumed in processing and transportation and rebuilds the connection between people and nature, which is a way to care for the environment. At the same time, less consumption of processed food lowers the risk of exposure for workers in food processing and transportation industries. Gardening also brings people together, either by engaging people in the farm work or by allowing people to share their gardening knowledge with others. When sharing updates of my home gardening project in the SEEDING group, I received detailed guidance and encouragement from other home gardeners. The communication, care, and enlightenment from others in this turbulent time have become an indispensable source of life motivation. That is to say, gardening as a commoning activity is also a way to care for our social well-being. It creates connections among people with diverse social and cultural backgrounds in the time of physical separation.
5 Online sharing as commoning
Currently, the majority of family networks, businesses, and schools depend on online video communication technology. Many online activities of working, teaching, learning, collaborating, and sharing have emerged. The heavy reliance on the online video conference platforms (e.g., Zoom, one of the most widely used Apps) raises the question of how technology might contribute to a more inclusive and equitable future for knowledge exchange and socialization.
Even when the world comes to a halt, intellectual flows and simulations do not. Professor Jeffrey Hou from the University of Washington, Seattle, initiated a platform named disCO-commons: Distance Collaboration Commons in Support of Design for Social Change, Footnote 7 on which scholars, students, educators, and practitioners in architecture, design, and planning could contribute to a collection of academic resources. Discussions and debates around design thinking are also continued with Design Baithak, Footnote 8 a weekly Zoom event organized by Ahmed Ansari, an assistant professor at New York University. The discussants come from all parts of the country and across continents. Besides, many international conferences in academia have also switched to free online formats. Distance, time, and financial concerns are no longer barriers. In pre-pandemic times, academic collaborations at such scales would take months to plan and coordinate. COVID-19 and technology have miraculously pushed the progress of remote knowledge sharing and collaborations.
Concurrently, online social activities are taking place exponentially. Figure 7 shows a screenshot of our 2018 Carnegie Mellon Master of Urban Design alumni reunion, held on Zoom. Two years after graduation, friends from five different countries, across three continents, managed to meet virtually. Some of us are foreigners staying in the USA, some traveled home before the outbreak, and some are in their homeland but separated from the family. The moment we saw each other, memories of us being physically together were recalled. Technology shortened the geographical distance between us. Figure 8 shows an online yoga class that I joined. The teacher just completed her yoga training in Portland, Oregon, and kindly provided free online classes. In such a time of uncertainty, spending some time each day doing yoga, meditation, or stretching is a good way to relieve the anxiety and despair that the mainstream social media is trying to render. When the body is relaxed, the mind becomes composed.

Virtual alumni reunion (April 10, 2020. Screenshot provided by the author)

Remote yoga class (April 26, 2020. Screenshot provided by the author)
Despite the challenge of video bombs and internet interferences, online sharing has brought genuine excitement for the possibilities afforded by unique forms of information caregiving. With careful application and management of new technology, virtual communication has shown outstanding efficiency in (re)connecting people and promoting more accessible ways of education and socialization. Now that we have a firmer grasp on the planning, coordination, and execution of these online activities, we may start to imagine a network of virtual commoning.
6 Volunteering as commoning
It seems that our hands are tied because of the limitation of face-to-face contact with others. However, challenges always prelude opportunities. Coronavirus interrupts our normal socialization but offers unique volunteering opportunities that call for reciprocity among strangers. In April, the Carnegie Mellon University (CMU) Chinese Students and Scholars Association (CSSA) were planning to distribute packs of personal protective supplies sent by the Consulate General of PR China in New York to CMU Chinese students. I signed up to be the volunteer and was assigned to be the driver and distributor for our apartment building and several surrounding blocks (Fig. 9 ). Myself and 20 other volunteers collectively coordinated the transportation and distribution of over a thousand “Health Packs” with the assistance of CSSA staff, brainstorming and deciding the best timing, location, and method of distribution. The quick reaction and organization were all from the bottom-up. Two other volunteers and I took advantage of the fact that the foyer of my apartment building is separated from the lobby by a glass door. We placed the bags in the foyer and waited in the lobby (Fig. 10 ). Remaining mindful of social distancing rules, recipients came and lined up on the sidewalk outside the foyer. Each person who entered the foyer showed us their student ID against the glass door to confirm the pickup. For residents in the building, a digital signup sheet was circulated for them to fill in their apartment numbers. Based on the signup sheet, we left the bags directly in front of their apartment doors. Volunteering in this distribution, I witnessed the nurture of a sense of belonging and a connection with home in the Chinese student community.

The author picking up two boxes of “Health Packs” from the post office (April 17, 2020. Photography provided by the author)

A box packed with 24 “Health Packs” to distribute to Chinese students (April 17, 2020. Photography provided by the author)
Recent anti-Chinese rhetoric in the USA and around the world has put many Chinese citizens overseas in trepidation. Incidents of racism are on the rise, as President Donald Trump “continues to stoke xenophobia by using a racist name for the virus and associating it with Asian Americans” (Zhou 2020 , para 6). Now more than ever, Chinese students are questioning our identities and trying to find a sense of belonging, both physically and mentally. Physical isolations have also worsened the situation as the feelings of uncertainty and fear are internalized. Apart from providing material security, more importantly, “Health Packs” sent a signal of being cared for by others and were catalysts for commoning practices. In this case, each one of the volunteers and recipients was fulfilling his/her duty in connecting these worried and isolated individuals. Volunteering as a way of commoning demonstrates that, by carrying out small acts of care for others, we, regardless of ethnicity, religion, gender, or age, have the agency to overcome physical isolation and dismantle the difficulties posed by the crisis.
7 From a current me to a future we
As I put this paper together, the death toll of COVID-19 across the world has surpassed 650,000, Footnote 9 casting an even larger shadow of uncertainty over the future. The harder the crisis hits us, the more we have to look for the positive changes that it facilitates. The above-mentioned experiences and examples are personal and quotidian. However, what is personal and present allows us to imagine what is collective and future.
The three commoning examples that I have discussed are all manifestations of how care has connected us, which forms the premise for systematic changes. Because of care for the Earth, home gardeners and community farmers will contribute to building more sustainable food production and consumption systems. Because of care for our minds, online sharing will connect into global knowledge systems. Because of care for ourselves and each other, volunteering activities and mutual support will continue building more supportive, inclusive, and equitable social systems. We need to recognize that the scaling from individual commoning activities to larger neighborhood, local, and regional collaborative systems may require much more efforts, education, and time. Nonetheless, we can still continue fulfilling our own duties as connecting dots in the systems, weaving the collective networks.
The COVID-19 pandemic can be the most effective moment in which we disrupt unhealthy norms and validate new possibilities. Care-based commoning can be one of these possibilities. The emphasis on giving rather than taking, on solidarity rather than individuality, on care rather than indifference is what I would like to reflect on when engaging in and discussing everyday commoning experiences. Taking everyday commoning practices as the starting point, it is necessary to start imagining a new collaborative future that is no longer constrained by geospatial boundaries and physical contacts. In fact, since the beginning of the COVID-19 outbreak, care has been ubiquitous; we have all sensed it in the formats “of responsibility, of sharing, of reciprocity, of democratic organization, and of welfare” (Petrescu and Trogal 2017 , p. 194). As we remain physically apart, let us see this as an opportunity to practice our muscles of commoning and build the strength to care for ourselves and others.
Coverage on Wuhan lockdown can further be found on South China Morning Post ( https://www.scmp.com/news/china/society/article/3047278/wuhan-goes-shutdown-china-tries-contain-deadly-coronavirus ).
Larger numbers of confirmed cases are presented in darker colors in most COVID-19 live tracking maps, for instance, Baidu COVID-19 live data ( https://voice.baidu.com/act/newpneumonia/newpneumonia ) and Sina News COVID-19 live tracking ( https://news.sina.cn/zt_d/yiqing0121 ).
WeChat is the most widely used multi-purpose messaging, social media and mobile payment app in China.
The information of Pittsburgh’s first two COVID-19 cases is available on TribLIVE ( https://triblive.com/local/pittsburgh-allegheny/allegheny-county-to-announce-1st-coronavirus-cases/ ).
Student population percentage is calculated based on data provided by the US Census Bureau ( https://www.census.gov/quickfacts/pittsburghcitypennsylvania ).
The information is acquired from the study of coronavirus survival time on surfaces by US National Institutes of Health ( https://www.nih.gov/news-events/nih-research-matters/study-suggests-new-coronavirus-may-remain-surfaces-days ).
More information on the Distance Collaboration Commons in Support of Design for Social Change can be found on their Facebook page ( https://www.facebook.com/groups/880415052397554 ).
The time, guests and topics of Design Baithak can be found on the website ( https://sites.google.com/view/designbaithak/ ).
The COVID-19 death toll number is acquired from the Johns Hopkins Coronavirus Resource Center ( https://coronavirus.jhu.edu/map.html ).
Baibarac C, Petrescu D (2017) Open-source resilience: a connected commons-based proposition for urban transformation. Proc Eng 198:227–239. https://doi.org/10.1016/j.proeng.2017.07.157
Article Google Scholar
Bollier D (2014) Think like a commoner: a short introduction to the life of the commons. New Society Publishers, Gabriola Island, pp 9–20
Google Scholar
Bollier D (2020) Commoning as a pandemic survival strategy. Free, fair and alive: the insurgent power of the commons. https://www.freefairandalive.org/commoning-as-a-pandemic-survival-strategy/ . Accessed 2 April 2020
Bollier D, Helfrich S (eds) (2015) Patterns of commoning. Common Strategies Group, Amityville, New York, p 17
Corkery M, Karni A (2020) Trump administration restricts entry into U.S. from china. The New York Times. https://www.nytimes.com/2020/01/31/business/china-travel-coronavirus.html . Accessed 2 Jul 2020
Džokić A, Neelen M (2015) Instituting commoning. Footprint 9(1):21–34
Gibson-Graham JK, Cameron J, Healy S (2013) Take back the economy: an ethical guide for transforming our communities. University of Minnesota Press, London, pp 138–147
Book Google Scholar
Jian Y (2020) Urban home gardening takes root amid epidemic. Shanghai Daily. https://www.shine.cn/news/metro/2002262834/?fbclid=IwAR1cDp6qNN7-Sv5dPHdnl2P-Kpcb2jtlt3dhGlW8vQvs3386aWQIEgMBT24 . Accessed 26 Feb 2020
Jones T (2020) After coronavirus, the penny has dropped that wellbeing isn’t individual but social. The Guardian. https://www.theguardian.com/world/2020/apr/12/after-coronavirus-the-penny-has-dropped-that-wellbeing-isnt-individual-but-social . Accessed 2 May 2020
Morrow O, Parker B (2020) Care, commoning and collectivity: from grand domestic revolution to urban transformation. Urban Geogr. https://doi.org/10.1080/02723638.2020.1785258
Petrescu D, Trogal K (eds) (2017) The social (re)production of architecture: politics, values and actions in contemporary practice. Taylor and Francis Group, Routledge, pp 194–197
Sennett R (2012) Together: the rituals, pleasures and politics of cooperation. Yale University Press, New Haven, pp 9–13
Telford T, Kindy K (2020) Inside Smithfield, JBS and Tysons Food meat plants, fears grew of employees working sick, without protective gear. The Washington Post. https://www.washingtonpost.com/business/2020/04/25/meat-workers-safety-jbs-smithfield-tyson/ . Accessed 6 May 2020
Thackara J (2015) How to thrive in the next economy: designing tomorrow’s world today. Thames and Hudson, New York, pp 120–134
Troncoso S (2020) Commons: how the art of co-operation is the only way out of this crisis. Medium: The Commons Transition. https://medium.com/commons-transition/commons-how-the-art-of-co-operation-is-the-only-way-out-of-this-crisis-ab2c9ec96c08 . Accessed 27 July 2020
Wee S, Wang V (2020) China Grapples With Mystery Pneumonia-Like Illness. The New York Times. https://www.nytimes.com/2020/01/06/world/asia/china-SARS-pneumonialike.html . Accessed 8 May 2020
Zhou L (2020) How the coronavirus is surfacing America’s deep-seated anti-Asian biases. Vox. https://www.vox.com/identities/2020/4/21/21221007/anti-asian-racism-coronavirus . Accessed 5 May 2020
Download references
Author information
Authors and affiliations.
Carnegie Mellon University, Pittsburgh, PA, 15213, USA
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Chun Zheng .
Rights and permissions
Reprints and permissions
About this article
Zheng, C. Caring for the self and others: a reflection on everyday commoning amid the COVID-19 pandemic. Socio Ecol Pract Res 2 , 243–251 (2020). https://doi.org/10.1007/s42532-020-00062-3
Download citation
Received : 11 July 2020
Accepted : 13 August 2020
Published : 24 August 2020
Issue Date : September 2020
DOI : https://doi.org/10.1007/s42532-020-00062-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Everyday commoning
- Food supply chain
- Online sharing
- Healthy packs
Advertisement
- Find a journal
- Publish with us
- Track your research
COVID-19 reflections: the lessons learnt from the pandemic
by Alana Cullen , Lucy Lipscombe 03 February 2021
Imperial researchers reflect on the lessons they will take away from the pandemic.
Over the past 12 months the Imperial College London community has devoted an intense amount of time and research to COVID-19. Members of the community have been making fundamental scientific contributions to respond to coronavirus , from advising government policy to critical therapy research. A year on, Imperial researchers reflect on what lasting impact the pandemic has left on them.
Watch the clip above to hear the researchers’ insights.
A global contributor
Before I felt like just a person in the world, and now I feel like I’m one of those important people in the world! Dr Kai Hu
The first lesson is how fast- moving science is at this time. It is exciting to have been “on the forefront of vaccine discoveries” said Dr Anna Blakney, Assistant Professor at the University of British Columbia, formally a Research Fellow in Imperial’s Department of Infection and Immunity . Imperial has also been key in finding optimal treatments for COVID-19, with clinical academics such as Anthony Gordon , Professor of Anaesthesia and Critical Care and Intensive Care consultant, caring for critically ill patients in intensive care units as well as leading clinical trials. Findings from these trials include the effective use of an arthritis drug in reducing mortality in COVID-19 patients.
The science doesn’t stop there. Outside of the lab Imperial academics have been informing UK government policy. Since the emergence of coronavirus the team from the MRC Centre for Global Infectious Disease Analysis and Jameel Institute (J-IDEA) at Imperial have been predicting the course of the pandemic and informing policy. The team have also been supporting the COVID-19 response in New York State. Furthermore, Imperial academics including Professor Charles Bangham and Professor Wendy Barclay continue to advise the government as part of the Scientific Advisory Group for Emergencies (SAGE).
In total the Imperial community has contributed nearly 2,000 key workers to essential services and research, from biomedical engineers developing rapid COVID-19 tests to health economists, generating a wealth of knowledge about the science behind the pandemic.
“This is the first time where I feel like what I have learnt is very useful” said Dr Kai Hu, Research Associate in the Department of Infectious Disease. “Before I felt like just a person in the world, and now I feel like I’m one of those important people in the world.” Dr Kai Hu is part of Professor Robin Shattock’s COVID-19 vaccine team, who continue to develop an RNA vaccine .
Watch our full COVID reflections video below, including researchers sharing their hopes for the future.
Collaboration is key
Another key lesson learnt is how much stronger we are when we work together. Vaccine development, production and delivery have all been achieved in under 12 months – an unprecedented timeframe for any disease prevention tool. This goes to show that collaborative efforts with the right funding will go a long way in biomedical science. “I can work even harder than I thought I could work because we can come together as a team” says Dr Paul McKay , Senior Research Fellow in the Department of Infectious Disease. “Science is a competitive endeavour, but a collaborative endeavour too.”

Something that will leave a lasting impression is the kindness of community, family and friends. Kindness at this time has been “unparalleled” said Sonia Saxena , Professor of Primary Care and General Practitioner. From providing free meals to NHS workers to educational materials for homeschooling there has been a feeling of togetherness, even when apart, throughout these difficult times. Going forward, we can bring these lessons into science, bringing more collaboration and kindness into the everyday.
Article text (excluding photos or graphics) © Imperial College London.
Photos and graphics subject to third party copyright used with permission or © Imperial College London.
Alana Cullen Communications Division

Contact details
Email: [email protected] Show all stories by this author
Lucy Lipscombe Communications Division
Strategy-staff-community , Vaccines , Infectious-diseases , Viruses , JIDEA , Coronavirus , Staff-development , COVIDWEF , Public-health See more tags
Leave a comment
Your comment may be published, displaying your name as you provide it, unless you request otherwise. Your contact details will never be published.
Latest news

News in brief
Tracking global ocean change and using nuclear energy: news from imperial , virtuous circle, prestigious annual dinner celebrates the impact of philanthropy, new graduate centre, £10 million gift to propel imperial’s heart and lung research, most popular.

1 Global recognition:
Imperial ranks second in the world in major university ranking, 2 infection study:, covid-19 – how long am i infectious and when can i safely leave isolation, 3 bowel disease:, major cause of inflammatory bowel disease discovered, 4 psychedelic treatment:, magic mushroom compound increases brain connectivity in people with depression, latest comments, comment on iron deficiency may increase stroke risk through sticky blood: i had a stroke that resulted in paralysis of my left side including my left eye and drooping of my f…, comment on scientists find a salty way to kill mrsa: i am lokeshkumar and am postgraduate student from india and my major is bio-chemistry. it is a nice…, comment on imperial ranks second in the world in major university ranking: heartiest congratulations to the entire imperial college "family". it is indeed a true privilege to …, latest tweets.
Read these 12 moving essays about life during coronavirus
Artists, novelists, critics, and essayists are writing the first draft of history.
by Alissa Wilkinson

The world is grappling with an invisible, deadly enemy, trying to understand how to live with the threat posed by a virus . For some writers, the only way forward is to put pen to paper, trying to conceptualize and document what it feels like to continue living as countries are under lockdown and regular life seems to have ground to a halt.
So as the coronavirus pandemic has stretched around the world, it’s sparked a crop of diary entries and essays that describe how life has changed. Novelists, critics, artists, and journalists have put words to the feelings many are experiencing. The result is a first draft of how we’ll someday remember this time, filled with uncertainty and pain and fear as well as small moments of hope and humanity.
- The Vox guide to navigating the coronavirus crisis
At the New York Review of Books, Ali Bhutto writes that in Karachi, Pakistan, the government-imposed curfew due to the virus is “eerily reminiscent of past military clampdowns”:
Beneath the quiet calm lies a sense that society has been unhinged and that the usual rules no longer apply. Small groups of pedestrians look on from the shadows, like an audience watching a spectacle slowly unfolding. People pause on street corners and in the shade of trees, under the watchful gaze of the paramilitary forces and the police.
His essay concludes with the sobering note that “in the minds of many, Covid-19 is just another life-threatening hazard in a city that stumbles from one crisis to another.”
Writing from Chattanooga, novelist Jamie Quatro documents the mixed ways her neighbors have been responding to the threat, and the frustration of conflicting direction, or no direction at all, from local, state, and federal leaders:
Whiplash, trying to keep up with who’s ordering what. We’re already experiencing enough chaos without this back-and-forth. Why didn’t the federal government issue a nationwide shelter-in-place at the get-go, the way other countries did? What happens when one state’s shelter-in-place ends, while others continue? Do states still under quarantine close their borders? We are still one nation, not fifty individual countries. Right?
- A syllabus for the end of the world
Award-winning photojournalist Alessio Mamo, quarantined with his partner Marta in Sicily after she tested positive for the virus, accompanies his photographs in the Guardian of their confinement with a reflection on being confined :
The doctors asked me to take a second test, but again I tested negative. Perhaps I’m immune? The days dragged on in my apartment, in black and white, like my photos. Sometimes we tried to smile, imagining that I was asymptomatic, because I was the virus. Our smiles seemed to bring good news. My mother left hospital, but I won’t be able to see her for weeks. Marta started breathing well again, and so did I. I would have liked to photograph my country in the midst of this emergency, the battles that the doctors wage on the frontline, the hospitals pushed to their limits, Italy on its knees fighting an invisible enemy. That enemy, a day in March, knocked on my door instead.
In the New York Times Magazine, deputy editor Jessica Lustig writes with devastating clarity about her family’s life in Brooklyn while her husband battled the virus, weeks before most people began taking the threat seriously:
At the door of the clinic, we stand looking out at two older women chatting outside the doorway, oblivious. Do I wave them away? Call out that they should get far away, go home, wash their hands, stay inside? Instead we just stand there, awkwardly, until they move on. Only then do we step outside to begin the long three-block walk home. I point out the early magnolia, the forsythia. T says he is cold. The untrimmed hairs on his neck, under his beard, are white. The few people walking past us on the sidewalk don’t know that we are visitors from the future. A vision, a premonition, a walking visitation. This will be them: Either T, in the mask, or — if they’re lucky — me, tending to him.
Essayist Leslie Jamison writes in the New York Review of Books about being shut away alone in her New York City apartment with her 2-year-old daughter since she became sick:
The virus. Its sinewy, intimate name. What does it feel like in my body today? Shivering under blankets. A hot itch behind the eyes. Three sweatshirts in the middle of the day. My daughter trying to pull another blanket over my body with her tiny arms. An ache in the muscles that somehow makes it hard to lie still. This loss of taste has become a kind of sensory quarantine. It’s as if the quarantine keeps inching closer and closer to my insides. First I lost the touch of other bodies; then I lost the air; now I’ve lost the taste of bananas. Nothing about any of these losses is particularly unique. I’ve made a schedule so I won’t go insane with the toddler. Five days ago, I wrote Walk/Adventure! on it, next to a cut-out illustration of a tiger—as if we’d see tigers on our walks. It was good to keep possibility alive.
At Literary Hub, novelist Heidi Pitlor writes about the elastic nature of time during her family’s quarantine in Massachusetts:
During a shutdown, the things that mark our days—commuting to work, sending our kids to school, having a drink with friends—vanish and time takes on a flat, seamless quality. Without some self-imposed structure, it’s easy to feel a little untethered. A friend recently posted on Facebook: “For those who have lost track, today is Blursday the fortyteenth of Maprilay.” ... Giving shape to time is especially important now, when the future is so shapeless. We do not know whether the virus will continue to rage for weeks or months or, lord help us, on and off for years. We do not know when we will feel safe again. And so many of us, minus those who are gifted at compartmentalization or denial, remain largely captive to fear. We may stay this way if we do not create at least the illusion of movement in our lives, our long days spent with ourselves or partners or families.
- What day is it today?
Novelist Lauren Groff writes at the New York Review of Books about trying to escape the prison of her fears while sequestered at home in Gainesville, Florida:
Some people have imaginations sparked only by what they can see; I blame this blinkered empiricism for the parks overwhelmed with people, the bars, until a few nights ago, thickly thronged. My imagination is the opposite. I fear everything invisible to me. From the enclosure of my house, I am afraid of the suffering that isn’t present before me, the people running out of money and food or drowning in the fluid in their lungs, the deaths of health-care workers now growing ill while performing their duties. I fear the federal government, which the right wing has so—intentionally—weakened that not only is it insufficient to help its people, it is actively standing in help’s way. I fear we won’t sufficiently punish the right. I fear leaving the house and spreading the disease. I fear what this time of fear is doing to my children, their imaginations, and their souls.
At ArtForum , Berlin-based critic and writer Kristian Vistrup Madsen reflects on martinis, melancholia, and Finnish artist Jaakko Pallasvuo’s 2018 graphic novel Retreat , in which three young people exile themselves in the woods:
In melancholia, the shape of what is ending, and its temporality, is sprawling and incomprehensible. The ambivalence makes it hard to bear. The world of Retreat is rendered in lush pink and purple watercolors, which dissolve into wild and messy abstractions. In apocalypse, the divisions established in genesis bleed back out. My own Corona-retreat is similarly soft, color-field like, each day a blurred succession of quarantinis, YouTube–yoga, and televized press conferences. As restrictions mount, so does abstraction. For now, I’m still rooting for love to save the world.
At the Paris Review , Matt Levin writes about reading Virginia Woolf’s novel The Waves during quarantine:
A retreat, a quarantine, a sickness—they simultaneously distort and clarify, curtail and expand. It is an ideal state in which to read literature with a reputation for difficulty and inaccessibility, those hermetic books shorn of the handholds of conventional plot or characterization or description. A novel like Virginia Woolf’s The Waves is perfect for the state of interiority induced by quarantine—a story of three men and three women, meeting after the death of a mutual friend, told entirely in the overlapping internal monologues of the six, interspersed only with sections of pure, achingly beautiful descriptions of the natural world, a day’s procession and recession of light and waves. The novel is, in my mind’s eye, a perfectly spherical object. It is translucent and shimmering and infinitely fragile, prone to shatter at the slightest disturbance. It is not a book that can be read in snatches on the subway—it demands total absorption. Though it revels in a stark emotional nakedness, the book remains aloof, remote in its own deep self-absorption.
- Vox is starting a book club. Come read with us!
In an essay for the Financial Times, novelist Arundhati Roy writes with anger about Indian Prime Minister Narendra Modi’s anemic response to the threat, but also offers a glimmer of hope for the future:
Historically, pandemics have forced humans to break with the past and imagine their world anew. This one is no different. It is a portal, a gateway between one world and the next. We can choose to walk through it, dragging the carcasses of our prejudice and hatred, our avarice, our data banks and dead ideas, our dead rivers and smoky skies behind us. Or we can walk through lightly, with little luggage, ready to imagine another world. And ready to fight for it.
From Boston, Nora Caplan-Bricker writes in The Point about the strange contraction of space under quarantine, in which a friend in Beirut is as close as the one around the corner in the same city:
It’s a nice illusion—nice to feel like we’re in it together, even if my real world has shrunk to one person, my husband, who sits with his laptop in the other room. It’s nice in the same way as reading those essays that reframe social distancing as solidarity. “We must begin to see the negative space as clearly as the positive, to know what we don’t do is also brilliant and full of love,” the poet Anne Boyer wrote on March 10th, the day that Massachusetts declared a state of emergency. If you squint, you could almost make sense of this quarantine as an effort to flatten, along with the curve, the distinctions we make between our bonds with others. Right now, I care for my neighbor in the same way I demonstrate love for my mother: in all instances, I stay away. And in moments this month, I have loved strangers with an intensity that is new to me. On March 14th, the Saturday night after the end of life as we knew it, I went out with my dog and found the street silent: no lines for restaurants, no children on bicycles, no couples strolling with little cups of ice cream. It had taken the combined will of thousands of people to deliver such a sudden and complete emptiness. I felt so grateful, and so bereft.
And on his own website, musician and artist David Byrne writes about rediscovering the value of working for collective good , saying that “what is happening now is an opportunity to learn how to change our behavior”:
In emergencies, citizens can suddenly cooperate and collaborate. Change can happen. We’re going to need to work together as the effects of climate change ramp up. In order for capitalism to survive in any form, we will have to be a little more socialist. Here is an opportunity for us to see things differently — to see that we really are all connected — and adjust our behavior accordingly. Are we willing to do this? Is this moment an opportunity to see how truly interdependent we all are? To live in a world that is different and better than the one we live in now? We might be too far down the road to test every asymptomatic person, but a change in our mindsets, in how we view our neighbors, could lay the groundwork for the collective action we’ll need to deal with other global crises. The time to see how connected we all are is now.
The portrait these writers paint of a world under quarantine is multifaceted. Our worlds have contracted to the confines of our homes, and yet in some ways we’re more connected than ever to one another. We feel fear and boredom, anger and gratitude, frustration and strange peace. Uncertainty drives us to find metaphors and images that will let us wrap our minds around what is happening.
Yet there’s no single “what” that is happening. Everyone is contending with the pandemic and its effects from different places and in different ways. Reading others’ experiences — even the most frightening ones — can help alleviate the loneliness and dread, a little, and remind us that what we’re going through is both unique and shared by all.
Most Popular
The hottest place on earth is cracking from the stress of extreme heat, india just showed the world how to fight an authoritarian on the rise, the backlash against children’s youtuber ms rachel, explained, trump’s felony conviction has hurt him in the polls, cities know how to improve traffic. they keep making the same colossal mistake., today, explained.
Understand the world with a daily explainer plus the most compelling stories of the day.
More in Culture

Baby Reindeer’s “Martha” is, inevitably, suing Netflix

Kate Middleton’s cancer diagnosis, explained

Why are we so obsessed with morning routines?

Here are all 50+ sexual misconduct allegations against Kevin Spacey

Is TikTok breaking young voters’ brains?

This is your kid on smartphones Audio

World leaders neglected this crisis. Now genocide looms.

Why China is winning the EV war Video

The messy discussion around Caitlin Clark, Chennedy Carter, and the WNBA, explained
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Wiley - PMC COVID-19 Collection

A reflection on health and disease amid COVID‐19 pandemic
Si‐woon park.
1 Department of Rehabilitation Medicine, International St. Mary's Hospital, Catholic Kwandong University, Incheon South Korea
Associated Data
Data sharing not applicable to this article as no datasets were generated or analysed during the current study.
Coronavirus disease 2019 pandemic is persisting for more than a year and it's still far from being controlled. It is making a big impact not only on physical illness but also on mental and social aspects. In this situation, we need to reflect on current medical society's view of disease and health. The dominant paradigm in contemporary medicine is the reductionist view of disease and the biomedical model of health. As a result, the healthcare system seems to be more focused on virus eradication than on patient care. We need to look back on this position in view of humanities and ethics and broaden our perspective to an ecological view of disease and the sociomedical model of health. The quarantine and health care policy also needs to be re‐built with more focus on patient care.
1. INTRODUCTION
It's been a year and a half since coronavirus disease 2019 (COVID‐19) pandemic began. This new infectious disease, which had spread at a frightening rate in the early days, became a testing tool for each country's quarantine policy. Unlike the past epidemics, new policies—mass testing, tracing, and isolation—emerged owing to the advancement of information and technology. Some countries have been relatively successful in controlling the number of confirmed cases. However, we are still incompetent in preventing the spread of infectious diseases and confronting many socioeconomic problems over time. The vaccines developed with the greatest hope, although they showed quite good preventive efficacy, are still limited in preventing all the variants of the virus. We are still far from controlling the pandemic.
The current situation leads us to look back on what it means to live a healthy life, and what the healthcare system is for. In this article, I intended to take a look at the problems that emerged during the COVID‐19 pandemic and discuss the meaning of disease, health, and health care in terms of medical epistemology and ethics.
2. WHAT IS A DISEASE?
At the beginning of the COVID‐19 pandemic, the South Korean Government recommended screening polymerase chain reaction tests only for those who travelled abroad in certain areas and had a fever and respiratory symptoms. In South Korea, the relationship between the government and the medical association was not so cooperative because the government was planning healthcare policies that the medical association disagreed with. In the meantime, a doctor sent a suspected case to the public health centre for the COVID‐19 test. But the public health centre official refused testing because the case did not meet the indications for the test. 1 Later, the case was confirmed as positive, and the medical association criticized the bureaucracy of the government for its lack of medical expertise. The public and the opposition party also joined the criticism. And the government, being conscious of the people's vote, greatly expanded the indications for the test. Infection control became a political issue. As a result, the subjects to the test included asymptomatic individuals, and anybody who wanted to be tested could get it. The public's excessive fear of the virus also played a role in expanding test indications. Besides, the advanced IT situation in Korea made it technically possible. As the South Korean government's quarantine seemed to go relatively successful in limiting the number of confirmed cases, other countries began to implement similar methods of quarantine as South Korea did. The US Government at that time also faced criticism for having fewer COVID‐19 tests than South Korea, and more aggressive testing was launched to find out more confirmed cases.
As a result of this mass testing policy that has never been done before, the number of COVID‐19 confirmed cases increased drastically. On the contrary, the case fatality rate of COVID‐19 showed a tendency to decrease. The case fatality rate of COVID‐19 was reported to be lower than that of severe acute respiratory syndrome (SARS) or Middle East respiratory syndrome (MERS). 1 , 2 But if the screening test had been restricted to symptomatic cases, the case fatality rate may be higher than reported. The positive effect of this mass testing policy is that it can provide better knowledge regarding the infectivity of the virus. This information is important for establishing effective quarantine policies. However, there are also negative effects. First, the increase in the number of confirmed cases is being reported in the media every day and spreads public fear of the disease. Second, medical resources can be depleted as asymptomatic cases are also included in the management. As a result, patients with symptoms are at risk of being excluded from medical treatment.
An infectious disease develops from the interaction between agent, host, and environment, which is known as the epidemiological triad. Social distancing to suppress the spread of infectious diseases is the right measure in terms of controlling the environment of easy transmission. On the contrary, putting an infected host in an isolated environment with other patients is like leaving the host in a more risky, immune‐deteriorating environment. Even though the host had no symptoms in the first place, later he or she might develop symptoms while being isolated in a poor environment, and the disease could get worse.
Here comes a fundamental question about a disease. Is a test‐positive case without symptoms a patient? Can we say that those who are test positive are having a disease?
According to Encyclopedia Britannica, “disease” is defined as “any harmful deviation from the normal structural or functional state of an organism, generally associated with certain signs and symptoms and differing in nature from physical injury.” As seen in this definition, a disease is generally a phenomenon that involves symptoms and signs. In fact, the disease begins with symptoms that the patient complains of, and then the diagnostic process follows. And the goal of treatment is a relief of symptoms.
Since ancient times, a disease had been defined according to symptoms that the patient complains of. Medical theories arise in the process of explaining and treating symptoms. In ancient Greek medicine, represented by Hippocrates, the disease was seen as a disharmony resulted from fluid dysregulation, 3 and health care was provided based on the holistic care model. 4 In oriental medicine, the symptom was the basic unit and key term in medical theory. 5 The human body was seen as a microcosmos and harmony was emphasized for healing. After the modern era, the invention of microscopes and the discovery of microorganisms have introduced the pathology of diseases. Disease entities have begun to be defined according to pathologic findings. Descartes regarded the world as a giant clockwork machine and thought that one would have to disassemble it and look at the parts to understand it. This mechanistic view was applied to an understanding of the human body, and the reductionist view became the dominant paradigm in medicine. 6
Reductionism in medicine affected the diagnosis, treatment, and preventive approach of disease. The reductionist view is to diagnose a disease based on pathology, assume that the pathologic finding has a causal relationship with the symptoms, seek for a treatment to get rid of pathologic findings, and establish prevention strategies focused on eradicating observable pathology. Consequently, it became ambiguous whether the purpose of health care is an improvement of patient's condition or restoration of pathology. In the same way, it is believed that the detection of pathogens is more essential in the diagnosis of infectious disease than a clinical presentation of patients. Furthermore, by seeing infectious disease as evolutionary warfare between mankind and microorganism, strategies to eradicate microorganisms are considered to be more important than patient care.
The reductionist view, of course, has contributed a lot to the advancement of medicine, but because of its limitations, system theory has attracted attention as an alternative. 7 In contrast to the microscopic view of reductionism, system theory understands the world as a system and provides a macroscopic ecological perspective. The ecological perspective considers disease as disharmony in the entire system and attempts a multidimensional approach in diagnosis, treatment, and prevention of disease (Table 1 ).
Reductionist versus ecological view of infectious disease
| Reductionist view | Ecological view | |
|---|---|---|
| Relationship between agent and host | Conflict | Harmony |
| Diagnosis | Isolation of microorganism | Host response to microorganism |
| Treatment | Removal of microorganism | Focus on interaction between host, agent, and environment |
| Prevention | Eradication of microorganism |
In fact, COVID‐19 was initiated by the destruction of ecological balance. Global instability can lead to an increase in new epidemics. Therefore, to properly cope with emerging infectious diseases, we need to integrate knowledge from multiple disciplines and approach problems from a system perspective and ecological context. 8 The microscopic approach of molecular biology is important for understanding the origin and pathology of pathogens. Whereas, understanding the ecology of infectious diseases and agent–host interactions provides key knowledge in regard to transmission and manifestations of diseases, and thus help establish successful disease control strategies. 9 Recognizing that human health and global bio‐system are inextricably linked, efforts should be made to understand infectious diseases and provide solutions from a more ecological perspective. 10 Concentrated too much on reductionist view, we may lose the balanced view. We may fall into the fallacy of thinking newly emerging infectious diseases as problems to be solved solely by biological means rather than seeking more sustainable solutions for coexistence.
A disease entity is neither born nor discovered but defined. Pathologic finding per se is not a disease. Defining disease entities not only affects an individual's health status, but also affects the whole society in both ethical and economic aspects. 11 Now in this pandemic, we are experiencing the influence of disease control strategy, which is based on the reductionist view, on the whole society. It does not seem appropriate to set the number of confirmed cases as the goal of infection control without defining the disease entity. We should first define the disease entity we fight against and clarify who needs medical care.
3. WHAT IS HEALTH?
WHO defined health as “a state of complete physical, mental and social well‐being and not merely the absence of disease or infirmity.” This WHO definition has been criticized for the word “complete,” which is usually unachievable, and its disease‐centeredness. As an alternative, the definition of health as “the ability to adapt and self‐manage” has been proposed. 12 It makes more sense to define health as “a dynamic state of wellbeing characterized by a physical, mental and social potential, which satisfies the demands of a life commensurate with age, culture, and personal responsibility.” 13
Aside from the definition of health, WHO published and distributed “International Classification of Functioning, Disability and Health (ICF).” 14 ICF takes a more comprehensive approach to health. ICF sees health state in a functional point of view, defines domains of health as body structure, body function, activity, and participation, and identifies personal and environmental factors as modifiers. According to the holistic and social perspective of ICF, health is not just a matter of presence or absence of disease but encompasses the way how we live. This perspective enables us to seek ways of minimizing the negative impact of disease and impairment on activity and participation.
The dominant paradigm of current medical society is the biomedical model. The biomedical model sees health as a disease‐free or pathogen‐free state. Its perspective is restricted to body organ or body system level and focuses only on body structure and function. It often neglects social and system factors that affect health status and sees health problems only at the biological level of an individual. 11 To complement the limitations of the biomedical model, a sociologic perspective is required. In the sociomedical model, one can be said to be healthy if he or she can adapt to life situations even with the disease. The sociomedical model extends the concept of health to the level of whole person and society, and focuses on activity and participation (Table 2 ).
Biomedical versus sociomedical model of health
| Biomedical model | Sociomedical model |
|---|---|
| Absence of disease | Health in disease |
| Absence of pathogen | Adaptation to life situation |
| Body organ or body system level | Whole person or society level |
| Focus on body structure and function | Focus on activity and participation |
Absurdly, as the pandemic persists, the quarantine policies limit activities and restrict the participation of individuals in everyday life, even when the virus itself that caused the pandemic does not cause serious symptoms or harm human body. From the health perspective of ICF, healthy lives are being threatened by activity limitations and participation restrictions in the absence of disease or impairment.
As new epidemics such as SARS and MERS emerged since the beginning of the 21st century, principles of quarantine ethics have been established. Upshur 15 suggested the following four principles: harm, proportionality, reciprocity, and transparency. Aside from these ethical principles, we need to ensure whether quarantine policies are effective. For proportionality, we need to estimate whether the potential benefits of quarantine surpass the negative effects resulted from it. Benefits of isolating asymptomatic or mild cases should be weighed against side effects such as stigma. Besides, we should also keep in mind that a high‐intensity quarantine policy can enhance public fear and anxiety, induce stigmatization, and provoke competition for limited resources. It may result in deepened economic polarization and a divided society. 16 Policymakers tend to take position of people who are not infected yet. To protect uninfected, they isolate and confine infected ones. Such a quarantine policy is not different from oppressing the minority for the benefit of the majority. Infectious disease usually affects more in poor people and poor countries. Policymakers should not ignore the principle of justice when making quarantine policy. 17
In South Korea, confirmed cases with no or mild symptoms are forced to be isolated in designated treatment centres. In March 2021, the media reported a case who committed suicide while being isolated in a designated centre. 2 According to press reports, the woman had been accused for violating self‐isolation after receiving test negative result a few weeks ago. She contacted an infected one again and took her second test to get positive result, so she was sent to a designated treatment centre for isolation. The police assumed that she was suffering from being isolated alone in a room. The coronavirus did not cause serious physical symptoms to this woman, but isolation under the quarantine policy caused very serious negative consequence.
This tragic incident was reported in the media and called public attention, but in fact, there are many other unknown cases that are experiencing mental illness during COVID‐19 pandemic. It is important to ensure that involuntary hospitalization be administered in an appropriate and respectful manner to protect the interests of both patients and the community. Special attention must be paid to prevent abuse of forced isolation just to alleviate public anxiety. 18
Media also reported cases who are suffering from social disadvantage after overcoming COVID‐19. Many people suffered from the stigma of having been a COVID‐19 patient even after they got test negative. They had to feel uncomfortable when meeting other people in community or in the workplace. They often were pressured to resign from the company they had been working for, and some of them were actually fired. 3 This irrationality comes from excessive public fear of the virus on the one hand. On the other hand, it also comes from the company's worries about the disadvantages they may get because of the quarantine policies. Though these patients defeated the virus and overcame the disease, they got participation restriction because of social prejudice and overly restrictive quarantine policies.
Even if it is not directly caused by infectious disease, economic depression and unemployment affect the whole society and hinder people's healthy lives. There has been a report that, among OECD countries, decline in employment during COVID‐19 pandemic period is large in South Korea, which implemented stronger quarantine policies than other countries. 4 Mass unemployment causes much greater social loss than the virus itself does. Mental distress a person may experience because of unemployment may cause more harm to health status than the virus itself does. We should not overlook this and make a misjudgment by looking only at gross economic indicators. 19 Just like exaggerated immune response against virus harms our own body, an overreaction of society against disease may harm our society's economic structure.
4. WHAT IS HEALTH CARE FOR?
In March 2020, early of the COVID‐19 pandemic, a tragic death occurred in Daegu, where the first outbreak occurred in South Korea. A healthy adolescent man died of pneumonia. According to media reports, 5 this high school student visited the hospital with symptoms of pneumonia and high fever, but was denied hospitalization as he was classified as a suspected COVID‐19 patient. Days ago, he had had to line up for about an hour on a rainy chilly day to buy facial masks which were in short supply at that time, even though he already had mild respiratory symptoms. After then he visited the hospital with a high fever, but could not receive proper treatment other than intravenous fluid supply in his parents' car. Later, in hindsight, he was hospitalized and treatment began, but this young man could not survive. This tragedy happened because suspected COVID‐19 patients were not allowed either to come to general hospitals or to be transferred to the designated COVID‐19 hospitals until confirmed. There was a loophole in health care caused by quarantine policy. The father of the young man moaned and said, “The result of complying with the COVID‐19 manual led to an unfair death of a young man.”
This case raises an important ethical question in pandemic situation. Is it ethically justifiable to ban infected people who need medical care from coming to hospitals under the cause of protecting the public? Under this policy, hospitals would avoid patients with respiratory symptoms. Even though they are not confirmed as positive, patients with respiratory symptoms cannot come to hospitals. Even when they manage to come to an emergency room, they will be isolated without receiving proper treatment. During the isolation, their symptoms may worsen or they may get a new infection. Healthcare policy is for all people including those who do not yet have the disease. Nevertheless, in essence, health care is primarily about taking care of sick people. Suppression of infectious disease cannot justify neglect of patients in medical need.
Pandemic situation caused many moral questions, and there has been debates in views of deontologist versus consequentialist. 20 Consequentialist may argue that rejection of treatment for the suspected cases is justified because if the suspected cases come to the hospital and spread the infection, it will have worse consequences at the public health level. Deontologist may argue that the reason why hospitals exist is to care for patients and it is the righteous duty of hospitals to treat patients while thoroughly complying with the quarantine policy, and that refusing patient care cannot be justified in any occasion. It is necessary to estimate consequences in terms of public health benefits, but in real world, accurate prediction of the consequences is usually impossible. If we justify refusal of care, it will be inevitable that early patients be killed for the cause of public health whenever a new epidemic emerges.
This case raises another ethical question in terms of redistribution of healthcare resources. Is it appropriate to set up facilities for forcible isolation of cases with mild or no symptoms in the shortage of hospital beds designated for COVID‐19 patients? This question also applies to the current quarantine policy that sets the number of test‐positive cases as the target indicator of infection control. Increasing test numbers and thus increasing the detection rate regardless of symptoms may be effective in counting the number of test‐positive cases, but medical resources can be run out early. More attention should be paid to ensure patient care and use limited medical resources efficiently. 21 The purpose of health care is not virus eradication but patient care. Even though we do not have the exact antiviral agent acting on coronavirus, we still can take care of patients and save lives.
The main purpose of quarantine in the early phase of pandemic was to reduce deaths from COVID‐19. Although the mortality of COVID‐19 was not higher than other previous epidemics, its high infectivity made it a priority to implement a policy to stop its spread. Lockdown in the early pandemic seems to have had a direct effect in reducing the number of confirmed cases. In countries where the number of confirmed cases increased because of the failure of the initial blockade, the number of deaths increased. However, the death toll of COVID‐19 is not solely explained by the number of confirmed cases. In a study that investigated mortality rates among countries, the difference between countries was explained by other factors such as the proportion of people over the age of 80, population density, the proportion of urban population, gross domestic product, number of hospital beds per population, average temperature in March, and incidence of tuberculosis. In some countries, more important factor than lockdown to reduce the number of deaths was medical resources, that is, the number of hospital beds. In particular, countries with high population density and a high proportion of older people over the age of 80 should focus on the increase in hospital beds. 22
These findings suggest that the healthcare system factor matters a lot in reducing COVID‐19 related mortality. According to a study that investigated clinical manifestations of COVID‐19, the progression rate from pneumonia to acute respiratory distress syndrome was significantly different among countries. It ranged from 3% to 63%. To reduce this rate, proper allocation of medical resources is critical. 23 Leaving patients untreated leads to high mortality. 24 Quarantine alone cannot guarantee a reduction in the number of deaths. In countries where healthcare is not warranted and medical costs are to be borne on their own, the mortality would be higher because of those who could not access health care. 25 Inequality is more pronounced in pandemic situation. Infectious disease affects more poor, neglected people, and minorities. 26
Apart from deaths directly caused by COVID‐19, medical care for other diseases is also at risk. One way to estimate the death toll during the COVID‐19 pandemic is to calculate the number of deaths in excess compared to the usual year. Last year's excess death statistics suggest a significant increase in deaths not only from COVID‐19 but also from other causes. 27 The number of excess deaths vary by country. In the United States, where the number of COVID‐19 confirmed and death cases were high, the rate of all‐cause excess mortality compared with mortality directly caused by COVID‐19 was 135%. On the contrary, in South Korea, where enhanced quarantine measures have been relatively successful in reducing the number of confirmed and death cases, this rate was 488%. This means that the success of the quarantine was accompanied by the sacrifice of other patients. 28 The reason for this may be that patients who needed medical care were hesitant to visit the hospital because of the fear of COVID‐19. Or it may be due to the shortage of medical resources caused by the pandemic. It was reported that diseases such as diabetes 29 or cancer, 30 which require long‐term management, are likely to be affected by the pandemic. From long term perspective, while it is important to minimize deaths from COVID‐19, it is also important to reduce all‐cause mortality and maintain health services for other diseases. 31
We need to reassure people that they will be well treated and recovered even if they are infected with COVID‐19. We should not leave people to be overwhelmed by fear and anxiety that they will suffer great physical and social harm induced by this pandemic.
5. CONCLUSION
COVID‐19 pandemic is not only a matter of biological science but also a human problem. It is not an isolated problem, but deeply connected with the human condition and society. To re‐establish sustainable community health amid this pandemic, humanistic reflection is required. 32 Current response to COVID‐19 pandemic arouses suspicion that the medical society is deeply immersed in the reductionist and biomedical view of disease and health. The ecological and sociomedical perspective is required to respond to this pandemic in more balanced manner.
Ethical reconsideration is also necessary for terms of the proportionality of the quarantine effects and the distribution of medical resources. It is advisable to stop testing people who do not present any symptoms or signs and try every effort to keep confirmed cases from stigmatization. It is not advisable to forbid suspected cases as well as patients with other diseases from coming to hospitals.
Policymakers need to make proper decisions about reestablishing COVID‐19 control strategy and rearranging healthcare resources with focus on patient care. Otherwise, more people will get more suffering not only from direct effects of the virus but also from social and economic complications induced by quarantine policy.
CONFLICTS OF INTEREST
The author declares no conflicts of interest.
AUTHOR CONTRIBUTION
Si‐Woon Park is the only author of this study.
ACKNOWLEDGMENT
No funding was received to assist with the preparation of this manuscript.
Park S‐W. A reflection on health and disease amid COVID‐19 pandemic . J Eval Clin Pract . 2022;1‐6. 10.1111/jep.13673 [ PMC free article ] [ PubMed ] [ CrossRef ]
1 The media articles cited in this paper were reported in Korean newspapers, and the websites of the articles are provided in footnotes. For this story, please see the following website: https://www.chosun.com/site/data/html_dir/2020/02/05/2020020503536.html .
2 This case story was reported in the Korean newspaper, https://insight.co.kr/news/32867 .
3 There have been a lot of newspaper articles reporting social disadvantages experienced by COVID‐19 confirmed cases. Some of those stories were reported on the following website: http://news.tvchosun.com/mobile/svc/osmo_news_detail.html?contid=2021011990116#none .
4 A Korean economics professor gave a presentation regarding this issue at a conference, and it was reported in a Korean newspaper: https://m.hani.co.kr/arti/society/labor/981317.html .
5 This case story was reported in many newspapers in South Korea. One of the reports is the following website: https://nocutnews.co.kr/news/5298772 . The article was written in Korean language and translated by the author in this manuscript.
DATA AVAILABILITY STATEMENT

Paragraph Writing on Covid 19
Ai generator.
COVID-19, caused by the coronavirus, significantly impacted global health and daily life. Action plans focused on prevention, treatment, and vaccination. Some sought religious exemptions from mandates. A health thesis statement might explore the pandemic’s effects on mental health. The tone is informative and serious. This paragraph highlights the comprehensive response to COVID-19.
Checkout → Free Paragraph Writer Tool
Short Paragraph on Covid-19
Covid-19 is a global pandemic caused by the novel coronavirus. It has significantly impacted daily life, with governments worldwide implementing lockdowns, social distancing, and mask mandates to curb the virus’s spread. The pandemic has highlighted the importance of healthcare systems and the need for vaccines. It has also emphasized global cooperation and resilience in facing unprecedented challenges.
Medium Paragraph on Covid-19
Covid-19, caused by the novel coronavirus, has had a profound impact on the world since its outbreak. The pandemic led to widespread lockdowns, social distancing measures, and mandatory mask-wearing to prevent the virus’s spread. Healthcare systems were overwhelmed, emphasizing the need for robust medical infrastructure and preparedness. The development and distribution of vaccines became a global priority, showcasing the importance of scientific research and international cooperation. Economies faced significant challenges, with businesses closing and unemployment rates rising. Despite these hardships, the pandemic also brought communities together, highlighting resilience, adaptability, and the critical role of healthcare workers in combating the crisis.
Long Paragraph on Covid-19
Covid-19, caused by the novel coronavirus SARS-CoV-2, emerged in late 2019 and rapidly spread across the globe, leading to an unprecedented pandemic. The virus’s high transmission rate prompted governments worldwide to implement stringent measures such as lockdowns, social distancing, and mask mandates to control its spread. These measures, while necessary, significantly disrupted daily life, impacting economies, education, and social interactions. Healthcare systems were strained, underscoring the need for better preparedness and robust medical infrastructure. The rapid development and global distribution of vaccines became a beacon of hope, demonstrating the power of scientific collaboration and innovation. The pandemic also highlighted the disparities in healthcare access and the importance of public health initiatives. Despite the immense challenges, communities showed resilience and adaptability, finding new ways to connect and support each other. The dedication of healthcare workers and the collective effort to combat the virus underscored the importance of global solidarity. Covid-19 has reshaped our world, teaching valuable lessons about preparedness, the significance of science, and the strength of human resilience in the face of adversity.
Tone-wise Paragraph Examples on Covid-19
Formal tone.
Covid-19, caused by the novel coronavirus SARS-CoV-2, represents an unprecedented global health crisis. The pandemic has led to widespread implementation of public health measures such as lockdowns, social distancing, and mandatory mask usage to mitigate the virus’s transmission. Healthcare systems worldwide faced significant strain, highlighting the critical need for robust medical infrastructure and emergency preparedness. The rapid development and distribution of vaccines have been pivotal in controlling the spread of the virus, underscoring the importance of scientific research and international cooperation. The pandemic has also revealed existing disparities in healthcare access and emphasized the necessity of coordinated global public health strategies to effectively manage such crises.
Informal Tone
Covid-19 has really shaken things up since it started spreading in late 2019. Caused by a new coronavirus, it led to lockdowns, social distancing, and everyone wearing masks. Daily life changed a lot, with schools and businesses shutting down, and everyone trying to stay safe. The healthcare system was hit hard, showing us just how important it is to be prepared. Vaccines were developed super quickly, giving us hope to get back to normal. Even though it was tough, people came together, supported each other, and adapted to the new normal. Covid-19 taught us a lot about resilience and the importance of healthcare.
Persuasive Tone
Covid-19, caused by the novel coronavirus, has highlighted the urgent need for better healthcare systems and global cooperation. The pandemic led to widespread lockdowns, social distancing, and mask mandates, disrupting daily life and economies. Our healthcare systems were overwhelmed, underscoring the critical need for robust medical infrastructure. The rapid development of vaccines showcased the power of scientific research and international collaboration. Now, more than ever, it is crucial to support and strengthen our healthcare systems, invest in scientific research, and promote global cooperation to ensure we are better prepared for future health crises. Let’s learn from this pandemic and build a stronger, healthier world together.

Reflective Tone
Reflecting on the impact of Covid-19, it’s clear that the pandemic has reshaped our world in profound ways. The novel coronavirus led to unprecedented global lockdowns, social distancing, and mask mandates, dramatically altering daily life. Our healthcare systems were tested like never before, revealing both strengths and weaknesses. The rapid development and distribution of vaccines highlighted the importance of scientific innovation and international cooperation. Amid the challenges, communities showed remarkable resilience and adaptability, finding new ways to connect and support one another. Covid-19 has taught us valuable lessons about preparedness, the significance of healthcare, and the power of human resilience in the face of adversity.
Inspirational Tone
Covid-19 has been a challenging journey, but it has also shown the incredible strength and resilience of humanity. The novel coronavirus led to global lockdowns, social distancing, and mask mandates, changing our daily lives dramatically. Despite these hardships, the rapid development and distribution of vaccines brought hope and showcased the power of scientific innovation and global cooperation. Communities came together, supporting each other and adapting to new realities. Healthcare workers became heroes, showing unparalleled dedication and bravery. Covid-19 has taught us the importance of unity, resilience, and the ability to overcome even the toughest challenges. Together, we can build a brighter, healthier future.
Optimistic Tone
Covid-19, caused by the novel coronavirus, brought significant challenges, but it also highlighted the resilience and adaptability of people worldwide. The pandemic led to lockdowns, social distancing, and mask-wearing, changing our daily routines. Despite these difficulties, the rapid development of vaccines brought hope and demonstrated the power of scientific progress. Communities came together, supporting one another and finding new ways to connect. Healthcare workers showed incredible dedication, and the world witnessed the strength of human spirit. Covid-19 has been a tough journey, but it also reinforced our ability to overcome adversity and work towards a healthier, more connected future.
Urgent Tone
The Covid-19 pandemic, caused by the novel coronavirus, demands our immediate attention and action. Since its outbreak, the virus has led to widespread lockdowns, social distancing, and mandatory mask usage, significantly disrupting daily life. Healthcare systems have been overwhelmed, highlighting the urgent need for better preparedness and robust medical infrastructure. The rapid development of vaccines has been crucial, but we must continue to prioritize public health measures and global cooperation to combat this crisis. Now is the time to invest in healthcare, support scientific research, and work together to overcome this pandemic. Immediate action is essential to protect lives and prevent further devastation.
Word Count-wise Paragraph Examples on Covid-19
Covid-19, caused by the novel coronavirus, has had a profound impact on the world since its outbreak. The pandemic led to widespread lockdowns, social distancing measures, and mandatory mask-wearing to prevent the virus’s spread. Healthcare systems were overwhelmed, emphasizing the need for robust medical infrastructure and preparedness. The development and distribution of vaccines became a global priority, showcasing the importance of scientific research and international cooperation. Economies faced significant challenges, with businesses closing and unemployment rates rising. Despite these hardships, the pandemic also brought communities together, highlighting resilience, adaptability, and the critical role of healthcare workers in combating the crisis. The rapid development and distribution of vaccines became a beacon of hope, demonstrating the power of scientific collaboration and innovation.
Covid-19, caused by the novel coronavirus SARS-CoV-2, emerged in late 2019 and rapidly spread across the globe, leading to an unprecedented pandemic. The virus’s high transmission rate prompted governments worldwide to implement stringent measures such as lockdowns, social distancing, and mask mandates to control its spread. These measures, while necessary, significantly disrupted daily life, impacting economies, education, and social interactions. Healthcare systems were strained, underscoring the need for better preparedness and robust medical infrastructure. The rapid development and global distribution of vaccines became a beacon of hope, demonstrating the power of scientific collaboration and innovation. The pandemic also highlighted the disparities in healthcare access and the importance of public health initiatives. Despite the immense challenges, communities showed resilience and adaptability, finding new ways to connect and support each other.
Covid-19, caused by the novel coronavirus SARS-CoV-2, emerged in late 2019 and rapidly spread across the globe, leading to an unprecedented pandemic. The virus’s high transmission rate prompted governments worldwide to implement stringent measures such as lockdowns, social distancing, and mask mandates to control its spread. These measures, while necessary, significantly disrupted daily life, impacting economies, education, and social interactions. Healthcare systems were strained, underscoring the need for better preparedness and robust medical infrastructure. The rapid development and global distribution of vaccines became a beacon of hope, demonstrating the power of scientific collaboration and innovation. The pandemic also highlighted the disparities in healthcare access and the importance of public health initiatives. Despite the immense challenges, communities showed resilience and adaptability, finding new ways to connect and support each other. The dedication of healthcare workers and the collective effort to combat the virus underscored the importance of global solidarity. Covid-19 has reshaped our world, teaching valuable lessons about preparedness, the significance of science, and the strength of human resilience in the face of adversity. The pandemic emphasized the need for robust healthcare systems, scientific innovation, and global cooperation. Despite the challenges, the collective resilience and adaptability of people worldwide have shown the strength of the human spirit in overcoming adversity.
Text prompt
- Instructive
- Professional
10 Examples of Public speaking
20 Examples of Gas lighting
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Reflecting on nursing practice during the COVID-19 pandemic
Affiliation.
- 1 School of Nursing, Midwifery and Social Work, Canterbury Christ Church University, Kent, England.
- PMID: 33016663
- DOI: 10.7748/ns.2020.e11569
The coronavirus disease 2019 (COVID-19) pandemic has resulted in significant challenges for nurses, both professionally and personally. In these unprecedented times, new opportunities to reflect on practice have emerged. Through reflection, whether individually or with others, nurses can explore areas of their practice that could be developed and improved. This article outlines the types of reflection and discusses its benefits and challenges, explaining how it is linked to nurses' regulatory revalidation processes. It also details various models and activities that nurses can use to reflect on their practice during the COVID-19 pandemic and beyond.
Keywords: COVID-19; continuing professional development; coronavirus; education; nurses’ wellbeing; personal development; practice learning; professional; professional issues; reflection.
© 2020 RCN Publishing Company Ltd. All rights reserved. Not to be copied, transmitted or recorded in any way, in whole or part, without prior permission of the publishers.
PubMed Disclaimer
Conflict of interest statement
None declared
Erratum for
- How to undertake intravenous infusion calculations. Brindley J. Brindley J. Nurs Stand. 2020 Jan 13. doi: 10.7748/ns.2020.e11444. Online ahead of print. Nurs Stand. 2020. PMID: 31930888
Similar articles
- Care-home Nurses' responses to the COVID-19 pandemic: Managing ethical conundrums at personal cost: A qualitative study. Birt L, Lane K, Corner J, Sanderson K, Bunn D. Birt L, et al. J Nurs Scholarsh. 2023 Jan;55(1):226-238. doi: 10.1111/jnu.12855. Epub 2022 Dec 4. J Nurs Scholarsh. 2023. PMID: 36464814 Free PMC article.
- Importance of reflection in revalidation. Coward M. Coward M. Nurs Manag (Harrow). 2019 Mar 26;26(2):37-41. doi: 10.7748/nm.2019.e1839. Epub 2019 Feb 27. Nurs Manag (Harrow). 2019. PMID: 31468762
- Mental health nurses' experience of resilience during COVID-19: A qualitative inquiry. Bui MV, McInnes E, Ennis G, Foster K. Bui MV, et al. Int J Ment Health Nurs. 2023 Dec;32(6):1735-1744. doi: 10.1111/inm.13213. Epub 2023 Aug 21. Int J Ment Health Nurs. 2023. PMID: 37605316
- Factors influencing adequate and effective clinical supervision for inpatient mental health nurses' personal and professional development: An integrative review. Howard V, Eddy-Imishue GK. Howard V, et al. J Psychiatr Ment Health Nurs. 2020 Oct;27(5):640-656. doi: 10.1111/jpm.12604. Epub 2020 Feb 9. J Psychiatr Ment Health Nurs. 2020. PMID: 31981445 Review.
- UK nurses' and midwives' experiences of healthful leadership practices during the COVID-19 pandemic: A rapid realist review. Dickson CAW, Davies C, McCormack B, Westcott L, Merrell J, Mcilfatrick S, Dewing J. Dickson CAW, et al. J Nurs Manag. 2022 Nov;30(8):3942-3957. doi: 10.1111/jonm.13790. Epub 2022 Oct 29. J Nurs Manag. 2022. PMID: 36063427 Free PMC article. Review.
Publication types
- Search in MeSH
- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
Why the Pandemic Probably Started in a Lab, in 5 Key Points

By Alina Chan
Dr. Chan is a molecular biologist at the Broad Institute of M.I.T. and Harvard, and a co-author of “Viral: The Search for the Origin of Covid-19.”
This article has been updated to reflect news developments.
On Monday, Dr. Anthony Fauci returned to the halls of Congress and testified before the House subcommittee investigating the Covid-19 pandemic. He was questioned about several topics related to the government’s handling of Covid-19, including how the National Institute of Allergy and Infectious Diseases, which he directed until retiring in 2022, supported risky virus work at a Chinese institute whose research may have caused the pandemic.
For more than four years, reflexive partisan politics have derailed the search for the truth about a catastrophe that has touched us all. It has been estimated that at least 25 million people around the world have died because of Covid-19, with over a million of those deaths in the United States.
Although how the pandemic started has been hotly debated, a growing volume of evidence — gleaned from public records released under the Freedom of Information Act, digital sleuthing through online databases, scientific papers analyzing the virus and its spread, and leaks from within the U.S. government — suggests that the pandemic most likely occurred because a virus escaped from a research lab in Wuhan, China. If so, it would be the most costly accident in the history of science.
Here’s what we now know:
1 The SARS-like virus that caused the pandemic emerged in Wuhan, the city where the world’s foremost research lab for SARS-like viruses is located.
- At the Wuhan Institute of Virology, a team of scientists had been hunting for SARS-like viruses for over a decade, led by Shi Zhengli.
- Their research showed that the viruses most similar to SARS‑CoV‑2, the virus that caused the pandemic, circulate in bats that live r oughly 1,000 miles away from Wuhan. Scientists from Dr. Shi’s team traveled repeatedly to Yunnan province to collect these viruses and had expanded their search to Southeast Asia. Bats in other parts of China have not been found to carry viruses that are as closely related to SARS-CoV-2.

The closest known relatives to SARS-CoV-2 were found in southwestern China and in Laos.
Large cities
Mine in Yunnan province
Cave in Laos
South China Sea

The closest known relatives to SARS-CoV-2
were found in southwestern China and in Laos.
philippines

The closest known relatives to SARS-CoV-2 were found
in southwestern China and Laos.
Sources: Sarah Temmam et al., Nature; SimpleMaps
Note: Cities shown have a population of at least 200,000.

There are hundreds of large cities in China and Southeast Asia.

There are hundreds of large cities in China
and Southeast Asia.

The pandemic started roughly 1,000 miles away, in Wuhan, home to the world’s foremost SARS-like virus research lab.

The pandemic started roughly 1,000 miles away,
in Wuhan, home to the world’s foremost SARS-like virus research lab.

The pandemic started roughly 1,000 miles away, in Wuhan,
home to the world’s foremost SARS-like virus research lab.
- Even at hot spots where these viruses exist naturally near the cave bats of southwestern China and Southeast Asia, the scientists argued, as recently as 2019 , that bat coronavirus spillover into humans is rare .
- When the Covid-19 outbreak was detected, Dr. Shi initially wondered if the novel coronavirus had come from her laboratory , saying she had never expected such an outbreak to occur in Wuhan.
- The SARS‑CoV‑2 virus is exceptionally contagious and can jump from species to species like wildfire . Yet it left no known trace of infection at its source or anywhere along what would have been a thousand-mile journey before emerging in Wuhan.
2 The year before the outbreak, the Wuhan institute, working with U.S. partners, had proposed creating viruses with SARS‑CoV‑2’s defining feature.
- Dr. Shi’s group was fascinated by how coronaviruses jump from species to species. To find viruses, they took samples from bats and other animals , as well as from sick people living near animals carrying these viruses or associated with the wildlife trade. Much of this work was conducted in partnership with the EcoHealth Alliance, a U.S.-based scientific organization that, since 2002, has been awarded over $80 million in federal funding to research the risks of emerging infectious diseases.
- The laboratory pursued risky research that resulted in viruses becoming more infectious : Coronaviruses were grown from samples from infected animals and genetically reconstructed and recombined to create new viruses unknown in nature. These new viruses were passed through cells from bats, pigs, primates and humans and were used to infect civets and humanized mice (mice modified with human genes). In essence, this process forced these viruses to adapt to new host species, and the viruses with mutations that allowed them to thrive emerged as victors.
- By 2019, Dr. Shi’s group had published a database describing more than 22,000 collected wildlife samples. But external access was shut off in the fall of 2019, and the database was not shared with American collaborators even after the pandemic started , when such a rich virus collection would have been most useful in tracking the origin of SARS‑CoV‑2. It remains unclear whether the Wuhan institute possessed a precursor of the pandemic virus.
- In 2021, The Intercept published a leaked 2018 grant proposal for a research project named Defuse , which had been written as a collaboration between EcoHealth, the Wuhan institute and Ralph Baric at the University of North Carolina, who had been on the cutting edge of coronavirus research for years. The proposal described plans to create viruses strikingly similar to SARS‑CoV‑2.
- Coronaviruses bear their name because their surface is studded with protein spikes, like a spiky crown, which they use to enter animal cells. T he Defuse project proposed to search for and create SARS-like viruses carrying spikes with a unique feature: a furin cleavage site — the same feature that enhances SARS‑CoV‑2’s infectiousness in humans, making it capable of causing a pandemic. Defuse was never funded by the United States . However, in his testimony on Monday, Dr. Fauci explained that the Wuhan institute would not need to rely on U.S. funding to pursue research independently.

The Wuhan lab ran risky experiments to learn about how SARS-like viruses might infect humans.
1. Collect SARS-like viruses from bats and other wild animals, as well as from people exposed to them.

2. Identify high-risk viruses by screening for spike proteins that facilitate infection of human cells.

2. Identify high-risk viruses by screening for spike proteins that facilitate infection of
human cells.

In Defuse, the scientists proposed to add a furin cleavage site to the spike protein.
3. Create new coronaviruses by inserting spike proteins or other features that could make the viruses more infectious in humans.

4. Infect human cells, civets and humanized mice with the new coronaviruses, to determine how dangerous they might be.

- While it’s possible that the furin cleavage site could have evolved naturally (as seen in some distantly related coronaviruses), out of the hundreds of SARS-like viruses cataloged by scientists, SARS‑CoV‑2 is the only one known to possess a furin cleavage site in its spike. And the genetic data suggest that the virus had only recently gained the furin cleavage site before it started the pandemic.
- Ultimately, a never-before-seen SARS-like virus with a newly introduced furin cleavage site, matching the description in the Wuhan institute’s Defuse proposal, caused an outbreak in Wuhan less than two years after the proposal was drafted.
- When the Wuhan scientists published their seminal paper about Covid-19 as the pandemic roared to life in 2020, they did not mention the virus’s furin cleavage site — a feature they should have been on the lookout for, according to their own grant proposal, and a feature quickly recognized by other scientists.
- Worse still, as the pandemic raged, their American collaborators failed to publicly reveal the existence of the Defuse proposal. The president of EcoHealth, Peter Daszak, recently admitted to Congress that he doesn’t know about virus samples collected by the Wuhan institute after 2015 and never asked the lab’s scientists if they had started the work described in Defuse. In May, citing failures in EcoHealth’s monitoring of risky experiments conducted at the Wuhan lab, the Biden administration suspended all federal funding for the organization and Dr. Daszak, and initiated proceedings to bar them from receiving future grants. In his testimony on Monday, Dr. Fauci said that he supported the decision to suspend and bar EcoHealth.
- Separately, Dr. Baric described the competitive dynamic between his research group and the institute when he told Congress that the Wuhan scientists would probably not have shared their most interesting newly discovered viruses with him . Documents and email correspondence between the institute and Dr. Baric are still being withheld from the public while their release is fiercely contested in litigation.
- In the end, American partners very likely knew of only a fraction of the research done in Wuhan. According to U.S. intelligence sources, some of the institute’s virus research was classified or conducted with or on behalf of the Chinese military . In the congressional hearing on Monday, Dr. Fauci repeatedly acknowledged the lack of visibility into experiments conducted at the Wuhan institute, saying, “None of us can know everything that’s going on in China, or in Wuhan, or what have you. And that’s the reason why — I say today, and I’ve said at the T.I.,” referring to his transcribed interview with the subcommittee, “I keep an open mind as to what the origin is.”
3 The Wuhan lab pursued this type of work under low biosafety conditions that could not have contained an airborne virus as infectious as SARS‑CoV‑2.
- Labs working with live viruses generally operate at one of four biosafety levels (known in ascending order of stringency as BSL-1, 2, 3 and 4) that describe the work practices that are considered sufficiently safe depending on the characteristics of each pathogen. The Wuhan institute’s scientists worked with SARS-like viruses under inappropriately low biosafety conditions .

In the United States, virologists generally use stricter Biosafety Level 3 protocols when working with SARS-like viruses.
Biosafety cabinets prevent
viral particles from escaping.
Viral particles
Personal respirators provide
a second layer of defense against breathing in the virus.
DIRECT CONTACT
Gloves prevent skin contact.
Disposable wraparound
gowns cover much of the rest of the body.

Personal respirators provide a second layer of defense against breathing in the virus.
Disposable wraparound gowns
cover much of the rest of the body.
Note: Biosafety levels are not internationally standardized, and some countries use more permissive protocols than others.

The Wuhan lab had been regularly working with SARS-like viruses under Biosafety Level 2 conditions, which could not prevent a highly infectious virus like SARS-CoV-2 from escaping.
Some work is done in the open air, and masks are not required.
Less protective equipment provides more opportunities
for contamination.

Some work is done in the open air,
and masks are not required.
Less protective equipment provides more opportunities for contamination.
- In one experiment, Dr. Shi’s group genetically engineered an unexpectedly deadly SARS-like virus (not closely related to SARS‑CoV‑2) that exhibited a 10,000-fold increase in the quantity of virus in the lungs and brains of humanized mice . Wuhan institute scientists handled these live viruses at low biosafet y levels , including BSL-2.
- Even the much more stringent containment at BSL-3 cannot fully prevent SARS‑CoV‑2 from escaping . Two years into the pandemic, the virus infected a scientist in a BSL-3 laboratory in Taiwan, which was, at the time, a zero-Covid country. The scientist had been vaccinated and was tested only after losing the sense of smell. By then, more than 100 close contacts had been exposed. Human error is a source of exposure even at the highest biosafety levels , and the risks are much greater for scientists working with infectious pathogens at low biosafety.
- An early draft of the Defuse proposal stated that the Wuhan lab would do their virus work at BSL-2 to make it “highly cost-effective.” Dr. Baric added a note to the draft highlighting the importance of using BSL-3 to contain SARS-like viruses that could infect human cells, writing that “U.S. researchers will likely freak out.” Years later, after SARS‑CoV‑2 had killed millions, Dr. Baric wrote to Dr. Daszak : “I have no doubt that they followed state determined rules and did the work under BSL-2. Yes China has the right to set their own policy. You believe this was appropriate containment if you want but don’t expect me to believe it. Moreover, don’t insult my intelligence by trying to feed me this load of BS.”
- SARS‑CoV‑2 is a stealthy virus that transmits effectively through the air, causes a range of symptoms similar to those of other common respiratory diseases and can be spread by infected people before symptoms even appear. If the virus had escaped from a BSL-2 laboratory in 2019, the leak most likely would have gone undetected until too late.
- One alarming detail — leaked to The Wall Street Journal and confirmed by current and former U.S. government officials — is that scientists on Dr. Shi’s team fell ill with Covid-like symptoms in the fall of 2019 . One of the scientists had been named in the Defuse proposal as the person in charge of virus discovery work. The scientists denied having been sick .
4 The hypothesis that Covid-19 came from an animal at the Huanan Seafood Market in Wuhan is not supported by strong evidence.
- In December 2019, Chinese investigators assumed the outbreak had started at a centrally located market frequented by thousands of visitors daily. This bias in their search for early cases meant that cases unlinked to or located far away from the market would very likely have been missed. To make things worse, the Chinese authorities blocked the reporting of early cases not linked to the market and, claiming biosafety precautions, ordered the destruction of patient samples on January 3, 2020, making it nearly impossible to see the complete picture of the earliest Covid-19 cases. Information about dozens of early cases from November and December 2019 remains inaccessible.
- A pair of papers published in Science in 2022 made the best case for SARS‑CoV‑2 having emerged naturally from human-animal contact at the Wuhan market by focusing on a map of the early cases and asserting that the virus had jumped from animals into humans twice at the market in 2019. More recently, the two papers have been countered by other virologists and scientists who convincingly demonstrate that the available market evidence does not distinguish between a human superspreader event and a natural spillover at the market.
- Furthermore, the existing genetic and early case data show that all known Covid-19 cases probably stem from a single introduction of SARS‑CoV‑2 into people, and the outbreak at the Wuhan market probably happened after the virus had already been circulating in humans.

An analysis of SARS-CoV-2’s evolutionary tree shows how the virus evolved as it started to spread through humans.
SARS-COV-2 Viruses closest
to bat coronaviruses
more mutations

Source: Lv et al., Virus Evolution (2024) , as reproduced by Jesse Bloom

The viruses that infected people linked to the market were most likely not the earliest form of the virus that started the pandemic.

- Not a single infected animal has ever been confirmed at the market or in its supply chain. Without good evidence that the pandemic started at the Huanan Seafood Market, the fact that the virus emerged in Wuhan points squarely at its unique SARS-like virus laboratory.
5 Key evidence that would be expected if the virus had emerged from the wildlife trade is still missing.

In previous outbreaks of coronaviruses, scientists were able to demonstrate natural origin by collecting multiple pieces of evidence linking infected humans to infected animals.
Infected animals
Earliest known
cases exposed to
live animals
Antibody evidence
of animals and
animal traders having
been infected
Ancestral variants
of the virus found in
Documented trade
of host animals
between the area
where bats carry
closely related viruses
and the outbreak site

Infected animals found
Earliest known cases exposed to live animals
Antibody evidence of animals and animal
traders having been infected
Ancestral variants of the virus found in animals
Documented trade of host animals
between the area where bats carry closely
related viruses and the outbreak site

For SARS-CoV-2, these same key pieces of evidence are still missing , more than four years after the virus emerged.

For SARS-CoV-2, these same key pieces of evidence are still missing ,
more than four years after the virus emerged.
- Despite the intense search trained on the animal trade and people linked to the market, investigators have not reported finding any animals infected with SARS‑CoV‑2 that had not been infected by humans. Yet, infected animal sources and other connective pieces of evidence were found for the earlier SARS and MERS outbreaks as quickly as within a few days, despite the less advanced viral forensic technologies of two decades ago.
- Even though Wuhan is the home base of virus hunters with world-leading expertise in tracking novel SARS-like viruses, investigators have either failed to collect or report key evidence that would be expected if Covid-19 emerged from the wildlife trade . For example, investigators have not determined that the earliest known cases had exposure to intermediate host animals before falling ill. No antibody evidence shows that animal traders in Wuhan are regularly exposed to SARS-like viruses, as would be expected in such situations.
- With today’s technology, scientists can detect how respiratory viruses — including SARS, MERS and the flu — circulate in animals while making repeated attempts to jump across species . Thankfully, these variants usually fail to transmit well after crossing over to a new species and tend to die off after a small number of infections. In contrast, virologists and other scientists agree that SARS‑CoV‑2 required little to no adaptation to spread rapidly in humans and other animals . The virus appears to have succeeded in causing a pandemic upon its only detected jump into humans.
The pandemic could have been caused by any of hundreds of virus species, at any of tens of thousands of wildlife markets, in any of thousands of cities, and in any year. But it was a SARS-like coronavirus with a unique furin cleavage site that emerged in Wuhan, less than two years after scientists, sometimes working under inadequate biosafety conditions, proposed collecting and creating viruses of that same design.
While several natural spillover scenarios remain plausible, and we still don’t know enough about the full extent of virus research conducted at the Wuhan institute by Dr. Shi’s team and other researchers, a laboratory accident is the most parsimonious explanation of how the pandemic began.
Given what we now know, investigators should follow their strongest leads and subpoena all exchanges between the Wuhan scientists and their international partners, including unpublished research proposals, manuscripts, data and commercial orders. In particular, exchanges from 2018 and 2019 — the critical two years before the emergence of Covid-19 — are very likely to be illuminating (and require no cooperation from the Chinese government to acquire), yet they remain beyond the public’s view more than four years after the pandemic began.
Whether the pandemic started on a lab bench or in a market stall, it is undeniable that U.S. federal funding helped to build an unprecedented collection of SARS-like viruses at the Wuhan institute, as well as contributing to research that enhanced them . Advocates and funders of the institute’s research, including Dr. Fauci, should cooperate with the investigation to help identify and close the loopholes that allowed such dangerous work to occur. The world must not continue to bear the intolerable risks of research with the potential to cause pandemics .
A successful investigation of the pandemic’s root cause would have the power to break a decades-long scientific impasse on pathogen research safety, determining how governments will spend billions of dollars to prevent future pandemics. A credible investigation would also deter future acts of negligence and deceit by demonstrating that it is indeed possible to be held accountable for causing a viral pandemic. Last but not least, people of all nations need to see their leaders — and especially, their scientists — heading the charge to find out what caused this world-shaking event. Restoring public trust in science and government leadership requires it.
A thorough investigation by the U.S. government could unearth more evidence while spurring whistleblowers to find their courage and seek their moment of opportunity. It would also show the world that U.S. leaders and scientists are not afraid of what the truth behind the pandemic may be.
More on how the pandemic may have started

Where Did the Coronavirus Come From? What We Already Know Is Troubling.
Even if the coronavirus did not emerge from a lab, the groundwork for a potential disaster had been laid for years, and learning its lessons is essential to preventing others.
By Zeynep Tufekci

Why Does Bad Science on Covid’s Origin Get Hyped?
If the raccoon dog was a smoking gun, it fired blanks.
By David Wallace-Wells

A Plea for Making Virus Research Safer
A way forward for lab safety.
By Jesse Bloom
The Times is committed to publishing a diversity of letters to the editor. We’d like to hear what you think about this or any of our articles. Here are some tips . And here’s our email: [email protected] .
Follow the New York Times Opinion section on Facebook , Instagram , TikTok , WhatsApp , X and Threads .
Alina Chan ( @ayjchan ) is a molecular biologist at the Broad Institute of M.I.T. and Harvard, and a co-author of “ Viral : The Search for the Origin of Covid-19.” She was a member of the Pathogens Project , which the Bulletin of the Atomic Scientists organized to generate new thinking on responsible, high-risk pathogen research.
- Share full article
Advertisement
COVID-19: Long-term effects
Some people continue to experience health problems long after having COVID-19. Understand the possible symptoms and risk factors for post-COVID-19 syndrome.
Most people who get coronavirus disease 2019 (COVID-19) recover within a few weeks. But some people — even those who had mild versions of the disease — might have symptoms that last a long time afterward. These ongoing health problems are sometimes called post- COVID-19 syndrome, post- COVID conditions, long COVID-19 , long-haul COVID-19 , and post acute sequelae of SARS COV-2 infection (PASC).
What is post-COVID-19 syndrome and how common is it?
Post- COVID-19 syndrome involves a variety of new, returning or ongoing symptoms that people experience more than four weeks after getting COVID-19 . In some people, post- COVID-19 syndrome lasts months or years or causes disability.
Research suggests that between one month and one year after having COVID-19 , 1 in 5 people ages 18 to 64 has at least one medical condition that might be due to COVID-19 . Among people age 65 and older, 1 in 4 has at least one medical condition that might be due to COVID-19 .
What are the symptoms of post-COVID-19 syndrome?
The most commonly reported symptoms of post- COVID-19 syndrome include:
- Symptoms that get worse after physical or mental effort
- Lung (respiratory) symptoms, including difficulty breathing or shortness of breath and cough
Other possible symptoms include:
- Neurological symptoms or mental health conditions, including difficulty thinking or concentrating, headache, sleep problems, dizziness when you stand, pins-and-needles feeling, loss of smell or taste, and depression or anxiety
- Joint or muscle pain
- Heart symptoms or conditions, including chest pain and fast or pounding heartbeat
- Digestive symptoms, including diarrhea and stomach pain
- Blood clots and blood vessel (vascular) issues, including a blood clot that travels to the lungs from deep veins in the legs and blocks blood flow to the lungs (pulmonary embolism)
- Other symptoms, such as a rash and changes in the menstrual cycle
Keep in mind that it can be hard to tell if you are having symptoms due to COVID-19 or another cause, such as a preexisting medical condition.
It's also not clear if post- COVID-19 syndrome is new and unique to COVID-19 . Some symptoms are similar to those caused by chronic fatigue syndrome and other chronic illnesses that develop after infections. Chronic fatigue syndrome involves extreme fatigue that worsens with physical or mental activity, but doesn't improve with rest.
Why does COVID-19 cause ongoing health problems?
Organ damage could play a role. People who had severe illness with COVID-19 might experience organ damage affecting the heart, kidneys, skin and brain. Inflammation and problems with the immune system can also happen. It isn't clear how long these effects might last. The effects also could lead to the development of new conditions, such as diabetes or a heart or nervous system condition.
The experience of having severe COVID-19 might be another factor. People with severe symptoms of COVID-19 often need to be treated in a hospital intensive care unit. This can result in extreme weakness and post-traumatic stress disorder, a mental health condition triggered by a terrifying event.
What are the risk factors for post-COVID-19 syndrome?
You might be more likely to have post- COVID-19 syndrome if:
- You had severe illness with COVID-19 , especially if you were hospitalized or needed intensive care.
- You had certain medical conditions before getting the COVID-19 virus.
- You had a condition affecting your organs and tissues (multisystem inflammatory syndrome) while sick with COVID-19 or afterward.
Post- COVID-19 syndrome also appears to be more common in adults than in children and teens. However, anyone who gets COVID-19 can have long-term effects, including people with no symptoms or mild illness with COVID-19 .
What should you do if you have post-COVID-19 syndrome symptoms?
If you're having symptoms of post- COVID-19 syndrome, talk to your health care provider. To prepare for your appointment, write down:
- When your symptoms started
- What makes your symptoms worse
- How often you experience symptoms
- How your symptoms affect your activities
Your health care provider might do lab tests, such as a complete blood count or liver function test. You might have other tests or procedures, such as chest X-rays, based on your symptoms. The information you provide and any test results will help your health care provider come up with a treatment plan.
In addition, you might benefit from connecting with others in a support group and sharing resources.
- Long COVID or post-COVID conditions. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/long-term-effects.html. Accessed May 6, 2022.
- Post-COVID conditions: Overview for healthcare providers. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-care/post-covid-conditions.html. Accessed May 6, 2022.
- Mikkelsen ME, et al. COVID-19: Evaluation and management of adults following acute viral illness. https://www.uptodate.com/contents/search. Accessed May 6, 2022.
- Saeed S, et al. Coronavirus disease 2019 and cardiovascular complications: Focused clinical review. Journal of Hypertension. 2021; doi:10.1097/HJH.0000000000002819.
- AskMayoExpert. Post-COVID-19 syndrome. Mayo Clinic; 2022.
- Multisystem inflammatory syndrome (MIS). Centers for Disease Control and Prevention. https://www.cdc.gov/mis/index.html. Accessed May 24, 2022.
- Patient tips: Healthcare provider appointments for post-COVID conditions. https://www.cdc.gov/coronavirus/2019-ncov/long-term-effects/post-covid-appointment/index.html. Accessed May 24, 2022.
- Bull-Otterson L, et al. Post-COVID conditions among adult COVID-19 survivors aged 18-64 and ≥ 65 years — United States, March 2020 — November 2021. MMWR Morbidity and Mortality Weekly Report. 2022; doi:10.15585/mmwr.mm7121e1.
Products and Services
- A Book: Endemic - A Post-Pandemic Playbook
- Begin Exploring Women's Health Solutions at Mayo Clinic Store
- A Book: Future Care
- Antibiotics: Are you misusing them?
- COVID-19 and vitamin D
- Convalescent plasma therapy
- Coronavirus disease 2019 (COVID-19)
- COVID-19: How can I protect myself?
- Herd immunity and respiratory illness
- COVID-19 and pets
- COVID-19 and your mental health
- COVID-19 antibody testing
- COVID-19, cold, allergies and the flu
- COVID-19 tests
- COVID-19 drugs: Are there any that work?
- COVID-19 in babies and children
- Coronavirus infection by race
- COVID-19 travel advice
- COVID-19 vaccine: Should I reschedule my mammogram?
- COVID-19 vaccines for kids: What you need to know
- COVID-19 vaccines
- COVID-19 variant
- COVID-19 vs. flu: Similarities and differences
- COVID-19: Who's at higher risk of serious symptoms?
- Debunking coronavirus myths
- Different COVID-19 vaccines
- Extracorporeal membrane oxygenation (ECMO)
- Fever: First aid
- Fever treatment: Quick guide to treating a fever
- Fight coronavirus (COVID-19) transmission at home
- Honey: An effective cough remedy?
- How do COVID-19 antibody tests differ from diagnostic tests?
- How to measure your respiratory rate
- How to take your pulse
- How to take your temperature
- How well do face masks protect against COVID-19?
- Is hydroxychloroquine a treatment for COVID-19?
- Loss of smell
- Mayo Clinic Minute: You're washing your hands all wrong
- Mayo Clinic Minute: How dirty are common surfaces?
- Multisystem inflammatory syndrome in children (MIS-C)
- Nausea and vomiting
- Pregnancy and COVID-19
- Safe outdoor activities during the COVID-19 pandemic
- Safety tips for attending school during COVID-19
- Sex and COVID-19
- Shortness of breath
- Thermometers: Understand the options
- Treating COVID-19 at home
- Unusual symptoms of coronavirus
- Vaccine guidance from Mayo Clinic
- Watery eyes
Related information
- Post-COVID Recovery & COVID-19 Support Group - Related information Post-COVID Recovery & COVID-19 Support Group
- Rehabilitation after COVID-19 - Related information Rehabilitation after COVID-19
- Post-COVID-19 syndrome could be a long haul (podcast) - Related information Post-COVID-19 syndrome could be a long haul (podcast)
- COVID-19 Coronavirus Long-term effects
We’re transforming healthcare
Make a gift now and help create new and better solutions for more than 1.3 million patients who turn to Mayo Clinic each year.
- DOI: 10.18502/kss.v9i18.16325
- Corpus ID: 270164428
Overcome COVID-19 through Collaboration between Components in Indonesia
- Fenty Aprina
- Published in KnE Social Sciences 30 May 2024
Figures and Tables from this paper

31 References
Acceptance of a covid-19 vaccine in southeast asia: a cross-sectional study in indonesia.
- Highly Influential
Key Guidelines in Developing a Pre-Emptive COVID-19 Vaccination Uptake Promotion Strategy
Covid-19 vaccines: current status and implication for use in indonesia., covid-19 outbreak in malaysia: actions taken by the malaysian government, factors influencing covid-19 vaccine acceptance in indonesia: an adoption of technology acceptance model, the challenge of reaching undocumented migrants with covid-19 vaccination, psychological factors affecting covid-19 vaccine acceptance in indonesia, predicitive modeling, empowering women, and covid-19 in south sumatra, indonesia, government communication, perceptions of covid-19, and vaccination intention: a multi-group comparison in china, sentiment analysis of covid-19 vaccine in indonesia using naïve bayes algorithm, related papers.
Showing 1 through 3 of 0 Related Papers
Masks Strongly Recommended but Not Required in Maryland, Starting Immediately
Due to the downward trend in respiratory viruses in Maryland, masking is no longer required but remains strongly recommended in Johns Hopkins Medicine clinical locations in Maryland. Read more .
- Vaccines
- Masking Guidelines
- Visitor Guidelines

COVID-19 Vaccine: What You Need to Know
The COVID-19 vaccine is very good at preventing serious illness, hospitalization and death. Because the virus that causes COVID-19 continues to change, vaccines are updated to help fight the disease. It is important to check the Centers for Disease Control and Prevention (CDC) COVID-19 vaccine information for the latest details. (Posted 11/22/23)
What is the COVID-19 vaccine?
The COVID-19 vaccine lessens the severity of COVID-19 by teaching the immune system to recognize and fight the virus that causes the disease.
For fall/winter 2023–2024, the updated COVID-19 vaccine is based on the XBB.1.5 variant. The updated vaccine is made by Pfizer-BioNTech, Moderna and Novavax. This season, only one shot of the vaccine is needed for most people, and there are no boosters. (People who are immunocompromised or ages 6 months to 4 years may need more than one 2023–2024 vaccine.)
How is the 2023–2024 COVID-19 vaccine different from previous COVID-19 vaccines?
The 2023–2024 COVID-19 vaccine targets XBB.1.5, a subvariant of Omicron. While none of the variants currently circulating are exact matches to the vaccine, they are all closely related to the XBB.1.5 strain. Studies show that the updated vaccine is effective against the variants currently causing the majority of COVID-19 cases in the U.S.
Who should get a COVID-19 vaccine?
Because the 2023–2024 vaccine is effective for recent strains of COVID-19, it is recommended that everyone stay up to date with this vaccine. Previous vaccines or boosters were not developed to target the more recent strains. For 2023–2024, the CDC recommends:
- Everyone age 5 and older receive one shot of the updated vaccine.
- Children ages 6 months to 4 years may need more than one shot to be up to date.
- People who are moderately or severely immunocompromised may need more than one shot.
You can review the full recommendations on the CDC’s Stay Up to Date with COVID-19 Vaccines webpage . Be sure to talk to your primary care doctor or pediatrician if you are unsure about vaccine recommendations.
What are the side effects of the COVID-19 vaccine?
Side effects vary and may last one to three days. Common side effects are:
- Soreness at the injection site
COVID-19 Vaccine and Pregnancy
COVID-19 vaccines approved by the Food and Drug Administration (FDA) are safe and recommended for people who are pregnant or lactating, as well as for those r intending to become pregnant.
People who are pregnant or were recently pregnant are at a greater risk for severe COVID-19. Having a severe case of COVID-19 while pregnant is linked to a higher risk of pre-term birth and stillbirth and might increase the risk of other pregnancy complications.
What should parents know about the COVID-19 vaccine and children?
The CDC recommends the 2023–2024 vaccine for adolescents and teenagers ages 12 and older, and for children ages 6 months through 11 years.
- Children age 5 and older need one shot of the updated vaccine.
Children are less likely to become seriously ill from COVID-19 than adults, although serious illness can happen. Speak with your pediatrician if you have questions about having your child vaccinated.
If I recently had COVID-19, do I need a 2023–2024 vaccine?
If you recently had COVID-19, the CDC recommends waiting about three months before getting this updated vaccine. If you encounter the virus again, having the updated vaccine will:
- Lessen your risk of severe disease that could require hospitalization
- Reduce the chance that you infect someone else with COVID-19
- Help keep you protected from currently circulating COVID-19 variants
How long should I wait to get this vaccine if I recently had an earlier version of a COVID-19 vaccine or booster?
People age 5 years and older should wait at least two months after getting the last dose of any COVID-19 vaccine before receiving the 2023–2024 vaccine, according to CDC guidance .
Is natural immunity better than a vaccine?
Natural immunity is the antibody protection your body creates against a germ once you’ve been infected with it. Natural immunity to the virus that causes COVID-19 is no better than vaccine-acquired immunity, and it comes with far greater risks. Studies show that natural immunity to the virus weakens over time and does so faster than immunity provided by COVID-19 vaccination.
Do I need a COVID-19 booster?
The 2023–2024 vaccine is a one-shot vaccine for most people, and there is no booster this season. (People who are immunocompromised or ages 6 months to 4 years may need more than one 2023–2024 vaccine.)
The FDA calls this an updated vaccine (not a “booster” like previous shots) because it builds a new immune response to variants that are currently circulating. This change reflects the current approach of treating COVID-19 similarly to the flu, with preventive measures such as an annual vaccination.
When should I get a COVID-19 vaccine?
Like the flu and other respiratory diseases, COVID-19 tends to be more active in the fall and winter, so getting a vaccine in the fall is recommended.
How quickly does the COVID-19 vaccine become effective?
It usually takes about two weeks for the vaccine to become effective. The CDC website provides more information on how the COVID-19 vaccines work .
How long does the COVID-19 vaccine last?
Studies suggest that COVID-19 vaccines are most effective during the first three months after vaccination.
Is it safe to get a flu and COVID-19 vaccine at the same time?
Yes, it safe to get both shots at the same time. Keep in mind that each has similar side effects and you may experience side effects from both.
Is the COVID-19 vaccine safe?
Yes. COVID-19 vaccines approved by the FDA meet rigorous testing criteria and are safe and effective at preventing serious illness, hospitalization and death. Millions of people have received the vaccines, and the CDC continues to monitor their safety and effectiveness as well as rare adverse events.
Where can I get a COVID-19 vaccine?
The COVID-19 vaccine is available at pharmacies. See vaccines.gov to find a convenient location.

Trauma Team Puts an Athlete Back in the Saddle

Patient Safety Infographic
Coronavirus: Younger Adults Are at Risk, Too
Related Topics
- Infectious Diseases

Preprints with The Lancet is part of SSRN´s First Look, a place where journals identify content of interest prior to publication. Authors have opted in at submission to The Lancet family of journals to post their preprints on Preprints with The Lancet. The usual SSRN checks and a Lancet-specific check for appropriateness and transparency have been applied. Preprints available here are not Lancet publications or necessarily under review with a Lancet journal. These preprints are early stage research papers that have not been peer-reviewed. The findings should not be used for clinical or public health decision making and should not be presented to a lay audience without highlighting that they are preliminary and have not been peer-reviewed. For more information on this collaboration, see the comments published in The Lancet about the trial period, and our decision to make this a permanent offering, or visit The Lancet´s FAQ page, and for any feedback please contact [email protected] .
Outpatient Treatment of COVID-19 and the Development of Long COVID Over 10 Months: A Multi-Center, Quadruple-Blind, Parallel Group Randomized Phase 3 Trial
42 Pages Posted: 6 Mar 2023
Carolyn Bramante
University of minnesota - minneapolis - general internal medicine, john b. buse.
University of North Carolina (UNC) at Chapel Hill - Endocrinology
David Liebovitz
Northwestern University - Division of General Internal Medicine
Jacinda Nicklas
University of Colorado at Denver - General Internal Medicine
Michael Puskarich
Hennepin County Medical Center - Emergency Medicine
Kenneth R. Cohen
UnitedHealth Group - Optum Labs
Hrishikesh Belani
University of California, Los Angeles (UCLA) - Department of Medicine, Olive View
Blake Anderson
Atlanta Veterans Affairs Medical Center; Emory University - Department of Medicine
Jared D. Huling
University of Minnesota - Minneapolis - Division of Biostatistics, School of Public Health
Christopher Tignanelli
University of Minnesota - Minneapolis - Institute for Health Informatics; University of Minnesota - Minneapolis - Department of Surgery; North Memorial Health Hospital - Department of Surgery
Jennifer Thompson
Vanderbilt University - Department of Obstetrics and Gynecology
Matthew Pullen
University of Minnesota - Minneapolis - Infectious Diseases
Esteban Lemus Wirtz
Lianne siegel, jennifer proper, david j. odde.
University of Minnesota - Department of Biomedical Engineering
Nichole Klatt
University of Minnesota - Minneapolis - Department of Surgery, Medical School
Nancy E. Sherwood
University of Minnesota - Minneapolis - Division of Epidemiology and Community Health
Sarah Lindberg
Amy b. karger.
University of Minnesota - Minneapolis - Department of Laboratory Medicine and Pathology
Kenneth B. Beckman
University of Minnesota - Minneapolis - University of Minnesota Genomics Center
Spencer Erickson
Sarah fenno, katrina hartman, michael rose.
Johns Hopkins University - Department of Medicine
Tanvi Mehta
Barkha patel, gwendolyn griffiths, thomas a. murray.
University of Minnesota - Minneapolis - Division of Biostatistics
David R. Boulware
Division of Infectious Diseases and International Medicine, Department of Medicine, University of Minnesota
Background: Post-acute sequelae of COVID, termed “Long COVID”, is an emerging chronic illness potentially affecting ~10% of those with COVID-19. We sought to determine if outpatient treatment with metformin, ivermectin, or fluvoxamine could prevent Long COVID. Methods: COVID-OUT (NCT04510194) was a decentralized, multi-site trial in the United States testing three medications (metformin, ivermectin, fluvoxamine) using a 2x3 parallel treatment factorial randomized assignment to efficiently share placebo controls. Participants, investigators, care providers, and outcomes assessors were masked to randomized treatment assignment. Inclusion criteria included: age 30 to 85 years with overweight or obesity, symptoms <7 days, enrolled within <=3 days of documented SARS-CoV-2 infection. Long COVID diagnosis from a medical provider was a pre-specified secondary outcome assessed by monthly surveys through 300 days after randomization and confirmed in medical records. Findings: Of 1323 randomized trial participants, 1125 consented for long-term follow up, and 95.1% completed >9 months of follow up. The median age was 45 years (IQR, 37 to 54), and 56% were female (7% pregnant). The median BMI was 30 kg/m2 (IQR, 27 to 34). Overall, 8.4% reported a medical provider diagnosed them with Long COVID; cumulative incidence: 6.3% with metformin and 10.6% with matched placebo. The hazard ratio (HR) for metformin preventing Long COVID was 0.58 (95%CI, 0.38 to 0.88; P=0·009) versus placebo. The metformin effect was consistent across subgroups, including viral variants. When metformin was started within <4 days of symptom onset, the HR for Long COVID was 0.37 (95%CI, 0.15 to 0.95). No statistical difference in Long COVID occurred in those randomized to either ivermectin (HR=0.99; 95%CI, 0.59 to 1.64) or fluvoxamine (HR=1.36; 95%CI, 0.78 to 2.34). Interpretations: A 42% relative decrease and 4.3% absolute decrease in the Long COVID incidence occurred in participants who received early outpatient COVID-19 treatment with metformin compared to exact-matching placebo. Trial Registration: ClinicalTrials.gov: NCT04510194. Funding: The trial was funded by the Parsemus Foundation, Rainwater Charitable Foundation, Fast Grants, and the UnitedHealth Group Foundation. Declaration of Interest: JBB reports contracted fees and travel support for contracted activities for consulting work paid to the University of North Carolina by Novo Nordisk; grant support by Dexcom, NovaTarg, Novo Nordisk, Sanofi, Tolerion and vTv Therapeutics; personal compensation for consultation from Alkahest, Altimmune, Anji, AstraZeneca, Bayer, Biomea Fusion Inc, Boehringer- Ingelheim, CeQur, Cirius Therapeutics Inc, Corcept Therapeutics, Eli Lilly, Fortress Biotech, GentiBio, Glycadia, Glyscend, Janssen, MannKind, Mellitus Health, Moderna, Pendulum Therapeutics, Praetego, Sanofi, Stability Health, Terns Inc, Valo and Zealand Pharma; and stock/options in Glyscend, Mellitus Health, Pendulum Therapeutics, PhaseBio, Praetego, and Stability Health. Ethical Approval: Institutional review boards at each site, and Advarra centrally, approved the protocol. An independent data safety monitoring board (DSMB) oversaw safety and efficacy monitoring, and an independent monitor oversaw study conduct in compliance with the Declaration of Helsinki, Good Clinical Practice Guidelines, and local requirements.
Keywords: Long COVID, COVID, Metformin, Randomized Clinical Trial
Suggested Citation: Suggested Citation
Carolyn Bramante (Contact Author)
University of north carolina (unc) at chapel hill - endocrinology ( email ), northwestern university - division of general internal medicine ( email ), university of colorado at denver - general internal medicine ( email ), hennepin county medical center - emergency medicine ( email ), unitedhealth group - optum labs ( email ), university of california, los angeles (ucla) - department of medicine, olive view ( email ), atlanta veterans affairs medical center ( email ), emory university - department of medicine ( email ).
Atlanta, GA United States
University of Minnesota - Minneapolis - Division of Biostatistics, School of Public Health ( email )
University of minnesota - minneapolis - institute for health informatics.
Minneapolis, MN United States
University of Minnesota - Minneapolis - Department of Surgery ( email )
420 Delaware St. SE Minneapolis, MN 55455 United States (612) 625-7911 (Phone)
North Memorial Health Hospital - Department of Surgery
Robbinsdale, MN United States
Vanderbilt University - Department of Obstetrics and Gynecology ( email )
University of minnesota - minneapolis - infectious diseases ( email ), university of minnesota - department of biomedical engineering ( email ).
Minneapolis, MN 55455 United States
University of Minnesota - Minneapolis - Department of Surgery, Medical School ( email )
University of minnesota - minneapolis - division of epidemiology and community health ( email ), university of minnesota - minneapolis - department of laboratory medicine and pathology ( email ), university of minnesota - minneapolis - university of minnesota genomics center ( email ), university of minnesota - minneapolis - general internal medicine ( email ), johns hopkins university - department of medicine ( email ), university of minnesota - minneapolis - division of biostatistics ( email ), division of infectious diseases and international medicine, department of medicine, university of minnesota ( email ), click here to go to thelancet.com, paper statistics, related ejournals, covid-19 ejournal.
Subscribe to this free journal for more curated articles on this topic
Preprints with The Lancet
Public health ejournal.
Subscribe to this fee journal for more curated articles on this topic

IMAGES
VIDEO
COMMENTS
Spring was an exceedingly challenging time because it wasn't only the COVID-19 context, but it was the murder of George Floyd. A lot of the students in my classes were out there in the streets protesting for social justice. In week nine or 10, one of the students turned on the camera and said, "The National Guard is right outside my window.
My content explains what my life was like during the last seven months of the Covid-19 pandemic and how it affected my life both positively and negatively. It also explains what it was like when I graduated from High School and how I want the future generations to remember the Class of 2020. Class assignment, Western Civilization (Dr. Marino).
Through this contextualized reflection on resilience, we hope to motivate strength and solidarity for providers, patients, and health systems, while proposing critical questions for our response moving forward. ... Recent CDC data show that black Americans were more likely to require hospitalization for COVID-19 than white Americans in the same ...
March 12, 2021. 11 min read. One year ago, the World Health Organization declared the spread of COVID-19 a worldwide pandemic. Reacting to the virus, schools at every level were sent scrambling ...
Students can choose to write a full-length college essay on the coronavirus or summarize their experience in a shorter form. To help students explain how the pandemic affected them, The Common App ...
Alex, a writer and fellow disabled parent, found the freedom to explore a fuller version of herself in the privacy the pandemic provided. "The way I dress, the way I love, and the way I carry ...
Prior to the spread of COVID-19, we had been reflecting with our partners on how difficult it is to change a system: Systems prefer the status quo and often require a crisis to transform. We are ...
This reflection offers a unique lens into my journey as an MPH student and budding public health nursing professional, during an unprecedented 9 months of the COVID‐19 pandemic. In October 2019, I fortunately began a public health nursing position even before I completed my MPH in May 2020. I transitioned from bedside nursing at a large ...
COVID-19: A year in reflections. The UC community shares their stories of a year of hardship, courage and resilience. March 19, 2021. Article by: UC Newsroom staff [email protected]. As we mark a full year since the global pandemic upended all of our lives, we asked members of the UC community to share their reflections on how these past ...
An elderly couple wearing face masks walks in Madrid on April 30, 2020 during a national lockdown to prevent the spread of the COVID-19 disease. Gabriel Bouys/AFP via Getty Images hide caption
However, as a result of COVID-19, the implementation period was cut by over half during the first term of the 2020 school year with an average implementation period of eight days across schools ...
Melva James, 42, is a cybersecurity consultant who grew up in Jackson, Miss., and lives in Massachusetts. The tumult of the past year inspired a dramatic life change. One of my best friend's ...
Reflective practice is a powerful tool and key for development (Kolb, 1984) because it enables 'continuous learning' as Schon (1983) highlights. Teachers who want to provide better learning, face to face or online, need to keep developing. However, reflecting in itself is insufficient to bring your skills and knowledge to the next level.
In this essay, I share my experiences and reflection on fighting the COVID-19 pandemic from the perspective of a Chinese student residing in Pittsburgh, USA. Three examples of "commoning"—acts of managing shared resources by a group of people—reveal the importance of care and collaboration in the time of uncertainty. First, when COVID-19 posed a threat to the food supply chain ...
This year's admissions essays became a platform for high school seniors to reflect on the pandemic, race and loss. ... added a question inviting students to write about the impact of Covid-19 on ...
Imperial researchers reflect on the lessons they will take away from the pandemic. Over the past 12 months the Imperial College London community has devoted an intense amount of time and research to COVID-19. Members of the community have been making fundamental scientific contributions to respond to coronavirus, from advising government policy ...
Read these 12 moving essays about life during coronavirus. Artists, novelists, critics, and essayists are writing the first draft of history. A woman wearing a face mask in Miami. Alissa Wilkinson ...
COVID‐19 pandemic is not only a matter of biological science but also a human problem. It is not an isolated problem, but deeply connected with the human condition and society. To re‐establish sustainable community health amid this pandemic, humanistic reflection is required.
This essay offers a philosophical and spiritual exploration of some of the language that has become part of daily life amidst the COVID-19 crisis. An Offering of Hope During COVID-19: A Personal Reflection J Relig Health. 2020 Dec;59(6) :2692-2696. ...
A practical, pragmatic, and rational ethical reflection is therefore needed to include these different elements. At the start of the COVID-19 pandemic, it was time to act and apply guidelines. 2. Almost a year later, the goal is to define an ethical vision capable of bringing countries together, while considering their specific characteristics.
The COVID-19 pandemic has amplified and revealed prevailing socioeconomic inequalities and the government's incompetency. The strict implementation of the lockdown has left most people without their safety nets. So far, Filipinos have been subsisting on daily earnings, but those who are homeless are left with no resources.
Alicia Sgroi, BSN, RN began working as an RN on a medical-surgical unit in February 2020. At the time, she and her colleagues knew a new coronavirus was coming to the United States. But the impact of the virus wasn't yet understood. When the first confirmed Covid -19 cases appeared in March in Florida, Sgroi became anxious and frightened.
Short Paragraph on Covid-19. Covid-19 is a global pandemic caused by the novel coronavirus. It has significantly impacted daily life, with governments worldwide implementing lockdowns, social distancing, and mask mandates to curb the virus's spread. The pandemic has highlighted the importance of healthcare systems and the need for vaccines.
The coronavirus disease 2019 (COVID-19) pandemic has resulted in significant challenges for nurses, both professionally and personally. In these unprecedented times, new opportunities to reflect on practice have emerged. Through reflection, whether individually or with others, nurses can explore areas of their practice that could be developed ...
Dr. Chan is a molecular biologist at the Broad Institute of M.I.T. and Harvard, and a co-author of "Viral: The Search for the Origin of Covid-19." This article has been updated to reflect news ...
2. The papers. In 'Higher Inequality in Latin America: A Collateral Effect of the Pandemic', Ivonne Acevedo, Francesca Castellani, María José Cota, Giulia Lotti and Miguel Székely explore the evolution of inequality in Latin America during the COVID-19 pandemic by using primary data from household and employment surveys collected in 2020.
People who had severe illness with COVID-19 might experience organ damage affecting the heart, kidneys, skin and brain. Inflammation and problems with the immune system can also happen. It isn't clear how long these effects might last. The effects also could lead to the development of new conditions, such as diabetes or a heart or nervous ...
The findings of the literature review show that the roles of and collaboration between public components, including the government, the Indonesian National Police, agencies, and the community, have an impact on the success of the Covid-19 vaccination in Indonesia. Vaccination against Covid-19 is one of the most important steps adopted by the government to limit the spread of the virus in the ...
The COVID-19 vaccine lessens the severity of COVID-19 by teaching the immune system to recognize and fight the virus that causes the disease. For fall/winter 2023-2024, the updated COVID-19 vaccine is based on the XBB.1.5 variant. The updated vaccine is made by Pfizer-BioNTech, Moderna and Novavax. This season, only one shot of the vaccine is ...
Interpretations: A 42% relative decrease and 4.3% absolute decrease in the Long COVID incidence occurred in participants who received early outpatient COVID-19 treatment with metformin compared to exact-matching placebo. Trial Registration: ClinicalTrials.gov: NCT04510194.