An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.


StatPearls [Internet].
Vital sign assessment.
Amit Sapra ; Ahmad Malik ; Priyanka Bhandari .
Affiliations
Last Update: May 1, 2023 .
- Definition/Introduction
Vital signs are an objective measurement of the essential physiological functions of a living organism. They have the name "vital" as their measurement and assessment is the critical first step for any clinical evaluation. The first set of clinical examinations is an evaluation of the vital signs of the patient. Triage of patients in an urgent/prompt care or an emergency department is based on their vital signs as it tells the physician the degree of derangement that is happening from the baseline. Healthcare providers must understand the various physiologic and pathologic processes affecting these sets of measurements and their proper interpretation. If we use a triage method where we select patients without determining their vital signs, it may not give us a reflection of the urgency of the patient's presentation. [1] The degree of vital sign abnormalities may also predict the long-term patient health outcomes, return emergency department visits, and frequency of readmission to hospitals, and utilization of healthcare resources.
Traditionally, the vital signs consist of temperature, pulse rate, blood pressure, and respiratory rate. Even though there are a variety of parameters that may be useful along with the traditional four vital sign parameters, studies have only found pulse oximetry and smoking status to have significance in patient outcomes. [2] Pulse oximetry sometimes helps to clarify the patient's physiological functions, which would sometimes be unclear by checking just the traditional vital signs. The inclusion of smoking status has the premise that the patient will be provided counseling by the provider on quitting smoking. In the past, some health care systems in the United States had used "pain as the fifth vital sign'. This approach is being abandoned due to the unintended opioid crisis that the country is currently facing. [3]
- Issues of Concern
Patient safety is a fundamental concern in any health care organization, and early detection of any clinical deterioration is of paramount importance whether the patient is in the emergency department or on the hospital floor. The early detection of changes in vital signs typically correlates with faster detection of changes in the cardiopulmonary status of the patient as well as up-gradation of the level of service if needed. Vital signs assessment currently uses electronic equipment, but there is evidence that, outside of the intensive care units, respiratory rate assessment through observation, leading to insufficient, subjective, and unreliable results. [4]
In a case-control study conducted by Rothschild and colleagues, early warning criterion among patients on the medical floor, the presence of respiratory rate over 35/min (OR=31.1) was most strongly associated with a life-threatening adverse event. [5] Early warning score (EWS) tools, mostly using vital sign abnormalities, are critical in predicting cardiac arrest and death within 48 hours of measurement, even though the effect on in-hospital health outcomes and utilization of resources remains unknown. [5]
It seems intuitive that the higher the frequency of vital sign measurement, the faster the chances of clinical deterioration are detected. There is variability between institutes within and across nations depending on the acuity of clinical condition, any active intervention carried out, the amount of staff availability, cost issues, organizational practices, and leadership styles. The weighted average score deduced from the vital sign measurements (i.e., an early warning score) is used to determine the timing of the next observation sets. [4] [5]
- Clinical Significance
Temperature
Body temperature is a variable, which is complex as well as nonlinear and is affected by many sources of internal and external variables. The normal body temperature for a healthy adult is approximately 98.6 degrees Fahrenheit/37.0 degrees centigrade. The human body temperature typically ranges from 36.5 to 37.5 degrees centigrade (97.7 to 99.5 degrees Fahrenheit. [6] Body temperature is regulated in the hypothalamus in a narrow thermodynamic range and maintained to optimize the synaptic transmission of biochemical reactions. [7]
Clinical decisions, especially in the pediatric population regarding the investigation and management, are based on the results of temperature measurement alone. Whereas at one end, missing that the patient's fever is severe or detecting a falsely positive fever reading can cause the patient to receive wrongful management. Galileo was the first scientist to uncover the concept of thermometers that began in the 16th century. In the year, 1709 Daniel Fahrenheit developed an alcohol-filled thermometer as well as a mercury-filled thermometer. [8]
Health care providers use the axillary, rectal, oral, and tympanic membrane most commonly to record body temperature, and the devices most commonly used are the electronic and infrared thermometers. They can monitor temperature at different sites, and each site has its range as well as advantages and disadvantages. As clinicians, the understanding of these site-specific differences is crucial. For example, the oral temperature, which is the most commonly used method, is considered very convenient and reliable. Here we place the thermometer under the tongue and close the lips around it. The posterior sublingual pocket is the area that gives the highest reliability. The other commonly used methods are tympanic temperature, where the thermometer where we insert the thermometer into the ear canal, and the axillary temperature where we place the thermometer in the axilla while adducting the arm of the patient. Both these sites are convenient but generally considered less accurate and hence not recommended. [8]
For measuring the rectal temperature, the thermometer is inserted through the anus into the rectum after applying a lubricant. This method is very inconvenient, but since it measures the internal measurement, it is very reliable. It is usually considered the "gold standard" method of recording temperature. Gut temperature, measured with an ingested pill, also gives readings close to the rectal temperature. Besides the site, the time of day is an essential factor leading to variability in the temperature record, secondary to the circadian rhythm. The inability to consider this physiological diurnal variation of temperature can lead to the wrong conclusion that an individual's temperature suggests a disease state when it is a normal temperature at that time of day. There is also a variation of the body temperature in a regularly cycling female, referred to as the "circamensal" rhythm. Understanding of this rhythm is paramount in teaching patients, trying to conceive about the fertile period of the cycle. Besides the change with diurnal variation and menstrual variation, a person's relative physical fitness and age can affect the degree of temperature change during a day. Studies show that younger patients and fitter record larger temperature amplitudes, while older and less fit people record lesser amplitude changes. [9] Some studies have demonstrated a seasonal variation in body temperature; we need more research in this regard to reach a definitive conclusion. [9]
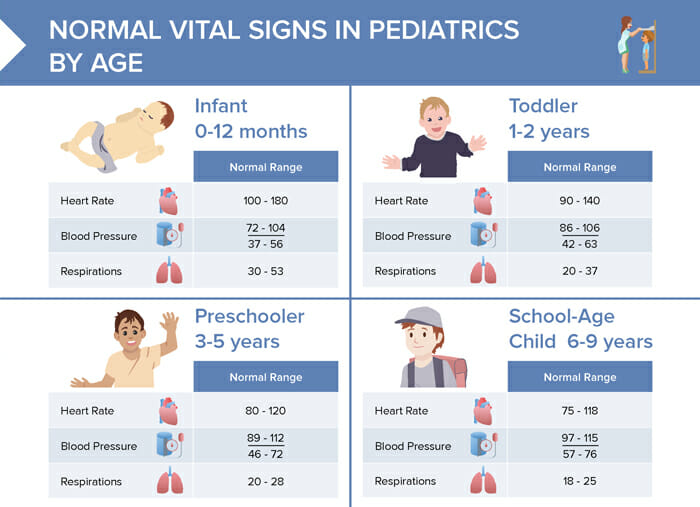
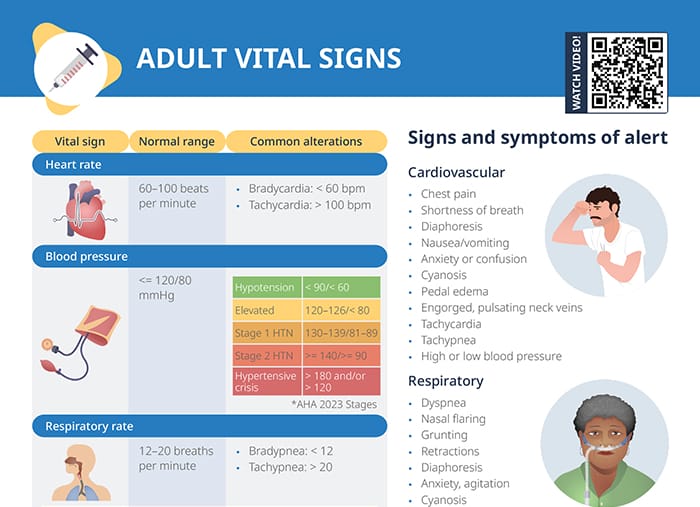
The most common sites of measuring the peripheral pulses are the radial pulse, ulnar pulse, brachial pulse in the upper extremity, and the posterior tibialis or the dorsalis pedis pulse as well as the femoral pulse in the lower extremity. Clinicians measure the carotid pulse in the neck. In day-to-day practice, the radial pulse is the most frequently used site for checking the peripheral pulse, where the pulse is palpated on the radial aspect of the forearm, just proximal to the wrist joint. Parameters for assessment of pulse include its rate, rhythm, volume, amplitude, and rate of increase, besides its symmetry The rate of the pulse is significant to measure for assessing the physiological and pathological processes affecting the body. The normal range used in an adult is between 60 to 100 beats/minute with rates above 100 beats/minute and rates below 60 beats per minute, referred to as tachycardia and bradycardia, respectively. The age-specific heart rate given for the pediatric age range appears in table -2.
Assessing whether the rhythm of the pulse is regular or irregular is essential. The pulse could be regular, irregular, or irregularly irregular. Changes in the rate of the pulse, along with changes in respiration are called sinus arrhythmia. In sinus arrhythmia, the pulse rate becomes faster during inspiration and slows down during expiration. Irregularly irregular pattern is more commonly indicative of processes like atrial flutter or atrial fibrillation. We should also be checking for the radial and the femoral pulse simultaneously. If there is any delay between the pulses, it could indicate conditions like the coarctation of the aorta. Assessing the volume of the pulse is equally essential. A low volume pulse could be indicative of inadequate tissue perfusion; this can be a crucial indicator of indirect prediction of the systolic blood pressure of the patient. If we can palpate the radial pulse, the systolic blood pressure is generally more than 80 mmHg. If we can palpate the femoral pulse, the systolic blood pressure is more than 70 mmHg, and if we can palpate the carotid pulse, the systolic blood pressure is more than 60 mmHg. [10] Checking for symmetry of the pulses is important as asymmetrical pulses could be seen in conditions like aortic dissection, aortic coarctation, Takayasu arteritis, and subclavian steal syndrome. Besides the above-stated parameters, amplitude and rate of increase is also an important consideration. Low amplitude and low rate of increase could be seen in conditions like aortic stenosis, besides weak perfusion states. High amplitude and rapid rise can be indicative of conditions like aortic regurgitation, mitral regurgitation, and hypertrophic cardiomyopathy.
Respiratory Rate
The respiratory rate is the number of breaths per minute. The normal breathing rate is about 12 to 20 breaths per minute in an average adult. In the pediatric age group, it is defined by the particular age group. Parameters important here again include rate, depth of breathing, and pattern of breathing. Rates higher or lower than expected are termed as tachypnea and bradypnea, respectively. Tachypnea is described as a respiratory rate of more than 20 breaths per minute that could occur in physiological conditions like exercise, emotional changes, or pregnancy. Pathological conditions like pain, pneumonia, pulmonary embolism, asthma, foreign body aspiration, anxiety conditions, sepsis, carbon monoxide poisoning, and diabetic ketoacidosis can also present with tachypnea. Bradypnea described as ventilation less than 12 breaths per minute can be seen due to worsening of any underlying respiratory condition leading to respiratory failure or due to usage of central nervous system depressants like alcohol, narcotics, benzodiazepines, or metabolic derangements. Apnea is the complete cessation of airflow to the lungs for a total of 15 seconds. It appears in cardiopulmonary arrests, airway obstructions, the overdose of narcotics, and benzodiazepines.
The depth of breathing is also a crucial parameter. Hyperpnea is described as an increased depth of breathing and is seen during exercise and in anxiety states, lung infections, and congestive heart failure. Hyperventilation, on the other hand, is described as both increased in the rate and depth of breathing and can again be seen in anxiety states like anxiety or due to exercise but is also seen in pathological conditions like diabetic ketoacidosis or lactic acidosis. The term hypoventilation describes the decreased rate and depth of ventilation. This condition results from excessive sedation, metabolic alkalosis, and in instances of obesity hypoventilation syndrome.
The pattern of breathing also gets affected in various conditions and indicates the underlying pathology. Biot respiration is a condition where there are periods of increased rate and depth of breathing, followed by periods of no breathing or apnea. These can vary in length of time. This pattern is suggestive of raised intracranial pressure as in space-occupying lesions of the skull or conditions like meningitis. Cheyne-Stokes respiration is a peculiar pattern of breathing where there is an increase in the depth of ventilation followed by periods of no breathing or apnea. This presentation occurs in conditions of raised intracranial pressure but is also seen with excessive usage of sedatives and worsening congestive heart failure. Kussmaul breathing refers to the increased depth of ventilation, although the rate remains regular. This presentation is in patients with renal failure and diabetic ketoacidosis. Orthopnea refers to difficulty in respiration occurring on lying horizontal but gets better when the patient sits up or stands It is seen characteristically in congestive heart failure. Paradoxical ventilation refers to the inward movement of the abdominal or chest wall during inspiration, and outward movement during expiration, which is seen in cases of diaphragmatic paralysis, muscle fatigue, and trauma to the chest wall.
Blood Pressure
Blood pressure is an essential vital sign to comprehend the hemodynamic condition of the patient. Unfortunately, though, there are a lot of inter-person variabilities when measuring it. Many times, the basic measurement techniques are not followed and lead to erroneous results.
All healthcare providers should be aware of making sure all the essential pre-requisites are met before checking the blood pressure of the patient. The patient should not have taken any caffeinated drink at least one hour before the testing and should not have smoked any nicotine products at least 15 minutes before checking the pressure. They should have emptied their bladder before checking the blood pressure. Full bladder adds 10 mmHg to the pressure readings. It is advisable to have the patient be seated for at least five minutes before checking their blood pressure. This step takes care of or at least minimizes the higher readings that could have occurred secondary to rushing in for the clinic appointment. The providers should not be having a conversation with the patient while checking his blood pressure. Talking or active listening adds 10 mmHg to the pressure readings. The patient’s back and feet should be supported, and their legs should be uncrossed. Unsupported back and feet add 6 mmHg to the pressure readings. Crossed legs add 2 to 4 mmHg to the pressure readings. The arm should be supported at the heart level. Unsupported arm leads to 10 mmHg to the pressure readings. The patient’s blood pressure should get checked in each arm, and in younger patients, it should be tested in an upper and lower extremity to rule out the coarctation of the aorta. Using the correct cuff size is very important. Smaller cuff sizes give falsely high, and larger cuff sizes give a falsely lower blood pressure reading. [11]
- Nursing, Allied Health, and Interprofessional Team Interventions
Variability of Vital Signs in the Geriatric Age Group
Since vital signs are an indication of the changes in physiological processes, they tend to change with age. With age, core body temperature tends to be lower, and the ability of the body to change with different kinds of stressors becomes minimized. Even subtle variation from the core body temperature can be a significant finding as fever in an older patient often indicates a more severe infection and is associated with increased rates of life-threatening consequences. [12]
There can be a decrease in response to changes in the oxygen and carbon dioxide at the molecular level along with anatomical changes resulting due to stiffness of muscles and compliance of the chest wall. Respiratory rate sometimes might be the most neglected of the vital signs reported in hospitalized patients but is more sensitive than other vital signs in picking up a critically ill patient. [13]
The aging blood vessels also lead to higher arterial stiffness, leading to higher systolic blood pressure and increased pulse pressure. There is also the issue of orthostatic hypotension due to decreased autonomic responsiveness. This response becomes exaggerated with the use of polypharmacy and reduced fluid intake. Thus, it is imperative to check orthostatic vitals in this population. Resting heart rate, in contrast, is often observed to increase with age due to deconditioning and autonomic dysregulation. [14]
Limitations of Vital Signs
Accurately measuring vital signs is a clinical skill that needs time and practice to refine. A review of literature is abundant about the inter-observer variability observed and reported secondary to lack of this skill. Clinicians should be wary of this and always re-check the vital signs themselves if there is a profound or unexpected change. Clinics and organizations should continuously strive to check and educate their nursing and ancillary staff to sharpen these skills.
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
VItal Sign Tables Table 1: Types of Digital Thermometers for Use by Age 6 Table 2: Normal Heart Rate (beats/minute) as per the Pediatric Advanced Life Support (PALS) Guidelines. Table 3: Normal Respiratory Rate (Beats/Minute) as per the Pediatric Advanced (more...)
Vital Signs Table 5: Acceptable Blood Pressure Dimensions for Various arm sizes. Contributed by Amit Sapra, MD
Vital Signs Table 6: BP targets by different organizations Contributed by Amit Sapra, MD
Vital Signs Table 7: Normal Blood Pressure as per the Pediatric Advanced Life Support (PALS) Guidelines. Contributed by Amit Sapra, MD
Disclosure: Amit Sapra declares no relevant financial relationships with ineligible companies.
Disclosure: Ahmad Malik declares no relevant financial relationships with ineligible companies.
Disclosure: Priyanka Bhandari declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Sapra A, Malik A, Bhandari P. Vital Sign Assessment. [Updated 2023 May 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Suicidal Ideation. [StatPearls. 2024] Suicidal Ideation. Harmer B, Lee S, Duong TVH, Saadabadi A. StatPearls. 2024 Jan
- Review Technology Assessment: Early Sense for Monitoring Vital Signs in Hospitalized Patients [ 2016] Review Technology Assessment: Early Sense for Monitoring Vital Signs in Hospitalized Patients Helfand M, Christensen V, Anderson J. 2016 May
- Assessing sensitivity and specificity of the Manchester Triage System in the evaluation of acute coronary syndrome in adult patients in emergency care: a systematic review protocol. [JBI Database System Rev Implem...] Assessing sensitivity and specificity of the Manchester Triage System in the evaluation of acute coronary syndrome in adult patients in emergency care: a systematic review protocol. Nishi FA, de Motta Maia FO, de Lopes Monteiro da Cruz DA. JBI Database System Rev Implement Rep. 2015 Nov; 13(11):64-73.
- The prevalence and diagnostic utility of systemic inflammatory response syndrome vital signs in a pediatric emergency department. [Acad Emerg Med. 2015] The prevalence and diagnostic utility of systemic inflammatory response syndrome vital signs in a pediatric emergency department. Scott HF, Deakyne SJ, Woods JM, Bajaj L. Acad Emerg Med. 2015 Apr; 22(4):381-9. Epub 2015 Mar 16.
- Review Nursing handover of vital signs at the transition of care from the emergency department to the inpatient ward: An integrative review. [J Clin Nurs. 2019] Review Nursing handover of vital signs at the transition of care from the emergency department to the inpatient ward: An integrative review. Cross R, Considine J, Currey J. J Clin Nurs. 2019 Mar; 28(5-6):1010-1021. Epub 2018 Oct 23.
Recent Activity
- Vital Sign Assessment - StatPearls Vital Sign Assessment - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers

- school Campus Bookshelves
- menu_book Bookshelves
- perm_media Learning Objects
- login Login
- how_to_reg Request Instructor Account
- hub Instructor Commons
- Download Page (PDF)
- Download Full Book (PDF)
- Periodic Table
- Physics Constants
- Scientific Calculator
- Reference & Cite
- Tools expand_more
- Readability
selected template will load here
This action is not available.

1.3: Vital Signs
- Last updated
- Save as PDF
- Page ID 44497

- Ernstmeyer & Christman (Eds.)
- Chippewa Valley Technical College via OpenRN
Vital signs are typically obtained prior to performing a physical assessment. Vital signs include temperature recorded in Celsius or Fahrenheit, pulse, respiratory rate, blood pressure, and oxygen saturation using a pulse oximeter. See Figure \(\PageIndex{1}\) [1] for an image of a nurse obtaining vital signs. Obtaining vital signs may be delegated to unlicensed assistive personnel (UAP) for stable patients, depending on the state’s nurse practice act, agency policy, and appropriate training. However, the nurse is always accountable for analyzing the vital signs and instituting appropriate follow-up for out-of-range findings. See Appendix A to review a checklist for obtaining vital signs.

The order of obtaining vital signs is based on the patient and their situation. Health care professionals often place the pulse oximeter probe on the patient while proceeding to obtain their pulse, respirations, blood pressure, and temperature. However, in some situations this order is modified based on the urgency of their condition. For example, if a person loses consciousness, the assessment begins with checking their carotid pulse to determine if cardiopulmonary resuscitation (CPR) is required. [2]
Temperature
Accurate temperature measurements provide information about a patient’s health status and guide clinical decisions. Methods of measuring body temperature vary based on the patient’s developmental age, cognitive functioning, level of consciousness, and health status, as well as agency policy. Common methods of temperature measurement include oral, tympanic, axillary, and rectal routes. It is important to document the route used to obtain a patient’s temperature because of normal variations in temperature in different locations of the body. Body temperature is typically measured and documented in health care agencies in degrees Celsius (ºC). [3]
Oral Temperature
Normal oral temperature is 35.8 – 37.3ºC (96.4 – 99.1ºF). An oral thermometer is shown in Figure \(\PageIndex{2}\). [4] The device has blue coloring, indicating it is an oral or axillary thermometer, as opposed to a rectal thermometer that has red coloring. Oral temperature is reliable when it is obtained close to the sublingual artery. [5]

Remove the probe from the device and slide a probe cover (from the attached box) onto the oral thermometer without touching the probe cover with your hands. Place the thermometer in the posterior sublingual pocket under the tongue, slightly off-center. Instruct the patient to keep their mouth closed but not bite on the thermometer. Leave the thermometer in place for as long as is indicated by the device manufacturer. The thermometer typically beeps within a few seconds when the temperature has been taken. Read the digital display of the results. Discard the probe cover in the garbage (without touching the cover) and place the probe back into the device. [6] See Figure \(\PageIndex{3}\) [7] of an oral temperature being taken.

Some factors can cause an inaccurate measurement using the oral route. For example, if the patient recently consumed a hot or cold food or beverage, chewed gum, or smoked prior to measurement, a falsely elevated or decreased reading may be obtained. Oral temperature should be taken 15 to 25 minutes following consumption of a hot or cold beverage or food or 5 minutes after chewing gum or smoking. [8]
Tympanic Temperature
The tympanic temperature is typically 0.3 – 0.6°C higher than an oral temperature. It is an accurate measurement because the tympanic membrane shares the same vascular artery that perfuses the hypothalamus (the part of the brain that regulates the body’s temperature). See Figure \(\PageIndex{4}\) [9] of a tympanic thermometer. The tympanic method should not be used if the patient has a suspected ear infection. [10]

Remove the tympanic thermometer from its holder and place a probe cover on the thermometer tip without touching the probe cover with your hands. Turn the device on. Ask the patient to keep their head still. For an adult or older child, gently pull the helix (outer ear) up and back to visualize the ear canal. For an infant or child under age 3, gently pull the helix down. Insert the probe just inside the ear canal but never force the thermometer into the ear. The device will beep within a few seconds after the temperature is measured. Read the results displayed, discard the probe cover in the garbage (without touching the cover), and then place the device back into the holder. [11] See Figure \(\PageIndex{5}\) [12] for an image of a tympanic temperature being taken.

Axillary Temperature
The axillary method is a minimally invasive way to measure temperature and is commonly used in children. It uses the same electronic device as an oral thermometer (with blue coloring). However, the axillary temperature can be as much as 1ºC lower than the oral temperature. [13]
Remove the probe from the device and place a probe cover (from the attached box) on the thermometer without touching the cover with your hands. Ask the patient to raise their arm and place the thermometer probe in their armpit on bare skin as high up into the axilla as possible. The probe should be facing behind the patient. Ask the patient to lower their arm and leave the device in place until it beeps, usually about 10–20 seconds. Read the displayed results, discard the probe cover in the garbage (without touching the cover), and then place the probe back into the device. See Figure \(\PageIndex{6}\) [14] for an image of an axillary temperature. [15]

Rectal Temperature
Measuring rectal temperature is an invasive method. Some sources suggest its use only when other methods are not appropriate. However, when measuring infant temperature, it is considered a gold standard because of its accuracy. The rectal temperature is usually 1ºC higher than oral temperature. A rectal thermometer has red coloring to distinguish it from an oral/axillary thermometer. [16] See Figure \(\PageIndex{7}\) [17] for an image of a rectal thermometer.

Before taking a rectal temperature, ensure the patient’s privacy. Wash your hands and put on gloves. For infants, place them in a supine position and raise their legs upwards toward their chest. Parents may be encouraged to hold the infant to decrease movement and provide a sense of safety. When taking a rectal temperature in older children and adults, assist them into a side lying position and explain the procedure. Remove the probe from the device and place a probe cover (from the attached box) on the thermometer. Lubricate the cover with a water-based lubricant, and then gently insert the probe 2–3 cm inside the anus or less, depending on the patient’s size. [18] Remove the probe when the device beeps. Read the result and then discard the probe cover in the trash can without touching it. Cleanse the device as indicated by agency policy. Remove gloves and perform hand hygiene.
See Table \(\PageIndex{1}\) for normal temperature ranges for various routes.
Query \(\PageIndex{1}\)
Pulse refers to the pressure wave that expands and recoils arteries when the left ventricle of the heart contracts. It is palpated at many points throughout the body. The most common locations to assess pulses as part of vital sign measurement include radial, brachial, carotid, and apical areas as indicated in Figure \(\PageIndex{8}\). [20]

Pulse is measured in beats per minute. The normal adult pulse rate (heart rate) at rest is 60–100 beats per minute with different ranges according to age. See Table \(\PageIndex{2}\) for normal heart rate ranges by age. It is important to consider each patient situation when analyzing if their heart rate is within normal range. Begin by reviewing their documented baseline heart rate. Consider other factors if the pulse is elevated, such as the presence of pain or crying in an infant. It is best to document the assessment when a patient is resting and comfortable, but if this is not feasible, document the circumstances surrounding the assessment and reassess as needed. [21]
Pulse Characteristics
When assessing pulses, the characteristics of rhythm, rate, force, and equality are included in the documentation.
Pulse Rhythm
A normal pulse has a regular rhythm, meaning the frequency of the pulsation felt by your fingers is an even tempo with equal intervals between pulsations. For example, if you compare the palpation of pulses to listening to music, it follows a constant beat at the same tempo that does not speed up or slow down. Some cardiovascular conditions, such as atrial fibrillation, cause an irregular heart rhythm. If a pulse has an irregular rhythm, document if it is “regularly irregular” (e.g., three regular beats are followed by one missed and this pattern is repeated) or if it is “irregularly irregular” (e.g., there is no rhythm to the irregularity). [22]
The pulse rate is counted with the first beat felt by your fingers as “One.” It is considered best practice to assess a patient’s pulse for a full 60 seconds, especially if there is an irregularity to the rhythm. [23]
Pulse Force
The pulse force is the strength of the pulsation felt on palpation. Pulse force can range from absent to bounding. The volume of blood, the heart’s functioning, and the arteries’ elastic properties affect a person’s pulse force. [24] Pulse force is documented using a four-point scale:
- 3+: Full, bounding
- 2+: Normal/strong
- 1+: Weak, diminished, thready
- 0: Absent/nonpalpable
If a pulse is absent, a Doppler ultrasound device is typically used to verify perfusion of the limbs. The Doppler is a handheld device that allows the examiner to hear the whooshing sound of the pulse. This device is also commonly used when assessing peripheral pulses in the lower extremities, such as the dorsalis pedis pulse or the posterior tibial pulse. See the following hyperlink to a video demonstrating the use of a Doppler device.
Video Review of Using a Doppler Ultrasound Device to Assess a Pulse [25] : Doppler Device – How to
Pulse Equality
Pulse equality refers to a comparison of the pulse forces on both sides of the body. For example, a nurse often palpates the radial pulse on a patient’s right and left wrists at the same time and compares if the pulse forces are equal. However, the carotid pulses should never be palpated at the same time because this can decrease blood flow to the brain. Pulse equality provides data about medical conditions such as peripheral vascular disease and arterial obstruction. [26]
Radial Pulse
Use the pads of your first three fingers to gently palpate the radial pulse. The pads of the fingers are placed along the radius bone on the lateral side of the wrist (i.e., the thumb side). Fingertips are placed close to the flexor aspect of the wrist (i.e., where the wrist meets the hand and bends). See Figure \(\PageIndex{9}\) [27] for correct placement of fingers in obtaining a radial pulse. Press down with your fingers until you can feel the pulsation, but not so forcefully that you are obliterating the wave of the force passing through the artery. Note that radial pulses are difficult to palpate on newborns and children under the age of five, so the brachial or apical pulses are typically obtained in this population. [28]

Carotid Pulse
The carotid pulse is typically palpated during medical emergencies because it is the last pulse to disappear when the heart is not pumping an adequate amount of blood. [29]
Locate the carotid artery medial to the sternomastoid muscle, between the muscle and the trachea, in the middle third of the neck. With the pads of your three fingers, gently palpate one carotid artery at a time so as not to compromise blood flow to the brain. See Figure \(\PageIndex{10}\) [30] for correct placement of fingers in a seated patient. [31]

Brachial Pulse
A brachial pulse is typically assessed in infants and children because it can be difficult to feel the radial pulse in these populations. If needed, a Doppler ultrasound device can be used to obtain the pulse.
The brachial pulse is located by feeling the bicep tendon in the area of the antecubital fossa. Move the pads of your three fingers medially from the tendon about 1 inch (2 cm) just above the antecubital fossa. It can be helpful to hyperextend the patient’s arm to accentuate the brachial pulse so that you can better feel it. You may need to move your fingers around slightly to locate the best place to accurately feel the pulse. You typically need to press fairly firmly to palpate the brachial pulse. [32] See Figure \(\PageIndex{11}\) [33] for correct placement of fingers along the brachial artery.

Apical Pulse
The apical pulse rate is considered the most accurate pulse and is indicated when obtaining assessments prior to administering cardiac medications. It is obtained by listening with a stethoscope over a specific position on the patient’s chest wall. Read more about listening to the apical pulse and other heart sounds in the “ Cardiovascular Assessment ” chapter.
Query \(\PageIndex{2}\)
Respiratory Rate
Respiration refers to a person’s breathing and the movement of air into and out of the lungs. Inspiration refers to the process causing air to enter the lungs, and expiration refers to the process causing air to leave the lungs. A respiratory cycle (i.e., one breath while measuring respiratory rate) is one sequence of inspiration and expiration. [34]
When obtaining a respiratory rate, the respirations are also assessed for quality, rhythm, and rate. The quality of a person’s breathing is normally relaxed and silent. However, loud breathing, nasal flaring, or the use of accessory muscles in the neck, chest, or intercostal spaces indicate respiratory distress. People experiencing respiratory distress also often move into a tripod position, meaning they are leaning forward and placing their arms or elbows on their knees or on a bedside table. If a patient is demonstrating new signs of respiratory distress as you are obtaining their vital signs, it is vital to immediately notify the health care provider or follow agency protocol.
Respirations normally have a regular rhythm in children and adults who are awake. A regular rhythm means that the frequency of the respiration follows an even tempo with equal intervals between each respiration. However, newborns and infants commonly exhibit an irregular respiratory rhythm.
Normal respiratory rates vary based on age. The normal resting respiratory rate for adults is 10–20 breaths per minute, whereas infants younger than one year old normally have a respiratory rate of 30–60 breaths per minute. See Table \(\PageIndex{3}\) for ranges of normal respiratory rates by age. It is also important to consider factors such as sleep cycle, presence of pain, and crying when assessing a patient’s respiratory rate. [35]
Read more about assessing a patient’s respiratory status in the “ Respiratory Assessment ” chapter.
Oxygen Saturation
A patient’s oxygenation status is routinely assessed using pulse oximetry, referred to as SpO2. SpO2 is an estimated oxygenation level based on the saturation of hemoglobin measured by a pulse oximeter. Because the majority of oxygen carried in the blood is attached to hemoglobin within the red blood cells, SpO2 estimates how much hemoglobin is “saturated” with oxygen. The target range of SpO2 for an adult is 94-98%. For patients with chronic respiratory conditions, such as chronic obstructive pulmonary disease (COPD), the target range for SpO2 is often lower at 88% to 92%. Although SpO2 is an efficient, noninvasive method to assess a patient’s oxygenation status, it is an estimate and not always accurate. For example, if a patient is severely anemic and has a decreased level of hemoglobin in the blood, the SpO2 reading is affected. Decreased peripheral circulation can also cause a misleading low SpO2 level.
A pulse oximeter includes a sensor that measures light absorption of hemoglobin. See Figure \(\PageIndex{12}\) [37] for an image of a pulse oximeter. The sensor can be attached to the patient using a variety of devices. For intermittent measurement of oxygen saturation, a spring-loaded clip is attached to a patient’s finger or toe. However, this clip is too large for use on newborns and young children; therefore, for this population, the sensor is typically taped to a finger or toe. An earlobe clip is another alternative for patients who cannot tolerate the finger or toe clip or have a condition, such as vasoconstriction and poor peripheral perfusion, that could affect the results.

The target range of SpO2 for an adult is 94-98%. For patients with chronic respiratory conditions, such as chronic obstructive pulmonary disease (COPD), the target range for SpO2 is often lower at 88% to 92%.
Read more about pulse oximetry in the “ Oxygen Therapy ” chapter.
Nail polish or artificial nails can affect the absorption of light waves from the pulse oximeter and decrease the accuracy of the SpO2 measurement when using a probe clipped on the finger. An alternative sensor that does not use the finger should be used for these patients or the nail polish should be removed. If a patient’s hands or feet are cold, it is helpful to clip the sensor to the earlobe or tape it to the forehead.
Blood Pressure
Read information about how to accurately obtain blood pressure measurement in the “ Blood Pressure ” chapter.
Interpreting Results
After obtaining a patient’s vital signs, it is important to immediately analyze the results, recognize deviations from expected normal ranges, and report deviations appropriately. As a nursing student, it is vital to immediately notify your instructor and/or collaborating nurse caring for the patient of any vital sign measurement out of normal range.
- “ US Navy 110714-N-RM525-060 Hospitalman Seckisiesha Isaac, from New York, prepares to take a woman's temperature at a pre-screening vital signs stat.jpg ” by U.S. Navy photo by Mass Communication Specialist 2nd Class Jonathen E. Davis is licensed under CC0 ↵
- Vital Sign Measurement Across the Lifespan by Ryerson University is licensed under CC BY-SA 4.0 ↵
- “Thermometer-oral-768x548.jpg” by British Columbia Institute of Technology is licensed under CC BY 4.0 . Access for free at med.libretexts.org/Bookshelves/Nursing/Book%3A_Vital_Sign_Measurement_Across_the_Lifespan_(Lapum_et_al.)/02%3A_Temperature/2.17%3A_Oral_Temperature↵
- “Oral-Temperature-Wide-768x512.jpg" by British Columbia Institute of Technology is licensed under CC BY 4.0 . Access for free at med.libretexts.org/Bookshelves/Nursing/Book%3A_Vital_Sign_Measurement_Across_the_Lifespan_(Lapum_et_al.)/02%3A_Temperature/2.17%3A_Oral_Temperature↵
- Vital Sign Measurement Across the Lifespan by Ryerson University is licensed under CC BY-SA 4.0 . ↵
- “Tympanic-Thermometer.jpg” by British Columbia Institute of Technology is licensed under CC BY 4.0 . Access for free at med.libretexts.org/Bookshelves/Nursing/Book%3A_Vital_Sign_Measurement_Across_the_Lifespan_(Lapum_et_al.)/02%3A_Temperature/2.18%3A_Tympanic_Temperature↵
- “Tympanic-Temperature-Correct-2.jpg” by British Columbia Institute of Technology is licensed under CC BY 4.0 . Access for free at med.libretexts.org/Bookshelves/Nursing/Book%3A_Vital_Sign_Measurement_Across_the_Lifespan_(Lapum_et_al.)/02%3A_Temperature/2.18%3A_Tympanic_Temperature↵
- “Axilla-Temperature-1-768x596.jpg” by British Columbia Institute of Technology is licensed under CC BY 4.0 . Access for free at med.libretexts.org/Bookshelves/Nursing/Book%3A_Vital_Sign_Measurement_Across_the_Lifespan_(Lapum_et_al.)/02%3A_Temperature/2.19%3A_Axillary_Temperature↵
- “Thermometer-rectal-768x479.jpg” by British Columbia Institute of Technology is licensed under CC BY 4.0 . Access for free at med.libretexts.org/Bookshelves/Nursing/Book%3A_Vital_Sign_Measurement_Across_the_Lifespan_(Lapum_et_al.)/02%3A_Temperature/2.20%3A_Rectal_Temperature↵
- Vital Sign Measurement Across the Lifespan by Ryerson University is licensed under CC BY-SA 4.0↵
- “Radial-brachial-carotid-and-apical-pulse-final-930x1024.jpg” by British Columbia Institute of Technology is licensed under CC BY 4.0 . Access for free at med.libretexts.org/Bookshelves/Nursing/Book%3A_Vital_Sign_Measurement_Across_the_Lifespan_(Lapum_et_al.)/03%3A_Pulse_and_Respiration/3.15%3A_What_is_Pulse%3F↵
- Ryerson University. (2018, March 21). Doppler device - How to. [Video]. YouTube. All rights reserved. https://youtu.be/cn3aA0G1mgc ↵
- “Radial-pulse-correct.jpg” by British Columbia Institute of Technology is licensed under CC BY 4.0 . Access for free at med.libretexts.org/Bookshelves/Nursing/Book%3A_Vital_Sign_Measurement_Across_the_Lifespan_(Lapum_et_al.)/03%3A_Pulse_and_Respiration/3.18%3A_Radial_Pulse↵
- “Carotid-pulse-768x511.jpg” by British Columbia Institute of Technology is licensed under CC BY 4.0 . Access for free at med.libretexts.org/Bookshelves/Nursing/Book%3A_Vital_Sign_Measurement_Across_the_Lifespan_(Lapum_et_al.)/03%3A_Pulse_and_Respiration/3.19%3A_Carotid_Pulse↵
- “Brachial-pulse.jpg” by British Columbia Institute of Technology is licensed under CC BY 4.0 . Access for free at med.libretexts.org/Bookshelves/Nursing/Book%3A_Vital_Sign_Measurement_Across_the_Lifespan_(Lapum_et_al.)/03%3A_Pulse_and_Respiration/3.20%3A_Brachial_Pulse↵
- “02-Sat-Apparatus-1-1-1024x682.jpg” by British Columbia Institute of Technology is licensed under CC BY 4.0 . Access for free at med.libretexts.org/Bookshelves/Nursing/Book%3A_Vital_Sign_Measurement_Across_the_Lifespan_(Lapum_et_al.)/04%3A_Oxygen_Saturation/4.09%3A_How_is_Oxygen_Saturation_Measured%3F↵
Lecturio Nursing
Cheat Sheets
Nursing Knowledge
Normal Vital Signs
Table of contents, what are vital signs .
Vital signs are measurements of the body’s basic functions. Usually, they include:
- Heart rate (pulse)
- Blood pressure
- Respiratory rate
- Oxygen saturation
- Temperature
What is the purpose of vital signs in nursing?
Monitoring clients’ vital signs is a fundamental part of continuously evaluating their physical health. Changes in vital signs can give information about and indicate various changes in a client’s condition and guide the decisions about nursing interventions.
How to take vital signs
- Heart rate: place fingers over pulse point (radial artery), count beats for 30 seconds and double for beats per minute; or apical pulse with the stethoscope for 60 seconds
- Blood pressure: measured with blood pressure cuff and stethoscope
- Respiratory rate: observe the patient’s chest/breath without their awareness to avoid unnatural rates due to self-awareness
- Oxygen saturation: pulse oximeter
- Temperature: orally, rectally, axillary, or tympanic /temporal
When to take vital signs
Vital signs are taken frequently in clinical settings, for example:
- On admission
- In routine checkups
- Before and after surgeries, procedures, medications
- To monitor critical changes in emergency situations
- Based on symptom changes (e.g., patient feeling faint)
What is a normal heart rate?
The normal range for a resting heart rate is between 60 and 100 beats per minute.
Common alterations include:
- Bradycardia , defined as less than 60 beats per minute
- Tachycardia , defined as more than 100 beats per minute
What is the normal range for blood pressure?
Ideal blood pressure values are less or equal to 120/80.
Hypotension is noted with findings < 90/< 60 . Blood pressure that is too high is classified b the AHA 2023 stages as follows:
- 120–126/< 80: elevated blood pressure
- 120–126/82–89: stage 1 hypertension
- >= 140/ >= 90: stage 2 hypertension
- > 180 and/or > 120: hypertensive crisis
What is a normal respiratory rate?
A healthy adult with a normal respiratory rate will take between 12 and 20 breaths per minute.
- Bradypnea, less than 12 breaths per minute
- Tachypnea, more than 20 breaths per minute
What is the ideal oxygen saturation?
Oxygen saturation should ideally be 95–100%. Oxygen saturation below 90% means the client is presenting with hypoxemia .
What is a normal temperature for an adult?
The ideal temperature for an adult depends on the mode of measuring:
- Oral: 98.6–99.5°F (37–37.5°C)
- Temporal: 98.4–99.3°F (36.8–37.4°C)
- Axillary: 97.7–99°F (36.5–37.2°C)
- Rectal: 97.8–100.4°F (36.6–38°C)
The body becomes hypothermic when the temperature falls below 95°F (35°C).
Fever is defined as follows:
- Oral: > 100°F/37.8°C
- Temporal/Tympanic: > 100.4°F/37.8°C
- Axillary: > 99°F/37.2°C
- Rectal: > 100.4°F/38°C
Warning signs and symptoms
When checking vital signs and evaluating a patient, there are signs and symptoms of alert to keep in mind that require further attention and intervention:
Cardiovascular signs of alert
- Shortness of breath
- Diaphoresis
- Nausea/vomiting
- Anxiety or confusion
- Pedal edema
- Engorged, pulsating neck veins
- Tachycardia
- High or low blood pressure
Respiratory signs of alert
- Nasal flaring
- Retractions
- Anxiety, agitation
- Tripod position
- Low blood pressure
- Abnormal lung sounds
Neurological signs of alert
- Severe headache
- Altered vision
- Dizziness, loss of balance
- Loss of coordination
- Slurred speech
- Confusion/disorientation
- Memory loss
- Generalized or one-sided muscle weakness
- Loss of consciousness
RELATED TOPIC:
Normal Pediatric Vital Signs
FREE CHEAT SHEET
Free Download
Nursing Cheat Sheet
Master the topic with a unique study combination of a concise summary paired with video lectures.
- Data Privacy
- Terms and Conditions
- Legal Information
USMLE™ is a joint program of the Federation of State Medical Boards (FSMB®) and National Board of Medical Examiners (NBME®). MCAT is a registered trademark of the Association of American Medical Colleges (AAMC). NCLEX®, NCLEX-RN®, and NCLEX-PN® are registered trademarks of the National Council of State Boards of Nursing, Inc (NCSBN®). None of the trademark holders are endorsed by nor affiliated with Lecturio.
User Reviews
Get premium to test your knowledge.
Lecturio Premium gives you full access to all content & features
Get Premium to watch all videos
Verify your email now to get a free trial.
Create a free account to test your knowledge
Lecturio Premium gives you full access to all contents and features—including Lecturio’s Qbank with up-to-date board-style questions.
Vital Signs Chart
Better assess and evaluate your patient’s overall health with the help of the vital signs chart. Click here for a free template.

By Patricia Buenaventura on May 09, 2024.
Fact Checked by Nate Lacson.

What is a Vital Signs Chart?
A vital signs chart is a crucial medical document and resource designed to provide information and record fundamental physiological parameters that indicate the body's overall health. These essential signs, encompassing body temperature, pulse rate, respiration rate, and blood pressure, offer invaluable insights into an individual's well-being and aid healthcare professionals in assessing and monitoring health conditions.
To elaborate upon each parameter:
- Body temperature, which reflects the body's internal balance, is influenced by various factors such as activity levels, diet, and time of day.
- Pulse rate, denoting the heart's beats per minute, is a pivotal metric for cardiovascular health.
- Respiration rate, the pace of breathing, provides insights into respiratory function.
- Finally, blood pressure, though not strictly a vital sign, is often measured alongside the vital signs, offering information about the circulatory system.
The significance of a vital signs chart lies in its ability to assist in documenting these parameters over time, facilitating trend analysis, and aiding in identifying abnormalities during regular monitoring, whether in a medical facility, home setting, or during emergencies. Do note that the normal ranges for these signs vary based on factors such as age, BMI, sex, and overall health.
Accurate and comprehensive records, as written on a vital signs chart, play a pivotal role in diagnosing medical issues, tracking treatment efficacy, and ensuring timely interventions. By providing a standardized framework for documentation, these charts enhance communication among healthcare professionals, contributing to a holistic approach to patient care.
Printable Vital Signs Chart
Download this Vital Signs Chart to assess and evaluate your patient’s overall health.
How does it work?
Step 1. acquire the template.
For your convenience, access and download a valuable resource, such as the vital signs chart. Accomplish this task by either:
- Clicking the "Download Template" or "Use Template" button.
- Alternatively, locate the chart within Carepatron's template library on the app or website by searching for "Vital Signs Chart."
Step 2. Input essential details
If you want to use the chart beyond a visual aid for patient education, you should input critical patient information, including temperature, blood pressure, pulse, and respiratory rate.
Step 3. Analyze and interpret
Feel free to leverage the chart to compare the patient’s vital signs with established normal ranges and request additional diagnostic tests if they’re showing symptoms of an underlying issue and their test results don’t fall within the normal range.
Step 4. Secure the template copy
After consultation, you must safeguard the template and limit access to relevant parties exclusively.
For digital copies, we recommend utilizing Carepatron, a healthcare software that can safeguard electronic patient records because of compliance with global security standards, ensuring the protection of all medical records.

Vital Signs Chart example (sample)
Within this resource, we have crafted a PDF file that is accessible for both printing and digital use, featuring a completed template. Whether you seek guidance on utilizing these templates to evaluate and interpret your patient's results or teach them about managing their overall health when monitoring at home, you are encouraged to review, print, or save a copy. It's crucial to bear in mind that the details presented in this illustration are entirely fictional.
Furthermore, the approach demonstrated in utilizing this chart is just one of several potential methods to enhance its effectiveness. We suggest adapting it to meet your specific needs aligning it with data obtained from laboratory tests. You can examine the sample provided below or utilize the "Download Example PDF" button to acquire and print a copy for your reference.
Download this Vital Signs Chart example:

When would you use this chart?
The vital signs chart is a fundamental tool in healthcare, employed in various scenarios to assess and monitor an individual's health status. Here’s a list of some of them:
Admission process or home care visits
During the initial encounter, such as the admission process or home care visits, vital signs are measured and recorded on the chart to establish the client's baseline. This baseline serves as a reference point for future comparisons, aiding healthcare professionals in tracking changes over time.
Regular monitoring
Regular monitoring, commonly done during scheduled medical visits , is a standard practice, with vital signs typically measured every shift. This consistent assessment ensures the ongoing evaluation of an individual's physiological well-being. Additionally, vital signs are crucially measured after specific incidents, such as a fall, providing immediate insights into the potential impact on the individual's health.
Signs of impaired consciousness
The chart is especially utilized when there is a noticeable change in the client's status, such as a decreased level of consciousness. This allows for prompt identification of alterations in health conditions, facilitating timely interventions and adjustments to the treatment plan.
Symptoms of an underlying issue
The vital signs chart becomes instrumental when a client reports physical distress, indicating symptoms like dizziness or feeling cold. These reported symptoms prompt healthcare professionals to assess vital signs to identify underlying issues and determine the appropriate course of action.
What do the results mean?
Interpreting the results on a vital signs chart is crucial for understanding an individual's basic physiological functions and identifying potential health concerns. Here are some of the general interpretations you can write in your clinical notes when analyzing or interpreting:
Body temperature
Firstly, body temperature, though influenced by various factors such as gender, recent activity, and the menstrual cycle, has a normal range of 97.8 to 99 degrees Fahrenheit or 36.6 or 37 degrees Celsius for a healthy adult. A fever is indicated when the body temperature rises one degree or more above the standard, while hypothermia is defined by a drop below 95 degrees Fahrenheit or 35 degrees Celsius.
Pulse rate, representing the heart's beats per minute, and respiration rate, indicating the pace of breathing, are integral components of vital signs. Deviations from normal ranges in these parameters can indicate underlying pathologies, medication effects, or environmental influences.
Blood pressure
Similarly, blood pressure, though not strictly a vital sign, is often measured alongside them. Abnormal blood pressure readings may signify potential health issues and warrant further investigation.
Respiratory rate
The typical respiratory rate for adults in good health ranges from 12 to 20 breaths per minute1. Deviations below 12 or above 20 breaths per minute may indicate an irregularity in the standard respiratory processes.
Several factors could contribute to this variation when observing an abnormal respiratory rate. Conditions such as anxiety, fever, or cardiac issues may result in an accelerated breathing rate. Notably, an adult exhibiting a respiratory rate exceeding 20 breaths per minute indicates a potential illness, and a respiratory rate surpassing 24 breaths per minute suggests a critical state of health.
Commonly asked questions
Vital signs charts are used by multiple medical professionals like nurses, doctors, and specialists in different healthcare settings.
Vital signs charts are used during appointments, consultations, and when identifying underlying issues a patient may have especially if they exhibit symptoms of a particular disease or condition.
Vital Signs charts can be used in different ways. Some of them are educational resources, guides, references, and documents to record patient results.
Related Templates
Nursing Vital Signs Chart
Optimize patient care with our Nursing Vital Signs Chart. Track and analyze crucial health indicators for informed healthcare decisions.
Abnormal Vital Signs Chart
Detect health issues early with the Abnormal Vital Signs Chart. Download the PDF for proactive monitoring and better healthcare outcomes now!
Normal Vital Signs Chart
Enhance patient care with the Normal Vital Signs Chart, with an Abnormal Vital Signs Chart bonus, offering insights into various health issues.
EMT Vital Signs Chart
You can quickly refer to an EMT Vital Signs Chart when evaluating your patients during emergencies. Click here for a downloadable template copy!
Popular Templates
Barlow Test
Discover the Barlow Test for early detection of hip dysplasia in infants, with detailed explanations on procedures, benefits, and how to use our comprehensive template.
Elbow Valgus Stress Test
Discover how to perform the Elbow Valgus Stress Test. Get a free PDF template and example in this guide to help you learn more about this stress assessment.
Patient Registration Process Flowchart
Streamline your patient registration with our easy-to-follow flowchart template, designed for healthcare professionals to enhance efficiency and patient care.
Fever Nursing Care Plan
Carepatron's free PDF download provides a template for nursing care planning. It helps you understand the nursing diagnoses associated with fever and how to provide adequate care for patients.
Migraine Treatment Guidelines
Learn effective Migraine Treatment Guidelines to relieve debilitating headaches and improve your quality of life.
Thigh Thrust Test
Learn about the Thigh Thrust Test, a diagnostic tool in healthcare to assess hip joint pathology and potential causes of hip pain.
Balance Exercises for Seniors
Improve your balance and stability with these effective balance exercises for seniors. Download Carepatron's free PDF with examples and enhance your overall well-being today.
Nursing Diagnosis for Pneumonia
Explore our comprehensive guide on nursing diagnoses for pneumonia, including symptoms, treatments, and how our free template can enhance patient care.
Disturbed Thought Process Nursing Care Plan
Explore our detailed guide and free downloadable template for a Disturbed Thought Process Nursing Care Plan, including diagnosis, interventions, and nursing software solutions. Perfect for healthcare professionals.
Coaching Report Template
Explore our comprehensive Coaching Report Template to streamline your coaching sessions. Download our free full report template and elevate your coaching practice with Carepatron.
Ortolani Test
Learn about the Ortolani Test for detecting hip dislocation in infants, including the procedure, symptoms, and how to use our comprehensive test template.
Bunnell Littler Test
Learn how to perform the Bunnel Little Test for intrinsic tightness. Get a free PDF template and sample here.
Risk for Injury Care Plan
Download Carepatron's free PDF example of a risk for injury care plan to help assess and manage potential risks in healthcare settings.
List of Processed Foods to Avoid
Discover the extensive list of processed foods to avoid for a healthier lifestyle. Download Carepatron's free PDF guide now and take control of your diet.
Medicare Enrollment Period Chart
Get a free Medicare Enrollment Period Chart to help patients understand Medicare enrollment periods. Download the PDF template here.
Ruminating Thoughts Worksheet
Discover effective strategies to manage ruminating thoughts with our comprehensive worksheet, designed for mental health improvement and cognitive clarity.
Meningitis Nursing Care Plan
Access Carepatron's free PDF download of a Meningitis Nursing Care Plan and example to help with a nursing diagnosis for meningitis. Learn how to create an effective care plan for patients with meningitis.
Hypoglycemia Nursing Diagnosis
Learn about hypoglycemia nursing diagnosis and get Carepatron's free PDF download with examples to help you better understand and manage this condition.
Dyslexia Worksheets
Explore our Dyslexia Worksheets for effective reading, writing, and spelling support. Free examples are included for structured learning.
Dialysis Care Plan
Need help creating a dialysis care plan? Download Carepatron's free PDF and example to get started.
Medicare Eligibility Age Chart
Unlock key insights into Medicare eligibility with our detailed age chart and comprehensive guides, perfect for healthcare professionals and the public.
Coleman Block Test
Streamline the process of documentation during a Coleman Block Test with a patient by downloading our Coleman Block Test template today!
Appointment Schedule Template
Streamline scheduling process, optimize time management, and enhance productivity. Organize your appointment schedules with our Appointment Schedule Template.
Osteoporosis Care Plan
Developing an osteoporosis care plan is essential for managing this condition effectively. Download Carepatron's free PDF example to learn more.
Medicare Fact Sheet
Download a free Medicare Fact Sheet for your patients. Learn how Medicare works with our free template.
Antipsychotic Sedation Chart
Discover the essential functions of modern antipsychotic drugs, sedation charts, the benefits of medications, and how Carepatron enhances mental health treatment.
Conversation Skills Worksheet
Level up conversational abilities with our engaging Conversation Skills Worksheet. Practical exercises and goal-setting included. Download for free today!
Contingency Map
Understand and use Contingency Maps for behavior management in therapy, education, and parenting for improved decision-making.
Healthy and Unhealthy Food Worksheet
Download our free Healthy and Unhealthy Food Worksheet to help you identify nutritious choices and balance your diet. It includes a fun plate activity!
Diabetes Treatment Guidelines
Explore comprehensive Diabetes Treatment Guidelines for effective management and improved health outcomes.
Steinman Test
Learn about the Steinman Test, a diagnostic procedure for assessing shoulder stability and potential issues, in healthcare.
Medical Spa Business Plan
Discover how to launch and grow your medical spa with our comprehensive business plan guide. Tips, templates, and strategic insights for success.
PTSD Dissociation Test
Assess PTSD dissociation symptoms with Carepatron's free PDF download containing a test and examples for evaluation. Get insights and guidance on recognizing symptoms.
Medical Billing and Coding Practice Worksheets
Enhance medical billing & coding skills with our practice worksheets! Perfect for training & mastering critical concepts. Start learning today!
CVC Checklist
Discover an essential CVC checklist for efficient business operations. Streamline your processes and enhance productivity with our comprehensive guide.
Massage Therapy Invoice Template
Get access to a free Massage Therapy Invoice Template with Carepatron. Streamline your documentation and invoicing process with our PDF.
Ankle Injury Diagnosis Chart
Learn more about ankle injuries and have a step-by-step guide on diagnosing them with our free ankle injury diagnosis chart template.
Health Triangle Worksheets
Explore and improve your well-being across physical, mental, and social health with our comprehensive Health Triangle Worksheets.
Cholecystitis Treatment Guidelines
Explore our Cholecystitis Treatment Guidelines for managing acute conditions. Download the PDF now.
Schizophrenia Treatment Guidelines
Discover the latest Schizophrenia Treatment Guidelines, including antipsychotic medication, psychosocial interventions, and cognitive behavioral therapy.
Breast Cancer Treatment Guidelines
Explore comprehensive Breast Cancer Treatment Guidelines for informed decisions. Learn about the latest protocols and options for adequate care.
Rheumatoid Arthritis Diagnosis Criteria
Learn about the essential Rheumatoid Arthritis Diagnosis Criteria for accurate identification and timely treatment in healthcare.
Face Sheet (Medical)
Explore the benefits of using a medical face sheet for efficient patient care, including quick patient data access and insurance verification.
Medicare 8-minute Rule Chart
Master the Medicare 8-Minute Rule with our comprehensive chart and guide. Simplify billing for time-based therapy services and maximize reimbursement.
Cataract Evaluation
Streamline your Cataract Evaluation process by using our template for documentation. Download for free today!
Wheelchair Evaluation
Download our Wheelchair Evaluation template to streamlines the documentation process through a evaluation of clients' mobility and seating needs.
Pediatric BMI Chart
Download our Pediatric BMI Chart for a resource that can assist you in assessing and documenting a child's weight status.
Bariatric Psychological Evaluation
Explore our comprehensive guide on Bariatric Psychological Evaluation to understand the importance, process, and benefits for surgery candidates.
Medical Fishbone Diagram
Explore the Medical Fishbone Diagram to identify the causes of healthcare issues with our free PDF template. Streamline problem-solving in clinical settings.
Navicular Stress Fracture Test
Explore diagnosis and treatment for navicular stress fractures with our free guide on tests, symptoms, and recovery strategies.
Triphasic BBT Chart
Discover how a Triphasic BBT Chart can help track fertility and early pregnancy signs. Download our free PDF for insights and examples.
Scaphoid Fracture Test
Explore the essential aspects of scaphoid fractures, including symptoms, risk factors, and treatments. Access our free Scaphoid Fracture Test PDF for better patient care.
Health Anxiety CBT Worksheets
Overcome health anxiety with our CBT worksheets designed to help you understand and manage your fears. Download our free example today.
Female Acupuncture Points Chart
Explore our Female Acupuncture Points Chart for a comprehensive guide on key acupuncture points and meridians to enhance women's health treatments.
Musculoskeletal Examination Checklist
Explore a comprehensive guide on musculoskeletal system examination, conditions, treatments, and FAQs with a free checklist PDF download.
Pain Management Coding Cheat Sheet
Streamline your medical billing and coding for pain management with our comprehensive cheat sheet. Download our free PDF today.
Body Neutrality Worksheet
Explore our Body Neutrality Worksheet to help individuals foster self-acceptance and focus on the functionality of their bodies. Download it now!
Massage Therapy Business Plan
Creating a massage therapy business plan? Download Carepatron's free PDF to guide you through the process and help you create a successful massage therapy business plan.
Food and Symptom Diary PDF
Track your food intake and symptoms on a symptom-free day with our convenient Food and Symptom Diary PDF report. Monitor your health quickly and effectively.
Newborn Exam Template
Streamline newborn examinations with our comprehensive template, ensuring thorough newborn assessment and care. Download now!
Learning Needs Assessment Nursing
Unleash your full potential! Master nursing skills & knowledge with Carepatron's LNA guide. Boost patient care & career growth.
Hypochondria Test
Explore our guide on illness anxiety disorder: signs, impact, and treatments. Download a free Hypochondria Test to start your journey to better health.
Binocular Vision Test
Carepatron's free PDF download provides a binocular vision test example that you can use to assess your vision. Learn more about binocular vision and how to conduct the test effectively.
Radical Forgiveness Worksheet
Unlock the power of Radical Forgiveness with our comprehensive worksheet. Guide your patients to healing and transformation with our template and guide.
PASS Assessment
Explore the use of a specialized test to assess postural control among stroke patients to craft a more targeted rehabilitation plan.
Eden's Test
Discover the significance of Eden's Test in diagnosing thoracic outlet syndrome. Learn how this maneuver aids in identifying neurovascular compression.
Esthetician Business Plan
Crafting an Esthetician Business Plan is crucial for success. Download Carepatron's free PDF to guide you in creating your own professional business plan.
Test for Muscle Weakness
Learn how to determine muscle weakness with Carepatron's free PDF download and example. This resource provides valuable information on assessing muscle strength and functionality.
Healthcare Marketing Plan
Download Carepatron's comprehensive Healthcare Marketing Plan PDF, which helps create a successful strategy that drives patient engagement, trust, and growth for your organization.
Hearing Aid Evaluation
Learn how to conduct a thorough hearing aid evaluation with our free PDF download. This comprehensive guide includes examples and tips for success.
OCD Treatment Guidelines
Navigate through the complexities of OCD with our comprehensive treatment guidelines. Discover evidence-based strategies for effective management.
Behavioral Health Treatment Plan
Explore effective mental health treatment plans with our free PDF template, which is ideal for mental health professionals seeking structured recovery paths.
Classical Conditioning Worksheet
Explore classical conditioning with our worksheet, perfect for students, therapists, and self-learners to deepen their understanding of behavior theories.
Action Planning Worksheet
Maximize project success with our Action Planning Worksheet. Track and measure progress effectively. Download free templates for complete project management.
Pharmacy Technician Worksheets
Unlock pharmacy tech skills with our free worksheets for exam prep, skill refreshment, and practical knowledge. Download now.
Cross Addiction Worksheet
Carepatron offers integrated software for therapy practice management, streamlining scheduling, billing, and clinical documentation for healthcare providers.
Type 2 Diabetes Treatment Guidelines
Get comprehensive guidelines and examples for treating Type 2 Diabetes in Carepatron's free PDF download.
Pain Management Treatment
Discover effective pain management treatments and examples through Carepatron's free PDF download. Learn about various strategies to alleviate pain and improve your quality of life.
Inner Child Healing Exercises
Unlock your healing journey with Inner Child Healing Exercises. Reconnect with your inner child, heal childhood trauma, and find emotional resilience.
Burnout Recovery Plan
Get your free PDF of a burnout recovery plan from Carepatron to help you overcome burnout and regain work-life balance. Explore practical recovery strategies.
Therapy Invoice Template
Our Therapy Invoice Template streamlines billing processes, enhances professionalism, and effortlessly keeps you organized. Download now!
Muscle Test
Discover everything you need to know about muscle testing, examples, and Carepatron's free PDF download to help you better understand this technique.
Five-Facet Mindfulness Questionnaire
Measure mindfulness with an evidence-based tool to gain clients' mindfulness profiles and improve clinical outcomes through tailored interventions.
Pisiform Fracture Test
Learn how to conduct the Pisiform Fracture Test. Get a free PDF template to record results and streamline your documentation.
90-90 Hamstring Test
Learn how to perform the 90-90 Hamstring Test. Access a free PDF template and example here.
Overhead Squat Assessment
Get access to a free Overhead Squat Assessment template. Learn how to perform this test and interpret the results.
Osteoarthritis Diagnosis Criteria
Understand the signs, causes, and effective criteria for diagnosis. Download our free PDF example for a detailed understanding.
Stages of Relapse Worksheet
Download our free Stages of Relapse Worksheet to effectively track and manage signs of emotional, mental, and physical relapse.
Cervical Flexion Rotation Test
Discover the Cervical Flexion Rotation Test for assessing upper cervical spine dysfunction, ideal for diagnosing cervicogenic headaches and neck issues.
Levels of Hoarding Test
Access a resource that will aid you in evaluating a patient's hoarding disorder. Download our Levels of Hoarding Test today!
Antisocial Personality Disorder Treatment Plan
Discover an effective treatment plan for Antisocial Personality Disorder to help individuals manage symptoms and improve quality of life.
Vineland Adaptive Behavior Scale
Learn more about the comprehensive Vineland Adaptive Behavior Scale, which assesses adaptive behaviors in individuals and provides targeted support.
Norton Scale
Learn about the Norton Scale, a tool used in healthcare to assess the risk of pressure ulcers. Understand its significance and application.
Medical Diagnosis Form
This form helps healthcare professionals gather patient information for accurate diagnosis. Download a free medical diagnosis form template.
Authenticity Test
Discover how authentic you are with our Authenticity Test. Uncover your true self, live more authentically, and improve your life satisfaction. Try it now!
IFS Treatment Plan
Download Carepatron's free PDF example of an Internal Family Systems (IFS) treatment plan. Learn how to create a comprehensive treatment plan using IFS therapy techniques.
Beers Criteria Template
Explore the Beers Criteria Template, guiding principles for safer medication use in older adults—essential knowledge for healthcare professionals.
Non-Medical Home Care Assessment Form PDF
Download, print, and fill out our Non-Medical Home Care Assessment Form PDF for thorough evaluation and personalized care plans. Streamline your caregiving process today!
Miracle Question Worksheet
Use a helpful tool when practicing solution-focused therapy to engage and build motivation among clients. Download your free PDF here.
Premenstrual Dysphoric Disorder DSM-5
Explore the criteria of Premenstrual Dysphoric Disorder (PMDD) as outlined in DSM-5, shedding light on panic disorder and its impact on mental health.
Normal Blood Sugar Levels Chart
Understand how a Normal Blood Sugar Levels Chart works. Get access to a free PDF template and example in this guide.
Height Weight Charts
Learn about height-weight charts and their use in healthcare practice. Find out your ideal weight and stay healthy!
Glasgow Coma Scale
The Glasgow Coma Scale (GCS) dates back to the 1970s and has become one of the most widely accepted measurements of impairment following brain injury. What better way to start using the GCS in your practice than with Carepatron’s free PDF GCS template download.
A1C Goals By Age Chart
Use our free A1C Goals by Age Chart to learn the recommended A1C goal for people of different ages. Download our free PDF and example here.
Mononucleosis Test Reports
Learn about the Mononucleosis Test, its purpose, and procedure, and get an example of the test results in this guide. Download a free PDF template here.
Nutrition Assessment
Precisely assess the nutritional needs of your patients and streamline your documentation process using our comprehensive and formatted nutrition assessment form.
1 minute heart rate recovery chart by age
Discover a 1-minute heart rate recovery chart by age and get an example for tracking your heart rate recovery. Download a free PDF today!
Abbey Pain Scale
Execute an effective pain management plan for your non-verbal patients with dementia. Determine their pain severity immediately using the Abbey Pain Scale.
Menstrual Cycle Phases
Gain an understanding of the menstrual cycle phases with our Menstrual Cycle Phases Chart, which aids fertility awareness and reproductive health.
Manual Muscle Testing
Improve patient assessment skills with our Manual Muscle Testing template. Download for free and easily record and interpret muscle strength results.
Pain Level Chart
Discover the utility of Pain Level Charts for effective pain assessment and communication. Download our free PDF template and learn how to use it effectively.
Admission Nursing Note
Discover what is included in an Admission Nursing Note and download a free PDF example to get started.
Join 10,000+ teams using Carepatron to be more productive
Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.
9 Module 10 – Vital Signs
Vital signs.
Learning Objectives
- Understand the importance of vital signs
- Demonstrate proper technique in obtaining vital signs
- Demonstrate understanding of interpreting vital signs
- Develop understanding of cardiovascular and respiratory disease processes
- Demonstrate working knowledge of oxygen delivery
Vital signs are measurements the healthcare team can take on a person that gives them key information on the functioning of a person’s key bodily processes like their blood and their breathing. The four basic vital signs are temperature , pulse , respiration , and blood pressure .
Always take vitals accurately; if vital signs cannot be taken for some reason, then vital sign measurements should not be guessed or estimated.
Vitals can help the team determine their illness, or the direction of their recovery. Vital signs can also be a general indication of health, or a sign that a patient is having a medical emergency.
Vitals measurements must be accurate, because they are important information for care planning, and give diagnosticians necessary information to make their diagnoses [1] .
Temperature
The human body only functions properly within a specific temperature range. Temperature refers to the amount of heat in the body. While the body has its own means of regulating temperature, but sometimes the balance between heat produced and heat lost tips into an unhealthy range.
A human’s body temperature will be slightly lower in the morning and will rise as the day progresses due to activity and wakefulness.
Standard average body temperature for a human is about 98.6 degrees Fahrenheit, though it fluctuates depending on how the measurement is taken. Normal temperature range is considered to be 97 – 99 degrees Fahrenheit.
Body temperature is affected by multiple factors such as age, exercise, stress, illness, and medications
- Age impacts body temperature due to associated loss of fatty tissues and diminished blood circulation.
- Exercise increases body temperature as muscles produce heat during activity.
- Stress can increase a person’s body temperature because of hormones like adrenaline, cortisol, and epinephrine. The human body’s temperature responds to its hormonal state.
- Drugs such as Tylenol, aspirin, and ibuprofen are considered fever-reducing drugs because they lower body temperature. Somebody is only considered “fever-free” if their body temperature stays within a normal range without the use of fever-reducing medication.
Sebastian Porta, Cory Kontros, Andrew Starr-Bochicchio, CC BY-SA 3.0
Taking someone’s temperature
A normal human temperature range is 97 – 99 degrees Fahrenheit. Subnormal body temperature could be caused by exposure to cold, alcohol use, illness and infection, and other factors.
A person has hypothermia when their body temperature is too low to permit normal functioning. Symptoms of hypothermia include cyanotic skin (pale and blueish in color), numbness, shivering, impaired breathing, slowed movement, and confusion and disorientation. If any of the symptoms are observed, alert the nurse.
A person’s temperature can be taken in different ways, and each method will have slightly different normal ranges. Always practice Standard Precautions while taking someone’s temperature by wearing gloves and other PPE as required. The most common methods of taking someone’s temperature are the oral, rectal, tympanic, and axillary [2] .
Oral temperature
Oral temperature is taken from the mouth, and is usually taken with a digital thermometer. A normal temperature range for most oral thermometers is 97.6 – 99.6 degrees Fahrenheit. Eating or drinking, smoking, or exercising within 30 minutes prior to taking oral temperature can produce an inaccurate reading.
Do not take oral temperature from people who are:
- unconscious
- in mouth pain
- using nasogastric tubes
- using oxygen
After performing the opening procedure, the NA should remove the thermometer and put on the plastic sheath. Put it in the person’s mouth to one side after instructing the person to hold the thermometer in their closed mouth.
When the thermometer indicates that it has read the temperature the NA should commit the number to memory before taking the thermometer from the person, discarding the sheath, and cleaning the thermometer in accordance with facility protocol.
Wait with the person and not leave the room while an oral temperature reading is being taken. The process is finished after recording the temperature and performing the closing procedure.

Image marked with CC0 1.0 .
Rectal temperature
Rectal temperature is taken by inserting a thermometer ½ to 1 inch into a person’s rectum; a normal temperature range for a rectal reading is 98.6 – 100.6 degrees Fahrenheit. A person may need their rectal temperature taken if they cannot use an oral thermometer.
A person may be uncomfortable having their temperature taken in this way, so NAs should be respectful and explain the process thoroughly. The person must hold still during the temperature reading, so their being calm and cooperative is essential for taking accurate vital measurements.
To take someone’s rectal temperature NAs should always begin with clear and calming instructions on how the person needs to cooperate by sitting still during the process in order to get an accurate reading. Provide privacy when someone is exposed by closing their door and privacy screen.
NAs should prep the thermometer by lubricating the tip or applying a cover for the probe. Rectal thermometers look similar to oral thermometers. Once the thermometer is prepped and the person is positioned in left-lying Sims’ with only their buttocks exposed, the thermometer tip can be inserted ½ to 1 inch in the person’s rectum.
Never force an object into someone’s rectum; if the thermometer encounters resistance, the NA should stop. The person’s buttocks should be covered again while the thermometer gets the reading; the NA must hold onto the thermometer at all times.
After recording the temperature, clean the thermometer according to facility policy.
Tympanic temperature
Tympanic temperature is a temperature reading taken from the person’s ear canal. A normal reading for tympanic temperature is between 96.6 and 99.7 degrees.

After preparing the thermometer, gently position the person’s head right in front of them and straighten the ear canal by tenderly gripping the outer edge of the ear at about 11 o’clock, and pulling it up and back. Tympanic thermometers should only be inserted about ¼ to ½ an inch into the ear canal.
Keep holding the ear and the thermometer until the thermometer is finished with the reading. The reading should be memorized immediately.
After committing the reading to memory, Image by wuestenigel, CC BY 2.0 the NA can clean the thermometer or discard the disposable sleeve, discard gloves and wash hands, and record the person’s temperature on their chart.
Temporal temperature
A temporal thermometer is a non-invasive thermometer that takes a person’s temperature by being swiped across their forehead. It is especially useful for children, and people who require a noninvasive approach. A normal reading for a temporal thermometer falls between 97.6 and 99.6 degrees Fahrenheit.
Axillary temperature
Axillary temperature is taken at the person’s armpit. While this method is less accurate than oral, rectal, and tympanic temperature, it is also safer and less invasive than methods that require inserting a thermometer into an orifice. A normal range for axillary temperature is between 96.6 and 98.6 degrees Fahrenheit.
When taking a person’s temperature always perform the opening procedure and allow for privacy. Once the thermometer has been prepared, help the person remove their arm from their sleeve and tuck the thermometer into the person’s armpit. The person should hold their arm close to their chest to keep the thermometer in place. The reading will take between 8 and 10 minutes.
Once the reading is complete the NA should commit the number to memory before discarding gloves and washing hands, and helping the person get re-situated in their clothing. The temperature reading should be recorded immediately along with the method used to take it.
The three vital signs other than temperature (pulse, respiration, and blood pressure) all closely involve the circulatory system. In other words, a person’s vital signs closely relate to the workings of their heart. A person’s heart is located on the right side of their chest and is about the size of a fist. The heart is made of muscle tissue and, through its contractions, is responsible for the movement of blood throughout the body. The heart pumps about 7,000 liters of blood through the body every day.
FuseSchool – Global Education. (2017, April 6). Heartbeat and Pulse | Physiology | Biology | FuseSchool [Video]. Youtube. https://www.youtube.com/watch?v=DLmmN0jy-s0
The heart consists of four hollow chambers; there are two atria, which fill with blood before being pumped to other areas of the body, and two ventricles, which pump blood to the lungs, head, and all the way to the feet. When the heart beats it makes a lubb-dubb sound.
The “lubb” part of that sound is the systole , or the part of the heartbeat when the heart contract and makes the motion that pumps blood. The diastole is the “dubb,” or the part of the heartbeat when the heart relaxes, refills with blood, and prepares to make another contraction. During diastole, blood from the atria flow into the ventricles before being pumped to other parts of the body.
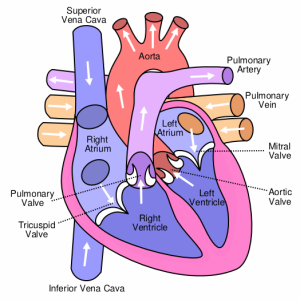
created by Wapcaplet, CC BY-SA 3.0
Measuring pulse
Pulse is an important vital sign that will need to be measured regularly. Pulse refers to the rhythm of blood moving against an arterial wall, and is measured as “beats per minute” (BPM). Pulse can be measured in many different areas on the body, technically anywhere an artery is close enough to the surface of the skin for a person to feel the rhythm of blood.
The normal range for pulse in adults is 60 – 100 BPM, with most adults averaging about 70 – 80 BPM. When counting a person’s pulse, in addition to counting BPM, NAs should pay close attention to the rhythm and force of the beats [3] . A pulse’s rhythm should be regular as in the time between beats is roughly equal; a pulse should feel strong but not thumping.
Use to visually mark the passage of 30 seconds; trying to count both seconds and beats at the same time makes errors likely.
When taking a radial pulse , the NA should gently and firmly place two fingertips on the thumb side of the person’s inner wrist. The person may also appreciate some extra support to support their arm and hand. Count each pulse beat for exactly 30 seconds. However many beats the person’s pulse has in 30 seconds should be doubled to find the beats per minute. If the pulse is irregular then the NA should count the pulse for the full 60 seconds.
The apical pulse is taken for a full 60 seconds and is located on the left side of a person’s chest, just below their nipple. Apical pulse is used for persons with irregular heart rhythms, heart disease, and heart medications [4] . The apical pulse is taken using a stethoscope; NAs should make sure that the earpiece and diaphragm (flat piece placed in contact with the person whose pulse is being taken) of the stethoscope have been wiped off properly before use. The stethoscope should also be cleaned after use.
The apical-radial pulse is a way of measuring pulse that takes both the apical and radial pulse into account. Counting an apical-radial pulse will require two people, one to take the apical pulse and one to take the radial pulse. The apical pulse is usually either the same or higher than pulse taken at other areas of the body; if the apical pulse is lower than pulses elsewhere, it is an indication of very poor circulation. When the apical pulse is higher than the radial pulse the difference is called the pulse deficit.
https://www.youtube.com/watch?v=yhoi2nVE9o8
Skills Lab. (2017, August 20). B 804 Assessing apical-radial pulse [Video]. Youtube. https://www.youtube.com/watch?v=yhoi2nVE9o8
Blood pressure
While pulse is the rate at which blood is pumped through veins and arteries, blood pressure refers to the amount of force exerted upon the walls of an artery by the blood. A person’s blood pressure is determined the amount of force with which the heart contracts, the amount of blood pumped with each heartbeat, and how easily and smoothly the blood is able to flow through the blood vessels.
Blood pressure readings are recorded as the systolic blood pressure over the diastolic blood pressure; they look like a fraction, such as 110/70. The top number, systolic pressure, measures the force of blood as the heart contracts, while the lower diastolic number measure the force of blood as the heart is at rest in between lub-dubs. The normal range for systolic blood pressure is 90 – 119, while the normal range for diastolic blood pressure is 60 – 90.
Hypo- and hypertension
Hypotension is the word for low blood pressure. A person is considered hypotensive is their systolic blood pressure falls below 90 or their diastolic blood pressure falls below 60. Postural hypotension is a common form of hypotension where a person experiences a sudden drop in blood pressure when they stand or sit up quickly. A person with postural hypotension may become lightheaded, dizzy, or event faint if they stand or sit up quickly.
Hypertension is high blood pressure. Hypertension can be dangerous in its own right, and is a symptom of many different heart conditions and circulatory problems. There are a few different classifications of high blood pressure [5] .
- Elevated: Systolic pressure 120 – 129 and diastolic less than 80
- Stage 1 of hypertension: Systolic 130 – 139, or diastolic 80 – 89 (only one needs to be present for classification)
- Stage 2 of hypertension: Systolic pressure 140 or higher, or diastolic 90 or higher
- Hypertensive crisis: Systolic pressure 180 or higher, and/or diastolic pressure 120 or higher. A person in hypertensive crisis will require immediate emergency medical services.
Hypertension is widely known as the “silent killer.” Hypertension can develop in people of any age, and is diagnosed when a person’s blood pressure is regularly above 130 (systolic) and/or above 80 (diastolic). Symptoms of hypertension include headaches, dizziness, and blurred vision.
Long-term hypertension usually occurs when a person’s blood vessels harden and narrow; it can also be caused by high levels of stress and pain, arterial plaque buildup, as a side effect of medications, and other factors.
Hypertension can lead to heart attacks, especially when it is related to a blockage of a blood vessel, also called an occlusion . Occlusions can cause ischemia , which is when an area does not get sufficient blood supply, which can also lead to a stroke.
NAs will need to take frequent blood pressure readings on people with hypertension to closely observe and record any abnormally high readings or sudden changes from the person’s usual readings.
TED Ed. (2015, July 3). How blood pressure works – Wilfred Manzano [Video]. Youtube.com. https://www.youtube.com/watch?v=Ab9OZsDECZw
Measuring blood pressure
Blood pressure is measured using a tool called a sphygmomanometer . Sphygmomanometers are either manual or digital. To take someone’s blood pressure, the NA will need the sphygmomanometer, a stethoscope (only if using a manual sphygmomanometer), a blood pressure cuff, and alcohol wipes.
Sphygmomanometers are made of an armband that tightens either through the manual use of an attached handheld squeeze-ball air pump or the arm band will tighten automatically, as well as an interface where the blood pressure is displayed, and tubing that connects the arm band with the display.

“ sphygmomanometer ” by kndynt2099 is licensed under CC BY-NC 2.0 .
A person’s blood pressure should not be taken if they have recently engaged in activities that raise or lower their blood pressure. Examples include exercise within the last 30 minutes, and the presence of caffeine, tobacco, and other drugs.
Be careful of placement when taking blood pressure. The sphygmomanometer’s arm band should not be placed on an arm that has an IV line, a cast, burns or injuries, recent physical trauma, a mastectomy or another surgical incision on that side, or dialysis treatment. Arms that are paralyzed or have been amputated should not be used to measure blood pressure.
Taking a person’s blood pressure manually requires substantial concentration and focused listening. After performing the opening procedure and cleaning the equipment, discuss the procedure with the person and ask them to cooperate by remaining calm, quiet, and still.
After making sure the cuff is completely deflated, the NA should wrap the blood pressure cuff around the person’s bare arm positioned palm-up at about heart level, with the cuff’s center placed about 2 inches over the inside of the elbow.
Place the stethoscope over the artery on the inner elbow and tighten the valve on the arm cuff until it is closed but not too tight. Use the handpump to inflate the cuff to 170 – 200. The valve should slowly be opened until a pulse beat is heard; if a pulse is heard immediately at the original number, deflate and begin the process at a higher pressure.
Listen carefully while deflating the cuff. The number on the gauge when the first pulse becomes clearly audible is the systolic blood pressure and the first number in the reading. The gauge reading when the pulse beat sound changes or disappears is the diastolic blood pressure. Once the diastolic pressure is observed the NA can fully release the cuff valve before removing it. The systolic and diastolic numbers should be recorded immediately after handwashing. If the reading is abnormal or a significant change from other readings, inform the nurse.
Obtaining a blood pressure reading on someone is much simpler with an automatic sphygmomanometer than with the manual variety. After performing the opening procedure, the NA should make sure the cuff is totally deflated before positioning it so the center is right above the brachial artery. The cuff should be snug. Next, turn on the blood pressure machine and select the proper settings. After the machine performs the reading the NA should chart the blood pressure immediately and details like the arm used and the time the measurement was obtained.
RegisteredNurseRN. (2019, June 4). Blood Pressure Measurement: How to Check Blood Pressure Manually [Video]. Youtube. https://www.youtube.com/watch?v=UGOoeqSo_ws
Respiration
Respiration is the process of breathing, or moving air into and out of the lungs. Our lungs extract the oxygen from the air and use it to replenish the oxygen in our blood. Respiration occurs in two parts; we inhale during inspiration, and exhale during expiration; a full respiration is both an inspiration and expiration, or one breath in and one breath out. The normal rate of respiration for adults is between 12 and 20 breaths per minute [6] .
Nobody breathes in exactly the same way, however in general a person’s breathing should be effortless and quiet. Occasional sighing is normal, though if sighing is consistent and regularly it could be a sign that they are breathing too shallowly.
When a person breathes it activates their diaphragm, a small and powerful muscle beneath the lungs, and the intercostal muscles, which are the three layers of muscle tissue between the lungs and the ribcage. As inspiration occurs the muscle system expand and makes space for the inflating lungs, and upon exhalation the muscles contract and help to squeeze the leftover carbon out of the molecules. The bronchiole carry air to the alveoli, which help oxygen enter the blood stream.
Measuring respiration
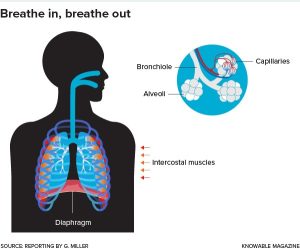
NAs can obtain a count on a person’s respirations during the same process as getting their radial pulse. After the first 30 seconds spent taking a person’s radial pulse, the NA should keep their fingers on the person’s radial pulse while switching to counting their breaths for the next 30 seconds.
A person’s respirations often change when they know that their breathing is being observed. Instead of explicitly telling them, transition right from taking a person’s radial pulse to counting their respirations by observing or feeling the rise and fall of their chest. Respirations can be counted for 30 seconds and then multiplied by two to obtain respirations per minute; if breathing is irregular, respirations should be counted for the full 30 seconds. Image by knowablemag is licensed under CC BY-NC-ND 2.0
Observing respiration
Closely observe a person’s breathing for signs of irregularity and difficulty. If a person experiences apnea , the temporary absence of breathing, or dyspnea , labored or difficult breathing, they should alert the nurse immediately.
Other symptoms of breathing problems include:
- irregular breathing or changes in breathing rhythm
- weak or shallow breathing
- breathing noises such as gurgling, wheezing, snoring sounds, grunting, etc
- use of shoulders and chest during respiration
- breathing abnormally fast or slow
- skin and lip discoloration
Problems with a person’s breath often result from or precede an adverse medical event, and must be reported immediately.
Vital sign review
RegisteredNurseRN. (2019, May 13). Vital Signs Nursing: Respiratory Rate, Pulse, Blood Pressure, Temperature, Pain, Oxygen [Video]. Youtube. https://www.youtube.com/watch?v=gUWJ-6nL5-8&t=23s
Oxygen Delivery
What is respiration.
Respiration is the process of gas exchange between a person and their environment; the human body takes in oxygen from the environment, removes the oxygen to fuel its blood and cells, and then expels carbon dioxide back into the environment. The average adult takes about 20 breaths per minute.
The lungs are where blood exchanges carbon dioxide waste from the body’s cells with fresh oxygen to re-supply the cells with energy. The blood then transports oxygen throughout the body, while removing carbon dioxide from our cells and taking it back to the lungs to be disposed of. The body naturally strived for balance in oxygen and carbon levels, and when the balance is tipped someone may start to breathe irregularly in response.
Medical Animation Videos. (2014, February 4). Gas exchange in lungs physiology video animation – made easy [Video]. Youtube. https://www.youtube.com/ watch?v=AJpur6XUiq4
Factors impacting oxygen delivery
Different factors impact a person’s oxygen needs and ease of respiration. A person’s oxygen needs are impacted by their overall respiratory health; how wide and clear the airways are, levels of inflammation, and the health of the person’s lungs and air sacs all contribute to oxygen needs [7] .
Circulatory health: The circulatory system delivers the oxygen to the rest of the body. Blood vessels must be open and flexible enough to deliver large amounts of blood to every area of the body. Capillaries are tiny blood vessels that widely distribute blood throughout the body including the areas that don’t have large blood vessels, such as our fingers, ears, and scalp. Capillaries are everywhere, are about the thickness of a small hair, and have extremely thin walls to promote the exchange of fluid, gas, and nutrients between blood vessels and other tissues.
Anemia is a condition where people do not have enough red blood cells. Anemia can result in some areas of the body being deprived of oxygen.
As a person ages their blood has a lower red blood cell (hemoglobin) count. Red blood cells carry the oxygen to different parts of the body. The fewer red blood cells a person has, the less effective will their oxygen delivery system will be.
As a person ages their blood vessels become stiffer and inelastic, which also inhibits oxygen delivery.
Exercise: When a person exercises their body uses much more oxygen than when it is at rest. Exercise can have a positive impact on a person’s oxygen delivery system by expanding lung capacity and widening blood vessels, or a negative one by worsening symptoms of respiratory conditions such as asthma.
Nervous system is also involved in respiration; the nerves throughout our body send signals to our brain when our oxygen needs change and when something is wrong. Impairments to the nervous system can impact a person’s breathing. For example, if somebody is paralyzed from the neck down they may require an assistive device to continue delivering oxygen.
Aging: Lung and respiratory muscle strength diminish with age, and lung and airway tissue loses elasticity.
Environment: The particulate content and air quality of the air a person breathes can cause negative side effects. Persons who smoke cigarettes, especially if they’ve been smoking for a long time, will have harmed their respiratory system. Environmental pollutants can have a harmful impact on a person’s ability to breathe well. Seasonal or environmental allergies have a negative impact on a person’s respiratory system when the allergen is present, sometimes causing airways to swell and close, or causing breathing to be interrupted by severe congestion.
MotivationalDoc. (2015, December 6). Proper Breathing Exercise to Strengthen Lungs to Keep Healthy – Dr Mandell [Video]. Youtube. https://www.youtube.com/watch?v=y3LUlag7W1s
Abnormal Respiration and Oxygen
Abnormal respiration patters are described in healthcare contexts using some technical terminology. When communicating with other members of the care team it will be helpful for NAs to know some key terms about breathing [8] .
- Apnea : not breathing, usually for a short period of time. Many people have sleep apnea, which means they temporarily stop breathing at times when they are asleep.
- Tachypnea : breathing abnormally fast
- Bradypnea : breathing abnormally slowly
- Hypoventilation : not taking in enough oxygen or removing enough carbon dioxide
- Hyperventilation : breathing very quickly and taking in too much oxygen
- Dyspnea: difficulty breathing
- Orthopnea: shortness of breath that only occurs when the person is laying down
EMTPrep. (2019, November 18). Hypoventilation and Hyperventilation – EMTprep.com [Video]. Youtube. https://www.youtube.com/watch?v=aVyAWjaGT8Q
Hypoxia is the term for low oxygen levels. The symptoms of hypoxia occur across physical and behavioral systems because the entire human organism relies on oxygen. Symptoms of hypoxia include:
- restlessness
- disorientation
- changes in personality
- skin discoloration
- poor focus and concentration
- increased pulse
If any of these symptoms are observed, particularly when accompanied by other symptoms on the list, should alert the nurse.
Respiratory illness
Diseases that affect the respiratory system come in many different forms. These diseases can be acute or chronic; an acute disease is one that comes on somewhat quickly and has a relatively short duration, while a chronic disease lasts a long time and may be a lifelong condition.
While the goal of treatment is almost always to return a person to their normal functioning, approaches to treatment and the extent to which a respiratory illness impacts a person’s lifestyle may depend in part on whether the illness is acute or chronic. Sometimes managing symptoms is the only realistic care goal.
Chronic Obstructive Pulmonary Disease (COPD)
Chronic obstructive pulmonary disease (COPD) is a disease that gets worse over time that results in dyspnea due to obstructed airways. There is no cure for COPD, and if patients were smoking at the point of diagnosis then they must stop immediately [9] . Treatment can be helpful in hindering the disease’s progression, even though a return to full respiratory functioning is highly improbable. Chronic bronchitis and emphysema are the two illnesses grouped under COPD.
Chronic bronchitis occurs when the bronchial tubes become inflamed repeatedly and for long periods of time, and is caused by general air pollution, pollution in one’s environment (such as secondhand smoke), and cigarette smoking.
There is also an acute variety of bronchitis caused by infection that sometimes develops out of a bad cold and involves the coughing up of yellow-green mucus from the lungs.
The bronchial tubes branch from the throat into the lungs and help to facilitate the gas transfer between the lungs and the environment; bronchial inflammation can result in difficulty breathing and chest pain. The scarring and long-term inflammation of the bronchial tubes leads to a persistent cough. Eventually the lung tissue also scars and becomes prone to irritation and infection.
Chronic bronchitis and cigarette smoking lead to emphysema , a disease where the air-sacs in the lungs, called alveoli, become damaged and break. Symptoms of emphysema are a persistent cough and dyspnea. Medications, oxygen, and respiratory therapy may be prescribed to slow the disease and make the person more comfortable.
When treating a person with COPD, always practice meticulous infection control practices, and follow the care plan closely concerning medications and oxygen delivery. It is also important to extend patience and understanding to residents’ feelings of anger, fatigue, anxiety, and frustration over their difficulty breathing and respiratory problems.
Pneumonia is a respiratory illness caused by lung inflammation, and has many different causes. Depending on the cause, pneumonia may be communicable. The alveoli fill with fluid and lung tissue becomes inflamed, leading to difficulty breathing and an aggressive wet cough.
Pneumonia can be bacterial, viral, fungal, or in response to a pollutant; anything that causes the lungs to inflame and fill with fluid could be a potential cause of pneumonia. People at high-risk for developing pneumonia are the very young and elderly, habitual smokers, people who have had a stroke, people who are immobile or on bed rest, people with another respiratory illness, people who receive tube-feedings, and people who must use a ventilator.
Tuberculosis
Tuberculosis (TB) is a bacterial infection usually of the lungs, but can impact other areas of the body as well. Symptoms of TB include extensive coughing, dyspnea and chest pain, coughing up blood, fever, chills, and sweats, and exhaustion.
TB is airborne, which means it is spread through droplets of moisture and mucus expelled into the air through an infected person’s speaking, coughing, laughing, singing, etc.
NAs should use isolation-level precautions whenever caring for somebody with TB, including the use of a respirator mask.
A person is less likely to spread (or contract) TB in spaces with excellent ventilation and air circulation, and in a spaces where people wear PPE like masks and respirators.

Any tissues that comes into contact with mucus should be flushed or placed in a biohazard bag and re moved.
Caring for persons with respiratory illness
NAs can assist residents with respiratory illnesses by positioning them upright and making sure their body stays aligned. NAs may also position a person so they are bent over a table with a pillow on it; this position can take some of the weight off their chest and may partially alleviate dyspnea.
Some resident will need exercises including deep breathing and forceful coughing to help open their airways and slow the weakening of their chest muscles. Deep breathing and coughing exercises may be included in a person’s care plan to mitigate respiratory illnesses; always closely follow the person’s care plan.
Deep breathing
A deep breathing exercise involves taking a deep breath, holding it in for 3 – 5 seconds, and then exhaling as long as possible. A coughing exercise may follow a deep breathing exercise, and involves the resident holding a pillow or blanket tightly against their abdomen, taking a deep breath, and coughing as hard as they can. Have tissues and a basin ready to catch anything that is coughed up. Always check the care plan for details on the type of exercises and number of repetitions to use.
An incentive spirometer is a device used to dictate deep and slow breathing exercises, usually following surgery. NAs should prompt people to use the incentive spectrometer as prescribed in their care plan; however if the person is resistant or refuses the NA should not push the matter and should instead report it to the nurse instead.
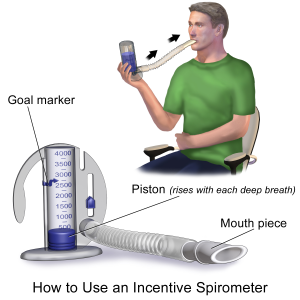
Image by BruceBlaus is licensed under CC BY-SA 4.0 .
NAs should clean the mouthpiece of the spirometer device prior to use. The person should close their mouth around the mouthpiece and inhale slowly and deeply while trying to keep the indicator at the proper level. They can then exhale slowly. The number of repetitions and frequency of incentive spirometer exercises will be detailed in the care plan.
Oxygen delivery
Oxygen is totally essential to every part of the human body. Some people may require oxygen therapy, where oxygen is delivered directly to their lungs using mechanical assistance. A person may need additional oxygen delivery after a surgery, due to a respiratory illness, or any illness that impacts the person’s oxygen levels [10] .
NAs should never hook somebody up to oxygen, take them off of oxygen, or change the settings on their oxygen delivery system.
Some require additional oxygen temporarily or at different points throughout the day and night, while others may need to be connected to an oxygen device at all times.
Oxygen is usually delivered either through a nasal cannula or by a face mask. A nasal cannula is a two-pronged device attached to a tube, where the prongs are inserted into the wearer’s nostrils. The cannula’s tubing is attached to the source of additional oxygen. Nasal cannulas are common in long-term care contexts.
Face masks fit over the nose, mouth, and chin of the wearer, are held there by a band that stretches around the wearer’s head above the ears, and are connected to an oxygen source by tubing similar to that used with a nasal cannula. Face mask oxygen delivery is less convenient and less comfortable than using a nasal cannula because it irritates the skin and prevents any talking, eating, and drinking.
Delivery systems
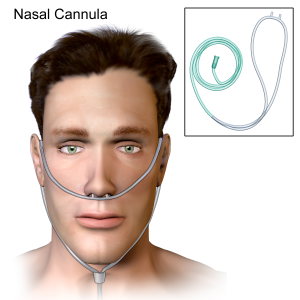
When the oxygen comes from the wall outlet, the cannula or mask’s tubing will simply hook into the designated spot on the wall in their room. If they are using a tank of compressed gaseous or liquid oxygen then the tank will likely be on a cart.
Oxygen concentrators are devices that gather oxygen from the surrounding air and deliver it to the recipient in a concentrated form; they come in various shapes, sizes, and levels of portability. Oxygen concentrators usually plug into electrical outlets.
BruceBlaus, CC BY-SA 4.0
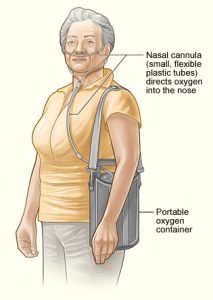
National Heart Lung and Blood Institute (NIH), CC 1.0
Oxygen Safety and Comfort
Oxygen safety is paramount. Compressed and concentrated oxygen is highly flammable. Anything that could possibly cause a spark becomes an extreme fire hazard around an oxygen delivery system; no unnecessary electrical devices or wool linens around an oxygen system, nor anything that could cause a spark.

- Oxygen tanks must be well secured in their holders to prevent damage, oxygen leaks, and explosions. They must always be kept upright and in the proper holder. Oxygen concentrators should be used in a well-ventilated space with adequate air circulation.
- Never use petroleum-based products for a person’s skin care when they are on oxygen. NAs should use water-based lubricants and skin care products that do not pose a fire safety risk.
- NAs should observe the oxygen delivery tubing to make sure it is clean and free of kinks, and changed in accordance with facility policy. Image by Nesdon Booth ( CCBY3.0 )
- NAs should keep a close eye on the oxygen delivery system’s measurements: is the oxygen flow rate remaining at the level prescribed in the person’s care plan? Are the oxygen levels adequate, or does the person’s oxygen tank need to be replaced.
VITAS Healthcare. (2017, November 20). Demonstrations: The Dangers of Oxygen [Video]. Youtube. https://www.youtube.com/watch?v=LrfHnKtKvws
NAs should make a point of providing emotional support to persons on oxygen. Requiring an oxygen delivery system can be a jarring experience; they are uncomfortable, may be difficult to use and disruptive to a person’s routines, and can come with feelings of claustrophobia and loss of control. NAs should provide a listening ear, and encourage the person to continue with the activities they can healthily maintain so their psycho-social needs to do not go unmet.
Reporting and Recording
Report any adverse side-effects or indications of problems with patients using oxygen, including:
- sore, crusty, or reddened areas on the person’s skin
- discoloration in the person’s skin or eyes
- changes in vital signs
- complaints of pain and tightness
Artificial airways
A person may need an artificial airway to ensure that their airways are kept open so the lungs can continue to take in new oxygen and expel carbon dioxide. Without an open airway the lungs cannot function, and the person will not have enough oxygen to live.
Artificial airways are necessary when the person’s airways would otherwise be obstructed due to illness, injury, or surgery. An artificial airway is created when a doctor or nurse inserts a tube, through a process known as intubation, into the person’s windpipe (trachea). The tube may be inserted through the person’s mouth or nose, or through a surgically created opening in the neck. There are a few different kinds of artificial airways [11] .
An oropharyngeal airway is a relatively short, curved plastic tube inserted through the person’s mouth that prevents their tongue from blocking their airway.
An endotracheal airway is inserted through the person’s mouth or nose, and extends into their trachea and sits between their vocal cords.
A tracheostomy is a surgically created stoma in the neck that leads into the trachea. A tracheostomy tube delivers oxygen directly into the trachea. People with tracheostomies will need attentive, sanitary care.
- Caring for a tracheostomy includes maintaining meticulous infection control measures by cleaning the area around the stoma (opening), helping the nurse with changing dressings, and assisting with cleaning the tracheostomy tubing. If the NA notices any gurgling or otherwise abnormal noises coming from the device when the person breathes, they should tell the nurse since the tubing may need to be cleaned.
- Perform oral care every two hours as directed in the care plan. Patients with tracheostomies are at high risk for aspiration, so oral care may need to be performed with specific tools meant for people using artificial airways.
Let a nurse know if you see:
- respiratory difficulty
- discoloration in the skin or eyes
- sores or breaks in the mouth or the skin
- changes in vitals
- loose dressings or tape
- disconnected tubing
- Tracheostomies are cleaned using a process called suctioning. Suctioning involves the use of a pump to remove all secretions from the person’s airway, and may need to be done regularly. NAs cannot perform the suctioning procedure, it must be done by a nurse or a respiratory therapist. If a person with a tracheostomy shows signs of respiratory distress such as noises, shortness of breath, or pain then they may need suctioning.
- NAs should be as supportive as possible when a person needs an artificial airway, particularly during moments of acute discomfort. When a person is having extreme difficulty breathing, maintaining conversation and light touch can be comforting.
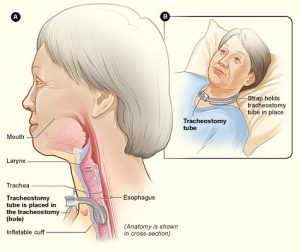
Caring for artificial airways
When caring for somebody with an artificial airway, NAs should regularly closely inspect the tubing and any adhesives that keep tubing in place. If the tubing falls out or comes undone, remain with the person and alert the nurse using the person’s call light.
Positioning matters more than usual for someone using an artificial airway. Always follow the care plan regarding positioning and repositioning.
Artificial airways are uncomfortable. Always practice empathetic communication. Some people using artificial airways cannot speak, so the NA will have to devise alternative means of communication through writing, typing, or gestures.
If the NA observes any signs of abnormal respiration, discoloration in the skin or eyes, secretions in tubing, drainage from surgical sites, or emotional distress, they should alert the nurse.
Mechanical ventilators & chest tubes
A person who cannot breathe on their own may require the assistance of a mechanical ventilator to breathe for them by automatically moving air into and out of the lungs. Ventilators supply a person’s body with oxygen through an artificial airway; because the air bypasses the larynx and vocal cords, a person using a mechanical ventilator will be unable to speak. NAs should be a frequent and calming presence to a person on a ventilator by checking in with them, spending extra time with them if possible, and devising modes of communication to use when the person cannot speak.

NAs should pay close attention to a person on a ventilator, and always make sure that their call light is easily within reach.
If there are any alarms or irregular beeping coming from the mechanical ventilator, notify the nurse immediately. Notify the nurse if a person on a ventilator is exhibiting any signs of respiratory distress, or pain and discomfort.
Practice careful infection control with people who are using ventilators; HAIs are common results of ventilator use in facilities.
NAs will not hook or unhook anybody to or from a mechanical ventilator. The NA’s primary role will be to closely observe the ventilator’s tubing and connections to make sure everything is smooth and free of blocks or kinks, and to provide oral care often and as directed. NAs should work with the person to find effective ways of communicating when they are unable to speak.
Image by BreathDriver, CC BY-SA 4.0
A person may require chest tubes in between layers of lung tissue to help drain air, blood, or other fluids. The tube is attached to a drainage system which allows for the removal of gas or fluids.
NAs must be careful and aware of all tubing and tubing connections, and try to prevent kinks from forming. The system must be completely airtight.
The drainage collection system must be kept below the person’s chest at all times.
The NA should notify the nurse immediately with any changes in the condition of the ventilation system or the patient. Indications of respiratory distress, disconnected or malfunctioning tubing, and coughing up blood must be urgently addressed.
The Nursing Assistant’s Role
NAs have a specific and important set of responsibilities when caring for respiratory patients using oxygen, artificial airways, and chest tubes. While NAs do not insert or connect oxygen, artificial airways, or chest tubes, they perform vital tasks in their observation, and in the care of the people who need them.

- NAs should regularly check to make sure that the oxygen flow is set to the correct amount. Always ask or check the care plan if unsure about a person’s prescribed oxygen treatment. If the oxygen flow is incorrect, tell the nurse immediately.
- A person’s mouth, nose, and skin can develop sores and irritation when using respiratory equipment. Maintaining good oral and skin care can help make a person’s experience less uncomfortable, and will help prevent infections. Maintain communication throughout care tasks even when the person is unconscious and unresponsive.
- Follow the care plan instructions for deep breathing and coughing exercises, and incentive spirometer use. Remain positive and encouraging during these exercises, and exercise patience and empathy when the person expresses frustration.
- Reposition people frequently in accordance with the care plan and instructions from the nurse.
- Alert the nurse immediately if observing any disconnections in the oxygen equipment, any changes in the amount or quality of the drainage, changes in the condition of the device or the person, and any signs and symptoms of hypoxia or respiratory distress.
- Observe and chart carefully and thoroughly.
Key Takeaways
- Vital signs are measurements of some mechanisms part of a body’s basic functional processes. Vital signs include temperature, pulse, respiration, and blood pressure. It is essential that NAs take vital measurements accurately, and alert the nurse if a resident’s vital signs are abnormal.
- Always obtain vital signs properly and respectfully. Chart vitals right after taking them so they are remembered correctly. If temperature, pulse, blood pressure, or respirations are abnormal, they may clue the care team into an ongoing problem or an active medical emergency.
- Hypertension and hypotension are common cardiovascular disorders. While both are dangerous, hypertension can be deadly, cause heart attacks, and points to severe cardiac diseases. Chronic obstructive pulmonary disease (COPD), pneumonia, and tuberculosis are some common respiratory diseases. COPD is an incurable respiratory disease that progresses as alveoli and lung tissue scar and engage in excessive mucus production.
- Some patients may require additional oxygen using an oxygen supply or a mechanical ventilator. When using an oxygen supply, the oxygen will either be delivered using a nasal cannula or a face mask. NAs should not hook up oxygen, unhook oxygen, or change any of the levels on an oxygen supply device. When caring for someone using additional oxygen, make sure that they are comfortable, the tubing is free of kinks that could block flow, and the oxygen is flowing at the rate prescribed in the care plan. Always practice oxygen-specific fire safety, and do not use items that may produce a spark.
Comprehension Questions
1) The normal temperature range for a human is considered to be _____ degrees Fahrenheit, though it varies depending on factors like age, activity level, and illness.
a.97.6 – 99.6
b. 98 – 99.5
d. 96.6 – 98.6
2) Please list the four vital signs, and describe what each of them mean.
3) The systole is ________ , while the diastole is __________ .
a. the top number on a blood pressure reading; the bottom number on a blood pressure reading
b. the atria; the ventricles
c. the motion of the heart as it contracts; the motion of the heart as it refills with blood
d. “dub”; “lub”
4) Respiration is _________ ; the body takes in ______ to distribute throughout the body, and removes _______ .
a. the exchange of gas between a person and their environment; oxygen; carbon
b. the inhalation of fluids during eating and drinking; food or fluid; air
c. the exchange of gas between a person and their environment; air; oxygen
d. the exchange of gas between a ventilator and a person; carbon; oxygen
5) Respond to the following sentences with T (true) or F (false).
____ Aging impacts the circulatory system as hemoglobin decreases and blood vessels harden.
____ Symptoms of hypoxia include oxygen saturation, restlessness, and high energy levels.
____ Some respiratory illnesses cannot be cured. When an illness cannot be cured and lasts a long time it is acute.
____ Hyperventilation includes an excess of oxygen.
____ Someone experiencing hypoxia may act differently, and not seem like themselves.
6) How does someone use an incentive spirometer?
a. By exhaling forcefully into the mouthpiece to get the piston as high as possible
b. By shaking it up and down while inhaling and exhaling slowly
c. By inhaling slowly and trying to keep the piston at the appropriate level
d. By inhaling deeply and blowing back into it again
7) Which of the following should nursing assistants do for someone receiving oxygen therapy? Select any that apply.
a. Adjust the oxygen levels to the prescribed levels in the care plan
b. Remove nasal cannula tubing for cleaning
c. Provide careful skincare around the cannula or mask area
d. Carefully observe the resident for signs of difficulty breathing, and observe but do not change oxygen settings.
8) What is a tracheostomy?
a. An opening through which mucus and secretions can be removed from the lungs
b. A stoma in the neck that allows somebody with mouth sores to speak
c. An opening in the neck that allows oxygen to be pushed directly into the trachea
d. An opening in the neck that removes drainage from the vocal cords
9) Please list at least three adverse side-effects of oxygen use nursing assistants should report to the nurse and record in the resident’s chart.
10) Respond to the following sentences with T (true) or F (false).
____ Oxygen may come from a wall outlet, a portable oxygen tank, or a device called an oxygen compressor.
____ Smoking near oxygen is acceptable as long as you blow the smoke away from the tank.
____ Residents receive oxygen through a nasal cannula, a face mask, or in liquid form.
____ Post an “oxygen in use” sign outside of resident’s doors when they use oxygen so that the rest of the healthcare team is aware of the fire hazard.
____ When tracheostomy tubing becomes disconnected, NAs should hook it up again as quickly as possible as long as they have been trained.
11) Think back to the nursing process (assess, diagnose, plan, implement, evaluate/assess). What goes into each step of the nursing process, and what role do vitals measurement play in each step?
12) How might oxygen use impact someone’s psychosocial needs and wellbeing? How should nursing assistants respond to a person for whom oxygen use is negatively impacting their emotional and social wellbeing?
- Vital Sign Measurement Across the Lifespan - 2nd Canadian Edition by Jennifer L. Lapum; Margaret Verkuyl; Wendy Garcia; Oona St-Amant; and Andy Tan is licensed under a Creative Commons Attribution 4.0 International License, except where otherwise noted. ↵
- RegisteredNurseRN. How to take temperature in 6 different ways. https://www.registerednursern.com/take-temperature-6-different-ways/ ↵
- May Clinic Staff. How to take your pulse. https://www.mayoclinic.org/how-to-take-pulse/art-20482581 ↵
- Cleveland Clinic. Apical Pulse. https://my.clevelandclinic.org/health/articles/23346-apical-pulse ↵
- Sorrentino, S. A., & Remmert, L. N. (2019). Mosby's essentials for nursing assistants (6th ed.). Elsevier. ↵
- Nursing Assistant, Chapter 7 by Chippewa Valley Technical College is licensed under a Creative Commons Attribution 4.0 International License , except where otherwise noted. ↵
- Dugan, D. (2020). Nursing assisting: A foundation in caregiving (5th ed.), Chapter 20. Hartman. ↵
- Sorrentino, S. A., & Remmert, L. N. (2019). Mosby's essentials for nursing assistants (6th ed.), Chapter 30. Elsevier. ↵
- World Health Organization. Common Respiratory Diseases. https://www.who.int/health-topics/chronic-respiratory-diseases#tab=tab_3 ↵
- American Lung Association. Oxygen Therapy. https://www.lung.org/lung-health-diseases/lung-procedures-and-tests/oxygen-therapy ↵
- NetCE. (2020, November 1). Respiratory Care: Artificial Airways, Mechanical Ventilation, and Chest Tubes. https://www.netce.com/coursecontent.php?courseid=2094 ↵
How much heat is being generated by a person's body
The number of times a person's heart beats per minute
Breathing, or number of breaths
The amount of force exerted by blood against the arterial and vascular walls
The heart's contracting and pushing blood throughout the body
The heart relaxing and filling with blood again
Low blood pressure
Low blood pressure brought on by moving from a sitting to a standing position
High blood pressure
blockage of the blood vessel
Insufficient blood supply to a given area
A tool used to take blood pressure. It consists of an arm band, a pressure gauge, and sometimes a handpump.
absence of breathing
difficulty breathing
Small blood vessels that cover the body and distribute blood to tissue
breathing abnormally or unhealthily fast
breathing abnormally slowly
Not taking in enough oxygen, or removing enough carbon dioxide. There is too much carbon dioxide in the blood.
Breathing too quickly and taking in too much oxygen
Low oxygen levels
Breathlessness while sitting, which is relieved when standing
A disease that comes on quickly and lasts a relatively short duration
A disease that lasts a long time, and may be a lifelong condition
A progressive disease that causes difficulty breathing due to obstructed airways. Airways may be obstructed by factors such as inflammation and respiratory breakdown.
A respiratory illness caused by lung inflammation and the alveoli filling with fluid
Devices used to keep a person's airways open and unobstructed
Short plastic tube that prevents a tongue from blocking an airway
A tube that is inserted into a person's mouth and sits between their vocal chords
Surgically created opening in the neck that allows air to enter the trachea directly
A machine that moves air into and out of the lungs for people who cannot do it themselves
Caregiving for the Human Condition; an OER for Nursing Assistant Instruction Copyright © by Illinois Central College is licensed under a Creative Commons Attribution 4.0 International License , except where otherwise noted.
Share This Book

IMAGES
VIDEO
COMMENTS
Objective 16 Record vital signs on chart, graph and Nursing Assistant notes. Charting temperature, pulse, respiration (TPR) Report normal and abnormal TPR to licensed nurse. Record on hospital flow sheets, graphic records, and Nursing Assistant notes according to facility policies. Record in the order of TPR. Record temperature.
Answer any questions they may have. Thank them for their participation. Complete Assignment Documentation Form attached and turn in to your lab faculty by due dates. Vital Signs Assignment Documentation Form 10 points: 1/2 point for measurable data 1/2 point for general appearance statement. Date/Time Client initials
Vital signs - Download as a PDF or view online for free. Vital signs - Download as a PDF or view online for free ... Respiration and Blood Pressure are the vital signs, these are also called as cardinal signs." 3. • They reflect the body's physiological status and provide information about the person with current condition or state of ...
To access this valuable resource, healthcare professionals can download the Normal Vital Signs Chart PDF and use it as a reference during routine check-ups, emergencies, or continuous monitoring. Implementing this chart ensures accurate and consistent vital sign documentation, contributing to enhanced healthcare decision-making.
VITAL SIGNS 2/26/2021 JONES H.M-MBA/DMS 1. 2. Temperature, pulse, respiration and blood pressure (B/P) are the most frequent measurements taken by Health Care Providers as they reflect the function of three body processes that are essential for life. Regulation of body temperature Heart function Breathing 2/26/2021 JONES H.M-MBA/DMS 2.
Vital signs are an objective measurement of the essential physiological functions of a living organism. They have the name "vital" as their measurement and assessment is the critical first step for any clinical evaluation. The first set of clinical examinations is an evaluation of the vital signs of the patient. Triage of patients in an urgent/prompt care or an emergency department is based on ...
• Synthesize knowledge about various methods and techniques of vital sign measurement across the lifespan • Integrate knowledge about alternative methods of vital sign measurements • Assess normal and abnormal vital sign values • Evaluate significance of vital sign findings • Generate best interventions based on vital sign findings xiv
Vital signs include temperature recorded in Celsius or Fahrenheit, pulse, respiratory rate, blood pressure, and oxygen saturation using a pulse oximeter. See Figure 1.3.1 1.3. 1 [1] for an image of a nurse obtaining vital signs. Obtaining vital signs may be delegated to unlicensed assistive personnel (UAP) for stable patients, depending on the ...
Blood pressure is used as a vital sign measure. • Since blood pressure is used as a vital sign measure, there are two measurements that are usually taken - the diastolic and systolic pressures. •Systolic Pressure= the peak pressure in the arteries, which occurs when the ventricles of the heart are pumping blood out.
Measuring vital signs is a crucial component in taking care of a client's health. Vital signs help assess the general physical health of a person, provide clues to possible diseases, and help monitor the progress of the client's health status. As a nurse, you will measure and interpret vital signs. Figure 1: Commonly measured vital signs.
Nursing Vital Signs Chart Example (sample) The Nursing Vital Signs Chart PDF is a user-friendly template designed for healthcare practitioners to document and interpret vital signs easily. This printable resource features clear sections for patient identification, date/time stamps, and vital sign entries, including heart rate, blood pressure, respiratory rate, temperature, and oxygen saturation.
Chapter 25: Vital Signs:-Vital signs are indicators of physiologic functioning and reflect the health status of a person. Vital signs are used to monitor the functions of the body. Vital signs include: 1. Temperature (96.7-100) 2. Pulse (60-100bpm) 3. Respiration (12-20) 4. Blood pressure (120/80) 5.
The vital signs are body temperature, pulse, respirations, and blood pressure. Recently, many agencies have designated pain as a fifth vital sign. These signs, which should be looked at together, are checked to monitor the functions of the body. The signs reflect changes in function that otherwise might not be observed.
ment and interpretation of the vital signs are important compo-nents of assessment that can yield information about underlying health status. Client teaching concerning the vital signs is a key aspect of health promotion. Typical or normal ranges of values for vital signs have been established for clients of various age groups (Table 26-1). Dur-
How to take vital signs. Heart rate: place fingers over pulse point (radial artery), count beats for 30 seconds and double for beats per minute; or apical pulse with the stethoscope for 60 seconds. Blood pressure: measured with blood pressure cuff and stethoscope. Respiratory rate: observe the patient's chest/breath without their awareness to ...
This document provides information on vital signs including temperature, pulse, respiration, and blood pressure. It discusses normal ranges for these signs and factors that can influence them. Specific methods for measuring each vital sign are described along with typical equipment. Temperature can be taken orally, axillary, rectally, or via ...
For your convenience, access and download a valuable resource, such as the vital signs chart. Accomplish this task by either: Clicking the "Download Template" or "Use Template" button. Alternatively, locate the chart within Carepatron's template library on the app or website by searching for "Vital Signs Chart." Step 2. Input essential details.
Vital signs vital signs assignments: fundamentals of nursing chapter 24 fundamentals of nursing study guide chapter 24 ati (fundamentals module book) ch. 27 ati. Skip to document. ... (01FM) How to Download Student Data Files; Lab techniques doc - is a manual with practice questions; Calculating Density Practice-1;
W eight has been designated as either the h or sixth vital. sign in adults and children (19, 20). In 2017, 13% o f the adult. population or 1.9 billion persons w orldwide were obese (19). Scott ...
Vital signs are measurements of some mechanisms part of a body's basic functional processes. Vital signs include temperature, pulse, respiration, and blood pressure. It is essential that NAs take vital measurements accurately, and alert the nurse if a resident's vital signs are abnormal. Always obtain vital signs properly and respectfully.
Normal Ranges for Adult Vital Signs. Temperature: Oral 97.6 - 99.6 Rectal 98.6 - 100.6 Axillary 96.6 - 98.6. Pulse: 60 - 90 beats per minute. Respirations: 12 - 28 breaths per minute. Blood pressure: Systolic (top number) should be less than 130 Diastolic (bottom number) should be less than 85.
PDF | Please cite this article as- Sapra A, Malik A, Bhandari P. Vital Sign Assessment. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2020. | Find, read and cite all the research ...
Vital Signs&FHSIS Assignment - Free download as Word Doc (.doc / .docx), PDF File (.pdf), Text File (.txt) or read online for free. Scribd is the world's largest social reading and publishing site.