- Human Reproduction: Reproductive Development Process Words: 690
- The Beginning of Human Life: Fertilization Process Words: 903
- Assisted Reproduction: Description Words: 543
- Human Body. Male and Female Reproductive Systems Words: 2701
- Why Witches Were Accused in Human Reproduction Issues Words: 352
- Student Misconceptions Regarding Reproduction and Heredity Words: 562
- The Reproductive System of Females Words: 388
- Reproductive Adaptations and Embryonic Development Words: 374

Human Reproduction: Fertilization
Introduction, background of the study.
Fertilization is the initial stage of human reproduction or procreation which involves the fusion of a female’s ovum or egg with the male’s sperm in the ampulla of the uterus (Cummings, 2009, p.165). The union occurs when a male and a female engage in sexual intercourse whereby during ejaculation, the sperms in the vagina travel through the cervix into the uterus and finally into the oviduct/fallopian tube. The whole process occurs within thirty minutes after the sperms are introduced into the vagina. Apart from ejaculation during sexual intercourse, the sperms can be introduced into the vagina through artificial insemination or the process of in-vitro fertilization; the union between the egg and the sperm cell can be initiated artificially (Cummings, 2009, p.165). The process through which the sperm cells move from the vagina to the oviduct also referred to as swimming is aided by the whip-like contractions of the tail of the sperm cells and the vigorous contraction of the muscular female uterine walls.
When the sperm cell encounters a mature egg, it releases enzymes found in the Acrosome which digest the outer layer of the ovum thereby allowing the sperm plasma to sail through and fuse with the ovum’s plasma membrane. This is followed by the disconnection of the sperm head from the rest of the sperm cell after which the fertilized egg moves from the oviduct into the uterus.
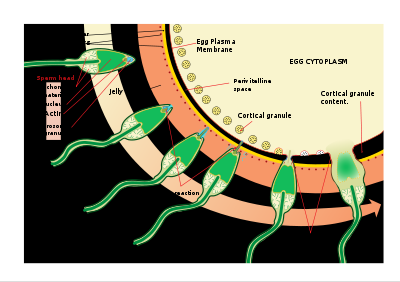
It is evident from the diagram above that only one sperm cell can cross the outer layer of the ovum and fertilize a mature egg. The other sperm cells aid in the chemical changes that occur on the outer layer of the egg that eventually block the entry of additional sperm cells. The subsequent processes after fertilization include implantation followed by fetal development or pregnancy and finally childbirth or parturition.
The report is aimed at outlining the processes involved in human reproduction starting from fertilization through implantation, pregnancy, and finally to childbirth.
The report entails a detailed insight into the process of fertilization, particularly the processes that occur before fertilization such as sperm capacitation and acrosome reaction. It also documents the process of hormonal release that occurs before implantation. The three trimesters of pregnancy are also discussed in detail. Finally, the report provides an account of all three stages of childbirth.
Human Reproduction
Fertilization.
Fertilization entails the fusion of an egg and the sperm cell. However, fertilization in itself entails a chain of episodes whose interruption leads to the failure of the whole process. The process begins with changes in the sperm cell which prepare it for additional processes. Thus the process of fertilization entails sperm capacitation, sperm-Zona Pellucida binding, the acrosome reaction, penetration of the Zona Pellucida, the egg activation and cortical reactions, and finally the Zona reaction (Bowen, 2000, p.1 of 3).
Before fertilization, the fresh sperm cells introduced in the vagina through the process of ejaculation undergo several chemical and structural changes referred to as capacitation. This is the process of removing the seminal components protecting the sperm cells followed by the rearrangement of the lipid and protein constituents of the plasma membrane of the sperm cells (Bowen, 2000, 0.1 of 3). The purpose of capacitation is to increase the motility characteristics of the cells besides destabilizing their plasma membranes in readiness for the subsequent reactions. The interaction of the sperm cell with the Zona Pellucida layer of the ovum is a species-specific reaction that can as well be regarded as binding of the ligand to its specific receptor site. Specific glycoproteins on the surface of the ovum have been shown to act as the sperm receptors whose function is to bind to specific proteins on the sperm cell membrane.
The sperm acrosome consists of Zona-digesting enzymes which play a major role in the acrosome reaction which enables the sperm to sail through the Zona Pellucida of the ovum. The protein receptors on the surface of the ovum take part in a series of reactions that provide the sites for the fusion of the outer layer of the Acrosome to the plasma membrane of the egg. This process leads to the formation of vesicles and seepage of the Acrosomal contents through the process of exocytosis from the sperm head. Progressive Acrosome reaction leads to loss of the Acrosomal contents until the whole sperm head moves through the Zona Pellucida. In case a sperm cell loses its Acrosomal contents before reaching the inner surface of the egg, it fails to fertilize it (Bowen, 2000, p.1 of 3).
Egg activation entails the metabolic and physical changes in the egg which follows the binding of the sperm cell to the egg. The egg is thus activated from its resting state mainly in the second meiotic allotment phase into a zygote (Cummings, 2009, p.166). Subsequent reactions which follow sperm-egg fusion entail hardening of the Zona Pellucida and destruction of the sperm receptors thereby excluding the entry of additional sperm cells into the fertilized egg (Bowen, 2000, p.1 of 3).
Hormonal Release during Implantation
The processes which lead to the formation and maturation of the ova are collectively referred to as the ovarian cycle. They also entail the formation of oocytes and grounding of the uterine wall in readiness for implantation. All these processes are controlled by hormones from the ovary, anterior pituitary, and hypothalamus. The Hypothalamus secretes the Gonadotropin-releasing hormone (GnRH) which acts on the anterior pituitary thus causing the production of the Follicle Stimulating Hormone (FSH) and the Luteinizing Hormone (LH) (Grudzinskas & Yovich, 1995).
FSH mediates the development of the ovarian follicles and the production of another hormone known as estrogen from the follicles. Further growth of the follicles is maintained by the LH which also mediates the full production of estrogen from the follicles. LH further initiates and maintains the formation of female eggs in the ovary and the growth of the Corpus luteum. It also promotes the secretion of estrogen and progesterone among other hormones of the corpus luteum. Besides inhibiting the secretion of GnRH, FSH, and LH from the Hypothalamus and the Anterior Pituitary, Estrogen promotes the development of female sex characteristics. Estrogen and Progesterone prepare the uterine wall in readiness for implantation. The two hormones also promote the growth of mammary glands for milk production. Another hormone, Relaxin produced by the Corpus luteum relaxes the contraction of the uterus thereby promoting implantation (Grudzinskas & Yovich, 1995).
The Three Trimesters of Pregnancy
Pregnancy or fetal development comprises the period between fertilization and childbirth. It is divisible into three stages also known as trimesters which can last up to 12-13 weeks each. These stages entail several rounds of mitosis within the 36-39 weeks of pregnancy involving the zygote that eventually leads to the development of tissues and organs in the fetus (Cummings, 2009, p.166). The first trimester takes 14 weeks during which period the fetus develops from being an embryo to having discrete webbed fingers. It also moves constantly and at the end of the trimester, it develops intact fingerprints and it measures about three inches as illustrated in the picture below.

The second trimester begins at the end of the 14 weeks and lasts up to the 7 th month of pregnancy. During this stage, the fetus grows in length and puts on weight and at the end of this period; it weighs about 3 pounds and about measures about15 inches by length. Additionally, the skeleton changes from the cartilaginous bones to hard bone. The skin also smoothens as it begins to store fats. The eyes begin to open and close depending on the direction of light as shown below.

The third trimester starts immediately after the 7 months of pregnancy and lasts until childbirth. During this stage, the weight of the fetus increases to about 5-7 pounds and it can measure up to 19 inches when stretched. All the body organs are fully developed and the fat deposited in its body gives it a more rounded and smooth shape. As it can be seen in the diagram below, its head is facing the vaginal opening indicating that it is ready to be expelled. However, it should be noted that babies differ broadly at this point.

The Three Stages of Childbirth
Childbirth or parturition marks the end of the pregnancy during which period, one or more infants are expelled from the uterus. Normal human birth is divided into three stages which are preceded by six major phases of changes to the cervix. Pregnancy labor takes up to 12-24 hours for those women giving birth for the first time or shorter than this period for those who have had children (Gjerdingen & Froberg, 1991, p.29). The first stage or the dilation phase can last up to 20 hours. It begins when the cervix dilates up to 3 centimeters wide and widens further up to 10 centimeters during contraction of the uterine muscles.
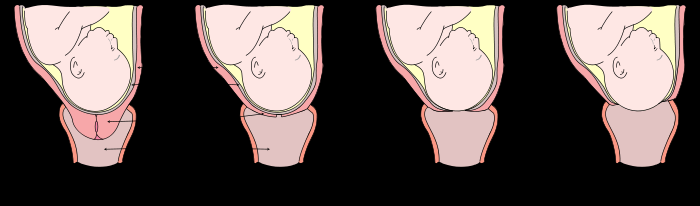
The diagram above shows the various stages of dilation that follow the initial dilation coupled with the active muscular contraction of the uterine muscles.
The second stage or the expulsion phase begins after the cervix has dilated fully and lasts until when the baby is expelled from the uterus. The stage is characterized by increased pressure on the cervix followed by placement of the baby’s head in the pelvis. Assisted by the downward pushing mechanisms from the mother, the head goes past the pubic arc to the outside through the introitus. Further contractions expel the lower body from the uterus. The third stage of childbirth or the placenta stage involves the expulsion of the afterbirth from the uterus. Further loss of blood by the mother is controlled by the uterine contractions after the placenta is expelled (Gjerdingen & Froberg, 1991, p.35).
Conclusions
The report has provided an in-depth account of human reproduction. It provides discussions on the activities which are involved in fertilization and implantation of the mature and fertilized egg on the endometrial wall. In addition, the report gives the details regarding the hormonal release which precedes implantation. Further, the three stages of pregnancy and fetal development are analyzed in this report. Finally, the report describes all three stages of childbirth. From the above discussion, it can be concluded that fertilization is a very important stage in human procreation. It entails a series of stages that lead to the fusion of the sperm cell and the oocytes to form an embryo. The embryo is maintained in the uterus through the process of implantation which enables the fertilized egg to fuse with the endometrial wall. Further divisions of the embryo give rise to tissues and organs observable in a full-grown fetus. The fetus is finally expelled from the uterus through the process of parturition.
Reference list
Cummings, M. 2009. Human heredity: principles and issues (8 th ed.) , Yolanda Cossio Publishers, UK.
Bowen, R. 2000. Fertilization: fertilization and early embryonic development . Web.
Gjerdingen, DK & Froberg, D.G. 1991.The fourth stage of labor: the health of birth mothers and adoptive mothers at six-weeks postpartum. Fam Med. Vol. 23, no.1, pp. 29–35.
Grudzinskas, J.G. & Yovich, J (eds.) 1995. Gametes: The Oocyte. Cambridge: Cambridge University Press.
Cite this paper
- Chicago (N-B)
- Chicago (A-D)
StudyCorgi. (2022, April 10). Human Reproduction: Fertilization. https://studycorgi.com/human-reproduction-fertilization/
"Human Reproduction: Fertilization." StudyCorgi , 10 Apr. 2022, studycorgi.com/human-reproduction-fertilization/.
StudyCorgi . (2022) 'Human Reproduction: Fertilization'. 10 April.
1. StudyCorgi . "Human Reproduction: Fertilization." April 10, 2022. https://studycorgi.com/human-reproduction-fertilization/.
Bibliography
StudyCorgi . "Human Reproduction: Fertilization." April 10, 2022. https://studycorgi.com/human-reproduction-fertilization/.
StudyCorgi . 2022. "Human Reproduction: Fertilization." April 10, 2022. https://studycorgi.com/human-reproduction-fertilization/.
This paper, “Human Reproduction: Fertilization”, was written and voluntary submitted to our free essay database by a straight-A student. Please ensure you properly reference the paper if you're using it to write your assignment.
Before publication, the StudyCorgi editorial team proofread and checked the paper to make sure it meets the highest standards in terms of grammar, punctuation, style, fact accuracy, copyright issues, and inclusive language. Last updated: September 12, 2024 .
If you are the author of this paper and no longer wish to have it published on StudyCorgi, request the removal . Please use the “ Donate your paper ” form to submit an essay.

Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.
18.2 Introduction to the Reproductive System
Created by CK-12 Foundation/Adapted by Christine Miller
It’s All about Sex
A tiny sperm from dad breaks through the surface of a huge egg from mom. Voilà! In nine months, a new son or daughter will be born. Like most other multicellular organisms, human beings reproduce sexually. In human sexual reproduction, males produce sperm and females produce eggs, and a new offspring forms when a sperm unites with an egg. How do sperm and eggs form? And how do they arrive together at the right place and time so they can unite to form a new offspring? These are functions of the reproductive system.
What Is the Reproductive System?
The reproductive system is the human organ system responsible for the production and fertilization of gametes (sperm or eggs) and, in females, the carrying of a fetus. Both male and female reproductive systems have organs called gonad s that produce gametes. A gamete is a haploid cell that combines with another haploid gamete during fertilization , forming a single diploid cell called a zygote . Besides producing gametes, the gonads also produce sex hormones. Sex hormones are endocrine hormones that control the development of sex organs before birth, sexual maturation at puberty, and reproduction once sexual maturation has occurred. Other reproductive system organs have various functions, such as maturing gametes, delivering gametes to the site of fertilization, and providing an environment for the development and growth of an offspring.
Sex Differences in the Reproductive System
The reproductive system is the only human organ system that is significantly different between males and females. Embryonic structures that will develop into the reproductive system start out the same in males and females, but by birth, the reproductive systems have differentiated. How does this happen?
Sex Differentiation
Starting around the seventh week after conception in genetically male (XY) embryos, a gene called SRY on the Y chromosome (shown in Figure 18.2.2) initiates the production of multiple proteins. These proteins cause undifferentiated gonadal tissue to develop into male gonads (testes). The male gonads then secrete hormones — including the male sex hormone testosterone — that trigger other changes in the developing offspring (now called a fetus), causing it to develop a complete male reproductive system. Without a Y chromosome, an embryo will develop female gonads (ovaries) that will produce the female sex hormone estrogen. Estrogen, in turn, will lead to the formation of the other organs of a normal female reproductive system.
Homologous Structures
Undifferentiated embryonic tissues develop into different structures in male and female fetus es . Structures that arise from the same tissues in males and females are called homologous structure s . The male testes and female ovaries, for example, are homologous structures that develop from the undifferentiated gonads of the embryo. Likewise, the male penis and female clitoris are homologous structures that develop from the same embryonic tissues.
Sex Hormones and Maturation
Male and female reproductive systems are different at birth, but they are immature and incapable of producing gametes or sex hormones. Maturation of the reproductive system occurs during puberty, when hormones from the hypothalamus and pituitary gland stimulate the testes or ovaries to start producing sex hormones again. The main sex hormones are testosterone in males and estrogen in females. Sex hormones, in turn, lead to the growth and maturation of the reproductive organs, rapid body growth, and the development of secondary sex characteristics. Secondary sex characteristic s are traits that are different in mature males and females, but are not directly involved in reproduction. They include facial hair in males and breasts in females.
Male Reproductive System
The main structures of the male reproductive system are external to the body and illustrated in Figure 18.2.3. The two testes (singular, testis) hang between the thighs in a sac of skin called the scrotum . The testes produce both sperm and testosterone . Resting atop each testis is a coiled structure called the epididymis (plural, epididymes). The function of the epididymes is to mature and store sperm. The penis is a tubular organ that contains the urethra and has the ability to stiffen during sexual arousal. Sperm passes out of the body through the urethra during a sexual climax (orgasm). This release of sperm is called ejaculation.
In addition to these organs, the male reproductive system consists of several ducts and glands that are internal to the body. The ducts, which include the vas deferens (also called the ductus deferens), transport sperm from the epididymis to the urethra . The glands, which include the prostate gland and seminal vesicles , produce fluids that become part of semen. Semen is the fluid that carries sperm through the urethra and out of the body. It contains substances that control pH and provide sperm with nutrients for energy.
Female Reproductive System
The main structures of the female reproductive system are internal to the body and shown in the following figure. They include the paired ovaries , which are small, ovoid structures that produce ova and secrete estrogen . The two oviducts (sometimes called Fallopian tubes or uterine tubes) start near the ovaries and end at the uterus . Their function is to transport ova from the ovaries to the uterus. If an egg is fertilized, it usually occurs while it is traveling through an oviduct. The uterus is a pear-shaped muscular organ that functions to carry a fetus until birth. It can expand greatly to accommodate a growing fetus, and its muscular walls can contract forcefully during labour to push the baby out of the uterus and into the vagina. The vagina is a tubular tract connecting the uterus to the outside of the body. The vagina is where sperm are usually deposited during sexual intercourse and ejaculation . The vagina is also called the birth canal because a baby travels through the vagina to leave the body during birth.
The external structures of the female reproductive system are referred to collectively as the vulva . They include the clitoris , which is homologous to the male penis. They also include two pairs of labia (singular, labium), which surround and protect the openings of the urethra and vagina.
18.2 Summary
- The reproductive system is the human organ system responsible for the production and fertilization of gametes and, in females, the carrying of a fetus .
- Both male and female reproductive systems have organs called gonads ( testes in males, ovaries in females) that produce gametes ( sperm or ova) and sex hormones (such as testosterone in males and estrogen in females). Sex hormones are endocrine hormones that control the prenatal development of reproductive organs, sexual maturation at puberty, and reproduction after puberty .
- The reproductive system is the only organ system that is significantly different between males and females. A Y-chromosome gene called SRY is responsible for undifferentiated embryonic tissues developing into a male reproductive system. Without a Y chromosome, the undifferentiated embryonic tissues develop into a female reproductive system.
- Structures such as testes and ovaries that arise from the same undifferentiated embryonic tissues in males and females are called homologous structures .
- Male and female reproductive systems are different at birth, but at that point, they are immature and nonfunctioning. Maturation of the reproductive system occurs during puberty, when hormones from the hypothalamus and pituitary gland stimulate the gonads to produce sex hormones again. The sex hormones, in turn, cause the changes of puberty.
- Male reproductive system organs include the testes , epididymis , penis , vas deferens , prostate gland , and seminal vesicles .
- Female reproductive system organs include the ovaries , oviducts , uterus , vagina , clitoris , and labia .
18.2 Review Questions
- What is the reproductive system?
- Explain the difference between the vulva and the vagina.
18.2 Explore More
Sex Determination: More Complicated Than You Thought, TED-Ed, 2012.
The evolution of animal genitalia – Menno Schilthuizen, TED-Ed, 2017.
Hormones and Gender Transition, Reactions, 2015.
Attributions
Figure 18.2.1
Sperm-egg by Unknown author on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/public_domain).
Figure 18.2.2
Y Chromosome by Christinelmiller on Wikimedia Commons is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0) license.
Figure 18.2.3
3D_Medical_Animation_Vas_Deferens by https://www.scientificanimations.com on Wikimedia Commons is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0) license.
Figure 18.2.4
Blausen_0399_FemaleReproSystem_01 by BruceBlaus on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
References
Blausen.com Staff. (2014). Medical gallery of Blausen Medical 2014. WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436.
Reactions. (2015, June 8). Hormones and gender transition. YouTube. https://www.youtube.com/watch?v=l5knvmy1Z3s&feature=youtu.be
TED-Ed. (2012, April 23). Sex determination: More complicated than you thought. YouTube. https://www.youtube.com/watch?v=kMWxuF9YW38&feature=youtu.be
TED-Ed. (2017, April 24). The evolution of animal genitalia – Menno Schilthuizen. YouTube. https://www.youtube.com/watch?v=vcPJkz-D5II&feature=youtu.be
The male reproductive cell.
The body system by which humans reproduce and bear live offspring.
One of a pair of organs that secrete sex hormones and produce gametes; testis in males and ovary in females.
A mature haploid male or female germ cell which is able to unite with another of the opposite sex in sexual reproduction to form a zygote.
The term used when a cell has half the usual number of chromosomes.
The fusion of haploid gametes, egg and sperm, to form the diploid zygote.
The union of the sperm cell and the egg cell. Also known as a fertilized ovum, the zygote begins as a single cell but divides rapidly in the days following fertilization. After this two-week period of cell division, the zygote eventually becomes an embryo.
An endocrine hormone secreted mainly by gonads that controls sexual development and reproduction.
An unborn offspring of a mammal, in particular an unborn human baby more than eight weeks after conception.
Structures that are similar in related species because it was inherited from a common ancestor; or structure that develops from the same undifferentiated embryonic tissue in males and females of the same species, such as the testis and ovary in humans.
A part of the brain that secretes hormones and connects the brain with the endocrine system.
The master gland of the endocrine system that secretes many hormones, the majority of which regulate other endocrine glands.
The male sex hormone secreted mainly by the testes.
The female sex hormone secreted mainly by the ovaries.
A trait that is different in males and females but is not directly involved in reproduction, such as male facial hair and female breasts.
Two male reproductive organs that produce sperm and secrete testosterone; male gonad.
A pouch-like external structure of the male reproductive system, located behind the penis, that contains the testes, epididymes, and part of the vas deferens.
One of two male reproductive organs where sperm mature and are stored until they leave the body during ejaculation.
The male reproductive organ containing the urethra, through which semen and urine pass out of the body.
One of a pair of thin tubes that transports sperm from an epididymis to an ejaculatory duct during ejaculation; also called sperm duct.
A tube-like organ of the urinary system that carries urine out of the body from the bladder and, in males, also carries semen out of the body.
A gland in the male reproductive system that secretes fluid into semen and provides nourishing substances to sperm.
One of a pair of glands of the male reproductive system that secretes fluid into semen.
Fluid containing sperm and glandular secretions, which nourishes sperm and carries them through the urethra and out of the body.
A pair of female reproductive organs that produces eggs and secretes estrogen.
The gamete produced by a female.
One of two female reproductive organs that carry eggs from an ovary to the uterus and are the site where fertilization usually takes place.
The female reproductive organ in which first an embryo and then a fetus grows and develops until birth.
The female reproductive organ that receives sperm during sexual intercourse and provides a passageway for a baby to leave the mother’s body during birth.
The physical activity of sex between two people.
The process in males in which muscle contractions propel sperm from the epididymes and out through the urethra in semen.
External female reproductive structures, including the clitoris, labia, and vaginal and urethral openings.
The small, sensitive external female organ that is part of the vulva and may lead to sexual arousal and/or orgasm when stimulated.
The “lips” of the vulva, consisting of folds of tissue that protect the urethral and vaginal openings.
A hormone is a signaling molecule produced by glands in multicellular organisms that target distant organs to regulate physiology and behavior.
A period during which humans become sexually mature.
Human Biology Copyright © 2020 by Christine Miller is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License , except where otherwise noted.
Share This Book
18.3 Human Reproduction
Learning objectives.
- Describe human testicular and ovarian reproductive anatomies
- Describe spermatogenesis and oogenesis and discuss their differences and similarities
- Describe the role of hormones in human reproduction
- Describe the roles of reproductive hormones
As in all animals, the adaptations for reproduction in humans are complex. They involve specialized and different anatomies in the two sexes, a hormone regulation system, and specialized behaviors regulated by the brain and endocrine system.
Human Reproductive Anatomy
The reproductive tissues of male and female humans develop similarly in utero until about the seventh week of gestation when, in some cases, a low level of the hormone testosterone is released from the gonads. Testosterone causes the primitive gonads to differentiate into sexual organs, such as the scrotum and penis. When testosterone is absent, the primitive gonads develop into ovaries. Tissues that produce a penis in males produce a clitoris in females. The tissue that will become the scrotum in a male becomes the labia in a female. Thus the male and female anatomies arise from a divergence in the development of what were once common embryonic structures.
Male Reproductive Anatomy
Sperm are immobile at body temperature; therefore, the testes are external to the body so that a correct temperature is maintained for motility. In land mammals, including humans, the pair of testes must be suspended outside the body so the environment of the sperm is about 2 °C lower than body temperature to produce viable sperm. If the testes do not descend through the abdominal cavity during fetal development, the individual has reduced fertility.
The scrotum houses the testicles or testes (singular: testis), and provides passage for blood vessels, nerves, and muscles related to testicular function. The testes are a pair of male gonads that produce sperm and reproductive hormones. Each testis is approximately 2.5 by 3.8 cm (1.5 by 1 inch) in size and divided into wedge-shaped lobes by septa. Coiled in each wedge are seminiferous tubules that produce sperm.
The penis drains urine from the urinary bladder and is a copulatory organ during intercourse ( Figure 18.12 ; Table 18.1 ). The penis contains three tubes of erectile tissue that become engorged with blood, making the penis erect, in preparation for intercourse. The organ is inserted into the vagina culminating with an ejaculation. During orgasm, the accessory organs and glands connected to the testes contract and empty the semen (containing sperm) into the urethra and the fluid is expelled from the body by muscular contractions causing ejaculation. After intercourse, the blood drains from the erectile tissue and the penis becomes flaccid.
Semen is a mixture of sperm (about five percent of the total) and fluids from accessory glands that contribute most of the semen’s volume. Sperm are haploid cells, consisting of a flagellum for motility, a neck that contains the cell’s energy-producing mitochondria, and a head that contains the genetic material ( Figure 18.11 ). An acrosome (acrosomal vesicle) is found at the top of the head of the sperm. This structure contains enzymes that can digest the protective coverings that surround the egg and allow the sperm to fuse with the egg. An ejaculate will contain from two to five milliliters of fluid and from 50–120 million sperm per milliliter.
Sperm form in the walls of seminiferous tubules that are coiled inside the testes ( Figure 18.12 ; Table 18.1 ). The walls of the seminiferous tubules are made up of the developing sperm cells, with the least developed sperm at the periphery of the tubule and the fully developed sperm next to the lumen. The sperm cells are associated with Sertoli cells that nourish and promote the development of the sperm. Other cells present between the walls of the tubules are the interstitial cells of Leydig , which produce testosterone once the male reaches adolescence.
When the sperm have developed flagella they leave the seminiferous tubules and enter the epididymis ( Figure 18.12 ; Table 18.1 ). This structure lies along the top and posterior of the testes and is the site of sperm maturation. The sperm leave the epididymis and enter the vas deferens, which carries the sperm behind the bladder, and forms the ejaculatory duct with the duct from the seminal vesicles. During a vasectomy, a section of the vas deferens is removed, preventing sperm (but not the secretions of the accessory glands) from being passed out of the body during ejaculation and preventing fertilization.
The bulk of the semen comes from the accessory glands associated with the male reproductive system. These are the seminal vesicles , the prostate gland , and the bulbourethral gland ( Figure 18.12 ; Table 18.1 ). The secretions from the accessory glands provide important compounds for the sperm including nutrients, electrolytes, and pH buffering. There are also coagulation factors that affect sperm delivery and motility.
Visual Connection
Which of the following statements about the testicular reproductive system is false?
- The vas deferens carries sperm from the testes to the seminal vesicles.
- The ejaculatory duct joins the urethra.
- Both the prostate and the bulbourethral glands produce components of the semen.
- The prostate gland is located in the testes.
| Organ | Location | Function |
|---|---|---|
| Scrotum | External | Supports testes and regulates their temperature |
| Penis | External | Delivers urine, copulating organ |
| Testes | Internal | Produce sperm and male hormones |
| Seminal Vesicles | Internal | Contribute to semen production |
| Prostate Gland | Internal | Contributes to semen production |
| Bulbourethtral Glands | Internal | Neutralize urine in urethra |
Female Reproductive Anatomy
A number of female reproductive structures are exterior to the body. These include the breasts and the vulva, which consists of the mons pubis, clitoris , labia majora , labia minora , and the vestibular glands ( Figure 18.13 ; Table 18.2 ).
The breasts consist of mammary glands and fat. Each gland consists of 15 to 25 lobes that have ducts that empty at the nipple and that supply the nursing child with nutrient- and antibody-rich milk to aid development and protect the child.
Internal female reproductive structures include ovaries, oviducts, the uterus, and the vagina ( Figure 18.13 ; Table 18.2 ). The pair of ovaries is held in place in the abdominal cavity by a system of ligaments. The outermost layer of the ovary is made up of follicles, each consisting of one or more follicular cells that surround, nourish, and protect a single egg. During the menstrual period, a batch of follicular cells develops and prepares their eggs for release. At ovulation, one follicle ruptures and one egg is released. Following ovulation, the follicular tissue that surrounded the ovulated egg stays within the ovary and grows to form a solid mass called the corpus luteum . The corpus luteum secretes additional estrogen and the hormone progesterone that helps maintain the uterine lining during pregnancy. The ovaries also produce hormones, such as estrogen.
The oviducts , or fallopian tubes, extend from the uterus in the lower abdominal cavity to the ovaries, but they are not in contact with the ovaries. The lateral ends of the oviducts flare out into a trumpet-like structure and have a fringe of finger-like projections called fimbrae. When an egg is released at ovulation, the fimbrae help the nonmotile egg enter into the tube. The walls of the oviducts have a ciliated epithelium over smooth muscle. The cilia beat, and the smooth muscle contracts, moving the egg toward the uterus. Fertilization usually takes place within the oviduct and the developing embryo is moved toward the uterus. It usually takes the egg or embryo a week to travel through the oviduct.
Sterilization in females is called a tubal ligation; it is analogous to a vasectomy in males in that the oviducts are severed and sealed, preventing sperm from reaching the egg.
The uterus is a structure about the size of a person’s fist. The uterus has a thick muscular wall and is lined with an endometrium rich in blood vessels and mucus glands that develop and thicken during the female cycle. Thickening of the endometrium prepares the uterus to receive the fertilized egg or zygote, which will then implant itself in the endometrium. The uterus supports the developing embryo and fetus during gestation. Contractions of the smooth muscle in the uterus aid in forcing the baby through the vagina during labor. If fertilization does not occur, a portion of the lining of the uterus sloughs off during each menstrual period. The endometrium builds up again in preparation for implantation. Part of the uterus, called the cervix, protrudes into the top of the vagina.
The vagina is a muscular tube that serves several purposes. It allows menstrual flow to leave the body. It is the receptacle for the penis during intercourse and the pathway for the delivery of offspring.
| Organ | Location | Function |
|---|---|---|
| Clitoris | External | Sensory organ |
| Mons pubis | External | Fatty area overlying pubic bone |
| Labia majora | External | Covers labia minora; contains sweat and sebaceous glands |
| Labia minora | External | Covers vestibule |
| Greater vestibular glands | External | Secrete mucus; lubricate vagina |
| Breast | External | Produces and delivers milk |
| Ovaries | Internal | Produce and develop eggs |
| Oviducts | Internal | Transport egg to uterus; site of fertilization |
| Uterus | Internal | Supports developing embryo |
| Vagina | Internal | Common tube for intercourse, birth canal, passing menstrual flow |
Gametogenesis (Spermatogenesis and Oogenesis)
Gametogenesis, the production of sperm and eggs, involves the process of meiosis. During meiosis, two nuclear divisions separate the paired chromosomes in the nucleus and then separate the chromatids that were made during an earlier stage of the cell’s life cycle. Meiosis and its associated cell divisions produces haploid cells with half of each pair of chromosomes normally found in diploid cells. The production of sperm is called spermatogenesis and the production of eggs is called oogenesis .
Spermatogenesis
Spermatogenesis occurs in the wall of the seminiferous tubules, with the most primitive cells at the periphery of the tube and the most mature sperm at the lumen of the tube ( Figure 18.14 ). Immediately under the capsule of the tubule are diploid, undifferentiated cells. These stem cells, each called a spermatogonium (pl. spermatogonia), go through mitosis to produce one cell that remains as a stem cell and a second cell called a primary spermatocyte that will undergo meiosis to produce sperm.
The diploid primary spermatocyte goes through meiosis I to produce two haploid cells called secondary spermatocytes. Each secondary spermatocyte divides after meiosis II to produce two cells called spermatids. The spermatids eventually reach the lumen of the tubule and grow a flagellum, becoming sperm cells. Four sperm result from each primary spermatocyte that goes through meiosis.
Link to Learning
Visit this site to see the process of spermatogenesis.
Oogenesis occurs in the outermost layers of the ovaries. As with sperm production, oogenesis starts with a germ cell. In oogenesis, this germ cell is called an oogonium and forms during the embryological development of the individual. The oogonium undergoes mitosis to produce about one to two million oocytes by the time of birth.
The primary oocytes begin meiosis before birth ( Figure 18.15 ). However, the meiotic division is arrested in its progress in the first prophase stage. At the time of birth, all future eggs are in prophase I. This situation is in contrast with the testicular reproductive system in which sperm are produced continuously throughout the life of the individual. Starting at adolescence, anterior pituitary hormones cause the development of a few follicles in an ovary each month. This results in a primary oocyte finishing the first meiotic division. The cell divides unequally, with most of the cytoplasm and organelles going to one cell, called a secondary oocyte, and only one set of chromosomes and a small amount of cytoplasm going to the other cell. This second cell is called a polar body and usually dies. Cell division is again arrested, this time at metaphase II. At ovulation, this secondary oocyte is released and travels toward the uterus through the oviduct. If the secondary oocyte is fertilized, the cell continues through meiosis II, producing a second polar body and haploid egg, which fuses with the haploid sperm to form a fertilized egg (zygote) containing all 46 chromosomes.
Hormonal Control of Reproduction
The human reproductive cycles are controlled by the interaction of hormones from the hypothalamus and anterior pituitary with hormones from reproductive tissues and organs. The hypothalamus monitors and causes the release of hormones from the anterior pituitary gland. When the reproductive hormone is required, the hypothalamus sends a gonadotropin-releasing hormone (GnRH) to the anterior pituitary. This causes the release of follicle stimulating hormone (FSH) and luteinizing hormone (LH) from the anterior pituitary into the blood. Although these hormones are named after their functions in female reproduction, they are produced in both sexes and play important roles in controlling reproduction. Other hormones have specific functions in the male and female reproductive systems.
Male Hormones
At the onset of puberty, the hypothalamus causes the release of FSH and LH into the male system for the first time. FSH enters the testes and stimulates the Sertoli cells located in the walls of the seminiferous tubules to begin promoting spermatogenesis ( Figure 18.16 ). LH also enters the testes and stimulates the interstitial cells of Leydig, located in between the walls of the seminiferous tubules, to make and release testosterone into the testes and the blood.
Testosterone stimulates spermatogenesis. During adolescence, this hormone is also responsible for a deepening of the voice, the growth of facial, axillary, and pubic hair, an increase in muscle bulk, and the beginnings of the sex drive.
A negative feedback system occurs in the male with rising levels of testosterone acting on the hypothalamus and anterior pituitary to inhibit the release of GnRH, FSH, and LH. In addition, the Sertoli cells produce the hormone inhibin , which is released into the blood when the sperm count is too high. This inhibits the release of GnRH and FSH, which will cause spermatogenesis to slow down. If the sperm count reaches a low of 20 million/mL, the Sertoli cells cease the release of inhibin, and the sperm count increases.
Female Hormones
The control of reproduction in females is more complex. The female reproductive cycle is divided into the ovarian cycle and the menstrual cycle. The ovarian cycle governs the preparation of endocrine tissues and release of eggs, while the menstrual cycle governs the preparation and maintenance of the uterine lining ( Figure 18.17 ). These cycles are coordinated over a 22–32 day cycle, with an average length of 28 days.
As with the male, the GnRH from the hypothalamus causes the release of the hormones FSH and LH from the anterior pituitary. In addition, estrogen and progesterone are released from the developing follicles. As with testosterone in males, estrogen is responsible for the secondary sexual characteristics of females. These include breast development, flaring of the hips, and a shorter period for bone growth.
The Ovarian Cycle and the Menstrual Cycle
The ovarian and menstrual cycles are regulated by hormones of the hypothalamus, pituitary, and ovaries ( Figure 18.17 ). The ebb and flow of the hormones causes the ovarian and menstrual cycles to advance. The ovarian and menstrual cycles occur concurrently. The first half of the ovarian cycle is the follicular phase. Slowly rising levels of FSH cause the growth of follicles on the surface of the ovary. This process prepares the egg for ovulation. As the follicles grow, they begin releasing estrogen. The first few days of this cycle coincide with menstruation or the sloughing off of the functional layer of the endometrium in the uterus. After about five days, estrogen levels rise and the menstrual cycle enters the proliferative phase. The endometrium begins to regrow, replacing the blood vessels and glands that deteriorated during the end of the last cycle.
Which of the following statements about hormone regulation of the ovarian and menstrual cycle is false?
- LH and FSH are produced in the pituitary, and estrogen and progesterone are produced in the ovaries.
- Estradiol and progesterone secreted from the corpus luteum cause the endometrium to thicken.
- Both progesterone and estrogen are produced by the follicles.
- Secretion of GnRH by the hypothalamus is inhibited by low levels of estrogen but stimulated by high levels of estrogen.
Just prior to the middle of the cycle (approximately day 14), the high level of estrogen causes FSH and especially LH to rise rapidly then fall. The spike in LH causes the most mature follicle to rupture and release its egg. This is ovulation . The follicles that did not rupture degenerate and their eggs are lost. The level of estrogen decreases when the extra follicles degenerate.
Following ovulation, the ovarian cycle enters its luteal phase and the menstrual cycle enters its secretory phase, both of which run from about day 15 to 28. The luteal and secretory phases refer to changes in the ruptured follicle. The cells in the follicle undergo physical changes and produce a structure called a corpus luteum. The corpus luteum produces estrogen and progesterone. The progesterone facilitates the regrowth of the uterine lining and inhibits the release of further FSH and LH. The uterus is being prepared to accept a fertilized egg, should it occur during this cycle. The inhibition of FSH and LH prevents any further eggs and follicles from developing, while the progesterone is elevated. The level of estrogen produced by the corpus luteum increases to a steady level for the next few days.
If no fertilized egg is implanted into the uterus, the corpus luteum degenerates and the levels of estrogen and progesterone decrease. The endometrium begins to degenerate as the progesterone levels drop, initiating the next menstrual cycle. The decrease in progesterone also allows the hypothalamus to send GnRH to the anterior pituitary, releasing FSH and LH and starting the cycles again.
Career Connection
Reproductive endocrinologist.
A reproductive endocrinologist is a physician who treats a variety of hormonal disorders related to reproduction and infertility in people of any gender. The disorders include menstrual problems, infertility, pregnancy loss, sexual dysfunction, and menopause. Doctors may use fertility drugs, surgery, or assisted reproductive techniques (ART) in their therapy. ART involves the use of procedures to manipulate the egg or sperm to facilitate reproduction, such as in vitro fertilization.
Reproductive endocrinologists undergo extensive medical training, first in a four-year residency in obstetrics and gynecology, then in a three-year fellowship in reproductive endocrinology. To be board certified in this area, the physician must pass written and oral exams in both areas.
Pregnancy begins with the fertilization of an egg and continues through to the birth of the individual. The length of time of gestation , or the gestation period , in humans is 266 days and is similar in other great apes.
Within 24 hours of fertilization, the egg nucleus has finished meiosis and the egg and sperm nuclei fuse. With fusion, the cell is known as a zygote. The zygote initiates cleavage and the developing embryo travels through the oviduct to the uterus. The developing embryo must implant into the wall of the uterus within seven days, or it will deteriorate and die. The outer layers of the developing embryo or blastocyst grow into the endometrium by digesting the endometrial cells, and healing of the endometrium closes up the blastocyst into the tissue. Another layer of the blastocyst, the chorion, begins releasing a hormone called human beta chorionic gonadotropin (β-HCG) , which makes its way to the corpus luteum and keeps that structure active. This ensures adequate levels of progesterone that will maintain the endometrium of the uterus for the support of the developing embryo. Pregnancy tests determine the level of β-HCG in urine or serum. If the hormone is present, the test is positive.
The gestation period is divided into three equal periods or trimesters. During the first two-to-four weeks of the first trimester, nutrition and waste are handled by the endometrial lining through diffusion. As the trimester progresses, the outer layer of the embryo begins to merge with the endometrium, and the placenta forms. The placenta takes over the nutrient and waste requirements of the embryo and fetus, with the gestational parent’s blood passing nutrients to the placenta and removing waste from it. Chemicals from the fetus, such as bilirubin, are processed by the gestational parent’s liver for elimination. Some of the pregnant person’s immunoglobulins will pass through the placenta, providing passive immunity against some potential infections.
Internal organs and body structures begin to develop during the first trimester. By five weeks, limb buds, eyes, the heart, and liver have been basically formed. By eight weeks, the term fetus applies, and the body is essentially formed ( Figure 18.18 a ). The individual is about five centimeters (two inches) in length and many of the organs, such as the lungs and liver, are not yet functioning. Exposure to any toxins is especially dangerous during the first trimester, as all of the body’s organs and structures are going through initial development. Anything that interferes with chemical signaling during that development can have a severe effect on the fetus’ survival.
During the second trimester, the fetus grows to about 30 cm (about 12 inches) ( Figure 18.18 b ). It becomes active and the pregnant person usually feels the first movements. All organs and structures continue to develop. The placenta has taken over the functions of nutrition and waste elimination and the production of estrogen and progesterone from the corpus luteum, which has degenerated. The placenta will continue functioning up through the delivery of the baby. During the third trimester, the fetus grows to 3 to 4 kg (6.5–8.5 lbs.) and about 50 cm (19–20 inches) long ( Figure 18.18 c ). This is the period of the most rapid growth during the pregnancy as all organ systems continue to grow and develop.
Visit this website to see the stages of human fetal development.
Labor is the muscular contractions to expel the fetus and placenta from the uterus. Toward the end of the third trimester, estrogen causes receptors on the uterine wall to develop and bind the hormone oxytocin. At this time, the baby reorients, facing forward and down with the back or crown of the head engaging the cervix (uterine opening). This causes the cervix to stretch and nerve impulses are sent to the hypothalamus, which signals the release of oxytocin from the posterior pituitary. Oxytocin causes smooth muscle in the uterine wall to contract. At the same time, the placenta releases prostaglandins into the uterus, increasing the contractions. A positive feedback relay occurs between the uterus, hypothalamus, and the posterior pituitary to assure an adequate supply of oxytocin. As more smooth muscle cells are recruited, the contractions increase in intensity and force.
There are three stages to labor. During stage one, the cervix thins and dilates. This is necessary for the baby and placenta to be expelled during birth. The cervix will eventually dilate to about 10 cm. During stage two, the baby is expelled from the uterus. The uterus contracts and, in most cases, the person giving birth pushes as they compress the abdominal muscles to aid the delivery. The last stage is the passage of the placenta after the baby has been born and the organ has completely disengaged from the uterine wall. If labor should stop before stage two is reached, synthetic oxytocin, known as Pitocin, can be administered to restart and maintain labor.
This book may not be used in the training of large language models or otherwise be ingested into large language models or generative AI offerings without OpenStax's permission.
Want to cite, share, or modify this book? This book uses the Creative Commons Attribution License and you must attribute OpenStax.
Access for free at https://openstax.org/books/concepts-biology/pages/1-introduction
- Authors: Samantha Fowler, Rebecca Roush, James Wise
- Publisher/website: OpenStax
- Book title: Concepts of Biology
- Publication date: Apr 25, 2013
- Location: Houston, Texas
- Book URL: https://openstax.org/books/concepts-biology/pages/1-introduction
- Section URL: https://openstax.org/books/concepts-biology/pages/18-3-human-reproduction
© Jul 10, 2024 OpenStax. Textbook content produced by OpenStax is licensed under a Creative Commons Attribution License . The OpenStax name, OpenStax logo, OpenStax book covers, OpenStax CNX name, and OpenStax CNX logo are not subject to the Creative Commons license and may not be reproduced without the prior and express written consent of Rice University.
Human Reproduction
(0 reviews)
Hala Bastawros, Iowa State University
Copyright Year: 2023
Last Update: 2024
Publisher: Iowa State University Digital Press
Language: English
Formats Available
Conditions of use.
Table of Contents
- About this book
- The Female Reproductive System
- Female Endocrinology
- The Male Reproductive System
- Male Endocrinology
- Stages of Life
- Gametogenesis, Fertilization, and Implantation
- Genetic Disorders
- Normal Pregnancy
- Labor and Birth
- Contraception
- Infertility
- Sexual Transmitted Diseases
- Pelvic Pain
- About the Author
Ancillary Material
About the book.
This open textbook is designed to provide a deep understanding of the biological and biomedical aspects of human reproduction, covering a wide range of topics from basic reproductive biology to clinical applications. The book starts with foundational knowledge and progresses to more advanced topics while also including real-world clinical orientation for practical contexts.
About the Contributors
Dr. Bastawros earned her M.D. from Cairo University School of Medicine, Cairo, Egypt, in 1992, and obtained her USA Medical Certificate in 1999. With extensive experience in internal medicine, she has practiced in numerous teaching facilities. Dr. Bastawros is well-versed in instructing clinical signs, pathophysiology, and the effective management of various diseases. Since 2008, Dr. Bastawros has been an esteemed faculty member at Iowa State University, dedicating her efforts to educating pre-health professional career students.
Contribute to this Page
Development of the Reproductive System
Written by Vicky Theakston
Last updated July 17, 2024 • 21 Revisions •
The reproductive system is a collection of internal and external sex organs which work together for the purpose of sexual reproduction.
The development of these reproductive organs begins at an early stage in the embryo. There is a close link throughout with the development of the urinary system .
This article will look at the origins of both male and female sex organs; including the gonads, internal genitalia, and external genitalia.
Premium Feature
Indifferent stage.
In the first stage of gonadal development, it is impossible to distinguish between the male and female gonad. Thus, it is known as the indifferent stage .
The gonads begin as genital ridges – a pair of longitudinal ridges derived from intermediate mesoderm and overlying epithelium. They initially do not contain any germ cells.
In the fourth week, germ cells begin to migrate from the endoderm lining of the yolk sac to the genital ridges, via the dorsal mesentery of the hindgut. They reach the genital ridges in the sixth week.
Simultaneously, the epithelium of the genital ridges proliferates and penetrates the intermediate mesoderm to form the primitive sex cords . The combination of germ cells and primitive sex cords forms the indifferent gonad – from which development into the testes or ovaries can occur.
In a male embryo, the XY sex chromosomes are present. The Y chromosome contains the SRY gene , which stimulates the development of the primitive sex cords to form testis (medullary) cords. The tunica albuginea, a fibrous connective tissue layer, forms around the cords.
A portion of the testis cords breaks off to form the future rete testis. The remaining cords contain two types of cells:
- Sertoli cells (derived from the surface epithelium of the gland).
In puberty, these cords acquire a lumen and become the seminiferous tubules – the site within which sperm will be formed.
Located between the testis cords are the Leydig cells (derived from the intermediate mesoderm). In the eighth week, they begin production of testosterone – which drives differentiation of the internal and external genitalia.
In a female embryo, the XX sex chromosomes are present. As there is no Y chromosome, there is no SRY gene to influence development. Without it, the primitive sex cords degenerate and do not form the testis cords.
Instead, the epithelium of the gonad continues to proliferate, producing cortical cords . In the third month, these cords break up into clusters, surrounding each oogonium (germ cell) with a layer of epithelial follicular cells, forming a primordial follicle.
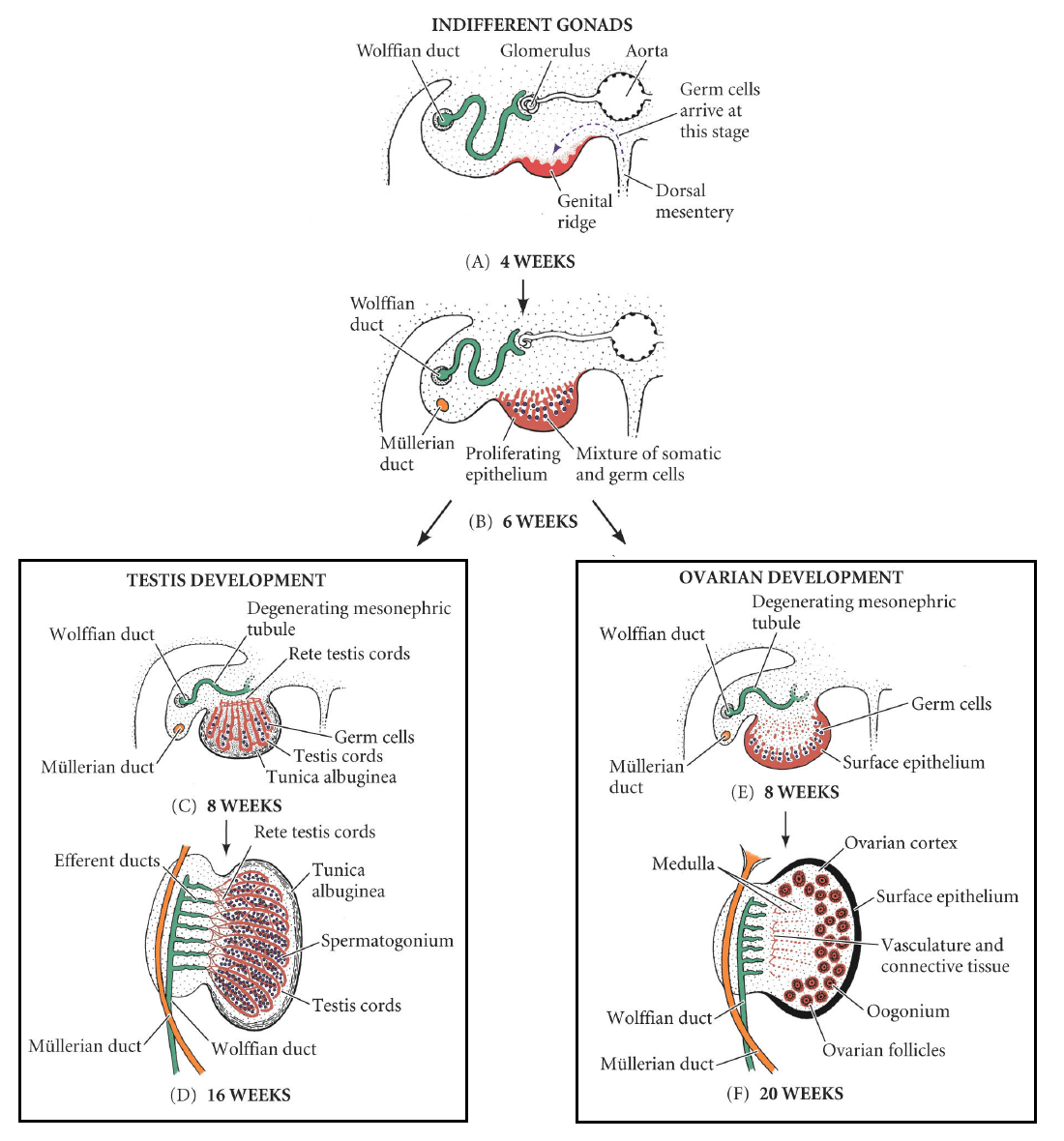
Fig 1 Development of the male and female gonad from the indifferent gonad.
The Internal Genitalia
In the first weeks of urogenital development, all embryos have two pairs of ducts, both ending at the cloaca . These are the:
- Mesonephric (Wolffian) ducts
- Paramesonephric (Mullerian) ducts
In the presence of testosterone (produced by the Leydig cells), the mesonephric ducts develop to form the primary male genital ducts. They give rise to the efferent ductules, epididymis, vas deferens and seminal vesicles.
Meanwhile, the paramesonephric ducts degenerate in the presence of anti-Mullerian hormone – produced by Sertoli cells in the testes. Its developmental remnant is the appendix testis; a small portion of tissue located on the upper pole of each testicle, which has no physiological function.
In the female, there are no Leydig cells to produce testosterone. In the absence of this hormone, the mesonephric ducts degenerate, leaving behind only a vestigial remnant – Gartner’s duct.
Equally, the absence of anti-Mullerian hormone also allows for development of the paramesonephric ducts . Initially, these ducts can be described as having three parts:
- Cranial – becomes the Fallopian tubes
- Horizontal – becomes the Fallopian tubes
- Caudal – fuses to form the uterus, cervix and upper portion of the vagina.
The lower portion of the vagina is formed by sinovaginal bulbs (derived from the pelvic part of the urogenital sinus).
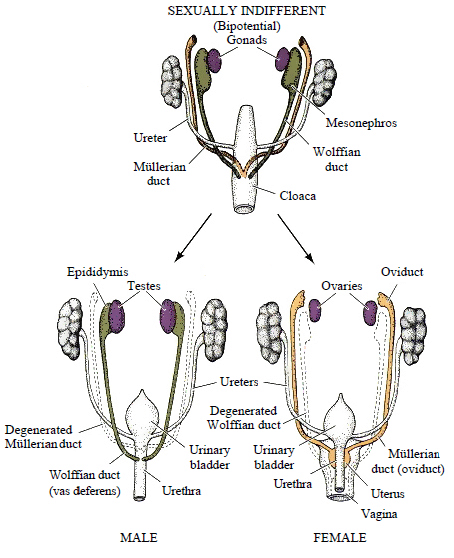
Fig 2 Development of the internal genitalia in the male and female.
Clinical Relevance
Bicornuate uterus.
Bicornate uterus is a relatively common structural defect. It occurs when there is incomplete fusion of the paramesonephric ducts.
This results in two distinct uterine horns, both opening into a single vagina. As it is asymptomatic, the condition is often only picked up on ultrasound scan during pregnancy.
This malformation is considered high-risk in pregnancy, as there is an associated risk of miscarriage and premature delivery.

Fig 3 A bicornate uterus, formed by failure of the paramesonephric ducts to fuse fully.
External Genitalia
The development of the external genitalia begins in the third week. Mesenchymal cells from the primitive streak migrate to the cloacal membrane to form a pair of cloacal folds .
Cranially, these folds fuse to form the genital tubercle . Caudally, they divide into the urethral folds (anterior) and anal folds (posterior).
Genital swellings develop either side of the urethral folds.
The development of the indifferent genitalia into the male genitalia is driven by the presence of androgens from the testes, namely dihydrotestosterone (DHT) .
There is rapid elongation of the genital tubercle, which becomes the phallus . The urethral folds are pulled to form the urethral groove – this extends along the caudal aspect of the phallus. The folds close over by the 4 th month, forming the penile urethra .
The genital swellings become the scrotal swellings , moving caudally to eventually form the scrotum.
Hypospadias
A condition in which there are one or more abnormal openings of the urethra along the inferior side of the penis. This is a result of incomplete closure of the urethral folds during development. Surgery is usually performed to correct the defect.
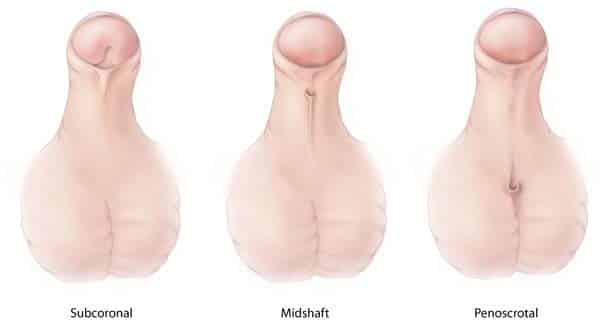
Fig 4 The different types of hypospadias.
Oestrogens in the female embryo are responsible for external genital development. The genital tubercle only elongates slightly to form the clitoris .
The urethral folds and genital swellings do not fuse, but instead form the labia minora and labia majora respectively.
The urogenital groove therefore remains open, forming the vestibule into which the urethra and vagina open.
Descent of the Gonads
While the gonads arise in the upper lumbar region, they are each tethered to the scrotum or labia by the gubernaculum – a ligamentous structure formed from mesenchyme.
As the body of the fetus grows, the testes become more caudal . They pass through the inguinal canal around the 28 th week and reach the scrotum by the 33 rd week. During their descent, the testes retain their original blood supply, with the testicular arteries branching from the lumbar aorta.
The scrotal ligament is the adult remnant of the gubernaculum.
The ovaries initially migrate caudally in a similar fashion to the testes from their origin on the posterior abdominal wall. However, they do not travel as far, reaching their final position just within the true pelvis.
The gubernaculum becomes the ovarian ligament and round ligament of the uterus .
Do you think you’re ready? Take the quiz below
Question 1 of 3
Recommended Reading
Forgot password.
Please enter your username or email address below. You will receive a link to create a new password via emai and please check that the email hasn't been delivered into your spam folder.
We use cookies to improve your experience on our site and to show you relevant advertising. To find out more, read our privacy policy .
Privacy Overview
Report question, rate this article.
- BiologyDiscussion.com
- Follow Us On:
- Google Plus
- Publish Now

Reproductive System in Humans | Essay | Humans | Reproductive Biology
ADVERTISEMENTS:
In this essay we will discuss about the male and female reproductive system in humans.
Essay on the Male Reproductive System :
During the developmental stages, the gonads of the genetic male fetus are induced to differentiate into testes. The testes of the male secrete testosterone, which is responsible for differentiation and development of the urinogenital system characteristic of the male. The testes remain inactive until puberty.
They are activated by the gonadotropins produced by the pituitary gland. Two sets of genes are required for the development of the male phenotype. The first set is located on the Y-chromosome and they encode the testes determining factor. These genes must be expressed for the undifferentiated gonad to form the testis.
In male the Mullerian ducts have to degenerate so that they may not form the female reproductive tract. Somatic cells of the developing testes secrete a Mullerian inhibiting substance, which helps in the regression of the Mullerian duct. Development of the male reproductive tract and secondary sexual characters are dependent upon androgens.
The fetal testes have to synthesize androgens at a critical time during the differentiation of the testis. A second set of genes is required for the complete development of the male. These genes encode the enzymes required for the conversion of cholesterol to testosterone and dihydrotestosterone.
Testis performs two important functions. It provides an environment for spermatogenesis and secretes the hormone testosterone, which regulates a number of reproductive activities. Testes are located within the scrotum. Each testis is oval in shape and is about 4 – 6 cm in length and 2 – 3 cm in diameter. A connective tissue sheath, the tunica albuginea, surrounds it. Spermatozoa are produced in convoluted seminiferous tubules.
These tubules converge to form the rete testis, which opens to efferential ductules and epididymis. The epididymis can be differentiated into head, body and tail. The tail continues as vas deferens. The outer layer of seminiferous tubules is made up of connective tissue and smooth muscle, while the inner layer consists of the Sertoli cells within which are embedded the spermatogonia and different stages of mature and immature spermatozoa.
Sertoli cells provide nourishment and other factors necessary for sperm maturation. The fully mature spermatozoa are released into the lumen of the seminiferous tubules and subsequently move slowly to the epididymis where they are stored in the tail region. In-between the seminiferous tubules are scattered the interstitial cells of Leydig, which produce androgens.
The parent substance from which the androgens are synthesized is cholesterol. Pregenolone is synthesized from cholesterol in the Leydig cells. Pregenenolone is converted into 17 – hydroxypregnenolone. This substance is converted to 17 – ketosteroids by side-chain cleavage and these, in turn are converted into testosterone. Testosterone is the principal steroid produced by the Leydig cells.
Hormonal Control of Testicular Function:
The anterior lobe of the pituitary gland secretes gonadotropins namely Follicle Stimulating Hormone (FSH) and Leutenizing Hormone (LH). The anterior pituitary is stimulated to release these hormones through Follicle Stimulating Hormone Releasing Hormone (FSH-RH) and Leutenizing Hormone Releasing Hormone (LH – RH) from the hypothalamus. These hormones are neurohormones.
GnRH and its Effects :
Gn-RH is a peptide containing 10 amino acid residues. It is secreted by the neurons whose cell bodies are located in the arcuate nucleus of the hypothalamus. Gonadotrophic releasing hormone is transported to the anterior pituitary gland through the portal circulation and stimulates the release of the two gonadotrophic hormones, LH and FSH.
GnRH is secreted intermittently a few minutes at a time once every 1 to 3 hours. The intensity in stimulus of this hormone is determined by the frequency of the cycle of secretion and by the GnRH released from each cycle.
Regulation of Spermatogenesis by FSH and Testosterone:
LH and FSH are secreted by the gonadotroph cells in the anterior lobe of the pituitary gland. LH and FSH are glycoproteins. The quantity of the carbohydrate bound to the protein in the hormone molecule varies considerably under different conditions, which may change the activity potential of the hormone.
FSH binds to specific FSH receptors attached to the Sertoli cells in the seminiferous tubules. This causes these cells to grow and stimulate the formation of spermatozoa in the seminiferous tubules of testes after maturity either continuously or seasonally depending upon the species. Simultaneously, testosterone also exerts a strong influence on spermatogenesis.
Hormones that stimulate spermatogenesis are:
a. Leutenizing Hormone:
It is secreted by the luteotrophs present in the anterior pituitary lobe. This hormone stimulates the interstitial cells of Leydig to secrete testosterone. Pituitary gonadotropin secretion is under tonic regulatory control. They undergo wide fluctuation in their circulating concentrations over short periods of time.
In human males LH is released after every 90 minutes. LH is released on exposure of a male to female, but successive presentation of the same female to a male mammal leads to habituation. LH specifically binds to Leydig cells while FSH binds to only Sertoli cells. This clearly establishes the individual roles of pituitary gonadotropins in regulating testicular function.
LH increases the cAMP levels in the interstitial cells of the testes but not the seminiferous tubules. FSH on the other hand, does not increase the cAMP levels in the Leydig cells, but stimulates the production of cAMP in seminiferous tubules in enriched fractions of the Sertoli cells.
b. Inhibin:
Inhibin is a peptide hormone produced by the Sertoli cells. It controls the secretion of pituitary FSH. Inhibin secretion by the Sertoli cells is regulated by influences deriving from maturing sperms. Pituitary FSH secretion normally is regulated by negative feedback by an inhibitory factor of Sertoli cell origin.
Granulosa cells from the ovarian follicle also secrete inhibin that acts directly on pituitary cells from males or females to supress FSH secretion. Administration of anti-inhibin antisera to rats of either sex causes increase in FSH levels. LH levels are not affected by anti inhibin antisera. The role of FSH and inhibin in the control of testicular and ovarian function is shown in Figure 1.

c. Prolactin:
Testicular receptors are maintained by one or more pituitary hormones other than the pituitary gonadotropins. Decrease in pituitary prolactin secretion decreases the testicular LH receptors, whereas prolactin treatment prevents loss of LH receptors in hypophysectomized animals. Thus, prolactin plays a role in the control of testicular Leydig cell LH receptor numbers.
d. Androgens:
Androgens control the differentiation and development of the male urinogenital system, the accessory sex organs and the external genital organs. Androgens produced by the testis are responsible for the growth and development of all those tissues that characterize the male.
Increased gonadotropins level during puberty increases the circulating levels of androgens. This increase in the level of androgens is responsible for initiating spermatogenesis and for the growth and development of the secondary sexual characteristics.
All androgens are steroid compounds. They can be synthesized from cholesterol or directly from acetyl coenzyme A. After secretion by the testes, about 97% of the hormone becomes either loosely bound to plasma albumin or tightly bound to a beta globulin called sex hormone binding globulin and circulates in blood in these states for 30 minutes to 1 hour.
By that time much of the testosterone becomes fixed to the tissues and is converted to a more active hormone known as dihydrotestosterone especially in some target organs like the prostate gland in adult and in external genitalia of the male fetus.

Intracellular Action of Testosterone :
Testosterone increases the rate of formation of proteins in target cells. In prostate gland testosterone enters the cells within a few minutes after secretion and is converted into dihydrotestosterone by an intracellular enzyme 5, α-reductase, Dihydrotestosterone binds to an intracelular receptor protein and this complex migrates to the nuclei and binds to a nuclear protein to induce the transcription process within 30 minutes.
RNA polymerase is activated and ultimately, the concentration of the cellular protein progressively increases. Thus, testosterone stimulates the production of protein and specifically those proteins in target organs responsible for the development of secondary sexual characteristics.
Some important target tissues do not have the reductase enzyme in their cells to convert testosterone into dihydrotestosterone. Therefore, in these tissues testosterone functions directly but only with its half potency. This direct action of testosterone is essential in male fetal tissues for the development of epididymis, vas deferens and seminal vesicles.
Spermatogenesis:
During sexual maturation, FSH and testosterone initiate spermatogenesis. FSH increases the size of the testis but does not increase the appearance of mature spermatozoa and secretory activity of the Leydig cells. For completion of spermatogenesis, testosterone is required. FSH initiates tie process of spermatogenesis while testosterone maintains it.
FSH interacts with the receptors located in the plasmalemma of the Sertoli ceils resulting in increased production of cAMP and the synthesis of an androgen binding protein (ABP). The ABP is subsequently secreted into the lumen of the seminiferous tubules. Leydig cells contain specific receptors for LH. In response to LH, testosterone released by the Leydig cells enters the seminiferous tubules through blood circulation.
Testosterone is actively taken up by the Sertoli cells. Within the Sertoli cells testosterone is bound to the androgen binding protein. This binding brings testosterone in close contact to spermatozoa on which maturation of the spermatozoa is dependent. Thus, the hormonal effects of testosterone on spermatogenesis are mediated through the Sertoli cells.
Androgen binding protein provides a mechanism for the accumulation of androgens within the Sertoli cells and its release into the lumen of the seminiferous tubules. From the lumen, ABP transports testosterone to the epididymis, where they mature and develop the potential for fertilization and motility.

Physiological Functions of Estrogens:
Estrogens and androgens are necessary for normal reproductive function in male. Information on estrogen functions in the male is obtained by the use of gene knockout technique involving a mutant mouse line without a functional estrogen receptor.
In mice without functional estrogen receptor, the testes atrophy progressively with decrease in the number of spermatozoa in epididymis, their viability and motility. Estrogen regulates the reabsorption of luminal fluid in the head of epididymis. Disruption of estrogen function causes spermatozoa to enter the epididymis in diluted rather than concentrated, resulting in infertility.
Essay on the Female Reproductive System:
As in the male, in female the ovary also performs the functions of gametogenesis and as an endocrine gland. Ova released from the ovary enter the oviducts and Fallopian tube. Fertilization of the ovum usually occurs in the fallopian tubes by the spermatozoa released by the male during copulation. The fertilized ovum descends into the uterus and is embedded in its wall for further development and embryogenesis.
The ovary consists of both epithelial and mesenchymal elements. The mesenchyme differentiates into interstitial tissue, which produces estrogen. The epithelial tissue is closely associated with the germinal elements of the ovary. It provides nutrition to the oocytes and is an important source of hormones required for different stages of the ovarian cycle.
The ovary is a solid structure covered by a visceral peritoneum of flattened cells. Inside this is a layer of cuboidal cells, the germinal epithelium. The stroma is divided into outer ovarian cortex and inner ovarian medulla. At birth, each oocyte is surrounded by a single layer of flattened granulosa cells. The combined structure is known as primordial follicle.
The primordial follicles are located near the periphery or cortex of the ovary, and are separated from each other by the stromal connective tissue and interstitial tissue. The primordial follicles remain inactive until puberty. The follicular epithelial cells are transformed into a single layer of cuboidal cells surrounding the oocyte.
The entire structure is known as primary follicle. During puberty, under the influence of hormones 6 to 12 primary follicles develop into secondary follicles. The granulosa cells secrete a mucoid material that forms the zona pellucida around the oocyte.
The granulosa cells develop protoplasmic processes that penetrate the zona pellucida and touch the plasmalemma of the oocyte. Out of the 6 to 12 primary follicles, during each menstrual cycle only one develops into a mature follicle while others become atretic and disappear. The granulosa cells continue to increase in number.
The interstitial tissue adjacent to the follicle becomes arranged concentrically around it to form the theca. Thecal cells adjacent to the follicle, the theca interna, are surrounded by an outer layer of interstitial cells forming the theca externa. Granulosa cells continue to proliferate and surrounding interstitial cells are incorporated into the theca. These changes are accompanied by accumulation of a fluid in the spaces between the granulosa cells.
A large vesicle or antrum is formed due to the enlargement of the follicle. Graulosa cells adhering to the surface of the oocyte form the coronal granulosa cells while the remaining cells in contact with the surrounding theca form the membrana granulosa. A streak of granulosa cells connects the cells around the ovum with the membrana granulosa.
The layer of granulosa cells around the ovum form the corona radiata. The oocyte acquires two membranes, the inner thin vitelline membrane and outer thick zona pellucida. The zona pellucida is surrounded by the corona radiata composed of enlarged follicular cells with fine canals between them. The fully formed mature follicle is known as Graffian follicle.
The solid follicle develops in it a small cavity called as the antrum. The antrum gradually becomes wider. Release of the oocyte is known as ovulation. A single ovum is expelled from a ovarian follicle into the abdominal cavity in the middle of each monthly menstrual cycle.
Ovulation is caused due to increased turgidity and contraction of smooth muscle fibers around the follicles. The ovum passes through one of the Fallopian tubes into the uterus, if it is fertilized by the sperm.
In rabbit ovulation occurs after copulation. Mammalian ovulation is a unique biological process as it involves the physical disruption of healthy tissue at the surface of the ovary. Ovulation requires a surge of pituitary gonadotropins. The capillaries in the follicular wall dilate after about 4-6 hours of the starting of the ovulatory process.
As the time of rupture approaches, the apex of a mature follicle protrudes more and more above the surface of the ovary and the follicle wall gradually becomes thinner. The apical most part of the follicle becomes translucent and rapidly protrudes above the normal wall of the follicle wall to form a stigma.
The follicle ruptures within several minutes after the formation of the stigma. The final rupture of the follicle is dependent upon the degradation of the collagenous connective tissue in the thecal layer of the follicle wall. After the rupture of the wall of the follicle, the oocyte and surrounding cells are extruded within a couple of minutes.
The purposes of the ovarian follicle are to:
(i) Preserve the resident oocyte,
(ii) Mature the oocyte at the optimal time,
(iii) Produce hormones to develop a proliferating endometrium,
(iv) Release of the oocyte at the proper time,
(v) Formation of a high quality corpus luteum for implantation, and
(vi) Secrete hormones required for gestation.
Corpus Luteum:
After rupture and release of the ovum from the Graffian follicle, the granulosa and thecal cells increase in number and the blood clot is absorbed. The granulosa cells start to accumulate large quantity of cholesterol and this process of leutenization forms the corpus luteum. Cells derived from the theca interna migrate into the luteal tissue to give rise to small luteal cells, theca lutein cells and fibrobasts.
Hormonal Influence on the Ovary:
The female hormonal system consists of three hormones:
(i) A hypothalamic releasing hormone, the gonadotropin releasing hormone (GnRH),
(ii) The anterior pituitary hormones, follicle stimulating hormone (FSH) and leutenizing hormone (LH) both of which are secreted on stimulation by the GnRH, and
(iii) The ovarian hormones, estrogen and progesterone secreted by the ovaries in response to the two pituitary hormones. These different hormones are not secreted in constant amounts and continuously throughout the menstrual cycle but are secreted at different rates during different parts of the cycle.
Estrogen Biosynthesis:
The two cell theory of estrogen secretion states that the thecal cells produce carbon 19 androgens and these are delivered to the granulose cells where they are converted into aromatic compounds, the estrogens (Fig. 3). This theory is supported by the observation that granulose cells from several species secrete estrogens if provided with an androgen substrate.

This theory is supported by the observation that granulosa cells of several species secrete estrogens if given an androgen substrate. Thecal cells also produce large amount of androgens. The CYP 17 gene that codes for 17-hydroxylase and C17-20 lyase is actively regulated by LH. Granulosa cells have an aromatase system.
As follicular maturation progresses, the ability of the granulosa cells to aromatize androgens increases. Estrogen production increases within the follicles during the preovulatory phase and is highest at the time of the LH and FSH surge.
Before exposure to a high level of LH, androgen and estrogen levels predominate; after the LH surge and during the luteal phase of the cycle, progesterone is the major steroid produced. A complex number of interactions involving LH, FSH, androgens, progesterone and estrogens are involved in the shift from estrogens to progesterone synthesis.
Modified version of the two cell theory states that LH stimulates androgen production within the thecal cells. Androgens are then aromatized within the thecal cells but are also made available to the granulosa cells for aromatization to estrogens.
The estrogens produced by the thecal cells are the major source of circulating levels of the steroid, whereas estrogens synthesized by the granulosa cells are regulated through FSH stimulation of cAMP production and later activation of aromatase activity.
Estradiol is oxidized to estrone in the liver (Fig. 4). Estrone is hydrated to form estriol. During pregnancy, the placenta is an additional source of androgens. Aromatization of androstenedione and testosterone is a major source of estrogens in the male and old females.

Biosynthesis of Progesterone:
The growth of the ovarian follicles before ovulation is dependent on FSH and LH, both acting together FSH promotes the growth of the follicle by acting through receptors on the granulosa cells and inducing the aromatase enzyme required for the conversion of androgens to estrogens.
The action of FSH is enhanced by androgens. Androgens arise from the theca under the control of LH. FSH receptors occur only on granulosa cells, while LH receptors present initially only in the theca. appear in the granulosa cells and are coupled to the cAMP as FSH receptors.
During the preovulatory surge, LH acting on the granulosa cells initiates luteinization, resulting in a reduction of aromatase activity and the enhancement of progesterone synthesis and secretion as the luteinized granulosa cells transform to become the corpus luteum. Synthesis of progesterone is an early step in the biosynthesis of androgens and estrogens within the thecal cell. Carpus luteum is the major source of circulating progesterone.
Effect of Gonadotrophic Hormones:
The ovarian changes during the sexual cycle depend completely on the gonadotrophic hormones, FSH and LH secreted by the anterior pituitary gland. Ovaries remain inactive until stimulated by these hormones. At the age of 11 to 16 years pituitary begins to secrete more FSH and LH, which initiates the menstrual cycle.
During the life cycle of a normal female, the reproductive phase is characterized by monthly rhythmical changes in the rate of secretion of female hormones and corresponding changes in the ovaries and sex organs. This rhythmical pattern is called as the female sexual cycle or menstrual cycle. The duration of the cycle usually is 28 days.
The menstrual cycle can be divided into three phases:
(i) Proliferation of the endometrium or proliferative phase,
(ii) Development of secretory changes in the endometrium or secretory phase, and
(iii) Degeneration of the endometrium of the uterus or degenerative phase. The menstrual cycle includes a period of bleeding called menstruation and the days are counted from the first day of bleeding in the menstrual period.
Proliferative Phase:
In the beginning of the menstrual cycle, the endometrium of the uterine wall is in a state of degeneration. After menstruation, only a thin layer of endometrial stroma and epithelial cells are left and these are located in the deeper portion of glands and crypts of endometrium.
Therefore, to prepare the uterine wall for implantation after ovulation, following changes occur:
(1) The adenohypophysis secretes FSH under the influence of FSH-RH from the hypothalamus. The hypothalamus secretes FSH-RH when decrease in the level of estrogen and progesterone secreted in the proceeding menstrual cycle remove its inhibitory effect.
(2) FSH stimulates the growth of selected few primary follicles and maturation of primary follicles.
(3) FSH stimulates the follicular cells to secrete estrogen, which inhibits the secretion of FSH and stimulates hypothalamic secretion of LH-RH. This in turn stimulates the secretion of leutenizing hormone by the pituitary.
(4) LH induces the mature Graffian follicle to burst and release the ovum. This process occurs after 14 days and is known as ovulation. The ovum at this stage is in secondary oocyte stage with the second meiotic division in progress.
(5) Estrogen prepares the wall of the uterus for implantation by proliferating the endometrial epithelial cells. Blood vessels in the uterine wall become elongated and coiled, and vascularization increases. Uterine glands secrete a nutritive fluid into the cavity. Glycogen and fat accumulate.
(6) Under the influence of estradiol, the lining of Fallopian tube is thickened and the ciliary movements are increased. These changes help in conveying the ovum to the uterus.
Secretory Phase (Progesterone Phase):
The stage lasting for about ten days can be further differentiated into the following steps:
(1) LH and prolactin are at their peak of secretion from the anterior lobe of the pituitary. They stimulate the follicular cells of the empty Graffian follicles after the release of the ovum to grow rapidly and become filled with a yellow substance called luteum.
The cavity of follicle becomes filled with blood and broken down thecal cells. The follicle is known as corpus luteum. The yellow corpus luteum secretes the ovarian hormones, progesterone and .small quantities of estradiol.
(2) Estrogen increases cellular proliferation in the uterine endometrium while progesterone causes swelling and secretory activity of the endometrium. This hormone stimulates the endometrial glands to secrete a nutrient fluid for the fetus.
Cytoplasm of the stromal cells, lipid and glycogen deposits and blood supply to the endometrium increase tremendously. At the peak of the secretory phase, usually about one week after ovulation, the endometrium becomes 5-6 mm thick. Progesterone is also required for proper implantation of the fetus.
(3) Progesterone inhibits the release of FSH to prevent the development of additional follicles and ova.
Menstrual or Bleeding Phase:
This phase lasting for 4-5 days is characterized by:
(1) In case of failure of fertilization, the secondary oocyte undergoes degeneration and autolysis. High levels of progesterone in blood inhibit the release of pituitary LH.
(2) Absence of LH brings about autolysis of the corpus luteum and subsequent decrease in the level of progesterone. Regression of the corpus luteum begins about a week after ovulation and after ten days it is replaced by a small, non-functional whitish structure called as the corpus albicans.
(3) The uterine wall degenerates due to the deficiency of progesterone and is sloughed off. Blood vessels rupture causing bleeding. The lining of the Fallopian tubes also degenerates and breaks down. The cast off uterine and Fallopian tissue, and blood from the ruptured blood vessels passes out through the vaginal opening.
This process is called as menstruation or menstrual flow. This occurs after about 25 days and continues for 3-5 days. During normal menstruation, about 50 to 100 ml of blood and 30 ml of serous fluid are lost. The menstrual flow does not clot because fibrinolysin is released along with endometrial breakage.
In case if excessive bleeding occurs, fibrinolysin cannot prevent clotting. The presence of clot during menstrual flow is a serious problem that needs clinical treatment. The basal part of the endometrium remains in tact during menstruation and is the source of new lining wall to the uterus during the next cycle.
(4) Degeneration of the carpus luteum decreases the levels of progesterone and estradiol, which in turn removes their inhibitory effect on hypothalamus. Therefore, the hypothalamus starts to secrete FSH-RH and this stimulates the pituitary to produce FSH.
Functions of Ovarian Hormones:
The ovarian follicles are sources of three types of steroid hormones; progestins, androgen, and estrogens. Their levels vary in the menstrual cycle and drastically change in the pregnancy. In the follicular stage of the menstrual cycle, estradiol is dominant, whereas during the luteal phase and during pregnancy, progesterone prevails over others.
Estrogens are mainly secreted by the ovary but minute quantities are also produced by adrenal cortex. During pregnancy, the placenta also contributes to the secretion of estrogens. Estrogens produced during the puberty in female are responsible for growth and development of the vagina, uterus, and oviducts, organs essential for the transportation of ovum, maturation of the zygote and implantation of the embryo.
Estrogens exert their effect on deposition of fat, growth and development of the mammary glands. In human females, three estrogens occur in significant quantities in the plasma. These are estradiol, estrone and estriol. The principal estrogen is estradiol. Small amount of estrone is secreted by the ovaries but most of it is formed from androgens secreted by the adrenal cortex.
Estriol a weak estrogen, is an oxidative product derived from both estradiol and estrone in the liver. The estrogenic potency of estradiol is 12 times higher than that of estrone and 80 times greater than that of estriol.
(i) Estrogens promote proliferation and growth of specific cells in the body and are mainly responsible for development of secondary sexual characteristics of the female.
(ii) During puberty secretion of the estrogens increases by 20 times or more. The female sex organs increase in size due to their influence. Ovaries, fallopian tubes, uterus and vagina are all enlarged. Fat deposits in the external genitalia, pubis, labia majora and labia minora. The vaginal epithelium becomes converted from cuboidal into a stratifed type which is more resistant to infection and trauma.
(iii) Estrogens cause glandular tissue to proliferate and number of ciliated epithelial cells increases. The activity of cilia is also increased to promote the transport of fertilized ovum towards uterus.
(iv) Estrogens promote the development of the stromal tissue of breasts, growth of duct system and deposition of fat in breasts.
Progestins:
The most important progestin is progesterone. Small quantities of 17-hydroxy progesterone is also secreted and it has the same effect. Progesterone is the ovarian hormone of pregnancy and is responsible for preparing the reproductive tract for implantation of the zygote and subsequent and maintenance of the pregnant state.
(a) Effects on Uterus:
The most important function of progesterone is to promote secretory changes in the uterine endometrium during the later half of monthly menstrual cycle thus preparing the uterus for implantation of fertilized ovum. Progesterone decreases the frequency and intensity of uterine contraction and thus helps in preventing expulsion of the implanted zygote.
(b) Effect on Fallopian Tubes:
Progesterone also promotes secretory changes in the mucosal lining of the Fallopian tubes. These secretions are required for the nutrition of the fertilized ovum.
(c) Effects on Breasts:
Progesterone promotes development of the lobules and alveoli of the breasts. This causes enlargement of the breasts. It cannot initiate the secretion of milk because milk secretion requires the hormone prolactin. It is speculated that preovulatory plasma levels of progesterone may trigger sexual behaviours in some species.
In rodents, progesterone is necessary for induction of sexual receptivity. Progesterone also plays a role in the nest- building activity and brooding behaviours in some birds. The following table summarizes the physiological actions of progesterone and estradiol.

Mechanisms of Action of Ovarian Steroid Hormones:
Estradiol and progesterone interact with cytoplasmic and nuclear protein receptors resulting in the release of the two-receptor subunits with attached steroid hormones from association with a heat shock protein. Identical subunits either singly or together interact directly with the DNA hormone responsive element to activate the transcriptional events leading to the translation of a cell specific protein.
Ovulation and Role of Luteinizing Hormone :
Ovulation is the process bf release of ovum from the ovarian Graffian follicles. This usually occurs in healthy normal women on fourteenth day after the last menstruation. Shortly before ovulation, the protruding outer wall of the follicles swells rapidly and a small area in the capsule called the stigma protrudes out.
In the next thirty minutes, fluid begins to ooze from the follicle through the stigma. Two minutes later, as a follicle becomes smaller due to loss of fluid, stigma ruptures and the ovum comes out surrounded by several thousand granulosa cells called the corona radiata.
Initiation of Ovulation:
Large quantity of luteinizing hormone is secreted by the pituitary gland. The LH in turn causes rapid secretion of follicular steroid hormone, progesterone.
Within a few hours two events occur:
(i) The theca externa (outer capsule of follicle) begins to release proteolytic enzymes from lysosomes that causes swelling of the follicle and degeneration of the stigma.
(ii) Simultaneously, there is rapid growth of new blood vessels into the wall of the follicles and at the same time prostaglandins are secreted in the follicular tissues. Finally, the combined follicle swelling and simultaneous degeneration of the stigma cause follicle rupture to discharge the ovum.
Ovulatory Surge of Leutenizing Hormone:
LH is essential for the growth and development of the follicle, and ovulation. About two days before the LH secretion increases markedly. FSH secretion also increases and the two hormones act together to produce rapid growth of the follicle during last few days before ovulation. LH secretion also has an effect on the theca cells to secrete progesterone.
The changes that occur can be summarized into:
(i) Rapid growth of the follicle,
(ii) Diminishing level of estrogen secretion, starting of the secretion of progesterone and ovulation occurs.
At the age of 40 to 50 years, sexual cycle in the female becomes irregular and ovulation fails to occur during many of the cycles. When secretion of female sex hormones and the process of ovulation stop completely, it is called menopause.
Throughout a womens reproductive life, about 400 follicles grow and ovulate. But at the age of about 45 years, only a few primordial follicles remain to be stimulated by FSH and LH, and production of estrogen decreases to zero when primordial follicles number becomes almost nil. Therefore, estrogen cannot inhibit the production of FSH and LH which are produced in large quantity in menopause.
The loss of estrogen causes many physiological changes in the function of the body such as:
(i) Extreme flushing of the skin,
(ii) Irritability,
(iii) Fatigue,
(iv) Anxiety and
(v) Decreased strength and calcification of bones throughout the body.
These symptoms are sometimes cured by regular administration of estrogen.
Related Articles:
- Hormonal Changes Take Place during Adolescence | Humans | Biology
- Estrogen: Meaning, Source, Biosynthesis (With Diagram)
Essay , Humans , Reproductive Biology , Reproductive System in Humans
- Anybody can ask a question
- Anybody can answer
- The best answers are voted up and rise to the top
Forum Categories
- Animal Kingdom
- Biodiversity
- Biological Classification
- Biology An Introduction 11
- Biology An Introduction
- Biology in Human Welfare 175
- Biomolecules
- Biotechnology 43
- Body Fluids and Circulation
- Breathing and Exchange of Gases
- Cell- Structure and Function
- Chemical Coordination
- Digestion and Absorption
- Diversity in the Living World 125
- Environmental Issues
- Excretory System
- Flowering Plants
- Food Production
- Genetics and Evolution 110
- Human Health and Diseases
- Human Physiology 242
- Human Reproduction
- Immune System
- Living World
- Locomotion and Movement
- Microbes in Human Welfare
- Mineral Nutrition
- Molecualr Basis of Inheritance
- Neural Coordination
- Organisms and Population
- Photosynthesis
- Plant Growth and Development
- Plant Kingdom
- Plant Physiology 261
- Principles and Processes
- Principles of Inheritance and Variation
- Reproduction 245
- Reproduction in Animals
- Reproduction in Flowering Plants
- Reproduction in Organisms
- Reproductive Health
- Respiration
- Structural Organisation in Animals
- Transport in Plants
- Trending 14
Privacy Overview
| Cookie | Duration | Description |
|---|---|---|
| cookielawinfo-checkbox-analytics | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Analytics". |
| cookielawinfo-checkbox-functional | 11 months | The cookie is set by GDPR cookie consent to record the user consent for the cookies in the category "Functional". |
| cookielawinfo-checkbox-necessary | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookies is used to store the user consent for the cookies in the category "Necessary". |
| cookielawinfo-checkbox-others | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Other. |
| cookielawinfo-checkbox-performance | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Performance". |
| viewed_cookie_policy | 11 months | The cookie is set by the GDPR Cookie Consent plugin and is used to store whether or not user has consented to the use of cookies. It does not store any personal data. |
Home — Essay Samples — Nursing & Health — Sexual Health — Male and Female Reproductive System: Functions and Diseases
Male and Female Reproductive System: Functions and Diseases
- Categories: Medicare Sexual Health
About this sample

Words: 614 |
Published: Jan 4, 2019
Words: 614 | Page: 1 | 4 min read
Works Cited
- Sadler, T. W. (2019). Langman's Medical Embryology. Wolters Kluwer.
- Moore, K. L., Persaud, T. V. N., & Torchia, M. G. (2019). The Developing Human: Clinically Oriented Embryology. Elsevier.
- Tortora, G. J., Derrickson, B. H., & Tortora, G. J. (2017). Principles of Anatomy and Physiology. John Wiley & Sons.
- Saladin, K. S. (2017). Anatomy & Physiology: The Unity of Form and Function. McGraw-Hill Education.
- Guyton, A. C., & Hall, J. E. (2020). Textbook of Medical Physiology. Elsevier.
- Moore, K. L., Persaud, T. V. N., & Torchia, M. G. (2015). Before We Are Born: Essentials of Embryology and Birth Defects. Elsevier.
- Johnson, M. H., & Everitt, B. J. (2018). Essential Reproduction. John Wiley & Sons.
- Berek, J. S., & Novak, E. R. (2019). Novak's Gynecology. Wolters Kluwer.
- Howkins, J., & Bourne, G. (2017). Dewhurst's Textbook of Obstetrics and Gynaecology. John Wiley & Sons.
- Zeleke, B. M., & Bell, R. J. (2019). Female Reproductive System (Anatomy and Function). In StatPearls [Internet]. StatPearls Publishing.

Cite this Essay
To export a reference to this article please select a referencing style below:
Let us write you an essay from scratch
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Get high-quality help

Dr. Karlyna PhD
Verified writer
- Expert in: Nursing & Health

+ 120 experts online
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
Related Essays
2 pages / 881 words
2 pages / 744 words
3 pages / 1262 words
4 pages / 1708 words
Remember! This is just a sample.
You can get your custom paper by one of our expert writers.
121 writers online
Still can’t find what you need?
Browse our vast selection of original essay samples, each expertly formatted and styled
Related Essays on Sexual Health
The video provides insights into the bill's objectives of modernizing the curriculum to offer comprehensive and inclusive sexual health education. It offers a balanced analysis of the bill, highlighting both [...]
Sex education is a vital component of a well-rounded education that equips students with the knowledge and skills needed to make informed decisions about their sexual health and relationships. Comprehensive sex education goes [...]
Sex education is a crucial component of personal development and overall well-being, yet it is often neglected beyond adolescence. While the focus tends to be on providing young people with the necessary knowledge and skills to [...]
Sex education in the United States has long been a contentious and polarizing issue. With varying beliefs, values, and ideologies shaping public discourse, the landscape of sex education programs across the country remains [...]
Across all cultures and civilizations, in every species and genus, sex is a pivotal biological activity that is practiced universally. There are hundreds of stigmas surrounding sex; some believe it has religious value, others [...]
Thomas Mappes developed his theory of sexual morality through a Kantian sexual ethic, by following the logic that one should never treat someone as a method to our own ends, we must treat others as an end in themselves. The [...]
Related Topics
By clicking “Send”, you agree to our Terms of service and Privacy statement . We will occasionally send you account related emails.
Where do you want us to send this sample?
By clicking “Continue”, you agree to our terms of service and privacy policy.
Be careful. This essay is not unique
This essay was donated by a student and is likely to have been used and submitted before
Download this Sample
Free samples may contain mistakes and not unique parts
Sorry, we could not paraphrase this essay. Our professional writers can rewrite it and get you a unique paper.
Please check your inbox.
We can write you a custom essay that will follow your exact instructions and meet the deadlines. Let's fix your grades together!
Get Your Personalized Essay in 3 Hours or Less!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free
- Biology Article
Female Reproductive System
The female reproductive system consists of the primary as well as accessory sex organs. The primary sex organs in females are a pair of ovaries, which produce ova or egg and they also secrete female sex hormones like progesterone and estrogen. The other accessory sex organs include the uterus, fallopian tubes, cervix and vagina. The external genitalia comprises the labia minora, labia majora and clitoris. The mammary glands are not considered genital organs but are important glands in the female reproductive system.
Let’s learn more about the female reproductive system with a well-labelled diagram.
Table of Contents:
Labelled diagram of female reproductive system.
- Female Reproductive System Anatomy
Menstrual Cycle
Reproduction control, frequently asked questions, female reproductive system anatomy.
The female reproductive system is framed to perform different functions. It creates egg cells that are essential for reproduction known as ova. The system is organized to deliver the ova to the region of fertilization. The egg fertilization takes place in the Fallopian tubes along with the sperm. The implanting in the walls of the uterus and initiating the stages of pregnancy is the next step of fertilized eggs. Apart from the above-mentioned functions, the female reproductive system is also involved in the production of female sex hormones to maintain the reproductive cycle.
The female reproductive system is composed of a pair of ovaries along with oviducts, vagina, cervix, uterus, and the external genitalia that are located in the pelvic region. These parts along with a pair of mammary glands that are integrated both functionally and structurally also support the process of ovulation, fertilization, birth and finally the child care.
Also check: Bartholin Ducts (Glands)
Ovaries act as the main female sex organs that produce the female gamete and various hormones . These organs are situated one on both the side of the lower abdomen. Each ovary measures about 2 to 4 cm in length which is then connected to the uterus and pelvic wall through ligaments. The ovary is surrounded by a thin covering of epithelium, encloses the ovarian stroma and is divided into two zones – outer cortex and the inner medulla. The cortex consists of various ovarian follicles in different stages of development. The ovarian follicle is called the basic unit of the female reproductive system. Each oviduct is divided into three anatomical regions- ampulla, isthmus, and infundibulum.
A uterus is also called the womb. It is a muscular, inverted pear-shaped organ of the female reproductive system. The walls of the uterus consist of three layers- the inner glandular layer, the middle thick layer, and the outer thin layer. These three layers are maintained by ligaments which are attached to the pelvic wall which then opens into the vagina from a narrow cervix. The cervical canal along with the vagina creates the birth canal. The vagina is a muscular tube which starts at the lower end of the uterus to the outside.
Fallopian Tubes
Fallopian tubes are a pair of muscular tubes and funnel-shaped structures, extend from the right and left of the superior corners of the uterus to the edge of the ovaries. These tubes are enclosed in small projections called fimbriae that swipe over the ovaries to pick up released ova and deliver them to the infundibulum for supplying the uterus. Each fallopian tube is covered by cilia that functions by carrying the ovum to the uterus.
Related Video:
The vagina is a muscular and elastic tube that connects the cervix to the external body. It functions as the receptacle for the penis in sexual intercourse and delivers sperm to the fallopian tubes and uterus. It also acts as a birth canal by expanding to allow delivery of the fetus during childbirth.
The external genitalia comprises the labia minora , labia majora and clitoris
Ovulation is the process of releasing the eggs from the ovaries. This process takes place as soon as the follicle is fully grown and reaches its size along with the accumulation of liquid in the follicle without a significant rise in pressure. As the follicle swells out, a small oval-shaped area, the stigma or macula pellucida appears sticking outward as a clear cone area and later undergoes localized changes in colour, integrity, and translucency. The secretion of estrogen hormones reaches the maximum level before the ovulation. After the surge of luteinizing hormone, ovulation occurs at the site of the stigma. This surge is essential for ovulation. Ovulation is the process in which the follicle is separated by releasing of follicular fluid along with the ovum surrounded by the corona radiata. The cells of the corona radiata will separate later in the presence of spermatozoa. In ruminants, the oocytes have already lost their corona at the time of ovulation. The very active fimbriae, end of the oviduct picks up the ovum. If fertilized ovum or zygote undergoes cleavage and makes its way to the uterus for implantation. If not fertilized, it degenerates within 24 hours.
All females, after reaching their puberty produce mature egg cell every month during a process called the menstrual cycle . During this period, an ovary discharges a mature egg, which travels to the uterus. In the uterus, if the egg is not fertilized, the lining in the uterine sheds away and a new cycle begins. Overall a menstrual cycle lasts for 28 days, in some cases, these cycles may either last for 21 days or as long as 35 days in some individuals. The entire process of the menstrual cycle is controlled by the endocrine system and the hormones involved are FSH, LH, estrogen, and progesterone. Both FSH and LH hormones are produced by the pituitary gland, whereas estrogen and progesterone hormones are produced by the ovaries. Alon with the hormonal disorders, there are many other factors, which are responsible for the disturbance in the menstrual cycle. The responsible factors include diet, exercise, stress and weight gain or loss affects the menstrual cycle. The cycle may be irregular at times, especially during puberty. The menstrual cycles occur every month from the time of puberty up to the age of 45 to 55, except during pregnancy. After the age of 55 ovaries slows down their production of hormone and release of mature eggs. Progressively, the menstrual cycle stops, therefore, the woman is no longer able to become pregnant.
Fertilization and Pregnancy
Following implantation, the placenta originates from maternal and fetal tissues, producing human chorionic gonadotropin (HCG) that helps in maintaining the level of corpus luteum in the ovary until the placenta begins synthesizing its own progesterone and estrogen hormones.
Estrogen and Progesterone
Estrogen and progesterone hormones are produced by the ovaries that foster the development of reproductive organs by maintaining the proper uterine cycle and by developing female secondary sex characteristics. During menopause, usually between age 45 and 55, the uterine cycle stops, and the ovaries are no longer produce estrogen and progesterone hormones. Infertility In general, infertility can be defined as the failure in couples of not getting pregnant, despite having carefully timed, unprotected sex for one year. It is estimated to be around 15% of all couples undergo infertility. The reasons behind this infertility in males and females are-
In Females:
- Blocked oviducts.
- Endometriosis.
- Low sperm count.
- Sperm abnormalities.
There are various birth control methods and some of them are as mentioned below.
- Abstinence.
- Birth control pills
- Intrauterine device.
- Male condom.
- Contraceptive implants.
- The morning after pills.
To know more about the female reproductive system and its functions, visit BYJU’S.
Recommended Video:

Further Reading
What are the three layers of the uterus?
The outer thin layer or the serous layer is the covering of the uterus derived from the peritoneum. Then comes the myometrium or the middle muscular layer. It is the thickest layer and is made of smooth muscle fibres. The third layer is the glandular layer called the inner mucus layer or the endometrium.
What is the cervix?
The cervix is the lower constricted part of the uterus that is divided into two portions. The upper supravaginal portion communicates with body of the uterus and the lower vaginal portion projects into the anterior wall of the vagina. The cervical canal along with the vagina creates the birth canal.
What are the functions of the ovary?
Female ovaries have two functions, endocrine and gametogenic functions. The endocrine function is the secretion of female sex hormones like the estrogen and progesterone. The gametogenic function is the production and release of the egg or ovum for reproduction.
Also check:
- External Reproductive System of Women
- Female External Features and Anatomy
- Human External Reproductive Organs
- Genital Openings in Females
- Functions of Vestibule in Female Reproductive System
Put your understanding of this concept to test by answering a few MCQs. Click ‘Start Quiz’ to begin!
Select the correct answer and click on the “Finish” button Check your score and answers at the end of the quiz
Visit BYJU’S for all Biology related queries and study materials
Your result is as below
Request OTP on Voice Call
| BIOLOGY Related Links | |
Leave a Comment Cancel reply
Your Mobile number and Email id will not be published. Required fields are marked *
Post My Comment
Sir please demo classes now
Register with BYJU'S & Download Free PDFs
Register with byju's & watch live videos.

- About Organismal Biology
- Phylogenetic Trees and Geologic Time
- Prokaryotes: Bacteria, Archaea, and Early Life on Earth
- Eukaryotes and their Origins
- Land Plants
- Animals: Invertebrates
- Animals: Vertebrates
- Climate Change over Geologic Time
- Mass Extinctions and the Tree of Life over Geologic Time
- Multicellularity, Development, and Reproduction
- Animal Reproductive Strategies
Animal Reproductive Structures and Functions
- Animal Development I: Fertilization & Cleavage
- Animal Development II: Gastrulation & Organogenesis
- Plant Reproduction
- Plant Development I: Tissue differentiation and function
- Plant Development II: Primary and Secondary Growth
- Principles of Chemical Signaling and Communication by Microbes
- Animal Hormones
- Plant Hormones and Sensory Systems
- Nervous Systems
- Animal Sensory Systems
- Motor proteins and muscles
- Motor units and skeletal systems
- Nutritional Needs and Principles of Nutrient Transport
- Nutrient Acquisition by Plants
- Water Transport in Plants: Xylem
- Sugar Transport in Plants: Phloem
- Nutrient Acquisition by Animals
- Animal Gas Exchange and Transport
- Animal Circulatory Systems
- The Mammalian Cardiac Cycle
- Ion and Water Regulation and Nitrogenous Wastes in Animals
- The Mammalian Kidney: How Nephrons Perform Osmoregulation
- Plant and Animal Responses to the Environment
Learning Objectives
- Identify and describe functions of key anatomical reproductive structures present in various types of animals, including the spermatheca, the cloaca, the ovary and related structures, and the testes and related structures
- Compare and contrast the process, products, and locations of male and female gametogenesis in mammals
- Describe roles of hormones in gametogenesis (spermatogenesis and oogenesis), ovulation, and implantation in placental mammals
- Explain how various medical interventions affect reproductive cycles and fertilization
Diversity of Animal Reproductive Anatomy
The information below was adapted from OpenStax Biology43.2
Many animal reproductive structures are very similar, even across different lineages. Reproductive structures produce gametes (eggs and sperm) and facilitate the meeting of gametes to produce a zygote (fertilized egg). In animals ranging from insects to humans, males produce sperm in testes, and the sperm are stored in the epididymis until ejaculation. Sperm are small, mobile, “low-cost” cells that are produced in high numbers. Females produce one ovum or several ova (eggs) that mature in the ovary . Eggs are large cells that require a substantial investment of time, energy, and nutrients to form, are non-mobile, and are rare relative to sperm numbers. Mature eggs are released from the ovary into the uterine tubes (aka fallopian tubes or oviducts) where they are either fertilized (animals that reproduce via internal fertilization), or are released in an aqueous environment (animals that reproduce via external fertilization).
The first half of Hank Green’s video below has a nice summary of these and other ideas we’ve discussed previously, and the second half introduces human reproductive anatomy before we take a deep dive into the structures and functions via dynamic hormonal regulation:
For sexually reproducing populations, we can biologically define females as the sex with ovaries that produce small numbers of large eggs, which subsequently travel down a uterine tube; and males as the sex with testes that produce large numbers of small sperm, stored in an epididymis. While this general anatomy holds true, here are some interesting differences in different animal lineages:
- Spermatheca: The spermatheca is a specialized sperm-storing sac present in females in some invertebrate species. Spermatheca are common in many insects, some mollusks, and some worms. After mating, the female stores the male’s sperm in the spermatheca for later use, sometimes up to a year or more. Fertilization can then be timed with environmental or food conditions that are optimal for offspring survival. Sperm may be stored from one male or from multiple males, depending on the species mating system. In some species, the female may mate only once in her lifetime, and use the sperm from this single mating to fertilize eggs throughout her life.
- Cloaca: The cloaca is a single, shared body opening that functions in the digestive, excretory (urine), and reproductive systems. Cloacas are found among many non-mammal vertebrates, such as most birds and reptiles. Mating between birds or reptiles usually involves positioning the cloaca openings opposite each other for transfer of sperm from male to female. Ducks are a rare exception, where the males have a penis.
- Uterus: The uterus is a structure present in placental mammals (not all mammals have a uterus!) which houses the developing offspring internal to the mother’s body. The uterus essentially serves as the location for development of an amniotic egg that is retained within the body. Depending on the species, the uterus may have two chambers in species that produce multiple offspring at a time (such as mice), or only one chamber in species that produce one offspring, (such as primates).
Mammalian (Human) Reproductive Anatomy, Gametogenesis, and Hormonal Regulation
The information below was adapted from OpenStax Biology 43.3
The remainder of this reading will focus on mammalian reproduction, featuring humans as a model organism. We’ll first look at females and then males, emphasizing the structures, the process of gametogenesis, and hormonal control of reproduction.
Gametogenesis is the production of gametes, or sperm and eggs. Gametogenesis requires meiosis (see the Biological Principles textbook page on Cell Division for help with this often confusing concept). Meiosis produces haploid cells with half the number of chromosomes normally found in diploid cells.
Hormones regulate gametogenesis in both male and female reproductive cycles, including some of the same hormones. For example, follicle stimulating hormone (FSH) and luteinizing hormone (LH) are named after their functions in egg production in females, but they play important roles in sperm production in males as well.
Human Female Reproductive Anatomy
Human female reproductive structures include both external and internal structures. External structures include the breasts and the vulva. Internal structures include ovaries, oviducts, the uterus, and the vagina, shown below.

This table briefly summarizes the major organs, locations, and functions of mammalian female reproductive anatomy:
| Organ | Function |
|---|---|
| Ovaries | Produces and develops (matures) eggs |
| Fallopian tubes (oviducts) | Site of fertilization; transports egg to uterus |
| Uterus | Supports developing embryo |
| Cervix | Allows passage between the uterus and the vagina |
| Vagina | Receives penis during intercourse, acts as birth canal, passes menstrual flow |
| Breasts | Produce and deliver milk |
Human females become capable of reproduction at sexual maturity, which follows puberty. During puberty, the hypothalamus in the brain signals the pituitary gland to produce two hormones, follicle-stimulating hormone ( FSH ) and luteinizing hormone ( LH ). In females, FSH and LH stimulate the ovaries to produce the female sex hormones, estrogen and progesterone. During puberty, these hormones initiate development of secondary sex characteristics (such as breasts) and cause the ovaries to begin producing mature eggs.
Ovaries are the site of egg development and maturation. Eggs develop and mature in structures called follicles , which are found throughout the ovary. Each follicle contains one immature egg. Egg development in humans occurs in small batches, with one or two eggs maturing on an approximately-monthly cycle called the ovarian cycle :
- In the first phase of the ovarian cycle, the several follicles become activated to promote development of the egg inside of them (recall that each follicle contains one immature egg).
- At the middle of the ovarian cycle, the most mature follicle will “rupture,” releasing one egg as illustrated below (rarely, a second follicle will rupture, resulting in ovulation of two eggs). The egg travels from the ruptured follicle into the oviducts (also called fallopian tubes ), where it will be fertilized if sperm are present. Over the course of about a week, the egg will travel through the oviduct into the uterus, where it will implant and result in pregnancy if fertilization previously occurred in the oviduct. Fertilization must take place in the oviduct, not the uterus.
- In the last phase of the ovarian cycle, the ruptured follicle (still in the ovary) becomes the corpus luteum , which secretes hormones that prevent menstruation until the egg has had time to be fertilized. If fertilization and implantation in the uterine wall occurs, then the corpus luteum continues to prevent menstruation; if fertilization does not occur, then the corpus luteum degenerates and menstruation occurs.
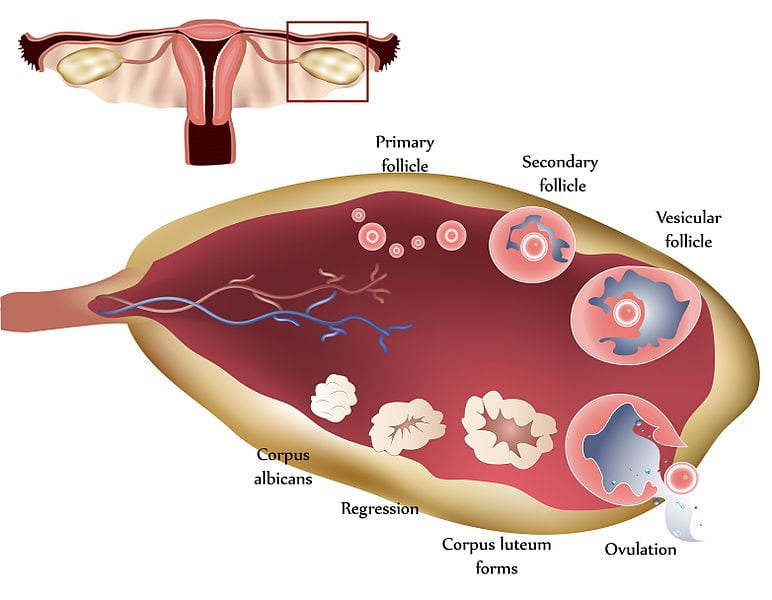
Female Gametogenesis: Oogenesis
Now that we have discussed the human female reproductive structures, let’s walk through the process of oogenesis , or egg production.
The process of oogenesis begins while the female herself is still an embryo! Oogenesis occurs in the ovaries, where egg stem cells, called oogonia , divide by mitosis to produce up to 2 million oocytes (a precursor to the egg). The oocytes start the process of meiosis, and then pause during meiosis I. This process occurs during embryonic development, meaning that a female mammal is born with every single egg she will be able produce during her lifetime already present (in an immature form) in her ovaries. This situation is very different from males, whose spermatogonia (the sperm equivalent to oogonia) do not begin producing spermatocytes (the sperm equivalent to oocytes) until puberty.
The oocytes remain paused in meiosis I until the onset of puberty, when a series of events can lead to egg maturation on an approximately monthly basis:
- Hormones from the pituitary cause some of the follicles to begin developing and the oocyte inside the follicle to finish meiosis I (recall that each follicle contains one immature egg).
- After completing meiosis I, the oocyte pauses during meiosis II.
- Though several follicles are activated during each cycle, typically only one follicle will release an oocyte. The released oocyte will begin traveling through the oviduct, still paused in meiosis II.
- If the oocyte is fertilized by a sperm cell, it will finish meiosis II to produce a single fertilized egg (a zygote). If it is not fertilized, the oocyte degrades without completing meiosis II.
One final point: when each oocyte undergoes meiosis to go from diploid to haploid, each oocyte produces only a single egg (this is different from spermatogenesis, which produces four sperm from each spermatocyte). The oocyte undergoes a process called unequal cytokinesis , meaning it divides unequally so that almost all of the cytoplasm goes into only one daughter cell rather than evenly distributed into both. The smaller cell is called a polar body, and it normally dies as development progresses.
The process of oogenesis is illustrated below:

Hormonal Control of Oogenesis
Now that we have discussed the structures and the processes of oogenesis, we’ll move into the most complex part: hormonal regulation of oogenesis. Oogenesis is directly controlled by four hormones: follicle stimulating hormone (FSH), luteinizing hormone (LH), progesterone, and estrogen. These hormones together regulate the ovarian and menstrual cycles . The ovarian cycle refers to the release of eggs, and the menstrual cycle refers to activities in the uterine lining in preparation for possible pregnancy. We will focus only on the ovarian cycle in this course.
We’ll start with a brief overview of the roles the hormones play:
- Follicle stimulating hormone (FSH) activates follicles within the ovary to promote development of egg cells, causing eggs to finish meiosis I and pause during meiosis II. (Recall that each follicle contains one immature egg cell which was paused in meiosis I.)
- Luteinizing Hormone (LH) promotes release of the most mature egg (or in rare cases, eggs), resulting in ovulation
- Progesterone suppresses release of more FSH or LH to block activation of new follicles, allowing time for the ovulated egg to be fertilized in the oviduct and then travel to the uterus where it will implant if previously fertilized.
- Estrogen can be thought of as an ‘enhancer’ in the ovarian cycle; it enhances the activation of follicles in response to FSH, and it also enhances suppression of follicles in response to progesterone. (Estrogen also has other roles outside of the ovarian cycle, including re-growing the lining of the uterus following menstruation, and it is responsible for the secondary sexual characteristics of females such as breast development.)
Now we’ll integrate the hormone activities into the three phases of the ovarian cycle. The ovarian cycle lasts approximately 28 days on average:
Follicular phase: The first half of the ovarian cycle is the follicular phase , named for the fact that the dominant feature is the activated follicles.
- During this phase, FSH is being released from the pituitary in the brain. The slowly rising levels of FSH prompt the follicles on the surface of the ovary to grow and begin maturing the egg inside for ovulation.
- As the follicles grow, they release estrogens. Estrogens enhance the effects of FSH. The more the follicles grow, the more estrogen they release; the increasing estrogen levels cause a positive feedback loop promoting more follicle growth, which in turn promotes more estrogen release.
- Within each follicle, the maturing egg finishes meiosis I (recall that the eggs began meiosis I while the female herself was an embryo), and then pauses again during meiosis II.
Ovulation occurs near the middle of the cycle (approximately day 14), when the high level of estrogen (produced by the developing follicles) causes a rapid rise and sharp spike in levels of LH and FSH to a lesser degree (both released from the pituitary in the brain).
- The spike in LH causes ovulation: one of the mature follicles ruptures and releases its egg (still paused in meiosis II). The other mature follicles will degenerate, and their eggs are lost.
- LH and FSH levels fall immediately after ovulation, and the level of estrogen decreases when the extra follicles degenerate.
- It takes about seven days for an egg to travel through the oviduct from the ovary to the uterus, and it must be fertilized while in the oviduct. If the egg is fertilized, it will complete meiosis II, producing a single mature (and fertilized) egg.
Luteal phase: Following ovulation, the ovarian cycle enters its luteal phase , named for the fact that the dominant feature is the corpus luteum , the structure the remains from the ruptured follicle.
- During this phase, the corpus luteum produces progesterone and estrogen. Progesterone inhibits the release of further FSH or LH, suppressing activation of any new follicles. The uterus becomes prepared to accept a fertilized egg, should fertilization occur.
- The inhibition of FSH and LH by progesterone prevents any further eggs and follicles from developing. The level of estrogen produced by the corpus luteum increases to a steady level for the next few days; estrogen enhances the effects of progesterone.
What happens next depends on whether the egg was fertilized while it was in the oviduct:
- If a fertilized egg does implant in the endometrial lining of the uterine wall, then embryo produces a hormone called human chorionic gonadotropin (hCG). hCG causes the corpus luteum to remain instead of degrading, which in turn causes the ovary to continue producing high levels of progesterone. Progesterone prevents initiation of another ovarian cycle during the pregnancy. (The placenta takes over this process later in pregnancy.) Because hCG is unique to pregnancy, it is the hormone detected by pregnancy tests.
The figure below visually compares the ovarian and uterine cycles as well as the hormone levels controlling these cycles.

This video provides a great overview of the human female reproductive system, emphasizing many of the points described above:
Human Male Reproductive Anatomy
As with females, human male reproductive structures include both external and internal structures. External structures include the testicles or testes (singular: testis) and the penis. Internal structures include the vas deferens, the seminal vesicles, the prostate gland, and the bulbourethral gland.
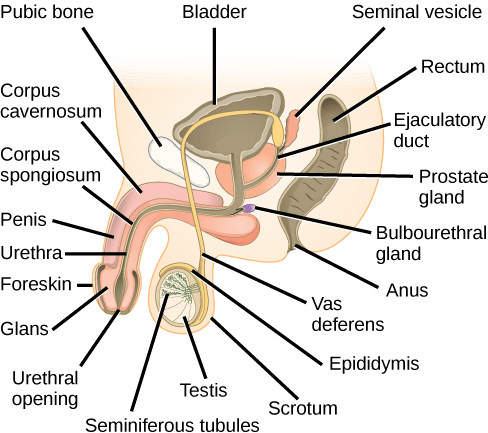
This table briefly summarizes the major organs, locations, and functions of mammalian male reproductive anatomy:
| Scrotum | External | Carry and support testes |
| Penis | External | Deliver urine, copulating organ |
| Testes | External | Produce sperm and male hormones |
| Seminal vesicles | Internal | Contribute to semen production |
| Prostate gland | Internal | Contribute to semen production |
| Bulbourethral glands | Internal | Clean urethra at ejaculation |
Human males become capable of reproduction at sexual maturity, which follows puberty. During puberty, the hypothalamus in the brain signals the pituitary gland to produce two hormones, follicle-stimulating hormone ( FSH ) and luteinizing hormone ( LH ). In males, FSH and LH stimulate the testes to produce sperm and the male sex hormone, testosterone. During puberty, these hormones together initiate development of secondary sex characteristics (such as larger penis and testes, and deeper voice) and cause the testes to begin producing mature sperm.
The scrotum houses the testes or testicles (singular: testis), which are the site of sperm development and maturation. Testes develop from the same tissue that produces ovaries in females; however, in terrestrial mammals, the cells that produce the testes migrate from within the body cavity to become external to the body during development. Why are testes external to the body in terrestrial mammals? Sperm become immobile when kept at body temperature; therefore, the scrotum and penis are external to the body in land mammals and kept at about 2 ° C lower than body temperature to maintain sperm motility. In cases where the testes do not descend through the abdominal cavity during fetal development, infertility can occur in land mammals due to the higher body temperature. Though sperm must be produced and stored at temperatures lower than body temperature in the testes, sperm are warmed to body temperature when deposited in the female reproductive tract. The immediate warming of sperm causes them to experience a burst of swimming activity, but then they begin to lose motility after several hours at body temperature.
Within the testes, sperm are produced in structures called the seminiferous tubules . Sperm production is regulated by Sertoli cells which protect the sperm stem cells and promote their development, and cells of Leydig which produce testosterone and regulate sperm development. Sperm mature as they proceed from the periphery to the lumen (interior) of the seminiferous tubules.
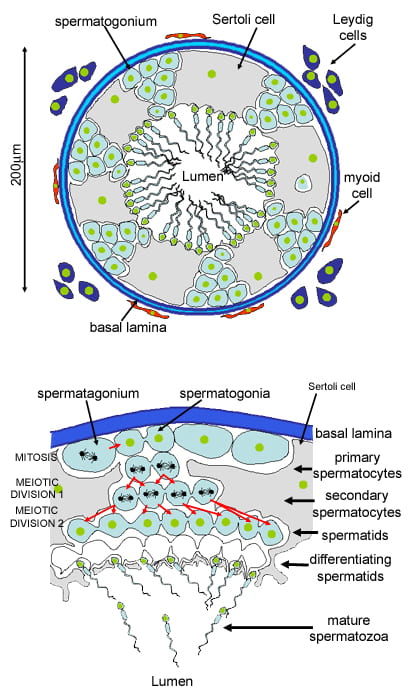
When the sperm have developed flagella and are nearly mature, they leave the testes and enter the epididymis , a structure which wraps around the testes and the location where sperm mature. During ejaculation, the sperm leave the epididymis and enter the vas deferens , which carries the sperm, behind the bladder, and forms the ejaculatory duct with the duct from the seminal vesicles.
Semen is a mixture of sperm and spermatic duct secretions and fluids from accessory glands. These glands are the seminal vesicles , the prostate gland , and the bulbourethral gland (all of which are illustrated above); together these glands contribute most of the semen’s volume:
- The seminal vesicles are a pair of glands that make thick, yellowish, and alkaline solution. Because sperm are only motile in an alkaline environment, a basic pH is important to reverse the acidity of the vaginal environment. The solution also contains mucus, fructose (a source of energy for the sperm cells), a coagulating enzyme, ascorbic acid (vitamin C), and local-acting hormones called prostaglandins (may help stimulate smooth muscle contractions in the uterus). The seminal vesicle glands account for 60 percent of the bulk of semen.
- The prostate gland acts as both a muscle and a gland. The muscle provides much of the force for ejaculation to occur. The glandular tissue makes a thin, milky fluid that contains citrate (stimulates sperm motility), enzymes, and prostate specific antigen (PSA). PSA is a proteolytic enzyme that helps to liquefy the ejaculate several minutes after release from the male. Prostate gland secretions account for about 30 percent of the bulk of semen.
- The bulbourethral gland releases its secretion just before the release of the bulk of the semen. The mucous secretions of this gland help lubricate and neutralize any acid residue in the urethra left over from urine. Secretions from the bulbourethral gland can also contain a few sperm; since these secretions are released prior to ejaculation, withdrawal of the penis from the vagina before ejaculation to prevent pregnancy may not work if sperm are present in the bulbourethral gland secretions.
Male Gametogenesis: Spermatogenesis
Spermatogenesis , illustrated below, occurs in the seminiferous tubules in the testes. Sperm stem cells, called spermatogonia , are present at birth but are inactive until puberty, when hormones from the pituitary cause the activation of the spermatogonia and the continuous production of sperm. Sperm production continues into old age. To produce sperm, a cell called a spermatocyte (a precursor to sperm) undergoes meiosis to produce four haploid spermatids (immature sperm). Once the spermatid develops a flagellum, (a tail that allows it to swim), it is called a sperm cell . Four sperm cells result from each spermatocyte that goes through meiosis. (Scroll up to compare this process to oogenesis in human females, and see how many similarities and differences you can identify.)
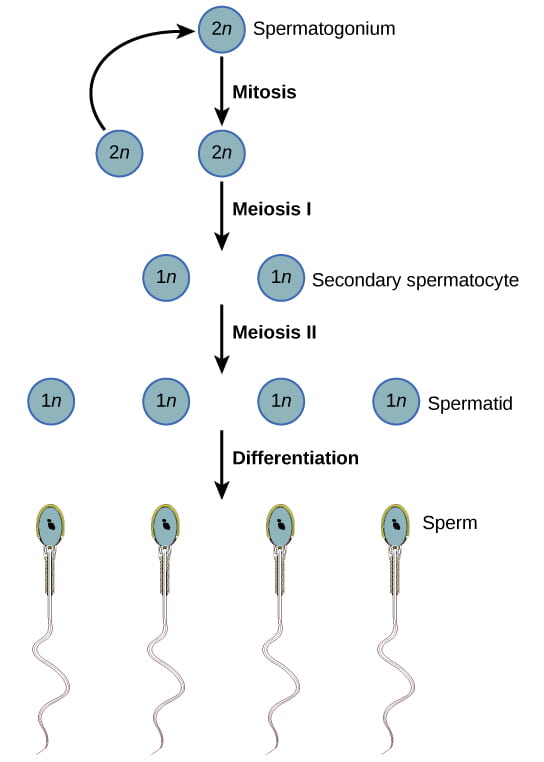
Hormonal Control of Spermatogenesis
The information below was adapted from OpenStax Biology 43.4
Now that we have discussed the structures and processes of spermatogenesis, we’ll move into discussion of hormone regulation. Just like oogenesis, spermatogenesis is controlled by follicle-stimulated hormone (FSH) and luteinizing hormone (LH). Testosterone also plays a role in spermatogenesis:
- FSH stimulates activity of the Sertoli cells to nourish the developing sperm and promote their development. Sertoli cells are located within the seminiferous tubules, and play an analogous role to follicle cells in the ovaries.
- LH stimulates the Leydig cells to produce testosterone, which promotes spermatogenesis. Leydig cells are located in the testes, outside of the seminiferous tubules.
- Testosterone further stimulates spermatogenesis by promoting maturation of the sperm after completing meiosis.
While this doesn’t occur in a monthly cycle as in females, the hormones do interact in a negative feedback cycle when sperm counts get too high (over about 20 million/ml): rising testosterone levels cause Sertoli cells to release the hormone inhibin, which acts on the hypothalamus and pituitary gland to inhibit the release of FSH and LH. The inhibition causes spermatogenesis to slow down; once the sperm levels are reduced, the Sertoli cells stop releasing inhibin, and the sperm count increases.
This video provides a great overview of the anatomy and function of the human male reproductive system:
Oogenesis vs Spermatogenesis
As we’ve seen in this reading and the videos, both eggs and sperm are produced via meiosis, but there are some big differences:
- Initiation : Egg production begins during embryonic development (before birth), then is arrested during meiosis until puberty; sperm production does not begin until puberty
- Completion : Egg production is not actually completed until after fertilization (!), while sperm production is complete prior to ejaculation
- Number : Egg production results in only a single egg from each egg stem cell; sperm production results in four sperm from each sperm stem cell.
- Timing : Once an individual enters puberty, sperm production is continuous in a “conveyor belt” process; egg production occurs one-at-a-time at each menstrual cycle.
Contraception and Birth Control
The information below was adapted from OpenStax Biology 43.5
We’ll wrap this discussion up with an overview of contraception. Contraception (prevention of pregnancy), can be categorized by according to whether they block gamete production or gamete union (fertilization):
- Hormone-based birth control methods use synthetic progesterone (sometimes in combination with estrogen), which inhibits production of FSH and LH, and thus prevent an egg from being maturing or being released. Progesterone is the primary hormone that blocks FSH and LH release, but estrogen enhances its effect and increases the reliability of this method. This method includes “the pill” as well as other methods of delivering the hormone(s) such as implants under the skin; methods such as skin implants are more reliable due to the continuous release of progesterone.
- Intrauterine devices (IUDs) are small T-shaped devices that are inserted into the uterus. IUDs induce an inflammatory response in the uterus that creates a toxic environment to the sperm and prevents them from reaching the oviducts. Some IUDs that contain progesterone which is continually secreted to suppress egg production and ovulation; others are copper-coated which alters the cervical mucus making it more difficult for sperm to reach the egg. Both types of IUDs are more reliable than standard hormone-based birth control.
- Emergency contraception, also known as “Plan B” or the “morning-after pill” is a hormone-based method of contraception containing a high dose of synthetic progesterone, which temporarily blocks egg maturation and ovulation, allowing time for sperm to die in the oviduct before the egg is released. It can also act after ovulation slowing down movement of the egg and thickening cervical mucus which slows movement of sperm. One common misconception about emergency contraception is that it prevents implantation after fertilization; however, it has no impact after fertilization.
- Barrier methods, such as condoms, cervical caps, and diaphragms, block sperm from entering the uterus, preventing fertilization. Spermicides are chemicals that are placed in the vagina that kill sperm. Sponges, which are saturated with spermicides, are placed in the vagina at the cervical opening. Combining spermicides with barrier methods is more effective than using either alone.
- Vasectomies block sperm from exiting the body during ejaculation (contrary to popular misconception, vasectomies do not block sperm production – only sperm release). A section of the vas deferens is removed, so sperm are still produced but cannot reach the urethra to be ejaculated. No other structures are affected, and so all other components of ejaculate are still present. Vasectomy is one of the most effective methods of birth control.
- Tubal ligation is the female equivalent to a vasectomy in that it involves severing and sealing the oviducts; eggs are still produced and ovulated from the ovaries, but they are unable to reach the oviducts for fertilization. However, unlike vasectomies which are performed through the scrotum, tubal ligation requires abdominal surgery to reach the oviducts. Tubal ligation is also among the most effective methods of birth control.
Methods of contraception to prevent pregnancy have varying probabilities of success. In the diagram below, the failure rate is the given as the percent of women who become pregnant during the first year of use of that method. Work through the methods in this diagram to determine the most effective strategies for preventing pregnancy. Methods in combination, such as spermicidal chemicals and barrier, prevent pregnancy more effectively than do the methods when used separately.
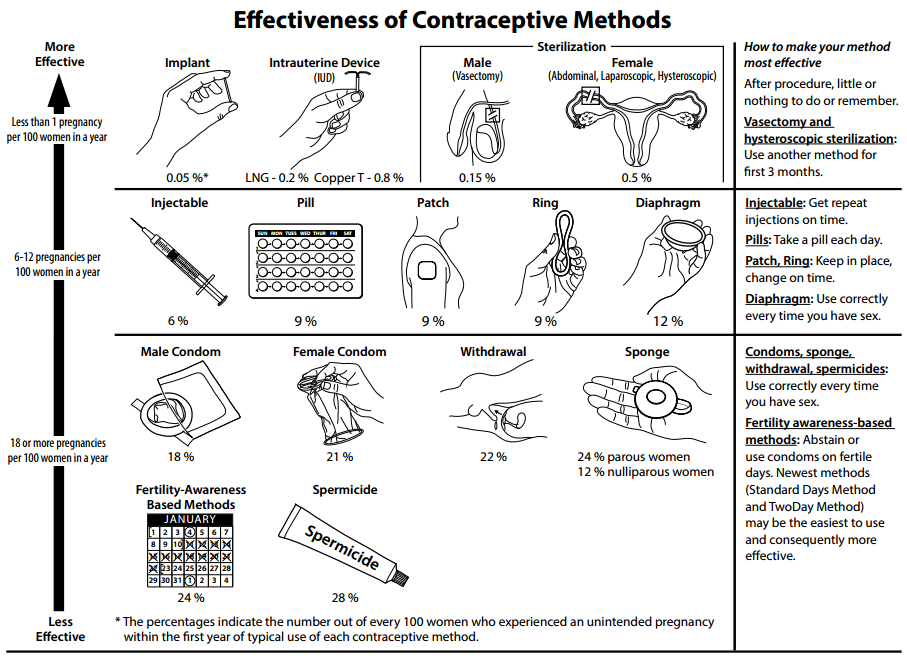
This video provides a quick overview of hormone-based birth control, with emphasis on emergency contraception:
- Entries RSS
- Comments RSS
- Sites@GeorgiaTech
Creative Commons License
Vannevar bush.
“Science has a simple faith, which transcends utility. It is the faith that it is the privilege of man to learn to understand, and that this is his mission.”
SEER Training Modules
of the page. Use an empty to account for some browsers not moving keyboard focus after jump. * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * --> Introduction to the Reproductive System
The major function of the reproductive system is to ensure survival of the species. Other systems in the body, such as the endocrine and urinary systems, work continuously to maintain homeostasis for survival of the individual. An individual may live a long, healthy, and happy life without producing offspring, but if the species is to continue, at least some individuals must produce offspring.
Within the context of producing offspring, the reproductive system has four functions:
- To produce egg and sperm cells
- To transport and sustain these cells
- To nurture the developing offspring
- To produce hormones
These functions are divided between the primary and secondary, or accessory , reproductive organs. The primary reproductive organs, or gonads, consist of the ovaries and testes. These organs are responsible for producing the egg and sperm cells gametes), and hormones. These hormones function in the maturation of the reproductive system, the development of sexual characteristics, and regulation of the normal physiology of the reproductive system. All other organs, ducts, and glands in the reproductive system are considered secondary, or accessory, reproductive organs. These structures transport and sustain the gametes and nurture the developing offspring.

- History & Society
- Science & Tech
- Biographies
- Animals & Nature
- Geography & Travel
- Arts & Culture
- Games & Quizzes
- On This Day
- One Good Fact
- New Articles
- Lifestyles & Social Issues
- Philosophy & Religion
- Politics, Law & Government
- World History
- Health & Medicine
- Browse Biographies
- Birds, Reptiles & Other Vertebrates
- Bugs, Mollusks & Other Invertebrates
- Environment
- Fossils & Geologic Time
- Entertainment & Pop Culture
- Sports & Recreation
- Visual Arts
- Demystified
- Image Galleries
- Infographics
- Top Questions
- Britannica Kids
- Saving Earth
- Space Next 50
- Student Center
- Introduction
Molecular replication
Molecular reproduction.
- Binary fission
- Multiple fission
- Reproduction of organisms
- Life cycles of plants
- Life cycles of animals
- The evolution of reproduction
- The evolution of variation control

reproduction
Our editors will review what you’ve submitted and determine whether to revise the article.
- Biology LibreTexts - Reproduction
- Khan Academy - Types of reproduction review
- Milne Library - Reproduction: development and physiology
- Merck Manuals - Professional Version - Conception and Prenatal Development
- National Center for Biotechnology Information - PubMed Central - Research in Reproduction: Challenges, Needs, and Opportunities
- Michigan State University Libraries - An Interactive Introduction to Organismal and Molecular Biology, 2nd ed. - Reproduction
- BCCampus Publishing - Reproduction Methods
- Table Of Contents
reproduction , process by which organisms replicate themselves.
In a general sense reproduction is one of the most important concepts in biology : it means making a copy, a likeness, and thereby providing for the continued existence of species . Although reproduction is often considered solely in terms of the production of offspring in animals and plants, the more general meaning has far greater significance to living organisms. To appreciate this fact, the origin of life and the evolution of organisms must be considered. One of the first characteristics of life that emerged in primeval times must have been the ability of some primitive chemical system to make copies of itself.
At its lowest level, therefore, reproduction is chemical replication. As evolution progressed, cells of successively higher levels of complexity must have arisen, and it was absolutely essential that they had the ability to make likenesses of themselves. In unicellular organisms, the ability of one cell to reproduce itself means the reproduction of a new individual; in multicellular organisms, however, it means growth and regeneration . Multicellular organisms also reproduce in the strict sense of the term—that is, they make copies of themselves in the form of offspring—but they do so in a variety of ways, many involving complex organs and elaborate hormonal mechanisms.
Levels of reproduction
The characteristics that an organism inherits are largely stored in cells as genetic information in very long molecules of deoxyribonucleic acid ( DNA ). In 1953 it was established that DNA molecules consist of two complementary strands, each of which can make copies of the other. The strands are like two sides of a ladder that has been twisted along its length in the shape of a double helix (spring). The rungs, which join the two sides of the ladder, are made up of two terminal bases. There are four bases in DNA : thymine, cytosine, adenine, and guanine. In the middle of each rung a base from one strand of DNA is linked by a hydrogen bond to a base of the other strand. But they can pair only in certain ways: adenine always pairs with thymine, and guanine with cytosine. This is why one strand of DNA is considered complementary to the other.

The double helices duplicate themselves by separating at one place between the two strands and becoming progressively unattached. As one strand separates from the other, each acquires new complementary bases until eventually each strand becomes a new double helix with a new complementary strand to replace the original one. Because adenine always falls in place opposite thymine and guanine opposite cytosine, the process is called a template replication —one strand serves as the mold for the other. It should be added that the steps involving the duplication of DNA do not occur spontaneously; they require catalysts in the form of enzymes that promote the replication process.
The sequence of bases in a DNA molecule serves as a code by which genetic information is stored. Using this code, the DNA synthesizes one strand of ribonucleic acid ( RNA ), a substance that is so similar structurally to DNA that it is also formed by template replication of DNA. RNA serves as a messenger for carrying the genetic code to those places in the cell where proteins are manufactured. The way in which the messenger RNA is translated into specific proteins is a remarkable and complex process. (For more detailed information concerning DNA, RNA, and the genetic code, see the articles nucleic acid and heredity: Chromosomes and genes ). The ability to synthesize enzymes and other proteins enables the organism to make any substance that existed in a previous generation. Proteins are reproduced directly; however, such other substances as carbohydrates, fats, and other organic molecules found in cells are produced by a series of enzyme-controlled chemical reactions, each enzyme being derived originally from DNA through messenger RNA. It is because all of the organic constituents made by organisms are derived ultimately from DNA that molecules in organisms are reproduced exactly by each successive generation.
Cell reproduction

The chemical constituents of cytoplasm (that part of the cell outside the nucleus) are not resynthesized from DNA every time a cell divides. This is because each of the two daughter cells formed during cell division usually inherits about half of the cellular material from the mother cell (see cell: Cell division and growth ), and is important because the presence of essential enzymes enables DNA to replicate even before it has made the enzymes necessary to do so.
Cells of higher organisms contain complex structures, and each time a cell divides the structures must be duplicated . The method of duplication varies for each structure, and in some cases the mechanism is still uncertain. One striking and important phenomenon is the formation of a new membrane . Cell membranes, although they are very thin and appear to have a simple form and structure, contain many enzymes and are sites of great metabolic activity. This applies not only to the membrane that surrounds the cell but to all the membranes within the cell. New membranes, which seem to form rapidly, are indistinguishable from old ones.
Thus, the formation of a new cell involves the further synthesis of many constituents that were present in the parent cell. This means that all of the information and materials necessary for a cell to reproduce itself must be supplied by the cellular constituents and the DNA inherited from the parent cell.

IMAGES
VIDEO
COMMENTS
gonad. gamete. viviparity. fertility. human reproductive system, organ system by which humans reproduce and bear live offspring. Provided all organs are present, normally constructed, and functioning properly, the essential features of human reproduction are (1) liberation of an ovum, or egg, at a specific time in the reproductive cycle, (2 ...
Female reproductive system. There are several organs and tissues that make up the female reproductive system, these include that ovaries, fallopian tubes, uterus, vagina, vulva, mammary glands and breasts. They are also involved in producing and transporting gametes and in the production of sex hormones. The female reproductive system is also ...
Human reproduction is an example of sexual reproduction. In human beings, both males and females have different reproductive systems; hence, they are known to exhibit sexual dimorphism. Males have testes- also called testicles, while the females have a pair of ovaries. Also read: Sexual Reproduction.
Female reproductive system. The human female reproductive system is a series of organs primarily located inside the body and around the pelvic region of a female that contribute towards the reproductive process. The human female reproductive system contains three main parts: the vagina, which leads from the vulva, the vaginal opening, to the uterus; the uterus, which holds the developing fetus ...
Fertilization is the initial stage of human reproduction or procreation which involves the fusion of a female's ovum or egg with the male's sperm in the ampulla of the uterus (Cummings, 2009, p.165). The union occurs when a male and a female engage in sexual intercourse whereby during ejaculation, the sperms in the vagina travel through the ...
The main structures of the male reproductive system are external to the body and illustrated in Figure 18.2.3. The two testes (singular, testis) hang between the thighs in a sac of skin called the scrotum.The testes produce both sperm and testosterone.Resting atop each testis is a coiled structure called the epididymis (plural, epididymes). The function of the epididymes is to mature and store ...
The Human Male Reproductive System: Cross-sectional diagram of the male reproductive organs. Only our species has a distinctive mushroom-capped glans, which is connected to the shaft of the penis by a thin tissue of frenulum (the delicate tab of skin just beneath the urethra). One of the most significant features of the human penis is the ...
Figure 18.13 The structures of the human ovarian reproductive system are shown. (credit a: modification of work by Gray's Anatomy; credit b: modification of work by CDC) The breasts consist of mammary glands and fat. Each gland consists of 15 to 25 lobes that have ducts that empty at the nipple and that supply the nursing child with nutrient ...
This open textbook is designed to provide a deep understanding of the biological and biomedical aspects of human reproduction, covering a wide range of topics from basic reproductive biology to clinical applications. The book starts with foundational knowledge and progresses to more advanced topics while also including real-world clinical orientation for practical contexts.
The reproductive system is a collection of internal and external sex organs which work together for the purpose of sexual reproduction.. The development of these reproductive organs begins at an early stage in the embryo. There is a close link throughout with the development of the urinary system.. This article will look at the origins of both male and female sex organs; including the gonads ...
Human reproduction is sexual reproduction that results in human fertilization to produce a human offspring. It typically involves sexual intercourse between a sexually mature human male and female. [1] During sexual intercourse, the interaction between the male and female reproductive systems results in fertilization of the ovum by the sperm to form a zygote. [1]
Reproductive System Research Essay Between the two reproductive systems, each contain their own function to provide for the human body. In the female reproductive system, the different parts include: the ovary, ovum, fallopian tube, uterus, cervix, vulva, and the vagina. These different parts contribute to the female reproductive cycle.
Male reproductive system: The male reproductive function is to produce sperm so it can transfer them to the female reproductive tract. The paired testes are very important in this process as they produce both sperm and androgen, testosterone is the most important male hormone as this supports the male reproductive process.
Essay on the Female Reproductive System: As in the male, in female the ovary also performs the functions of gametogenesis and as an endocrine gland. Ova released from the ovary enter the oviducts and Fallopian tube. Fertilization of the ovum usually occurs in the fallopian tubes by the spermatozoa released by the male during copulation.
The male reproductive system is a series of organs located outside and in pelvis region. The male reproductive systems main purpose is to provide sperm to fertilize the ovum. The major parts of the male are the sperm production and storage. The first category is sperm production and storage. The production of sperm occurs in the testes.
Get Help With Your Essay. If you need assistance with writing your essay, our professional essay writing service is here to help! Find out more about our Essay Writing Service. The journey begins in the male reproductive system. Hanging outside the pelvic cavity of a man lies a sack of skin which is known as a scrotum.
The female reproductive system is framed to perform different functions. It creates egg cells that are essential for reproduction known as ova. The system is organized to deliver the ova to the region of fertilization. The egg fertilization takes place in the Fallopian tubes along with the sperm. The implanting in the walls of the uterus and ...
Reproductive structures produce gametes (eggs and sperm) and facilitate the meeting of gametes to produce a zygote (fertilized egg). In animals ranging from insects to humans, males produce sperm in testes, and the sperm are stored in the epididymis until ejaculation. Sperm are small, mobile, "low-cost" cells that are produced in high numbers.
If you're seeing this message, it means we're having trouble loading external resources on our website. If you're behind a web filter, please make sure that the domains *.kastatic.org and *.kasandbox.org are unblocked.
Introduction to the Reproductive System. The major function of the reproductive system is to ensure survival of the species. Other systems in the body, such as the endocrine and urinary systems, work continuously to maintain homeostasis for survival of the individual. An individual may live a long, healthy, and happy life without producing offspring, but if the species is to continue, at least ...
cell division. asexual reproduction. (Show more) reproduction, process by which organisms replicate themselves. In a general sense reproduction is one of the most important concepts in biology: it means making a copy, a likeness, and thereby providing for the continued existence of species. Although reproduction is often considered solely in ...